Submitted:
02 September 2023
Posted:
05 September 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Epidemiology
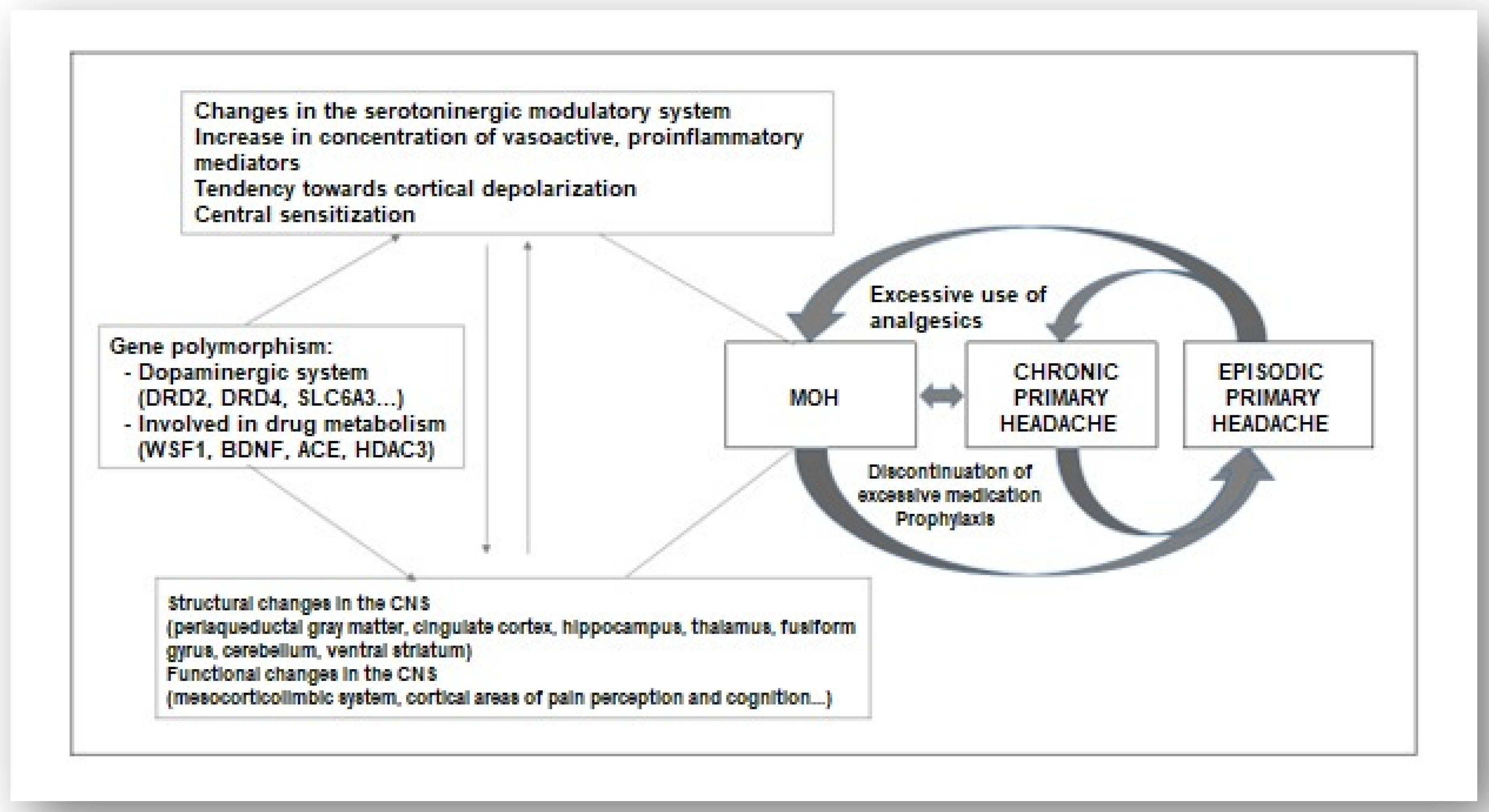
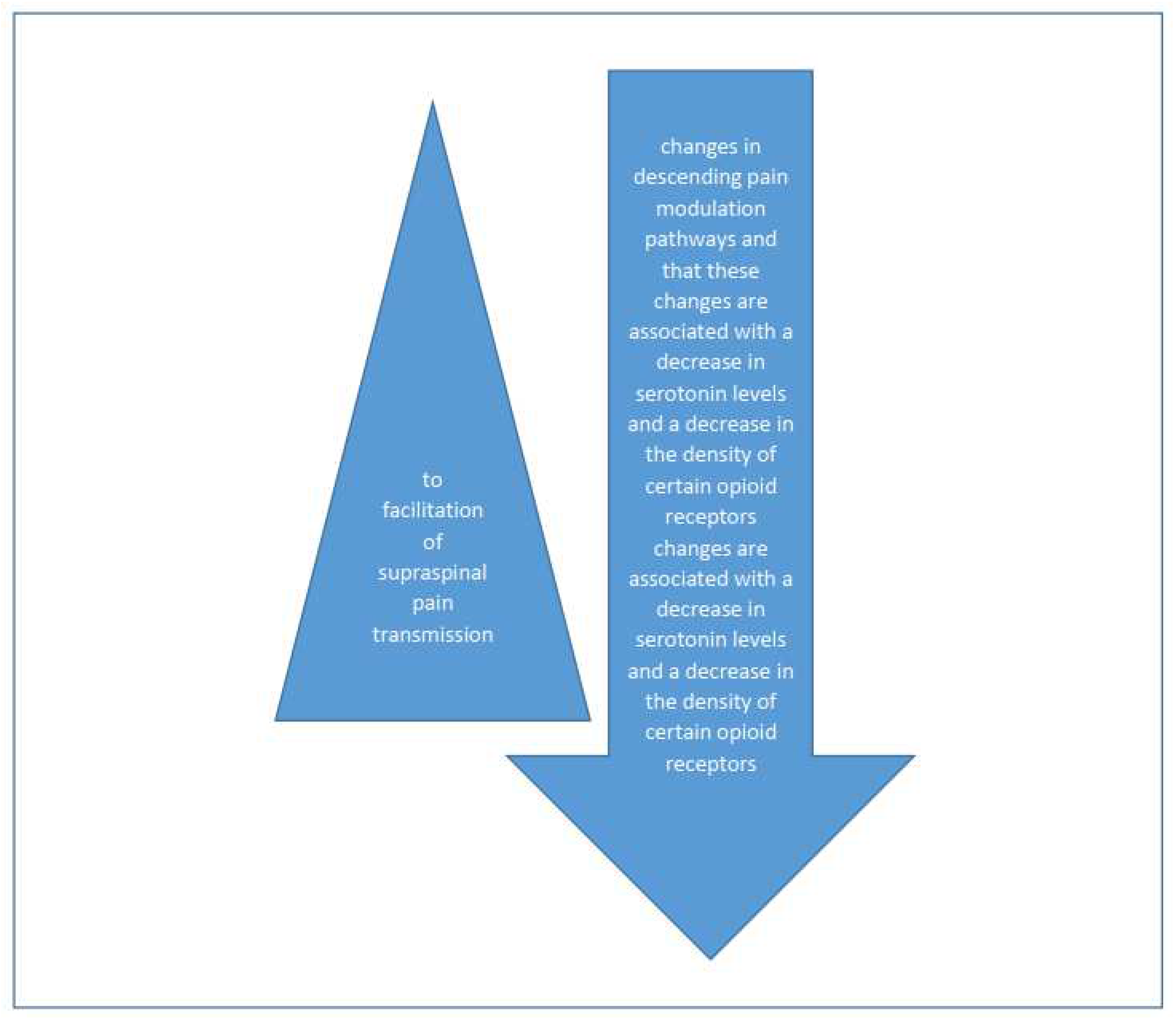
Pathophysiology
Risk Factors
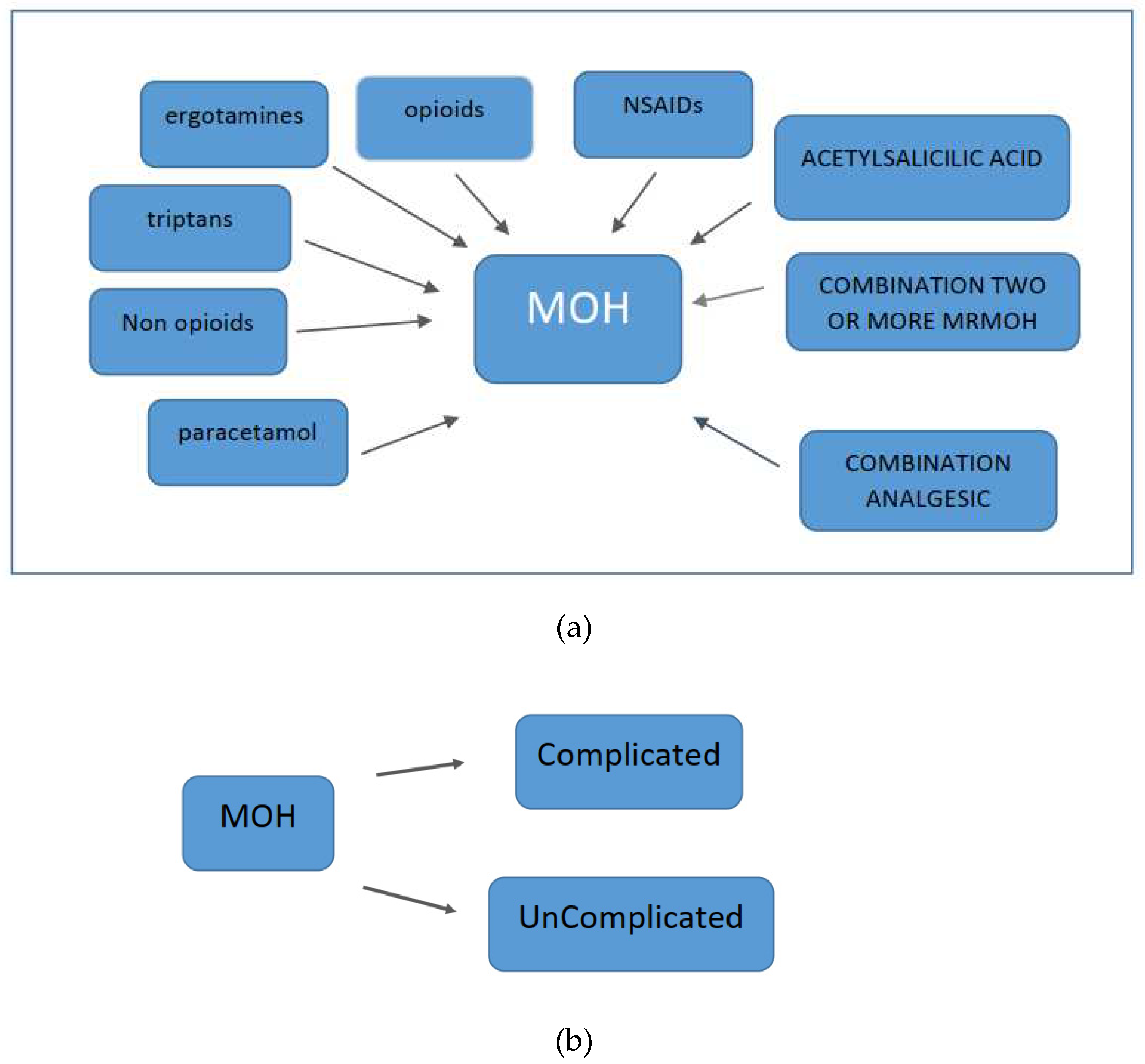
Type of excessively used therapy
Impact of medication overuse headache (MOH)
Comorbidities
Diagnosis
Headache of excessive use of ergotamine
Headache of excessive use of triptans
Headache due to overuse of opioids
Headache due to overuse ofcombined analgetics
Medication overuse headache attributed to multiple classes of drugs, rather than individual overuse
Medication overuse headache attributed to unverified overuse of various classes of drugs
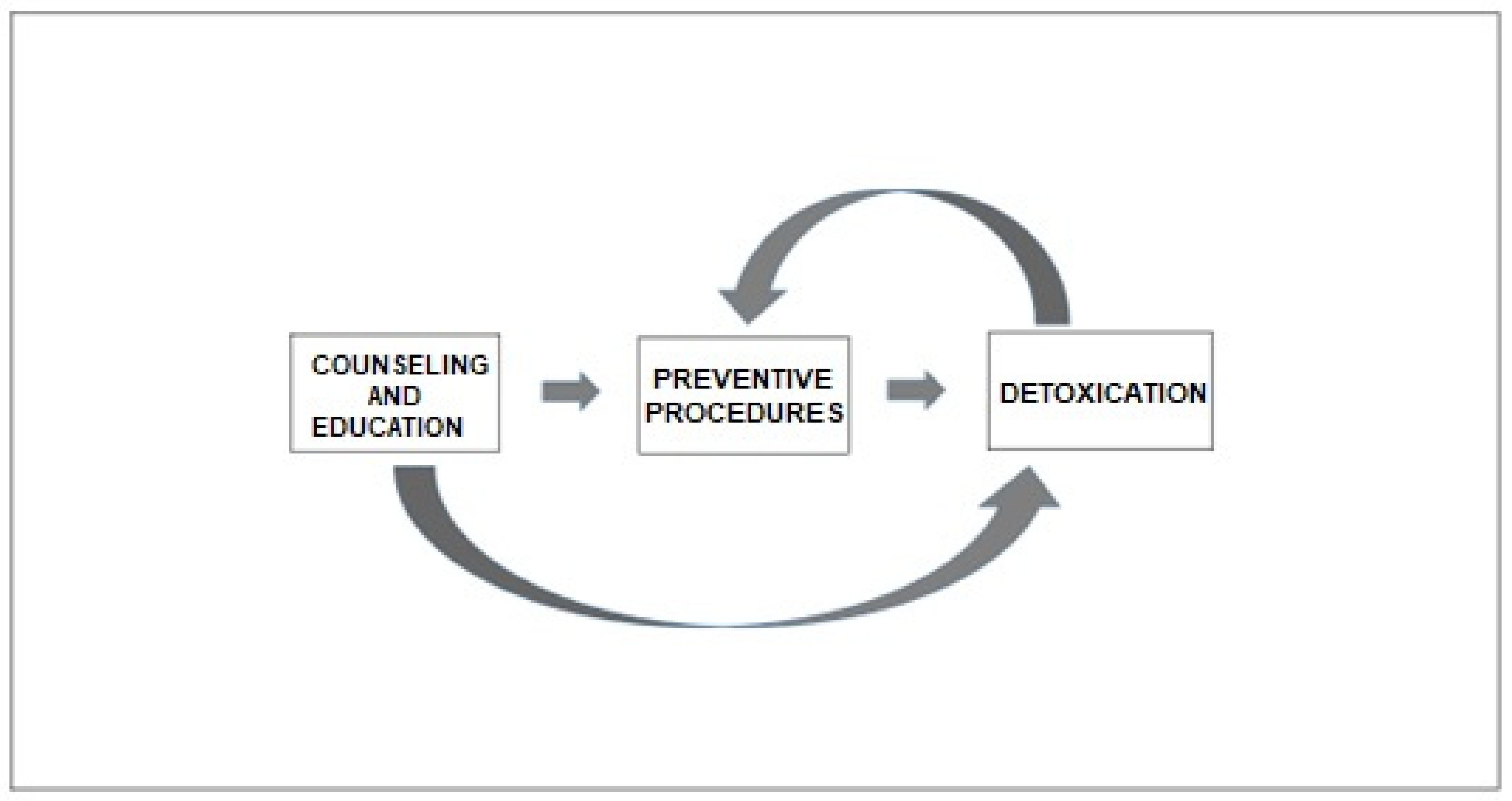
Therapy
Bridging therapy
Discontinuation of medications overused medications and preventive therapy
The treatment of medication overuse
Patient education and multidisciplinary care
Clinical monitoring and prognosis
Personal research
Conclusions
Conflicts of Interest
Abbreviations
| cAMP | cyclic adenosine monophosphate |
| CDS | color Doppler sonography |
| cGMP | cyclic guanosine monophosphate |
| CGRP | calcitonin gene-related peptide |
| CO | carbon monoxide |
| COX-2 | cyclooxygenase-2 |
| CRP | C-reactive protein |
| MOH | medication overuse headache |
| GTN | glyceryltrinitrate |
| GTT | tension-type headache |
| HIT | headache impact test |
| MIDAS | migraine disability assessment score |
| ICHD | international classification of headache disorders |
| MR | magnetic resonance |
| MRA | magnetic resonance angiography |
| MRV | magnetic resonance venography |
| MSG | monosodium glutamate |
| NO | nitric oxide |
| NSAIDs | nonsteroidal anti-inflammatory drugs |
| PACAP | Pituitary AdenylateCyclase-Activating Polypeptide |
| PDE | phosphodiesterase |
| ESR | erythrocyte sedimentation rateSUNA – short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms |
| SUNCT | eng.short-lasting unilateral neuralgiform headache with conjunctival injection and tearing |
| TAG | Trigeminal Autonomic Headache and Trigeminal Neuralgia |
Clinical Implications
References
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259.
