Introduction
Renal anemia is one of the common complications in patients with chronic kidney disease, and has a correlation with the severity of chronic kidney disease. Investigations show that more than 90% of uremic maintenance hemodialysis patients have renal anemia, which seriously threatens the life safety of patients [
1]. Renal anemia demonstrates a considerable incidence in patients with uremia, because the patient's renal function is impaired, the glomerular filtration is less than 30mL/min, and the serum creatinine exceeds 300μmol/L, and the hemoglobin shows a significant decrease. It presents with normochromic normocytic, hypoproliferative anemia that is associated with adverse reactions such as chills, lethargy, palpitations, shortness of breath, muscle weakness, loss of appetite, inability to concentrate, etc. [
2]. Additionally, it has a negative impact on the patient's intelligence and memory, showing a gradual decrease. Worse still, renal anemia can degrade the patient's mobility, thereby hindering their normal life and compromising the quality of life [
3,
4].
There are multiple contributors to renal anemia, but it is majorly associated with iron metabolism disorders in the body and absolute or relative insufficiency of iron and erythropoietin caused by renal dysfunction, as well as insufficient dialysis, malnutrition, invisible blood loss, and inflammation [
5]. At this stage, there are three commonly used methods for the treatment of renal anemia. ①Supplemention of erythrocyte production stimulators: the more commonly used drugs in clinical are recombinant human erythropoietin, daepetin-α, etc.; ②Iron supplementation: This method is a relatively basic treatment method that mainly corrects the patient's anemia by means of iron supplementation, and is aimed at the unsatisfactory effect of oral iron; ③ Targeted treatment of factors that affect or promote anemia, such as plasma clearance toxic substances, use of anti-erythropoietin antibodies, correction of malnutrition, etc. [
6,
7]. However, studies have shown that high-dose application of exogenous erythropoietin cannot completely correct the anemia [
8].
Roxadustat is an oral small-molecule hypoxia-inducible factor prolyl hydroxylase inhibitor drug, which can comprehensively regulate various factors that cause anemia, and can promote the level of endogenous erythropoietin and the absorption of iron, and the drug has a good corrective effect on the inhibition of erythropoiesis affected by inflammatory factors [
9]. Roxadustat can significantly increase hemoglobin levels in the treatment of anemia in non-dialysis-dependent chronic kidney disease patients, which is more effective than placebo [
10]. Inflammatory factors in the patient's body is linked to the level of hepcidin, and it causes iron retention and aggravates the disease when it increases. Roxadustat can play a role in reducing the level of inflammatory factors in patients, thereby reducing its impact on anemia in patients [
11].
HCT is an index to measure the ratio of red blood cells after centrifugal anticoagulation. Anemia, hemoconcentration or dilution are closely related to its measured value, so the change of its value is often used as the standard for evaluating the blood volume change of patients [
12]. Determination of SF contributes to diagnose iron deficiency anemia in patients. TSAT refers to the iron transport and the availability of iron to the bone marrow. A reasonable TSAT in dialysis patients can avoid the fluctuation of Hb and maintain at the standard level, which serves as the main diagnostic basis for iron bioavailability [
13]. In addition, the application of high-dose recombinant human erythropoietin (rHuEPO) may lead to the risk of hypertension, thromboembolism, and cardiovascular events. In clinical trials of roxadustat, a small number of patients experienced elevated blood pressure, but animal experiments indicated no increase of blood pressure [
14]. In light of this, this study observed the effect of roxadustat on blood pressure and micro-inflammatory response in patients with hemodialysis anemia.
