1. Introduction
The maturation of an arteriovenous fistula (AVF) is a complex process involving changes in both the artery and vein, characterized by their enlargement, and subsequential increasing blood flow. Over 80% of patients, suffering from chronic kidney disease (CKD), started hemodialysis (HD), in 2019, using catheter, due to the lack of AVF or inability to cannulate it. Depending on age, 58.7% to 64.8% of prevalent HD patients utilized a AVF and 15.0% to 20.2% utilized a graft.[
1] Typically, a prolonged maturation time is associated with factors preceding AVF formation, such as vein destruction and radial artery (RA) atherosclerosis. In addition, the type of anastomosis may increase the risk of intima-media hyperplasia and juxta anastomosis stenosis.[
2,
3] Finally, lower vessel sizes may result in technical errors during suturing by creating AVF, using the classic method (modus Rohl et al.).[
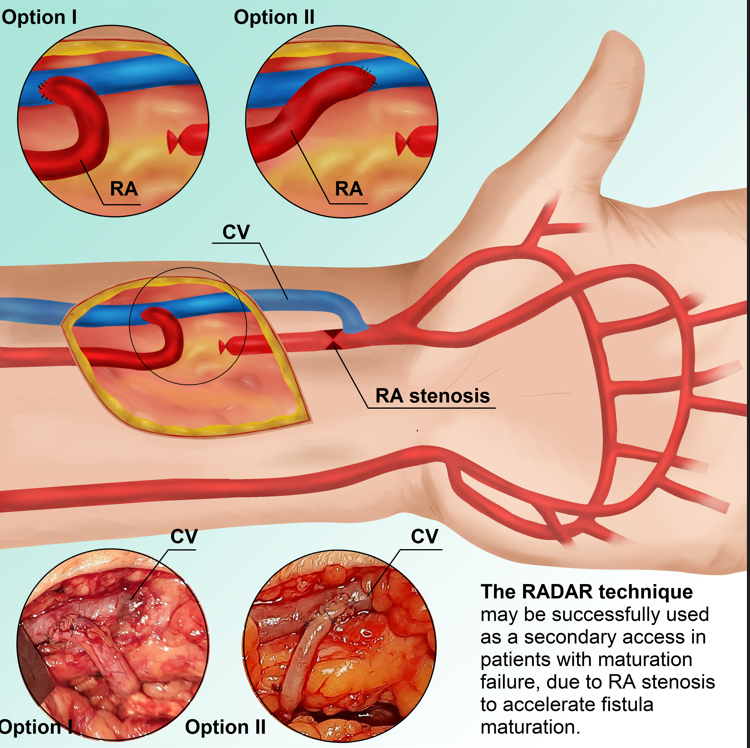
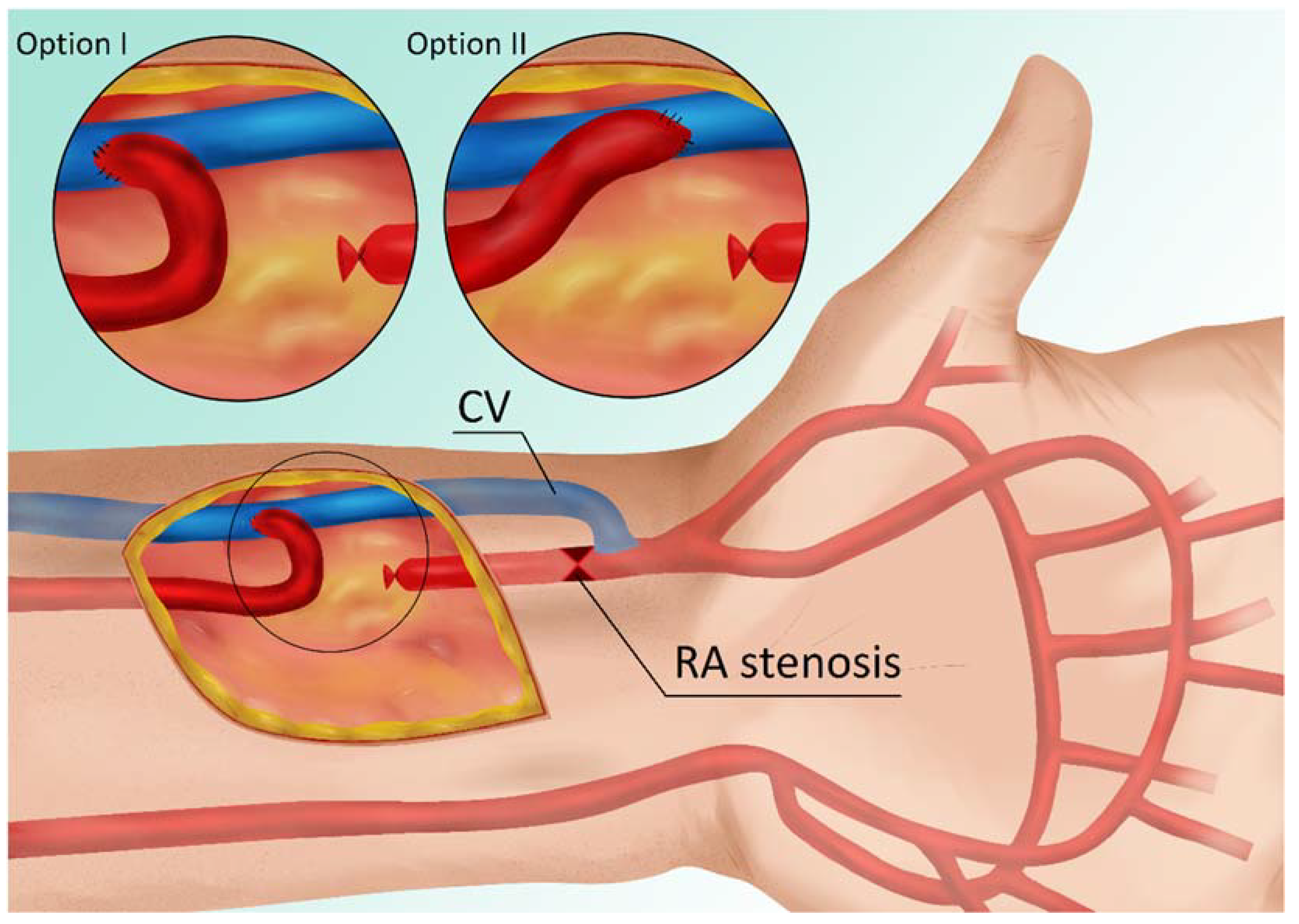
4] In patients with small vessels, there is a risk of narrowing the lumen of the radial artery in the proximal portion of the anastomosis (see red point X in
Figure 1), which either reduces the blood supply to the vein/fistula or causes the AVF to be supplied only by the ulnar artery.
In the case of AVF maturation failure, surgical or endovascular procedures are used. Studies demonstrated that surgical techniques are superior to endovascular ones.[