- World Health Organization, Lifting The Burden. Atlas of headache disorders and resources in the world. WHO, Geneva: 2011.
- Saylor, D. , and Steiner, TJ. The Global Burden of Headache. Semin Neurol 2018, 38, 182–190. [Google Scholar] [PubMed]
- Kristoffersen, E.S.; Lundqvist, C. Medication-overuse headache: epidemiology, diagnosis and treatment. Ther. Adv. Drug Saf. 2014, 5, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [CrossRef] [PubMed]
- Bigal, ME. , and Lipton, RB. Migraine chronification. Curr Neurol Neurosci Rep. 2011;11:139–148. Curr Neurol Neurosci Rep. 2011, 11, 139–148. [Google Scholar] [CrossRef]
- Vandenbussche, N.; Paemeleire, K.; Katsarava, Z. The Many Faces of Medication-Overuse Headache in Clinical Practice. Headache: J. Head Face Pain 2020, 60, 1021–1036. [Google Scholar] [CrossRef]
- Diener, HC. , Antonaci, F., Braschinsky, M., et al.. European Academy of Neurology guideline on the management of medication-overuse headache. Eur J Neurol. 2020. [Google Scholar] [CrossRef]
- Jonsson, P.; Jakobsson, A.; Hensing, G.; Linde, M.; Moore, C.D.; Hedenrud, T. Holding on to the indispensable medication –A grounded theory on medication use from the perspective of persons with medication overuse headache. J. Headache Pain 2013, 14, 43–43. [Google Scholar] [CrossRef]
- Westergaard, M.L.; Munksgaard, S.B.; Bendtsen, L.; Jensen, R.H. Medication-overuse headache: a perspective review. Ther. Adv. Drug Saf. 2016, 7, 147–158. [Google Scholar] [CrossRef]
- Vandenbussche,,N., Laterza, D., Lisicki, M., et al. Medication-overuse headache: A widely recognized entity amidst ongoing debate. J Headache Pain 2018, 19, 50. [CrossRef]
- Diener, H.-C.; Dodick, D.; Evers, S.; Holle, D.; Jensen, R.H.; Lipton, R.B.; Porreca, F.; Silberstein, S.; Schwedt, T. Pathophysiology, prevention, and treatment of medication overuse headache. Lancet Neurol. 2019, 18, 891–902. [Google Scholar] [CrossRef] [PubMed]
- Hershey, A.D.; Burdine, D.; A Kabbouche, M.; Powers, S.W. Genomic expression patterns in medication overuse headaches. Cephalalgia 2010, 31, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Schwedt, T.J.; Chong, C.D. Medication Overuse Headache: Pathophysiological Insights from Structural and Functional Brain MRI Research. Headache: J. Head Face Pain 2017, 57, 1173–1178. [Google Scholar] [CrossRef]
- Srikiatkhachorn, A.; le Grand, S.M.; Supornsilpchai, W.; Storer, R.J. Pathophysiology of Medication Overuse Headache-An Update. Headache: J. Head Face Pain 2013, 54, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Supornsilpchai, W.; le Grand, S.M.; Srikiatkhachorn, A. Cortical hyperexcitability and mechanism of medication-overuse headache. Cephalalgia 2010, 30, 1101–1109. [Google Scholar] [CrossRef]
- Bongsebandhu-Phubhakdi, S.; Srikiatkhachorn, A. Pathophysiology of Medication-overuse Headache: Implications from Animal Studies. Curr. Pain Headache Rep. 2011, 16, 110–115. [Google Scholar] [CrossRef]
- Green, A.L.; Gu, P.; De Felice, M.; Dodick, D.; Ossipov, M.H.; Porreca, F. Increased susceptibility to cortical spreading depression in an animal model of medication-overuse headache. Cephalalgia 2013, 34, 594–604. [Google Scholar] [CrossRef]
- Belanger, S.; Ma, W.; Chabot, J.-G.; Quirion, R. Expression of calcitonin gene-related peptide, substance P and protein kinase C in cultured dorsal root ganglion neurons following chronic exposure to mu, delta and kappa opiates. Neuroscience 2002, 115, 441–453. [Google Scholar] [CrossRef]
- De Felice, M.; Ossipov, M.H.; Wang, R.; Dussor, G.; Lai, J.; Meng, I.D.; Chichorro, J.; Andrews, J.S.; Rakhit, S.; Maddaford, S.; et al. Triptan-induced enhancement of neuronal nitric oxide synthase in trigeminal ganglion dural afferents underlies increased responsiveness to potential migraine triggers. Brain 2010, 133, 2475–2488. [Google Scholar] [CrossRef]
- Okada-Ogawa, A. , Porreca, F., Meng,ID.. Sustained morphine-induced sensitization and loss of diffuse noxious inhibitory controls (DNIC) in durasensitive medullary dorsal horn neurons. J Neurosci 2009, 29, 15828–15835. [Google Scholar] [CrossRef]
- Wanasuntronwong, A.; Jansri, U.; Srikiatkhachorn, A. Neural hyperactivity in the amygdala induced by chronic treatment of rats with analgesics may elucidate the mechanisms underlying psychiatric comorbidities associated with medication-overuse headache. BMC Neurosci. 2017, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Srikiatkhachorn, A.; Tarasub, N.; Govitrapong, P. Effect of chronic analgesic exposure on the central serotonin system: a possible mechanism of analgesic abuse headache. Headache: J. Head Face Pain 2000, 40, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Tohyama, Y.; Yamane, F.; Merid, M.F.; Diksic, M. Effects of selective 5-HT1A receptor antagonists on regional serotonin synthesis in the rat brain: An autoradiographic study with α-[14C]methyl-l-tryptophan. Eur. Neuropsychopharmacol. 2001, 11, 193–202. [Google Scholar] [CrossRef]
- Dobson, C.; Tohyama, Y.; Diksic, M.; Hamel, E. Effects of Acute or Chronic Administration of Anti-Migraine Drugs Sumatriptan and Zolmitriptan on Serotonin Synthesis in the Rat Brain. Cephalalgia 2004, 24, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Srikiatkhachorn, A.; Anthony, M. Platelet Serotonin in Patients with Analgesic-Induced Headache. Cephalalgia 1996, 16, 423–426. [Google Scholar] [CrossRef]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Coppola, G.; Currà, A.; Di Lorenzo, C.; Parisi, V.; Gorini, M.; Sava, S.L.; Schoenen, J.; Pierelli, F. Abnormal cortical responses to somatosensory stimulation in medication-overuse headache. BMC Neurol. 2010, 10, 126–126. [Google Scholar] [CrossRef]
