1. Introduction
Lipofibromatous hamartoma (LFH), first reported in 1953, is a rare, slowly-progressive soft tissue tumor, characteristic of the enlargement of the affected nerve by epineurial and perineurial proliferation of adipose and fibrous tissues.[
1,
2] Median nerve is the mostly commonly reported nerve of LFH, but there have been previous literatures of LFH occurring on other nerves, such as ulnar, radial, and peroneal nerves. Primary clinical manifestations are an enlarging mass and its nerve compression symptoms when it is large enough. The most common (approximately 1/3) associated anomaly has been reported to be macrodactyly, a condition of which is referred as macrodystrophia lipomatosa.[
3] However, the clinical presentations of LFH vary from asymptomatic to characteristic symptoms of compressive neuropathy.
While carpal tunnel syndrome (CTS) is the most common compressive neuropathy in adult population, but it is reported relatively rare in pediatric populations. While CTS is idiopathic in nature in adults, pediatric CTS are mostly secondary to anatomic variations, trauma, or congenital malformations.[
4] Second to mucopolsaccharidoses, the primary metabolic disorder causing pediatric CTS, LFH is considered a frequent cause to CTS. The two most discussed etiologies of LFH are repetitive microtrauma from the transverse carpal ligament to the median nerve and congenital anomaly.[
5] Differential diagnoses vary from benign to malignant soft tissue tumors, such as ganglion cysts, neurofibroma, schwannoma, and malignant peripheral nerve sheath tumors.[
2]
Since the first introduction of LFH in 1954, there have been approximately 200 cases of LFH of the median nerve, and pediatric cases.[
6] There have been about 25 cases of pediatric LFH occurred under age of 18.[
6,
12,
13,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33] However, even though most previous literatures depend on case reports or a small case series with short-term follow-up periods, some reported progressive declines in sensory and motor functions of the affected nerve in a long-term follow-ups of adult patients.[
8] Herein, we report a case of a 3-year-old female patient with LFH on the left median nerve, who was surgically decompressed via transverse carpal release with epineurolysis and was followed-up annually with ultrasonography assessments until the postoperative 10
th year.
2. Case Description
A three-year old female patient without underlying diseases visited the outpatient clinic at our institution with chief complaints of an enlarging mass and discomfort on volar aspect of the left wrist (
Figure 1). The mother recalled no history of trauma or congenital anomalies but a progressive enlarging solitary mass on the wrist for the past two weeks with mild pain in the beginning. The patient was otherwise unremarkable in medical conditions without any medications, and his immunizations were up to date.
Physical examination revealed a solitary, soft, mildly tender, palpable mass sizing approximately 1 × 1 centimeters on the center of the volar aspect of the wrist. No limitation in the wrist and finger ranges of motions, but the patient’s agitation escalated with passive movement of the wrist joint. For the pediatric patient with difficulty in expressive language yet, it was difficult to subjectively assess Tinel’s sign, Phalen’s test, or specific neuromuscular deficits, but no thenar atophies were noted (
Figure 1). Gross inspection did not indicate any congenital abnormalities, such as polydactyly, or café-au-lait spots.