2. Materials and Methods
2.1. Participants
This study included 100 hemodialysis anemia patients, all of whom were hospitalized in the Department of Nephrology of our hospital. A random number table was generated using a computer-based tool, and the patients were randomized into two groups. Before enrollment, all participants provided signed informed consent. The study protocol was approved by the hospital ethics committee, and all procedures were in compliance with the ethical guidelines in the Declaration of Helsinki. (
Table 1)
2.2. Inclusion and exclusion criteria
Inclusion criteria: ①Met the diagnostic criteria for renal anemia; ②All patients were on maintenance hemodialysis; ③Hemodialysis time was more than 3 months; ④All signed informed consent. ⑤Be able to strictly follow the doctor's orders to take medicine;
Exclusion criteria: ①with aplastic anemia and other blood system diseases; ②with active ulcer; ③ with malignant tumor; ④with allergy to the drugs in this study; ⑤severe insufficiency of organs such as liver and kidney; ⑥severe malnutrition (plasma albumin <25g/L); ⑦pregnant or lactating women; ⑧insufficient dialysis; ⑨ pure red blood cell aplastic anemia; ⑩ thalassemia.
2.3. Intervention methods
After admission, the patients were treated with basic drugs such as iron and lipid-lowering drugs according to their individual conditions. All patients underwent regular high-flux hemodialysis treatment, and the treatment time was controlled at 4h/time, 3 times/week.
Control group: patients in the control group were given recombinant human erythropoietin injection. After maintenance hemodialysis, intravenous injection of human erythropoietin injection was given, 3000IU/time, 1-3 times/week.
Study group: patients in the study group received roxadustat treatment, i.e., the patients took roxadustat capsules orally, and the initial dose was determined according to the individual weight of the patients (body weight>60kg, 120mg/time, body weight 45-60kg, 100mg/time), 3 times/time week. One course of treatment lasted for one week, and the two groups were treated consecutively for 12 weeks.
2.4. Observation indicators
2.4.1. Clinical efficacy