- Currà, A.; Coppola, G.; Gorini, M.; Porretta, E.; Bracaglia, M.; Di Lorenzo, C.; Schoenen, J.; Pierelli, F. Drug-induced changes in cortical inhibition in medication overuse headache. Cephalalgia 2011, 31, 1282–1290. [Google Scholar] [CrossRef]
- Munksgaard, S.B.; Bendtsen, L.; Jensen, R.H. Modulation of central sensitisation by detoxification in MOH: Results of a 12-month detoxification study. Cephalalgia 2013, 33, 444–453. [Google Scholar] [CrossRef]
- Riederer, F.; Marti, M.; Luechinger, R.; Lanzenberger, R.; von Meyenburg, J.; Gantenbein, A.R.; Pirrotta, R.; Gaul, C.; Kollias, S.; Sándor, P.S. Grey matter changes associated with medication-overuse headache: Correlations with disease related disability and anxiety. World J. Biol. Psychiatry 2012, 13, 517–525. [Google Scholar] [CrossRef]
- Michels, L.; Christidi, F.; Steiger, V.R.; Sándor, P.S.; Gantenbein, A.R.; Landmann, G.; Schreglmann, S.R.; Kollias, S.; Riederer, F. Pain modulation is affected differently in medication-overuse headache and chronic myofascial pain – A multimodal MRI study. Cephalalgia 2016, 37, 764–779. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Wilcke, T.; Leinisch, E.; Straube, A.; Kämpfe, N.; Draganski, B.; Diener, H.C.; Bogdahn, U.; May, A. Gray matter decrease in patients with chronic tension type headache. Neurology 2005, 65, 1483–1486. [Google Scholar] [CrossRef] [PubMed]
- Chanraud, S. , Di Scala, G., Dilharreguy, B., et al.. Brain functional connectivity and morphology changes in medication-overuse headache: clue for dependence-related processes? Cephalalgia 2014, 34, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, S.; Grazzi, L.; Muffatti, R.; Nava, S.; Ghielmetti, F.; Bertolino, N.; Mandelli, M.L.; Visintin, E.; Bruzzone, M.G.; Nigri, A.; et al. In Medication-Overuse Headache, fMRI Shows Long-Lasting Dysfunction in Midbrain Areas. Headache: J. Head Face Pain 2012, 52, 1520–1534. [Google Scholar] [CrossRef]
- Torta, D.; Costa, T.; Luda, E.; Barisone, M.; Palmisano, P.; Duca, S.; Geminiani, G.; Cauda, F. Nucleus accumbens functional connectivity discriminates medication-overuse headache. NeuroImage: Clin. 2016, 11, 686–693. [Google Scholar] [CrossRef]
- Fumal, A.; Laureys, S.; Di Clemente, L.; Boly, M.; Bohotin, V.; Vandenheede, M.; Coppola, G.; Salmon, E.; Kupers, R.; Schoenen, J. Orbitofrontal cortex involvement in chronic analgesic-overuse headache evolving from episodic migraine. Brain 2005, 129, 543–550. [Google Scholar] [CrossRef]
- Riederer, F. , Gantenbein, AR., Marti, M., et al.. Decrease of gray matter volume in the midbrain is associated with treatment response in medication-o,veruse headache: possible influence of orbitofrontal cortex. J Neurosci 2013, 33, 15343–15349. [Google Scholar] [CrossRef]
- Thorlund, K.; Sun-Edelstein, C.; Druyts, E.; Kanters, S.; Ebrahim, S.; Bhambri, R.; Ramos, E.; Mills, E.J.; Lanteri-Minet, M.; Tepper, S. Risk of medication overuse headache across classes of treatments for acute migraine. J. Headache Pain 2016, 17, 1–9. [Google Scholar] [CrossRef]
- Bigal, M.E.; Serrano, D.; Buse, D.; Scher, A.; Stewart, W.F.; Lipton, R.B. Acute Migraine Medications and Evolution From Episodic to Chronic Migraine: A Longitudinal Population-Based Study. Headache: J. Head Face Pain 2008, 48, 1157–1168. [Google Scholar] [CrossRef]
- Wilkinson, S.; Becker, W.; Heine, J. Opiate Use to Control Bowel Motility May Induce Chronic Daily Headache in Patients With Migraine. Headache: J. Head Face Pain 2001, 41, 303–309. [Google Scholar] [CrossRef]
- Bahra, A. , Walsh, M., Menon, S., et al. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache 2003, 43, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Hagen, K. , Albretsen, C., Vilming, ST., et al.. A 4-year follow-up of patients with medication-overuse headache previously included in a randomized multicenter study. J Headache Pain 2011, 12, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Cevoli, S.; Sancisi, E.; Grimaldi, D.; Pierangeli, G.; Zanigni, S.; Nicodemo, M.; Cortelli, P.; Montagna, P. Family History for Chronic Headache and Drug Overuse as a Risk Factor for Headache Chronification. Headache: J. Head Face Pain 2009, 49, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Limmroth, V. , Katsarava, Z., Fritsche, G., et al.. Features of m;edication overuse headache following overuse of different acute headache drugs. Neurology 2002, 59, 1011–1014. [Google Scholar] [CrossRef]
- Starling, AJ. , Hoffman-Snyder, C., Halker, RB., et al. Risk of development of medication overuse headache with nonsteroidal anti- inflammatory drug therapy for migraine: A critically appraised topic. Neurologist 2011, 17, 297–299. [Google Scholar] [CrossRef]
- Diener, H.-C.; Limmroth, V. Medication-overuse headache: a worldwide problem. Lancet Neurol. 2004, 3, 475–483. [Google Scholar] [CrossRef]
- Ashina, S.; Serrano, D.; Lipton, R.B.; Maizels, M.; Manack, A.N.; Turkel, C.C.; Reed, M.L.; Buse, D.C. Depression and risk of transformation of episodic to chronic migraine. J. Headache Pain 2012, 13, 615–624. [Google Scholar] [CrossRef]
- Migliore, S.; Paolucci, M.; Quintiliani, L.; Altamura, C.; D’aurizio, G.; Curcio, G.; Vernieri, F. Psychopathological profile of medication overuse headache patients, drug assumption and degree of disability. Neurol. Sci. 2018, 39, 169–170. [Google Scholar] [CrossRef]
- Ljubisavljevic, M. (2020). Ruminativni stil mišljenja, depresivnost, anksioznost, stres i kvalitet života kod pacijenata sa glavoboljom prekomerne upotrebe medikamenata. Master degree. 2020; Faculty for Phylosophy Nis.