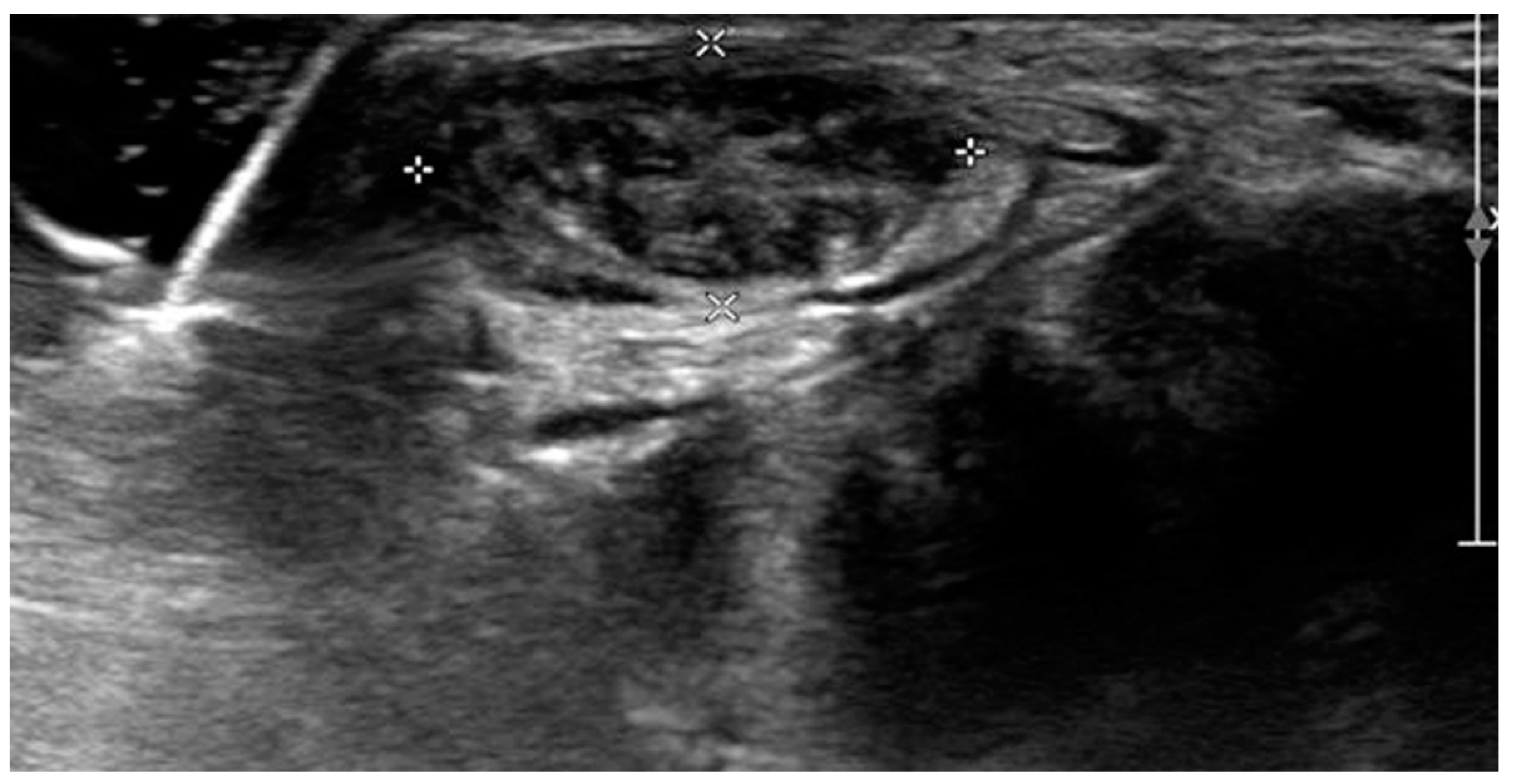
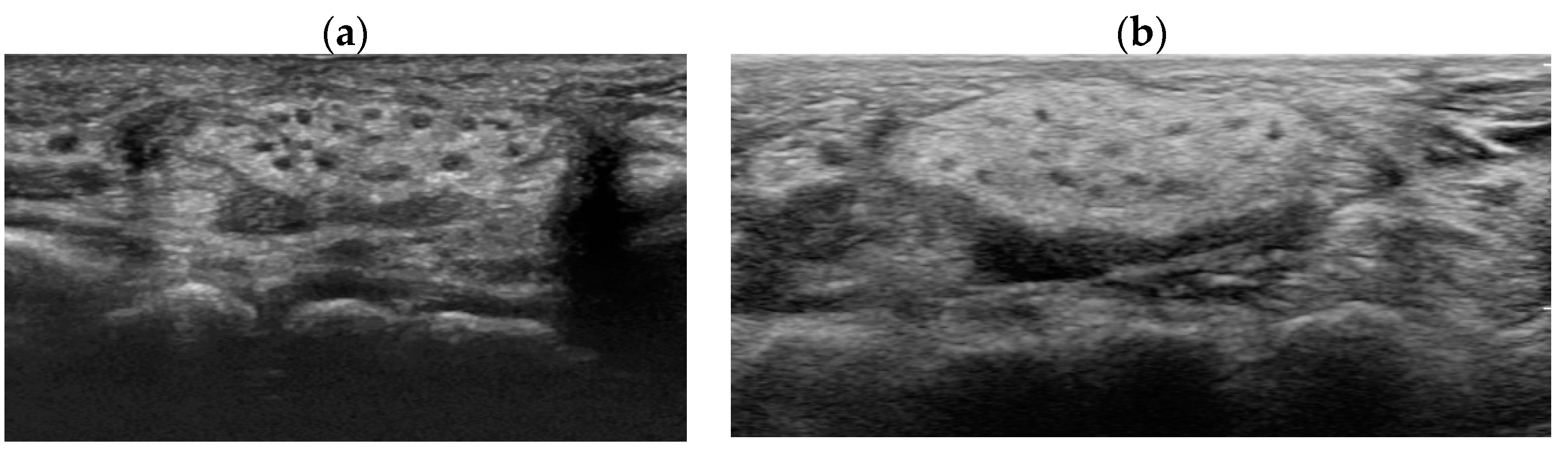
Ultrasonographic examination on the first visit to the clinic showed severely edematous and hypertrophied median nerve from the left wrist level down to the palm with low-echogenic intraneural multiple fascicles (
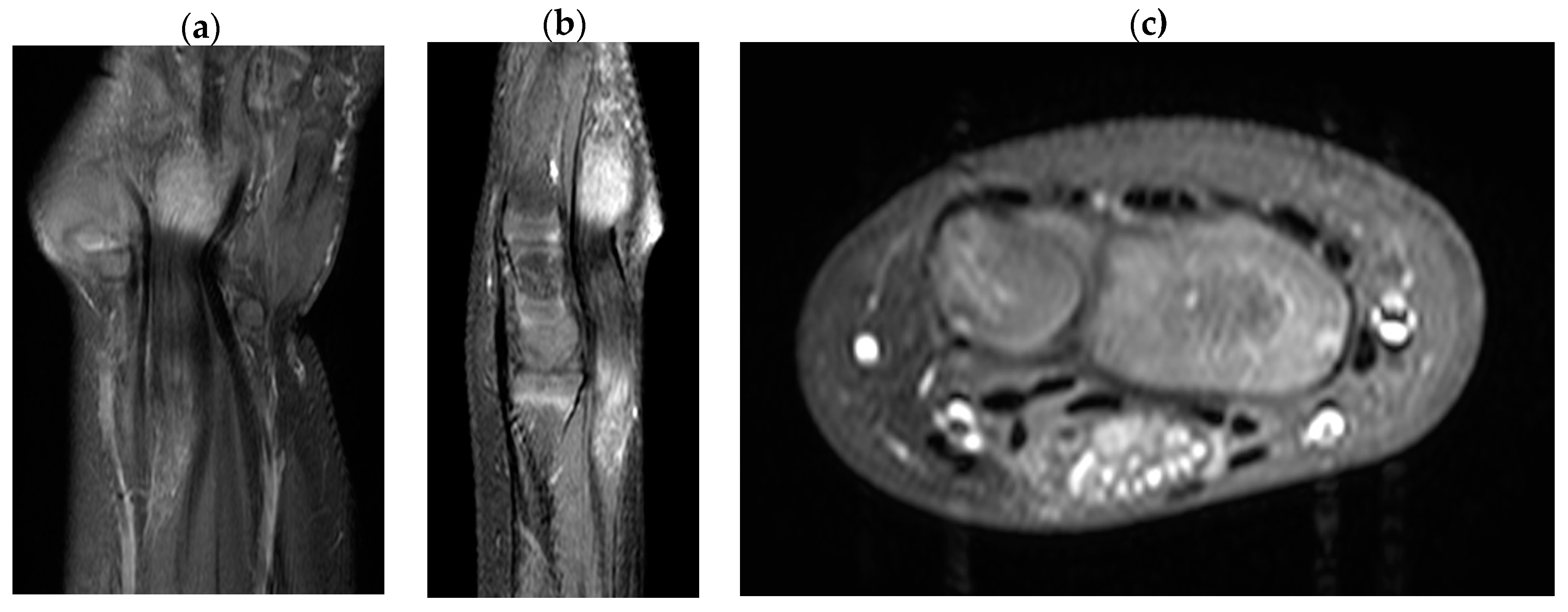
Figure 2). In addition, subsequent enhanced magnetic resonance imaging of the left wrist indicated fusiform enlargement the median nerve from the left forearm distal 1/3 area down to the left hand metacarpal area along with characteristic findings of longitudinally-oriented cable-like appearances of the tumor in addition to its invasion into flexor retinaculum
Figure 3).