5] Surgical reanastomosis proximal to a previously created AVF or accessory vein ligation are two surgical options. Since the vessels are dilated, because of the primary anastomosis, the reanastomosis is simplified and the side of the enlarged radial artery is connected to the end of the vein, resulting in a significantly higher blood flow than the first AVF. The need to ligate the vein distally and the irreversible closure of the primary anastomosis are disadvantages of this technique. In 2016, Sadaghianloo et al. demonstrated favorable outcomes of radial artery deviation and reimplantation (RADAR) technique with less juxta-anastomotic stenosis, increased maturation, and patency compared to standard radial-cephalic fistulas.[
6] However, this approach has a significant disadvantage, when performed as a primary AVF because it requires ligation of the radial artery and has been criticized by some authors.[
7] Nonetheless, we utilized this technique as a secondary fistula in patients whose primary fistula maturation process failed due to RA stenosis. We describe such solution and explain why the RADAR is an appropriate technique for reducing fistula maturation time in similar cases. This method was applied to three patients, and the diagnosis and procedure were described in detail.
2. Material and Methods
2.1. Description of Case 1.
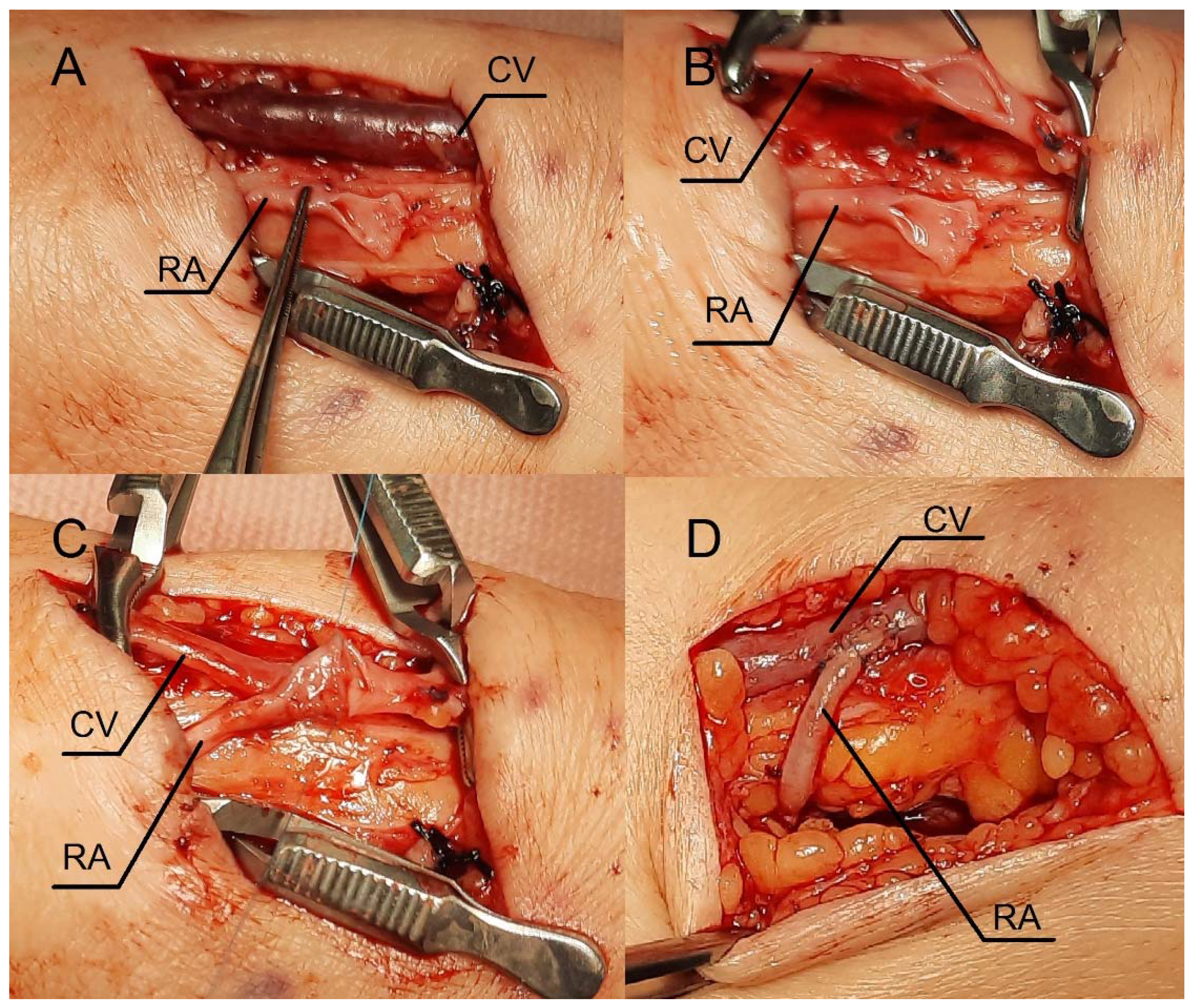