- Ljubisavljevic, M.; Ignjatovic, A.; Djordjevic, V.; Pesic, M.H.; Ljubisavljevic, S. Depression, Anxiety, Stress, and Health-Related Quality of Life Among Patients With Medication Overuse Headache in a Tertiary Headache Center: A Cross-Sectional Study. J. Neuropsychiatry 2021, 33, 132–143. [Google Scholar] [CrossRef]
- Ljubisavljevic, M.; Ignjatovic, A.; Ljubisavljevic, S. The Ruminative Thought Style with Associated Anxiety Influences the Occurrence of Medication-Overuse Headache. J. Clin. Neurol. 2021, 17, 419–427. [Google Scholar] [CrossRef]
- Sarchielli, P.; Corbelli, I.; Messina, P.; Cupini, L.M.; Bernardi, G.; Bono, G.; Di Piero, V.; Petolicchio, B.; Livrea, P.; Prudenzano, M.P.; et al. Psychopathological comorbidities in medication-overuse headache: a multicentre clinical study. Eur. J. Neurol. 2016, 23, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Mose, L.S.; Pedersen, S.S.; Jensen, R.H.; Gram, B. Personality traits in migraine and medication-overuse headache: A comparative study. Acta Neurol. Scand. 2019, 140, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Corbelli, I. , Caproni, S., Eusebi, P., et al.. Drug-dependence behavior and outcome of medication-overuse headache after treatment. J Headache Pain 2012, 13, 653–660. [Google Scholar] [CrossRef]
- Galli, F.; Tanzilli, A.; Simonelli, A.; Tassorelli, C.; Sances, G.; Parolin, M.; Cristofalo, P.; Gualco, I.; Lingiardi, V. Personality and Personality Disorders in Medication-Overuse Headache: A Controlled Study by SWAP-200. Pain Res. Manag. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sances, G.; Galli, F.; Ghiotto, N.; Allena, M.; Guaschino, E.; Frustaci, A.; Nappi, G.; Tassorelli, C. Factors associated with a negative outcome of medication-overuse headache: A 3-year follow-up (the ‘CARE’ protocol). Cephalalgia 2013, 33, 431–443. [Google Scholar] [CrossRef] [PubMed]
- Lantéri-Minet, M.; Duru, G.; Mudge, M.; Cottrell, S. Quality of life impairment, disability and economic burden associated with chronic daily headache, focusing on chronic migraine with or without medication overuse: A systematic review. Cephalalgia 2011, 31, 837–850. [Google Scholar] [CrossRef]
- Viana, M.; De Icco, R.; Allena, M.; Sances, G.; Højland, J.R.; Katsarava, Z.; Lainez, M.J.A.; Fadic, R.; Goicochea, M.T.; Nappi, G.; et al. Clinical Subtypes of Medication Overuse Headache - Findings From a Large Cohort. Headache: J. Head Face Pain 2019, 59, 1481–1491. [Google Scholar] [CrossRef]
- Mehuys, E.; Paemeleire, K.; Crombez, G.; Adriaens, E.; Van Hees, T.; Demarche, S.; Christiaens, T.; Van Bortel, L.; Van Tongelen, I.; Remon, J.-P.; et al. The heterogeneity of headache patients who self-medicate: a cluster analysis approach. Pain 2016, 157, 1464–1471. [Google Scholar] [CrossRef]
- Pini, L.-A.; Cicero, A.; Sandrini, M. Long-Term Follow-Up of Patients Treated for Chronic Headache with Analgesic Overuse. Cephalalgia 2001, 21, 878–883. [Google Scholar] [CrossRef]
- Saper,JR., and Lake, AE. Medication overuse headache: Type I and type II. Cephalalgia 2006, 26, 1262. [CrossRef]
- Munksgaard, SB. , Jensen, RH. Medication overuse headache. Headache 2014; 54: 1251-1257. Headache 2014, 54, 1251–1257. [Google Scholar] [CrossRef]
- Baumgartner, C.; Wessely, P.; Bingol, C.; Maly, J.; Holzner, F. Longterm Prognosis of Analgesic Withdrawal in Patients with Drug-Induced Headaches. Headache: J. Head Face Pain 1989, 29, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Bendtsen, L.; Munksgaard, S.; Tassorelli, C.; Nappi, G.; Katsarava, Z.; Lainez, M.; Leston, J.; Fadic, R.; Spadafora, S.; Stoppini, A.; et al. Disability, anxiety and depression associated with medication-overuse headache can be considerably reduced by detoxification and prophylactic treatment. Results from a multicentre, multinational study (COMOESTAS project). Cephalalgia 2013, 34, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Lampl, C.; Thomas, H.; Tassorelli, C.; Katsarava, Z.; Laínez, J.M.; Lantéri-Minet, M.; Rastenyte, D.; de la Torre, E.R.; Stovner, L.J.; Andrée, C.; et al. Headache, depression and anxiety: associations in the Eurolight project. J. Headache Pain 2016, 17, 1–9. [Google Scholar] [CrossRef]
- Cupini, LM. , Murtas,MD., Costa, C., et al. Obsessive-compulsive disorder and migraine with medication-overuse headache: research submission. Headache 2009, 49, 1005–1013. [Google Scholar] [CrossRef]
- Curone, M.; Tullo, V.; Mea, E.; Proietti-Cecchini, A.; Peccarisi, C.; Bussone, G. Psychopathological profile of patients with chronic migraine and medication overuse: study and findings in 50 cases. Neurol. Sci. 2011, 32, 177–179. [Google Scholar] [CrossRef]
- Radat, F. , and Lanteri-Minet, M. What is the role of dependence-related behavior in medication-overuse headache? Headache 2010, 50, 1597–1611. [Google Scholar] [CrossRef] [PubMed]
- Galli, F.; Pozzi, G.; Frustaci, A.; Allena, M.; Anastasi, S.; Chirumbolo, A.; Ghiotto, N.; Guidetti, V.; Matarrese, A.; Nappi, G.; et al. Differences in the Personality Profile of Medication-Overuse Headache Sufferers and Drug Addict Patients: A Comparative Study Using MMPI-2. Headache: J. Head Face Pain 2011, 51, 1212–1227. [Google Scholar] [CrossRef]
- Scher, AI. , Stewart, WF., Ricci, JA., et al. Factors associate,d with the onset and remission of chronic daily headache in a population-based study. Pain 2003; 106: 81–89. Pain 2003, 106, 81–89. [Google Scholar] [CrossRef]
- Bigal, M.E.; Liberman, J.N.; Lipton, R.B. Obesity and migraine: A population study. Neurology 2005, 66, 545–550. [Google Scholar] [CrossRef]
- Hershey, A.D.; Powers, S.W.; Nelson, T.D.; Kabbouche, M.A.; Winner, P.; Yonker, M.; Linder, S.L.; Bicknese, A.; Sowel, M.K.; McClintock, W.; et al. Obesity in the Pediatric Headache Population: A Multicenter Study. Headache: J. Head Face Pain 2009, 49, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Pakalnis, A. , and Kring, D. Chronic daily headache, medication overuse, and obesity in children and adolescents. J Child Neurol 2012, 27, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Sancisi, E.; Cevoli, S.; Vignatelli, L.; Nicodemo, M.; Pierangeli, G.; Zanigni, S.; Grimaldi, D.; Cortelli, P.; Montagna, P. Increased Prevalence of Sleep Disorders in Chronic Headache: A Case-Control Study. Headache: J. Head Face Pain 2010, 50, 1464–1472. [Google Scholar] [CrossRef] [PubMed]
- Katsarava, Z.; Fritsche, G.; Muessig, M.; Diener, H.; Limmroth, V. Clinical features of withdrawal headache following overuse of triptans and other headache drugs. Neurology 2001, 57, 1694–1698. [Google Scholar] [CrossRef] [PubMed]
- Fuh, JL. , Wang, SJ., Lu, SR., et al. Does medication overuse headache represent a behavior of dependence? Pain 2005, 119, 49–55. [Google Scholar] [CrossRef]
- Bigal, M.; Rapoport, A.; Sheftell, F.; Tepper, S.; Lipton, R. Transformed Migraine and Medication Overuse in a Tertiary Headache Centre — Clinical Characteristics and Treatment Outcomes. Cephalalgia 2004, 24, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Grande, R.B.; Aaseth, K.; Benth, J.S.; Gulbrandsen, P.; Russell, M.B.; Lundqvist, C. The Severity of Dependence Scale detects people with medication overuse: the Akershus study of chronic headache. J. Neurol. Neurosurg. Psychiatry 2009, 80, 784–789. [Google Scholar] [CrossRef]