The clinical efficacy was assessed after 12 weeks of treatment. Markedly effective: the clinical symptoms such as pale complexion, fatigue, palpitations, etc. are significantly mitigated, hemoglobin ≥100g/L, hematocrit increased ≥0.1 compared to baseline parameters; effective: clinical symptoms are mitigated, hemoglobin increased ≥15g/L, hematocrit ≥0.05; ineffective: clinical symptoms, hematocrit and hemoglobin were basically the same as the corresponding values at baseline, or even worsening. Total effective rate = (effective + markedly effective) number of cases/total number of cases × 100%.
2.4.2. Blood lipid metabolism
4ml of fasting cubital venous blood was collected from the two groups before treatment and after 12 weeks of treatment, and the levels of low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC) and triglyceride (TG) were detected by Roche 8000 automatic biochemical analyzer (made in Switzerland).
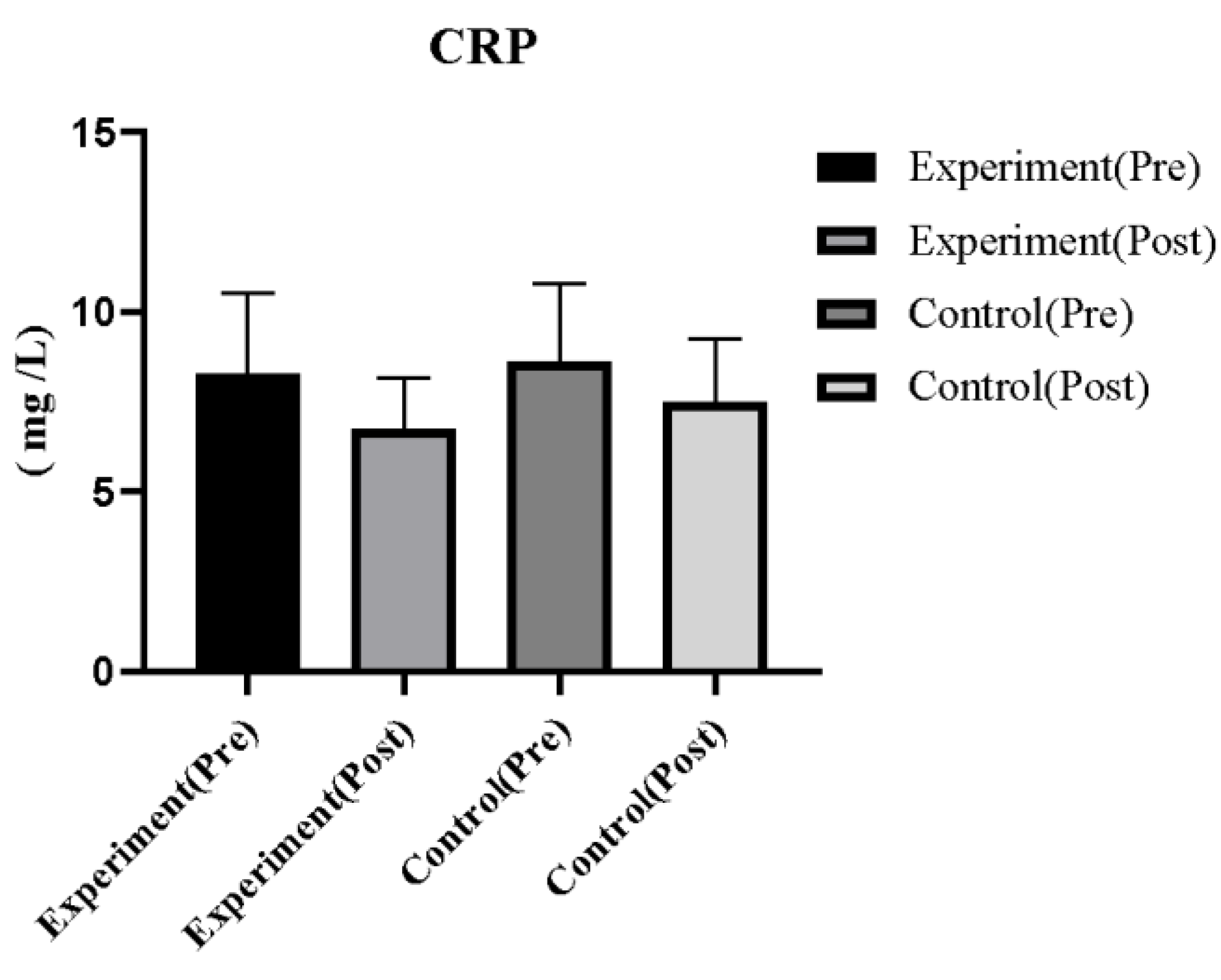
2.4.3. Levels of inflammatory factors
4 ml of fasting cubital venous blood was collected from the two groups before and after treatment, and serum was centrifuged by Baiyang BY-600A low-speed at a speed of 3000r/min, and a radius of 13cm, for 10 min, and the serum C-reactive protein (CRP) levels of the two groups were detected by enzyme-linked immunosorbent assay.
2.4.4. Iron metabolism-related indicators
Before and after treatment, the above sera were collected to detect serum transferrin saturation (TSAT) and ferritin levels in the two groups, and serum hepcidin levels in the two groups were detected by enzyme-linked immunosorbent assay.
2.4.5. Blood biochemical indicators
Including blood calcium, blood phosphorus, parathyroid hormone (PTH), albumin (Alb), and serum creatinine (SCr).
2.4.6. Anemia indicators
Red blood cells (RBC), Hb, hematocrit (Hct), and reticulocytes (RTC) were determined.
2.4.7. Adverse reactions
Adverse reactions in the two groups during the treatment period were recorded.
2.4.8. The mean arterial pressure of the patient before dialysis
The average value of the 4 blood pressure values were taken; for instance, the dialysis was performed on Monday, Wednesday, and Friday, and then the 4 values of the mean arterial pressure before dialysis on Wednesday were averaged.