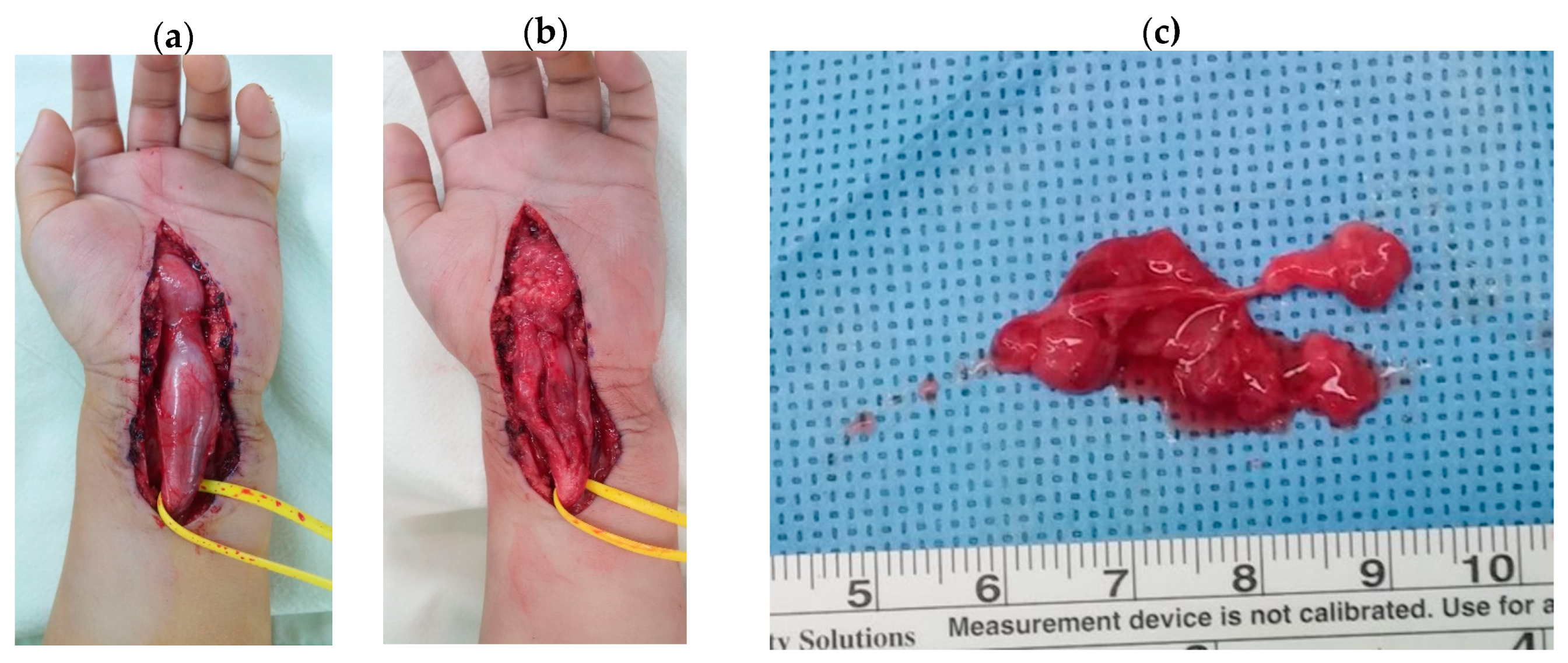
Upon the clinical and radiologic diagnosis of lipofibromatous harmartoma, the patient was scheduled for the decompression of median nerve with a biopsy. A zig-zag incision on the volar aspect of wrist was made from 10 centimeters proximal from the transverse carpal ligament down to metacarpal joints area. Surgical exploration found a fusiform enlargement starting from 2 centimeters proximal to transverse carpal ligament to the level of thenar crease, surrounding the transverse carpal ligament and the median nerve (
Figure 4). After the release of transverse carpal ligament, longitudinal epineurolysis along the median nerve revealed abundant fibro-adipose tissue embedded in the nerve fascicles of the median nerve with severe adhesion. Hypertrophied epineurium was partially resected, and fibro-fatty tissue surrounding the epineurium were biopsied (
Figure 4).