- Fritsche, G.; Frettlöh, J.; Hüppe, M.; Dlugaj, M.; Matatko, N.; Gaul, C.; Diener, H.-C. Prevention of medication overuse in patients with migraine. Pain 2010, 151, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Grande, R.B.; Aaseth, K.; Benth, J. .; Lundqvist, C.; Russell, M.B. Reduction in medication-overuse headache after short information. The Akershus study of chronic headache. Eur. J. Neurol. 2010, 18, 129–137. [Google Scholar] [CrossRef]
- Lundqvist, C. , Grande, RB., Aaseth, K., et al. The severity of dependence scale predicts prognosis of medication overuse headache. The Akershus study of chronic headache. Pain 2012, 153, 682–686. [Google Scholar] [CrossRef]
- Pascual, J.; Berciano, J. Daily chronic headache in patients with migraine induced by abuse of ergotamine-analgesics: Response due to a protocol of outpatient treatment. Neurologia 1993, 8, 212–215. [Google Scholar] [PubMed]
- Rossi, P.; Di Lorenzo, C.; Faroni, J.; Cesarino, F.; Nappi, G. Advice Alone Vs. Structured Detoxification Programmes for Medication Overuse Headache: A Prospective, Randomized, Open-Label Trial in Transformed Migraine Patients With Low Medical Needs. Cephalalgia 2006, 26, 1097–1105. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, E.S.; Straand, J.; Vetvik, K.G.; Benth, J. .; Russell, M.B.; Lundqvist, C. Brief intervention by general practitioners for medication-overuse headache, follow-up after 6 months: a pragmatic cluster-randomised controlled trial. J. Neurol. 2015, 263, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, ES. , Straand,J., Vetvik, KG., et al. Brief intervention for medication- overuse headache in primary care. The BIMOH study: a double-blind pragmatic cluster randomized parallel controlled trial. J Neurol Neurosurg Ps 2015, 86, 505–512. [Google Scholar] [CrossRef]
- Kristoffersen, E.S.; Straand, J.; Russell, M.B.; Lundqvist, C. Lasting improvement of medication-overuse headache after brief intervention - a long-term follow-up in primary care. Eur. J. Neurol. 2017, 24, 883–891. [Google Scholar] [CrossRef]
- Créac’h, C.; Frappe, P.; Cancade, M.; Laurent, B.; Peyron, R.; Demarquay, G.; Navez, M. In-patient versus out-patient withdrawal programmes for medication overuse headache: A 2-year randomized trial. Cephalalgia 2011, 31, 1189–1198. [Google Scholar] [CrossRef]
- Suhr, B. , Evers, S., Bauer, B., et al. Drug-induced headache: Long-term results of stationary versus ambulatory withdrawal therapy. Cephalalgia 1999, 19, 44–49. [Google Scholar] [CrossRef]
- Frich, JC. , Kristoffersen, ES., Lundqvist,C. GPs’ experiences with brief intervention for medication-overuse headache: A qualitati,ve study in general practice. Br J Gen Pract 2014, 64, e525–e531. [Google Scholar] [CrossRef]
- Paemeleire, K.; Crevits, L.; Goadsby, P.J.; Kaube, H. Practical management of medication-overuse headache. Acta Neurol. Belg. 2006, 106. [Google Scholar]
- Trucco, M.; Meineri, P.; Ruiz, L.; Gionco, M. Medication Overuse Headache: Withdrawal and Prophylactic Therapeutic Regimen. Headache: J. Head Face Pain 2010, 50, 989–997. [Google Scholar] [CrossRef]
- Obermann, M.; Katsarava, Z. Management of medication-overuse headache. Expert Rev. Neurother. 2007, 7, 1145–1155. [Google Scholar] [CrossRef] [PubMed]
- Tepper, SJ. Medication-overuse headache. Continuum (Minneapolis, Minn) 2012, 18, 807–822. [Google Scholar] [CrossRef] [PubMed]
- Schnider, P. , Aull, S., Baumgartner, C., et al. Long-term outcome of patients w;ith, headache and drug abuse after inpatient withdrawal: Five-year follow-up. Cephalalgia 1996, 16, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Engelstoft, I.M.S.; Carlsen, L.N.; Munksgaard, S.B.; Nielsen, M.; Jensen, R.H.; Bendtsen, L. Complete withdrawal is the most feasible treatment for medication-overuse headache: A randomized controlled open-label trial. Eur. J. Pain 2019, 23, 1162–1170. [Google Scholar] [CrossRef]
- Nielsen, M.; Carlsen, L.N.; Munksgaard, S.B.; Engelstoft, I.M.S.; Jensen, R.H.; Bendtsen, L. Complete withdrawal is the most effective approach to reduce disability in patients with medication-overuse headache: A randomized controlled open-label trial. Cephalalgia 2019, 39, 863–872. [Google Scholar] [CrossRef]
- Katsarava, Z.; Diener, H.-C. Medication Overuse Headache in Germany. Cephalalgia 2008, 28, 1221–1222. [Google Scholar] [CrossRef]
- Limmroth, V. , Biondi, D,. Pfeil, J., et al. T Dopiramate in patients with episodic migraine: reducing the risk for chronic forms of headache. Headache 2007, 47, 13–21. [Google Scholar] [CrossRef]
- Al-Hashel, J.Y.; Ahmed, S.F.; Alroughani, R. Prevalence of Primary Headache Disorders in Kuwait. Neuroepidemiology 2017, 48, 138–146. [Google Scholar] [CrossRef]
- Westergaard, M.L.; Lau, C.J.; Allesøe, K.; Gjendal, S.T.; Jensen, R.H. Monitoring chronic headache and medication-overuse headache prevalence in Denmark. Cephalalgia 2019, 40, 6–18. [Google Scholar] [CrossRef]
- Russell, M.B. Epidemiology and management of medication-overuse headache in the general population. Neurol. Sci. 2019, 40, 23–26. [Google Scholar] [CrossRef]
- Dodick, D.; Freitag, F. Evidence-Based Understanding of Medication-Overuse Headache: Clinical Implications. Headache: J. Head Face Pain 2006, 46, S202–S211. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Stark, R. Intravenous Lignocaine (Lidocaine) Infusion for the Treatment of Chronic Daily Headache with Substantial Medication Overuse. Cephalalgia 2003, 23, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gouveia, R.; Goadsby, P. Neuropsychiatric Side-Effects of Lidocaine: Examples from the Treatment of Headache and a Review. Cephalalgia 2009, 29, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Afridi, S.K.; Shields, K.G.; Bhola, R.; Goadsby, P.J. Greater occipital nerve injection in primary headache syndromes – prolonged effects from a single injection. Pain 2006, 122, 126–129. [Google Scholar] [CrossRef]
- Karadaş. ; Özön, A..; Özçelik, F.; Özge, A. Greater occipital nerve block in the treatment of triptan-overuse headache: A randomized comparative study. Acta Neurol. Scand. 2016, 135, 426–433. [Google Scholar] [CrossRef]
- Olesen, J. Detoxification for medication overuse headache is the primary task. Cephalalgia 2011, 32, 420–422. [Google Scholar] [CrossRef]
- Zeeberg, P.; Olesen, J.; Jensen, R. Efficacy of Multidisciplinary Treatment in a Tertiary Referral Headache Centre. Cephalalgia 2005, 25, 1159–1167. [Google Scholar] [CrossRef]
- Rossi, P.; Faroni, J.V.; Nappi, G. Short-term effectiveness of simple advice as a withdrawal strategy in simple and complicated medication overuse headache. Eur. J. Neurol. 2011, 18, 396–401. [Google Scholar] [CrossRef]
- Bendtsen, L.; Birk, S.; Kasch, H.; Aegidius, K.; Sørensen, P.S.; Thomsen, L.L.; Poulsen, L.; Rasmussen, M.-J.; Kruuse, C.; Jensen, R. Reference programme: Diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 2nd Edition, 2012. J. Headache Pain 2012, 13, 1–29. [Google Scholar] [CrossRef]