A 38-year-old female with chronic glomerulonephritis (focal segmental glomerulosclerosis), undergoing hemodialysis for 16 months, was admitted to our department due to a catheter-related infection. The patient was given standard care, consisting of an antibiotic based on the blood culture and an antibiotic lock to fill the catheter lumens. The catheter was maintained in place due to the patient's prompt clinical recovery and the lack of a tunnel infection signs. Eight months prior to admission, she had a distal radial-cephalic fistula (RCAVF) i.e., the anastomosis between the site of radial artery (RA) and the end of the cephalic vein (CV) (
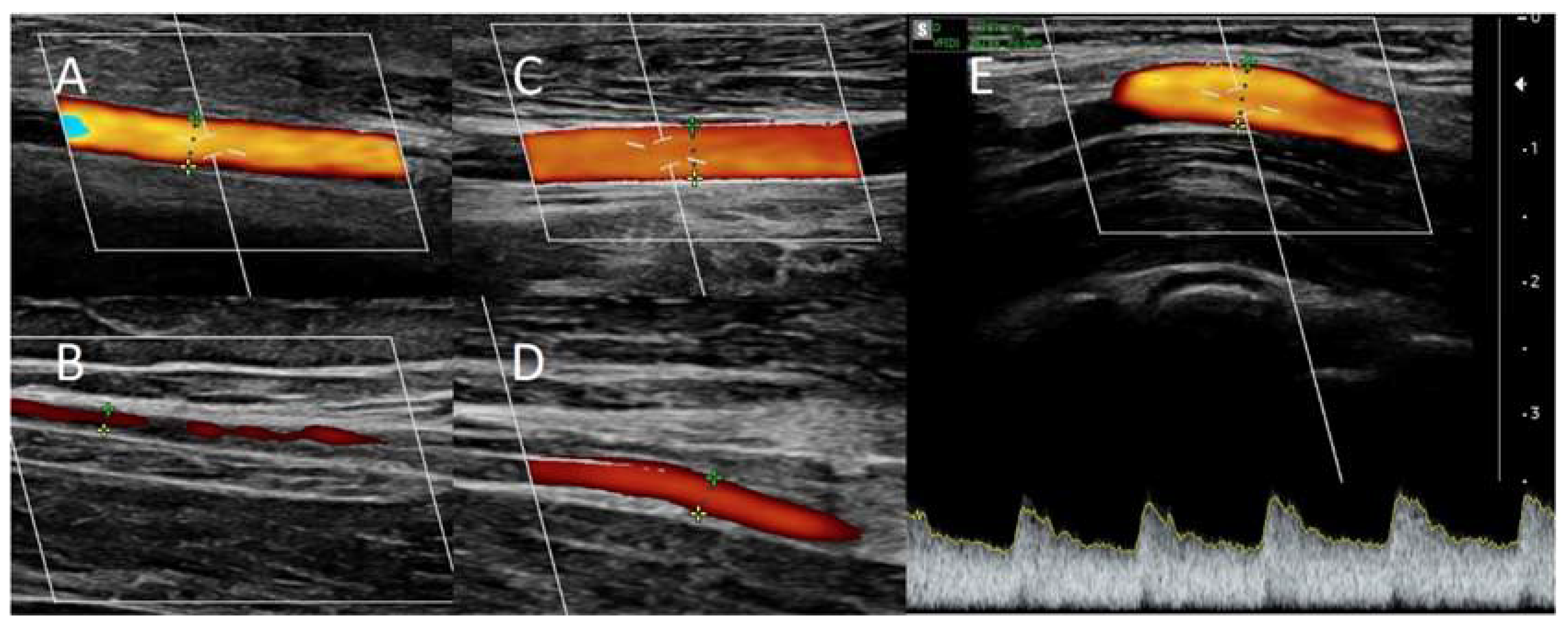
Figure 2A). Ultrasound examination revealed a brachial artery flow of 264 ml/min and vein diameters of 5.8 mm and 5 mm in the mid-forearm and elbow fossa, respectively. The dominant vessel supplying the fistula was the ulnar artery (UA), which was 4 mm in diameter and supplied the fistula via the palmar arches (
Figure 3A). The blood flow rate through the UA was 234 ml/min. Although the RA was patent, it only had a 1.3 mm cross-sectional diameter (
Figure 3B). Prior to admission, many failed attempts were undertaken to cannulate the AVF. However, the blood supply was insufficient to allow effective dialysis. Considering that the primary cause of delayed maturation was the stenosis of the radial artery in the proximal portion of the anastomosis (red point X in
Figure 1), it was decided to enhance the blood supply to the CV using the RADAR technique.