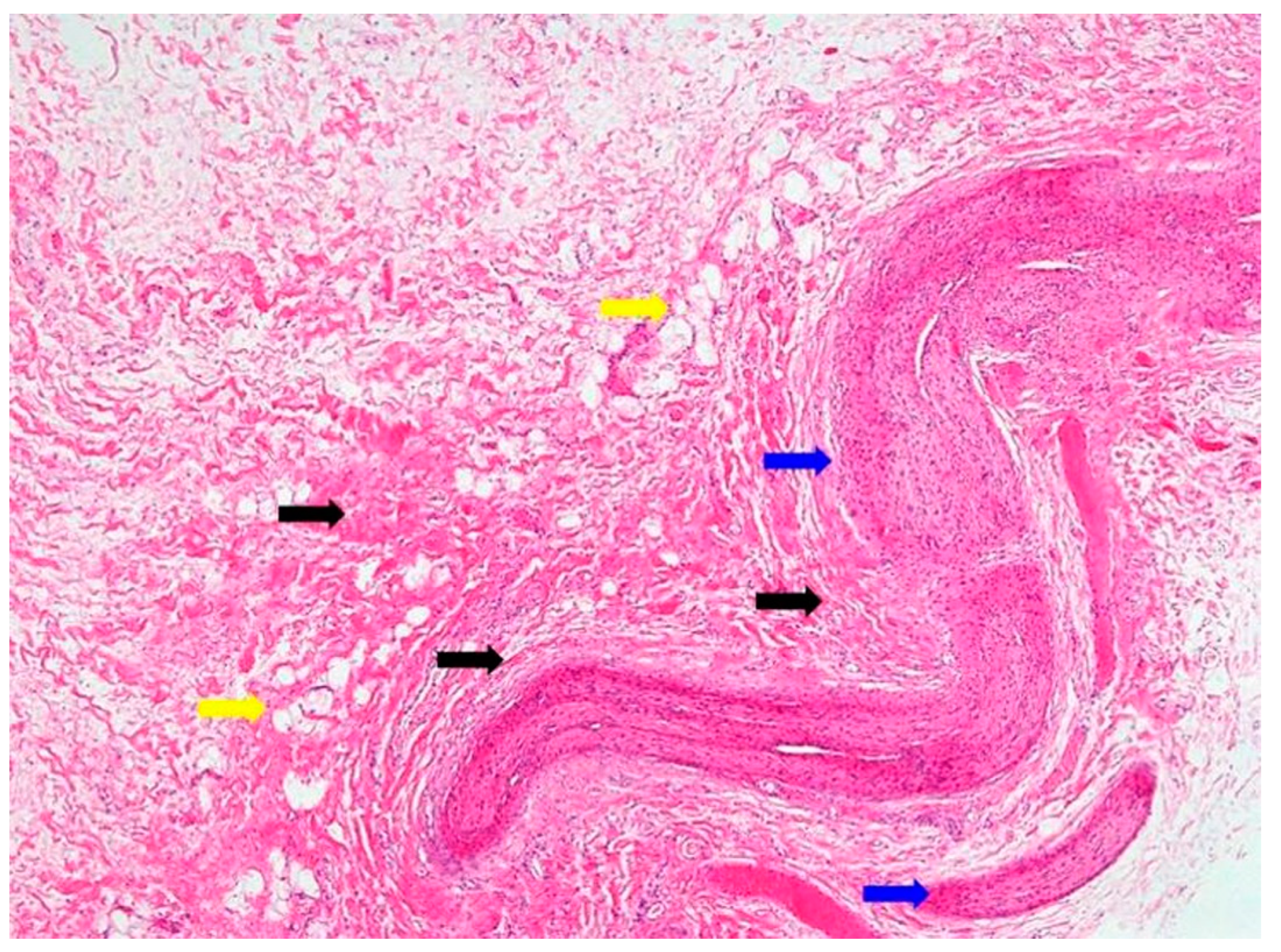
Histologic findings showed abundant thickened nerve bundles and accumulated fibrous and adipose tissues around epineurium, and it confirmed the diagnosis of lipofibromatous harmartoma in the median nerve (
Figure 5).