- Pijpers, JA. , Wiendels, NJ., Koppen, H., Ferrari, MD., Haan, J., Terwindt, GM. Medication-overuse headache. Ned Tijdschr Geneeskd 2018, 162, 1749. [Google Scholar]
- Radat, F.; Lanteri-Minet, M. What is the Role of Dependence-Related Behavior in Medication-Overuse Headache? Headache: J. Head Face Pain 2010, 50, 1597–1611. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; Jensen, R.; Allena, M.; De Icco, R.; Sances, G.; Katsarava, Z.; Lainez, M.; Leston, J.; Fadic, R.; Spadafora, S.; et al. A consensus protocol for the management of medication-overuse headache: Evaluation in a multicentric, multinational study. Cephalalgia 2014, 34, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, L.N.; Munksgaard, S.B.; Jensen, R.H.; Bendtsen, L. Complete detoxification is the most effective treatment of medication-overuse headache: A randomized controlled open-label trial. Cephalalgia 2017, 38, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Jellestad, P.L.; Carlsen, L.N.; Westergaard, M.L.; Munksgaard, S.B.; Bendtsen, L.; Lainez, M.; Fadic, R.; Katsarava, Z.; Goicochea, M.T.; Spadafora, S.; et al. Economic benefits of treating medication-overuse headache – results from the multicenter COMOESTAS project. Cephalalgia 2018, 39, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Bottiroli, S.; Allena, M.; Sances, G.; De Icco, R.; Avenali, M.; Fadic, R.; Katsarava, Z.; Lainez, M.J.; Goicochea, M.T.; Jensen, R.H.; et al. Changes in anxiety and depression symptoms associated to the outcome of MOH: A post-hoc analysis of the Comoestas Project. Cephalalgia 2017, 38, 646–654. [Google Scholar] [CrossRef]
- Granato, A.; Fantini, J.; Monti, F.; Furlanis, G.; Ilbeh, S.M.; Semenic, M.; Manganotti, P. Dramatic placebo effect of high frequency repetitive TMS in treatment of chronic migraine and medication overuse headache. J. Clin. Neurosci. 2018, 60, 96–100. [Google Scholar] [CrossRef]
- Zidverc-Trajkovic, J.; Pekmezovic, T.; Jovanovic, Z.; Pavlovic, A.; Mijajlovic, M.; Radojicic, A.; Sternic, N. Medication Overuse Headache: Clinical Features Predicting Treatment Outcome at 1-Year Follow-Up. Cephalalgia 2007, 27, 1219–1225. [Google Scholar] [CrossRef]
- Hagen, K.; Albretsen, C.; Vilming, S.; Salvesen, R.; Grøning, M.; Helde, G.; Gravdahl, G.; Zwart, J.-A.; Stovner, L. Management of Medication Overuse Headache: 1-Year Randomized Multicentre Open-Label Trial. Cephalalgia 2009, 29, 221–232. [Google Scholar] [CrossRef]
- Diener, H.-C.; Bussone, G.; Van Oene, J.; Lahaye, M.; Schwalen, S.; Goadsby, P. Topiramate Reduces Headache Days in Chronic Migraine: A Randomized, Double-Blind, Placebo-Controlled Study. Cephalalgia 2007, 27, 814–823. [Google Scholar] [CrossRef]
- Silberstein, S.D.; Lipton, R.B.; Dodick, D.W.; Freitag, F.G.; Ramadan, N.; Mathew, N.; Brandes, J.L.; Bigal, M.; Saper, J.; Ascher, S.; et al. Efficacy and Safety of Topiramate for the Treatment of Chronic Migraine: A Randomized, Double-Blind, Placebo-Controlled Trial. Headache: J. Head Face Pain 2007, 47, 170–180. [Google Scholar] [CrossRef]
- Diener, H.-C.; Dodick, D.; Goadsby, P.; Bigal, M.; Bussone, G.; Silberstein, S.; Mathew, N.; Ascher, S.; Morein, J.; Hulihan, J.; et al. Utility of Topiramate for the Treatment of Patients with Chronic Migraine in the Presence or Absence of Acute Medication Overuse. Cephalalgia 2009, 29, 1021–1027. [Google Scholar] [CrossRef]
- Sarchielli, P.; Messina, P.; Cupini, L.M.; Tedeschi, G.; Di Piero, V.; Livrea, P.; Pini, L.A.; Bernardi, G.; Bono, G.; Sandrini, G.; et al. Sodium valproate in migraine without aura and medication overuse headache: A randomized controlled trial. Eur. Neuropsychopharmacol. 2014, 24, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Dodick, D.W.; Turkel, C.C.; DeGryse, M.; Aurora, S.K.; Silberstein, S.D.; Lipton, R.B.; Diener, H.-C.; Brin, M.F. OnabotulinumtoxinA for Treatment of Chronic Migraine: Pooled Results From the Double-Blind, Randomized, Placebo-Controlled Phases of the PREEMPT Clinical Program. Headache J. Head Face Pain 2010, 50, 921–936. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, S.D.; Blumenfeld, A.M.; Cady, R.K.; Turner, I.M.; Lipton, R.B.; Diener, H.-C.; Aurora, S.K.; Sirimanne, M.; DeGryse, R.E.; Turkel, C.C.; et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J. Neurol. Sci. 2013, 331, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Negro, A.; Curto, M.; Lionetto, L.; Martelletti, P. A two years open-label prospective study of OnabotulinumtoxinA 195 U in medication overuse headache: a real-world experience. J. Headache Pain 2015, 17, 1–9. [Google Scholar] [CrossRef]
- Sandrini, G.; Perrotta, A.; Tassorelli, C.; Torelli, P.; Brighina, F.; Sances, G.; Nappi, G. Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J. Headache Pain 2011, 12, 427–433. [Google Scholar] [CrossRef]
- A Pijpers, J.; A Kies, D.; A Louter, M.; van Zwet, E.W.; Ferrari, M.D.; Terwindt, G.M. Acute withdrawal and botulinum toxin A in chronic migraine with medication overuse: a double-blind randomized controlled trial. Brain 2019, 142, 1203–1214. [Google Scholar] [CrossRef]
- Dressler, D. OnabotulinumtoxinA should be considered in medication overuse withdrawal in patients with chronic migraine. Brain 2019, 143, e5–e5. [Google Scholar] [CrossRef]
- Tiseo, C.; Ornello, R.; Pistoia, F.; Sacco, S. How to integrate monoclonal antibodies targeting the calcitonin gene-related peptide or its receptor in daily clinical practice. J. Headache Pain 2019, 20, 1–13. [Google Scholar] [CrossRef]
- Tepper, S. , Lipton, RB., Silberstein, S., et al. Long-term efficacy of erenumab in chronic migraine patients with acute medication overuse. Poster PF 109LB and E-Poster presentation, 60th American Headache Society Scientific Meeting, San Francisco. Headache 2023, 58, 160–162. [Google Scholar]
- Silberstein, S.D.; Cohen, J.M.; Seminerio, M.J.; Yang, R.; Ashina, S.; Katsarava, Z. The impact of fremanezumab on medication overuse in patients with chronic migraine: subgroup analysis of the HALO CM study. J. Headache Pain 2020, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.-C.; Schwedt, T.J.; Wang, S.-J.; Dodick, D.W. Treatment of medication-overuse headache: A systematic review. Cephalalgia 2015, 36, 371–386. [Google Scholar] [CrossRef] [PubMed]
- Santiago, M.D.S.; Carvalho, D.d.S.; Gabbai, A.A.; Pinto, M.M.P.; Moutran, A.R.C.; Villa, T.R. Amitriptyline and aerobic exercise or amitriptyline alone in the treatment of chronic migraine: a randomized comparative study. Arq. de Neuro-Psiquiatria 2014, 72, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Hepp, Z.; Dodick, D.W.; Varon, S.F.; Chia, J.; Matthew, N.; Gillard, P.; Hansen, R.N.; Devine, E.B. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: A retrospective claims analysis. Cephalalgia 2016, 37, 470–485. [Google Scholar] [CrossRef]
- Hedenrud, T.; Babic, N.; Jonsson, P. Medication Overuse Headache: Self-Perceived and Actual Knowledge Among Pharmacy Staff. Headache: J. Head Face Pain 2014, 54, 1019–1025. [Google Scholar] [CrossRef]