2.2. Procedure description in Case 1.
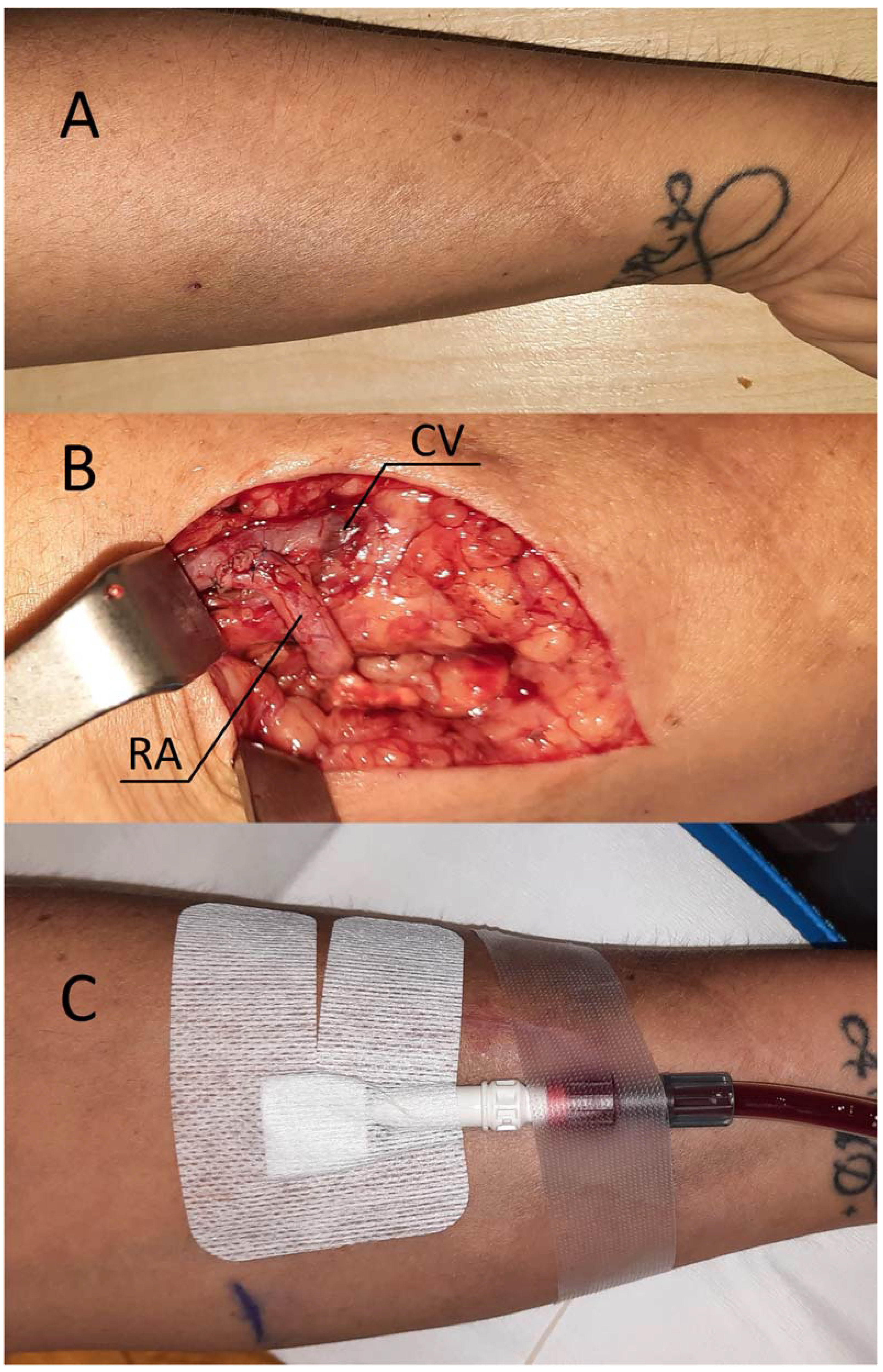
Local anesthesia consisting of 1% lignocaine solution was used during the procedure. An oblique incision was made in the distal part of the forearm, approximately 2 to 3 cm proximal to the primary fistula (
Figure 2B). The appropriate vessel fragments were dissected. Over the ligature, the radial artery was severed, and the blood supply was verified by momentarily releasing the clamp. The perceived blood flow was satisfactory. The cephalic vein was then clamped both distally and proximally and finally, and it was subsequently incised longitudinally. Both vessels were sutured with a continuous suture, i.e., the end of the artery was anastomosed with the side of the vein using an insoluble polypropylene vascular suture of 6-0 (
Figure 2B). During the procedure, the operator used a magnifying glass with 2.5 times magnification. We present the patients in whom option I of anastomosis (
Figure 1) was performed; however, option II was carried out in two additional cases. The vein filled with blood when the clamps were removed, and a typical murmur was noticed (
Figure 2B). The wound was closed using skin sutures. Ultrasound examination confirmed that the fistula was patent the day following the procedure. UA and RA diameter was 4 mm and 2 mm, respectively (
Figure 3C,D). The blood flow rate through the UA was 193 ml/min (
Figure 3C), while the brachial blood flow rate was 482 ml/min (
Figure 3E). The patient was discharged with a fistula that was functional. At the 3-week postoperative follow-up appointment, the fistula remained patent, and the first successful cannulation was performed 4 weeks after surgery (
Figure 1C).
2.3. Description of Case 2.