Postoperatively, the patient’s recovery was uneventful without any complications of pain, discomfort, or decreased joint movement. The patient was followed-up annually with the wrist sonographic examination (
Figure 6). At the 10
th-year follow-up, the patient remained asymptomatic with full opposition function and grip strengths without sensory deficits or further enlargement of the hamartoma in the median nerve, and electromyography and nerve conduction study confirmed no neurologic deficits.
3. Discussion
Since the first introduction in 1953, LFH is a slowly growing soft tissue tumor, which has been reported in 25 pediatric cases of median nerve involvement (
Table 1). Its characteristic clinical manifestations involving median nerve show pain, paresthesia (i.e. numbness, tinging, pin/needles), and motor deficits. Neurologic deficits, if present, are mostly irresponsive to conservative management and indicated for surgical management.[
2]
In the diagnosis of LFH, MRI plays a critical role by offering pathognomic radiologic features, low-intensity serpentine nerve fibers embedded in abundant high-intensity adipose and fibrous tissues, also known as “cable-like appearances”.[
9] In addition, ultrasonography also serves an essential tool for initial diagnosis and postoperative non-invasive radiologic follow-ups. Ultrasound imaging of LFH is characteristic of the enlarged cross-section of the affected nerve with hypoechoic fascicles embedded in the hyperechoic fibrous and adipose tissues, and recent ultrasonography has shown to provide as equivalent diagnostic evidence as MRIs.[
10] While MRIs are beneficial in assessing the extent of the lesion in the initial diagnosis, ultrasonography serves a critical role in serial postoperative follow-ups, as seen in the current case description. However, biopsy and histologic examinations are the only definitive measures for the diagnosis of LFH, which are characteristic of intertwining collagen, fibroblasts, and adipose cells separating nerve fascicles and infiltrating the space between the epineurium and perineurium without inflammation or myelin degeneration.[
2]
In treatment of LFH, there is no standard treatment consensus, and the patient management varies depending on the extent of the soft tissue lesion. Historically, the lipofibromatous lesions were complete excised surgically with devastating sequelae of motor and sensory deficits. However, the current treatment approach has been shifted toward more conservative. Patients with asymptomatic swelling without severe neurologic deficits are frequently closely observed, but surgical treatments for the patients with motor and sensory impairment aim to symptomatic relief from compressive neuropathy without invasive debulking. There have been several previous literatures on techniques for nerve dissections, but their postoperative functions are frequently disappointing.[
8,
11] In addition, nerve grafting after debulking and interaneural dissection have shown some positive results, but their results only showed short clinical follow-ups.[
12,
13] Consequently, tumor excision is generally reserved for the cases with progressive and recurring pain and neurologic deficits even after carpal tunnel release and nerve decompression.[
14] An interesting previous literature on Martin-Gruber anastomosis, a neural anastomosis between median and ulnar nerves, showed preserved hand and digital functions following radical excision of the main trunk of the median nerve.[
15]
It is critical to consider patient’s history, physical examination, and radiologic assessment all together before the decision on surgical treatment. As seen in the current case, when the patient is in the toddler age and incapable of expressive language, clinical assessment of certain signs and symptoms are often limited and challenging even in the postoperative follow-ups. Furthermore, due to its nature of rare entity, it is in reality difficult to compare among various surgical techniques for their effectiveness with a long-term follow-up under well-structured study design. Currently available literature on pediatric LFH lacks long-term follow-up outcomes, and they are mostly followed-up for less than a few years. Therefore, the current case report provides valuable clinical and radiologic outcomes without tumor or symptom recurrences through annual follow-ups consecutively for 10 years. For the 10 years of postoperative period, the patient was able to maintain intact motor and sensory functions without any pain or discomfort after the nerve decompression with the carpal tunnel release and epineurolysis of the median nerve.