Before and after treatment, 5ml of fasting venous blood was collected from patients, and an automatic biochemical analyzer was used to detect serum calcium, blood phosphorus, Alb, TG, TC, SCr, serum iron, ferritin, total iron binding capacity and other indicators, calculate TSAT; RBC, Hb, Hct and other indicators were detected by blood cell analyzer; CRP was detected by immunoturbidimetric method; PTH level was detected by immunochemical fluorescence method.
2.5. Statistical analysis
All data analysis were performed using SPSS 23.0 statistical software. The enumeration data were expressed as n (%) and analyzed by χ2 test, and the measurement data were expressed as the mean ± standard deviation (Mean ± SD), and the independent samples t test was used for comparison between groups, and the paired samples t test was used for comparison within groups. P values of <0.05 were considered statistically significant.
4. Discussion
Chronic kidney disease (CKD) is a long-term progressive disease characterized by progressive loss of renal function, which can eventually lead to end-stage renal disease. Renal anemia is a common complication, and the incidence of anemia increases with the progression of CKD [
15,
16,
17,
18]. The mechanism of renal anemia mainly includes the following aspects: (1) Various types of kidney diseases cause insufficient production of erythropoietin (EPO), and anemia caused by toxic substances in the plasma of patients with uremia that interfere with the production and metabolism of erythrocytes; (2) The reduction of EPO and the stimulation of inflammatory factors will cause the increase of hepcidin synthesis in the liver, which will eventually lead to the absorption and utilization of iron disorders; (3) When renal failure occurs, renal blood flow is reduced, the renal tubulointerstitium is destroyed, the sensitivity of EPO-secreting cells to hypoxia is reduced, the production of EPO is reduced, resulting in absolute deficiency of EPO, resulting in a reduction in the rate of erythropoiesis, and an inflammatory response state. The lack of hematopoietic raw materials, the inhibitory effect of PTH on the bone marrow, and acute and chronic blood loss will further aggravate the degree of anemia [
19,
20].
In recent years, erythropoietin recombinant variants have been used clinically to induce the production of erythrocytes, but they lacked the desired effect. Studies have also shown that long-term high-dose use will increase the incidence of cardiovascular and cerebrovascular, hypertension and other adverse events [
21]. Therefore, it is of great clinical significance to seek a safe and effective regimen for the treatment of renal anemia in uremic maintenance hemodialysis. Roxadustat belongs to a hypoxia-inducible factor prolyl hydroxylase inhibitor (HIF-PHI). When the partial pressure of oxygen is normal, the drug can inhibit the degradation of hypoxia-inducible factor and effectively maintain its stability. , and then promote the production of endogenous erythropoietin, improve the utilization rate of iron, and comprehensively regulate erythropoiesis [
22]. Roxadustat can effectively regulate the level of erythropoietin in the body after entering the patient's body. Among the substances that regulate and induce oxygen in the kidneys, hypoxia-inducible factor plays an important role, mainly composed of heterodimers, and also plays an important role in the regulatory factor of erythropoietin [
23].
The results of this study showed that after treatment, the clinical efficacy and ferritin saturation of the study group were higher, and the levels of LDL, TG, serum CRP, ferritin, and hepcidin were lower in the study group, suggesting that roxadustat treatment is effective in maintaining blood circulation. Dialysis patients with renal anemia have exact curative effect, can improve the blood lipid metabolism level, reduce the body's inflammatory response, and can regulate iron metabolism.Reason for analysis: Roxadustat is a novel drug for the treatment of renal anemia. It can stabilize the hypoxia-inducible factor, inhibit the degradation of hypoxia-inducible factor, increase the concentration of erythropoietin, and increase the expression of erythropoietin receptor. Sensitivity, promote the production of red blood cells, can increase the saturation of transferrin, reduce hepcidin, thereby promoting the body's utilization and absorption of iron [
24]. Studies have shown that hepcidin is a peptide substance (containing 25 amino acids) that can sequester iron in organs. In addition, the availability of stored iron is limited, thereby reducing the body's iron utilization and iron transport, resulting in functional deficiency. iron, thereby causing anemia of inflammation, and it is regulated by hypoxia-inducible factor [
25]. Relevant studies have shown that roxadustat can correct renal anemia in patients with chronic kidney disease by stabilizing hypoxia-inducible factor, thereby regulating erythropoietin synthesis, and regulating iron metabolism (promoting iron absorption, promoting iron transport, and reducing hepcidin) [
26]. Roxadustat can correct the anemia in patients with uremic maintenance hemodialysis renal anemia through multiple ways, such as improving the body's reabsorption of endogenous iron and the absorption of exogenous iron; simulating intracellular hypoxia to promote the body to produce endogenous erythropoietin; regulating the body's inflammatory response by reducing the level of hepcidin [
27,
28].