A 75-year-old woman with type 2 diabetes presented to our Clinic due to the progression of CKD. In a laboratory, serum creatinine (sCr) was found to be 4mg/dl, urea 156mg/dl, and potassium 4.5mmol/l. The estimated glomerular filtration rate (eGFR) was 16ml/min/1.73m2. She had distal radial-cephalic arteriovenous fistula (RCAVF) created six months before admission. Ultrasound examination revealed that fistula flow was 170ml/min whereas the diameter of the cephalic vein at the elbow crest and in the middle of the forearm were 5mm and 4.5mm, respectively. The radial and ulnar arteries were 1.9mm and 2.4mm in diameter, respectively. Both vessels exhibited focal atherosclerotic calcifications. In addition, in the distal section of the forearm we discovered a significant narrowing of RA, accompanied by an acceleration of the wave speed in Doppler, which, as we speculated, was the cause of the fistula maturation failure. Because the cephalic vein was patent, we planned to create a new fistula using RADAR technique to improve the blood flow through the AVF.
2.4. Procedure description in Case 2.
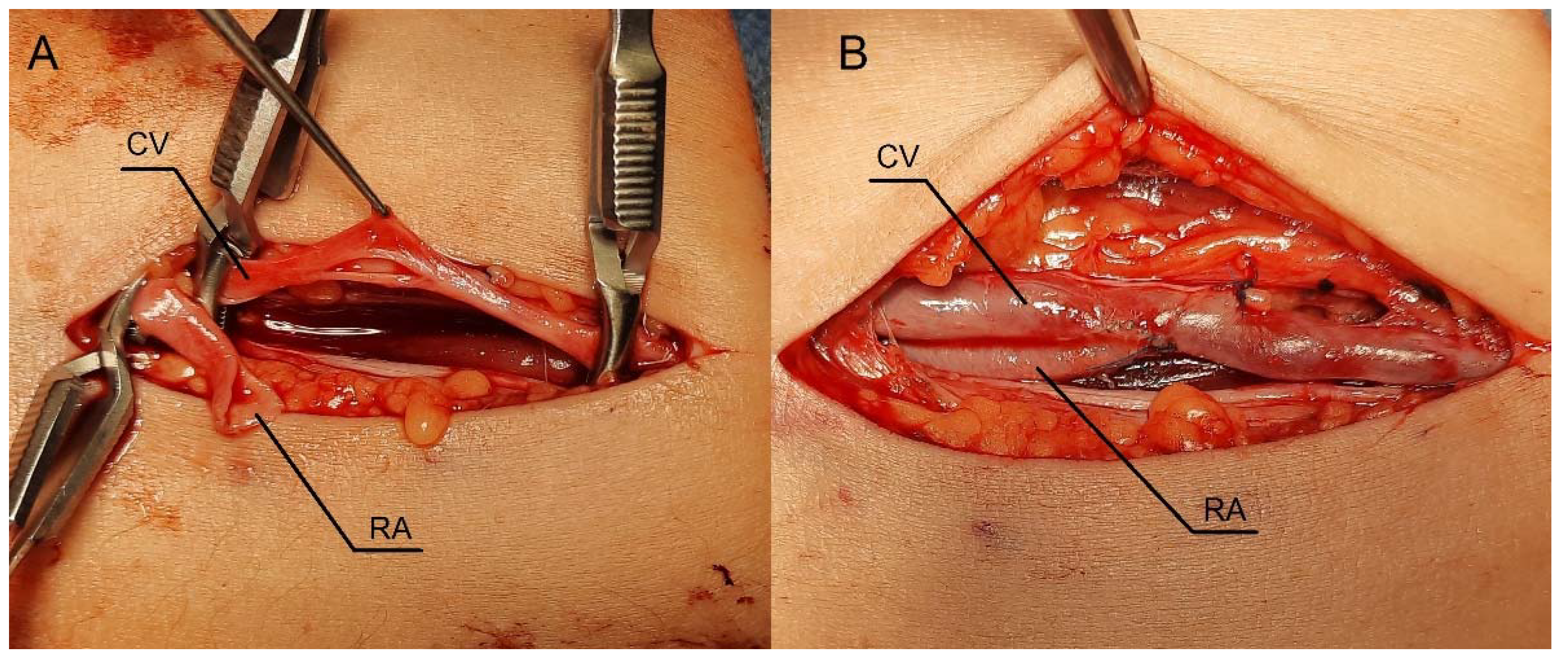
1% lignocaine was used for local anesthesia during the surgery. An oblique incision was made in the middle part of the forearm to dissect the vessels (
Figure 4A). It was a location where the radial artery appeared optimal for creating a fistula, as the Doppler ultrasound revealed a vessel fragment preceding the artery stenosis. RA was clamped and severed over ligature. (Future 4A) The vein was then longitudinally cut (
Figure 4B), and the artery was transferred to the vein (
Figure 4C). Anastomosis was carried out with continuous stitching using insoluble polypropylene vascular suture of 6-0. (