- Ong, J.J.Y.; Chan, Y.C. Medical Undergraduate Survey on Headache Education in Singapore: Knowledge, Perceptions, and Assessment of Unmet Needs. Headache: J. Head Face Pain 2017, 57, 967–978. [Google Scholar] [CrossRef]
- Carlsen, L.N.; Westergaard, M.L.; Bisgaard, M.; Schytz, J.B.; Jensen, R.H. National awareness campaign to prevent medication-overuse headache in Denmark. Cephalalgia 2017, 38, 1316–1325. [Google Scholar] [CrossRef]
- Scher, A.I.; Stewart, W.F.; Lipton, R.B. Caffeine as a risk factor for chronic daily headache: A population-based study. Neurology 2004, 63, 2022–2027. [Google Scholar] [CrossRef]
- Da Silva, A.N.; Lake, A.E. Clinical Aspects of Medication Overuse Headaches. Headache: J. Head Face Pain 2013, 54, 211–217. [Google Scholar] [CrossRef]
- de Goffau, M.J.; Klaver, A.R.; Willemsen, M.G.; Bindels, P.J.; Verhagen, A.P. The Effectiveness of Treatments for Patients With Medication Overuse Headache: A Systematic Review and Meta-Analysis. J. Pain 2017, 18, 615–627. [Google Scholar] [CrossRef]
- Krause, S.J.; Stillman, M.J.; Tepper, D.E.; Zajac, D. A Prospective Cohort Study of Outpatient Interdisciplinary Rehabilitation of Chronic Headache Patients. Headache: J. Head Face Pain 2017, 57, 428–440. [Google Scholar] [CrossRef] [PubMed]
- Gaul, C.; van Doorn, C.; Webering, N.; Dlugaj, M.; Katsarava, Z.; Diener, H.-C.; Fritsche, G. Clinical outcome of a headache-specific multidisciplinary treatment program and adherence to treatment recommendations in a tertiary headache center: an observational study. J. Headache Pain 2011, 12, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.; Hayes, J.; Pakalnis, A. A randomized trial of telephone-based motivational interviewing for adolescent chronic headache with medication overuse. Cephalalgia 2013, 34, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Rausa, M.; Palomba, D.; Cevoli, S.; Lazzerini, L.; Sancisi, E.; Cortelli, P.; Pierangeli, G. Biofeedback in the prophylactic treatment of medication overuse headache: a pilot randomized controlled trial. J. Headache Pain 2016, 17, 1–8. [Google Scholar] [CrossRef]
- Grazzi, L.; Andrasik, F.; D’Amico, D.; Leone, M.; Usai, S.; Kass, S.J.; Bussone, G. Behavioral and Pharmacologic Treatment of Transformed Migraine With Analgesic Overuse: Outcome at 3 Years. Headache: J. Head Face Pain 2002, 42, 483–490. [Google Scholar] [CrossRef]
- Jellestad, P.L.; Carlsen, L.N.; Westergaard, M.L.; Munksgaard, S.B.; Bendtsen, L.; Lainez, M.; Fadic, R.; Katsarava, Z.; Goicochea, M.T.; Spadafora, S.; et al. Economic benefits of treating medication-overuse headache – results from the multicenter COMOESTAS project. Cephalalgia 2018, 39, 274–285. [Google Scholar] [CrossRef]
- Chiang, C.-C.; Schwedt, T.J.; Wang, S.-J.; Dodick, D.W. Treatment of medication-overuse headache: A systematic review. Cephalalgia 2015, 36, 371–386. [Google Scholar] [CrossRef]
- Moore, A.J.; Shevell, M. Chronic Daily Headaches in Pediatric Neurology Practice. J. Child Neurol. 2004, 19, 925–929. [Google Scholar] [CrossRef]
- Gelfand, A.A.; Goadsby, P.J. Medication Overuse in Children and Adolescents. Curr. Pain Headache Rep. 2014, 18, 1–6. [Google Scholar] [CrossRef]
- Fritsche, G.; Eberl, A.; Katsarava, Z.; Limmroth, V.; Diener, H. Drug-Induced Headache: Long-Term Follow-Up of Withdrawal Therapy and Persistence of Drug Misuse. Eur. Neurol. 2001, 45, 229–235. [Google Scholar] [CrossRef]
- Katsarava, Z.; Limmroth, V.; Finke, M.; Diener, H.C.; Fritsche, G. Rates and predictors for relapse in medication overuse headache: A 1-year prospective study. Neurology 2003, 60, 1682–1683. [Google Scholar] [CrossRef] [PubMed]
- Altieri, M. , Di, GR., Di, CL., et al. Combined pharmacological and short-term psychodynamic psychotherapy for probable medication overuse headache: a pilot study. Cephalalgia 2009, 29, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Valguarnera, F.; Tanganelli, P. The efficacy of withdrawal therapy in subjects with chronic daily headache and medication overuse following prophylaxis with topiramate and amitriptyline. Neurol. Sci. 2010, 31, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Grazzi, L.; Sansone, E.; Raggi, A.; D’amico, D.; De Giorgio, A.; Leonardi, M.; De Torres, L.; Salgado-García, F.; Andrasik, F. Mindfulness and pharmacological prophylaxis after withdrawal from medication overuse in patients with Chronic Migraine: an effectiveness trial with a one-year follow-up. J. Headache Pain 2017, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bøe, M.G.; Thortveit, E.; Vatne, A. Chronic headache with medication overuse: Long-term prognosis after withdrawal therapy. Cephalalgia 2016, 37, 1215–1221. [Google Scholar] [CrossRef] [PubMed]
- Guerzoni, S.; Pellesi, L.; Baraldi, C.; Cainazzo, M.M.; Negro, A.; Martelletti, P.; Pini, L.A. Long-term Treatment Benefits and Prolonged Efficacy of OnabotulinumtoxinA in Patients Affected by Chronic Migraine and Medication Overuse Headache over 3 Years of Therapy. Front. Neurol. 2017, 8, 586–586. [Google Scholar] [CrossRef]
- Katsarava, Z.; Muessig, M.; Dzagnidze, A.; Fritsche, G.; Diener, H.; Limmroth, V. Medication Overuse Headache: Rates and Predictors for Relapse in a 4-year Prospective Study. Cephalalgia 2005, 25, 12–15. [Google Scholar] [CrossRef]
- Zidverc-Trajkovic, J.J.; Pekmezovic, T.; Jovanovic, Z.; Pavlovic, A.; Mijajlovic, M.; Radojicic, A.; Sternic, N. Long-term predictors of remission in patients treated for medication-overuse headache at a specialized headache center: A prospective cohort study. Cephalalgia 2016, 38, 265–273. [Google Scholar] [CrossRef]
- Rossi, P.; Faroni, J.; Nappi, G. Medication Overuse Headache: Predictors and Rates of Relapse in Migraine Patients With Low Medical Needs. A 1-Year Prospective Study. Cephalalgia 2008, 28, 1196–1200. [Google Scholar] [CrossRef]
- Raggi, A.; Giovannetti, A.M.; Leonardi, M.; Sansone, E.; Schiavolin, S.; Curone, M.; Grazzi, L.; Usai, S.; D’Amico, D. Predictors of 12-Months Relapse After Withdrawal Treatment in Hospitalized Patients With Chronic Migraine Associated With Medication Overuse: A Longitudinal Observational Study. Headache: J. Head Face Pain 2016, 57, 60–70. [Google Scholar] [CrossRef]
- Sances, G.; Ghiotto, N.; Galli, F.; Guaschino, E.; Rezzani, C.; Guidetti, V.; Nappi, G. Risk factors in medication-overuse headache: A 1-year follow-up study (care II protocol). Cephalalgia 2009, 30, 329–336. [Google Scholar] [CrossRef] [PubMed]
|
|
|
MOH is a secondary headache disorder, although pathophysiologically and clinically it represents a complication of most commonly occurring primary headaches. The diagnosis of MOH is clinical. MOH is a complex entity with biological, psychological, and social aspects. Assessing the risk of MOH occurrence and treatment success is crucial for primary and secondary prevention of MOH. Treatment for MOH is individualized. Discontinuation of medication overuse, transitional therapy, preventive therapy, and monitoring to prevent relapse, prior education, and patient awareness are the foundations of the therapeutic approach. multidisciplinary approach is necessary. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