In addition, roxadustat is also effective in improving blood biochemical indicators, anemia indicators and blood pressure. Because roxadustat can improve the level of hypoxia-inducible factor in the body after entering the patient's body, thereby promoting the level of erythropoietin, providing favorable conditions for the patient's hematopoietic function, thereby improving the patient's anemia status [
29]. In addition, roxadustat is the world's first oral HIF-PHI. After oral administration, the drug can inhibit the activity of prolyl hydroxylase (PHD) in the human body and effectively maintain the stability of hypoxia-inducible factor (HIF), promoting EPO/EPOR expression. In addition, when the drug is used to treat renal anemia, it can also reduce the serum hepcidin level in the body through different ways, and there is no need for additional intravenous iron supplementation. Therefore, sadustat can not only simulate the hypoxic environment in cells, and then produce a large amount of erythropoietin, but also promote the absorption of iron in the body without being affected by inflammation, and finally achieve the purpose of effectively correcting renal anemia [
30,
31]. The results of this study showed that there was no significant difference in the incidence of adverse reactions between the two groups during the treatment period between the control group and the study group, and the adverse reactions of the two groups could be relieved spontaneously without special treatment, suggesting that roxadustat in the treatment of maintenance hemodialysis kidney It has a good safety profile in patients with anemia.
With the continuous advancement of medical research, in-depth research on hypoxia-inducible factor (HIF) in recent years has provided a new therapeutic direction for the treatment of renal anemia. HIF promotes erythropoietin (EPO) gene synthesis under hypoxic conditions Under normal oxygen supply conditions, HIF is rapidly hydroxylated and degraded by prolyl hydroxylase (PHD) after synthesis, but the catalytic activity of PHD is inhibited under hypoxic conditions [
32]. Roxadustat is a kind of HIF-PHI, which inhibits the activity of PHD, so that the concentration of HIF remains stable, promotes the expression of EPO/erythropoietin receptor (EPOR), increases the utilization of iron, and relieves the symptoms of anemia. Therefore, the diagnosis and treatment effect of this method is more prominent [
33]. It can be seen that the clinical effect of oral roxadustat capsule in the treatment of patients with chronic kidney disease and renal anemia is better than that of subcutaneous injection of rHuEPO for injection. Our preliminary study showed that roxadustat treatment of anemia had little effect on blood pressure in maintenance hemodialysis patients compared with rHuEPO treatment. It has less impact on blood pressure and cardiac workload, and has a lower incidence of cardiovascular and cerebrovascular complications, which is worthy of in-depth clinical research and discussion. Further research is needed on the effect of roxadustat on blood pressure in patients and its mechanism.
This trial performed roxadustat treatment for patients with hemodialysis anemia, which has certain guiding significance, but there are still the following problems: (1) the sample size of this study is small, and only a single-center trial was conducted, which might lead to bias; (2) During the research process, the test results could not be evaluated blindly, and there might be measurement bias; (3) the observation period of this study was short and there was no long-term follow-up. Although the short-term clinical efficacy was observed, the long-term efficacy could not be evaluated.