Figure 4C). The weak thrill was felt immediately after the clamps were released. The ultrasound was carried out the following day. The flow rate of the fistula was 234ml/min. Since the fistula blood flow was not satisfactory, we scheduled next procedure three weeks later. The patient was readmitted to Clinic once more time. In ultrasound we identified additional stenosis in the RA near the last anastomosis. The second surgery was performed in a similar fashion, but the incision site was located 2-3 cm proximal to the previous procedure.
Figure 4D shows the fistula created with RADAR technique with significant thrill. Ultrasound examination reveals that fistula function has improved. The following day, the fistula flow rate was 376 ml/min. The vein in the elbow crest increases to 6.9mm in diameter. Two weeks after the procedure, at the outpatient clinic follow-up visit, the fistula was still patent, however there were no clinical or laboratory indication to initiate dialysis. The renal function of the patient and the AVF function is still being observed.
2.5. Description of Case 3.
47-year-old female with chronic kidney disease due to systemic lupus erythematosus and antiphospholipid syndrome on hemodialysis for 10 years. Nine years ago, she suffered an ischemic stroke. The left brachiocephalic fistula was used for hemodialysis and required ligation 10 months ago due to skin maceration posing a risk of rupture. At that time, a permanent catheter was implanted. She was admitted to our Clinic to create a new AVF. Due to favorable anatomical conditions, it was decided to create a primary snuff-box fistula on the right side. However, because of the low fistula flow, RCAVF was carried out on the wrist. Unfortunately, a thrombus developed in the middle third of the RA during the postoperative time. In consequence, the fistula flow rate during follow-up visits does not exceed 250 ml/min. Considering that the cephalic vein was patent, we decided to create a fistula using the RADAR technique proximal to the RA stenosis.
2.6. Procedure description in Case 3.
As in previous cases, the surgical site was determined by the results of the ultrasound examination. In the present case, the patent artery was found in the third proximal of the forearm. (
Figure 4A). The procedure was carried out as described above. In this case, however, the vein and artery are in close proximity to one another. After performing an anastomosis and releasing the clamps, a blood flow was detected in the vessel (
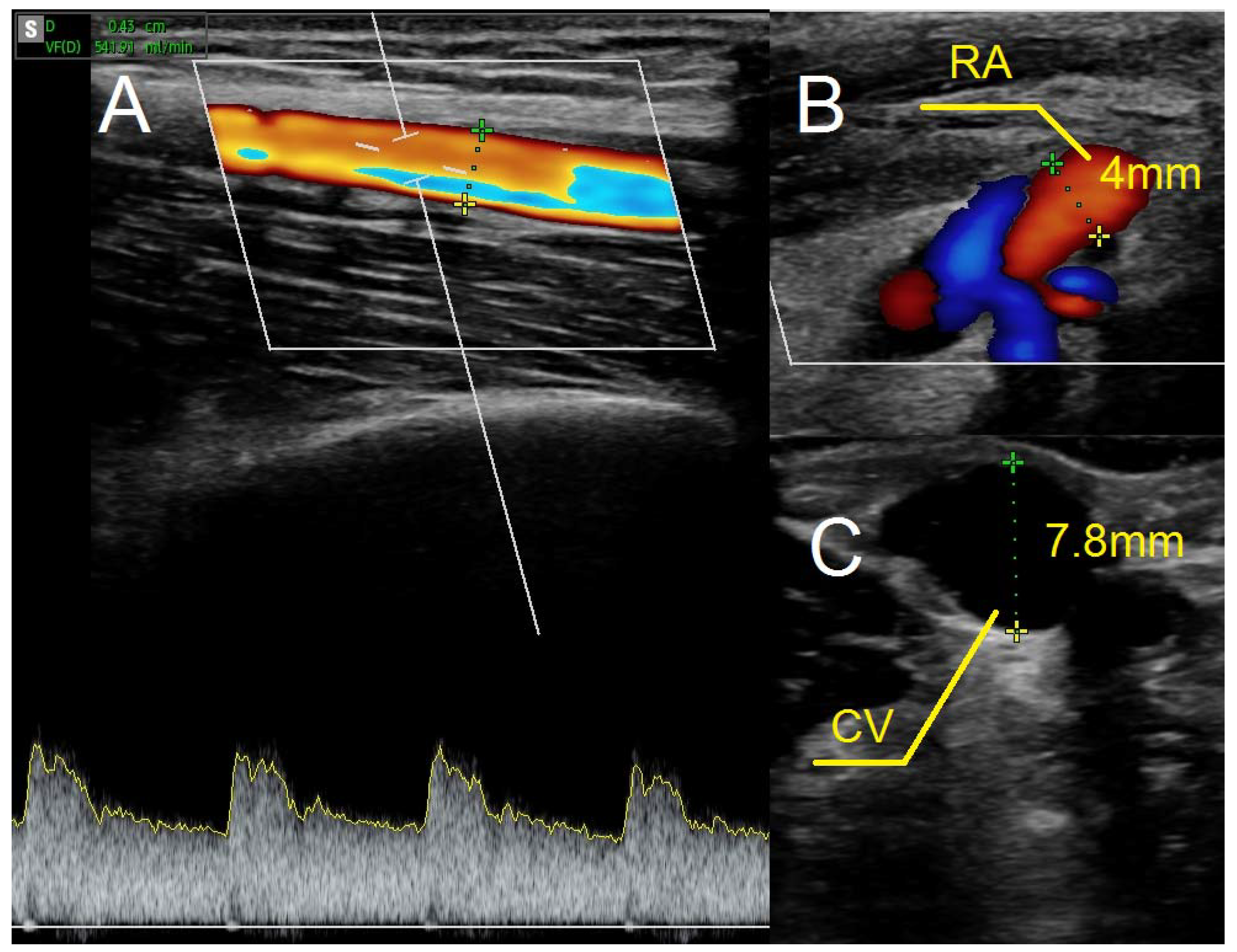
Figure 4B). The following day's ultrasound examination of the fistula revealed a flow rate of 541ml/min. (
Figure 5A) The diameter of the radial artery (
Figure 5B) and the cephalic vein (
Figure 5C) also increased to 4mm and 7.8mm, respectively. One month later, the fistula was successfully cannulated.
3. Resultes.
In each case, the parameters characterizing the fistula's function were improved. (
Table 1). Option I of RADAR technique was selected in case 1, whereas option II was used in cases 2 and 3. In two patients, the arteriovenous fistula (AVF) can be utilized shortly after surgery. In one patient (case 2), residual renal function was sufficient to maintain the patient in predialysis. There were no laboratory and clinical indications to initiate dialysis treatment. In this case, two RADAR interventions were required to achieve satisfactory AVF function. No acute complications occurred immediately after the surgery.
4. Discussion
In this study, we described a group of patients with delayed fistula maturation due to radial artery stenosis. In three patients, three different causes of radial artery (RA) stenosis were found. RA stenosis was associated with following causes: anastomosis suturing error by primary arteriovenous fistula in case 1, severe atherosclerosis in case 2, and RA thrombosis in an active lupus patient as a consequence of antiphospholipid syndrome in case 3. We adapted a radial artery deviation and reimplantation (RADAR) technique for this specific indication and found that all our patients' AVFs function improved. To our knowledge, this is the first report of this type of solution.
Failure of AVF maturation is the main barrier to establishing functional arteriovenous fistulas. RADAR is a new concept in AVF creation. Encouraging results reported by Sadaghianloo et al. with high patency rates make this approach interesting.[
6] However, RA ligation has been criticized by a number of authors, who point out serious drawbacks, such as an increased risk of hand ischemia and potential complications during fistula salvage, in cases of AVF thrombosis, in which emboli propagate into the artery.[
7] Classical native AVF, i.e. an extended dissection and mobilization of the cephalic vein (CV), allowing the vein to be brought toward the radial artery for an end-to-side anastomosis, according to Röhl et al. may fail due to technical errors in suturing the vessels, particularly in the case of small vessel sizes.[
4] According to our observations, arterial stenosis during arterial suturing often occurs in the proximal portion of the anastomosis (red point X in
Figure 1), which is a narrow segment of the artery and therefore susceptible to this type of technical error. At the same time, this stenosis or closure is critical for fistula function since blood flow from the ulnar artery (UA) via the palmar arches is often inadequate for fistula maturation. In such situations, the maturation period is typically long, and the fistula's blood flow does not exceed 300 ml/min. In these circumstances, blood flow is reduced in RA, and over time, degenerative changes develop as intimal hyperplasia. Due to the alterations in RA, the repair of such a dysfunctional AVF may provide some difficulties. Our new strategy is to use the RADAR technique as a secondary fistula, which has the following advantages:
1. The primary fistula is not ligated and the blood flow from the ulnar artery is maintained.
2. By connecting the end of the radial artery to the side of the vein, the blood supply to the cephalic vein is increased, thereby accelerating its maturation. In other words, the additional volume of flow from the RA enhances the total fistula blood flow as measured in the brachial artery.
3. Increased radial blood flow protects against the development of degenerative changes; consequently, a third fistula can be created proximally between the RA and the CV in cases of AVF thrombosis.
4. The risk of hand ischemia is theoretically reduced as both the UA and the large portion of the RA are patent. The occluded distal part RA is bridged by the distal CV (Figure 1). The only limitation is the venous valves, which may impede retrograde flow through the CV. However, this risk is minimal when the venous bridge is not long.
5. We have reported RA stenosis due to three possible causes of low fistula flow and maturation failure, but this approach can be used for any type of RA stenosis, including changes after the artery has been used as a vascular access in intensive care unit or cardiology procedures. In each of these circumstances, RADAR procedure may be considered.
6. We believe this technique allows clinicians to avoid upper fistulas involving the brachial artery and graft-based fistulas.
It should be emphasized that one possible disadvantage of this solution is venous hand congestion; however, neither our patients nor the group of RADAR patients in the study by Sadaghianloo et al noticed this complication. [
6]
5. Conclusions
The RADAR fistula may be successfully used as a secondary access in patients with maturation failure, due to RA stenosis to accelerate fistula maturation. This tailored strategy should be evaluated in prospective studies.
Author Contributions
Conceptualization, T.G., M.Ku. and K.L.; methodology, T.G. and M.Ku.; formal analysis, T.G. and A.K.; investigation, T.G. and K.L.; data curation, T.G.; writing—original draft preparation, T.G., A.K. and M.G.; writing—review and editing, A.K. and M.Ku.; visualization, T.G.; supervision, M.Ku., D.J. and M.Kr.; project administration, T.G.
Funding
The study is supported by the Wroclaw Medical University statutory funds (SUB.C160.23.046). It was investigator-initiated research. The funding body had no role in the study design, data collection, analyses, and interpretation, or in writing the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee at Wroclaw Medical University KB-607/2019.
Informed Consent Statement
The study was carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patients to publish the results obtained during the treatment.
Data Availability Statement
The data presented in this study are available in this article.
Acknowledgments
We would like to thank Mrs. Monika Mrozek for preparing the artwork.
Conflicts of Interest
The authors declare no conflict of interest.
References
- United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, , 2022.
- Gołębiowski, T.; Weyde, W.; Kusztal, M.; Porażko, T.; Augustyniak-Bartosik, H.; Madziarska, K.; Krajewska, M.; Koniński, P.; Sydor, A.; Letachowicz, K., et al. [Vascular access in diabetic patients. Are these patients "difficult"?]. Postepy Hig Med Dosw (Online) 2015, 69, 913-917. [CrossRef]
- Rothuizen, T.C.; Wong, C.; Quax, P.H.; van Zonneveld, A.J.; Rabelink, T.J.; Rotmans, J.I. Arteriovenous access failure: more than just intimal hyperplasia? Nephrol Dial Transplant 2013, 28, 1085-1092. [CrossRef]
- Röhl, L.; Franz, H.E.; Möhring, K.; Ritz, E.; Schüler, H.W.; Uhse, H.G.; Ziegler, M. Direct arteriovenous fistula for hemodialysis. Scand J Urol Nephrol 1968, 2, 191-195. [CrossRef]
- Tordoir, J.H.M.; Zonnebeld, N.; van Loon, M.M.; Gallieni, M.; Hollenbeck, M. Surgical and Endovascular Intervention for Dialysis Access Maturation Failure During and After Arteriovenous Fistula Surgery: Review of the Evidence. Eur J Vasc Endovasc Surg 2018, 55, 240-248. [CrossRef]
- Sadaghianloo, N.; Declemy, S.; Jean-Baptiste, E.; Haudebourg, P.; Robino, C.; Islam, M.S.; Hassen-Khodja, R.; Dardik, A. Radial artery deviation and reimplantation inhibits venous juxta-anastomotic stenosis and increases primary patency of radial-cephalic fistulas for hemodialysis. J Vasc Surg 2016, 64, 698-706.e691. [CrossRef]
- Jennings, W.C.; Glazer, S.M. Regarding "Radial artery deviation and reimplantation inhibits venous juxta-anastomotic stenosis and increases primary patency of radial-cephalic fistulas for hemodialysis". J Vasc Surg 2017, 65, 933-934. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).