4. Conclusions
Due to its rarity of LFH, the precise understandings of epidemiology, treatment, and prognosis are limited in the previous literature. The current case of LFH of the median nerve is the first to be reported in South Korea, and the high index of clinical suspicion for LFH is imperative especially in pediatric carpal tunnel syndrome. Even though very little is known about the predictive prognostic values of surgical techniques, 10-year consecutive follow-up of 3-year-old patient with LFH showed satisfactory outcomes after decompression with carpal tunnel release and epineurolysis. Furthermore, increased multidisciplinary clinical awareness of the tumorous condition is critical for best practice management
Author Contributions
Conceptualization, S.K.K; Investigation, S.J.Y, D.H.L, S.H.C.; Radiologic investigation, K.R.L.; Writing-draft, review, and editing, S.J.Y.; Supervision, S.K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Informed consent was obtained from the patient’s family for the publication of the case report.
Data Availability Statement
Not applicable
Acknowledgments
Not applicable
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mason, LM. AMERICAN Society for Surgery of the hand. The Journal of bone and joint surgery. American volume 1953, 35-a, 257-275.
- Tahiri, Y.; Xu, L.; Kanevsky, J.; Luc, M. Lipofibromatous hamartoma of the median nerve: a comprehensive review and systematic approach to evaluation, diagnosis, and treatment. The Journal of hand surgery 2013, 38, 2055–2067. [Google Scholar] [CrossRef]
- Razzaghi, A.; Anastakis, D.J. Lipofibromatous hamartoma: review of early diagnosis and treatment. Canadian journal of surgery. Journal canadien de chirurgie 2005, 48, 394–399. [Google Scholar]
- Potulska-Chromik, A.; Lipowska, M.; Gawel, M.; Ryniewicz, B.; Maj, E.; Kostera-Pruszczyk, A. Carpal tunnel syndrome in children. Journal of child neurology 2014, 29, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Haase, S.C. Lipofibromatous hamartoma of the median nerve. The Journal of hand surgery 2013, 38, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Shekhani, H.N.; Hanna, T.; Johnson, J.O. Lipofibromatous Hamartoma of the Median Nerve: A Case Report. Journal of radiology case reports 2016, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Amadio, P.C.; Reiman, H.M.; Dobyns, J.H. Lipofibromatous hamartoma of nerve. The Journal of hand surgery 1988, 13, 67–75. [Google Scholar] [CrossRef]
- Louis, D.S.; Hankin, F.M.; Greene, T.L.; Dick, H.M. Lipofibromas of the median nerve: long-term follow-up of four cases. The Journal of hand surgery 1985, 10, 403–408. [Google Scholar] [CrossRef]
- Okechi, H.; Dimostheni, A.; Kerscher, S.R.; Gugel, I.; Bevot, A.; Schaefer, J.F.; Schuhmann, M.U. Fibrolipomatous hamartomas of the median nerve in infancy and early childhood-imaging hallmarks, symptomatology, and treatment. European journal of pediatrics 2018, 177, 567–573. [Google Scholar] [CrossRef]
- Toms, A.P.; Anastakis, D.; Bleakney, R.R.; Marshall, T.J. Lipofibromatous hamartoma of the upper extremity: a review of the radiologic findings for 15 patients. AJR. American journal of roentgenology 2006, 186, 805–811. [Google Scholar] [CrossRef]
- Cui, Q.; Chhabra, A.B.; Leo, B.M.; Pannunzio, M.E. Lipofibromatous hamartoma of a digital nerve. American journal of orthopedics (Belle Mead, N.J.) 2008, 37, E146–148. [Google Scholar]
- Bains, R.; Kotwal, A.; Saeed, W. Recurrent carpal tunnel syndrome in a child due to fibrolipomatous hamartoma of the median nerve successfully treated by limited excision and decompression. Journal of plastic, reconstructive & aesthetic surgery : JPRAS 2006, 59, 1394–1397. [Google Scholar] [CrossRef] [PubMed]
- Elbayer, A.M.; Alharami, S.; Elhessy, A.H. Lipofibromatous Hamartoma of the Median Nerve: A Case Report. Cureus 2023, 15, e33516. [Google Scholar] [CrossRef] [PubMed]
- Louaste, J.; Zejjari, H.; Chkoura, M.; Houmadi, A.; Rachid, K. Carpal tunnel syndrome due to fibrolipomatous hamartoma of the median nerve. Hand (New York, N.Y.) 2011, 6, 76–79. [Google Scholar] [CrossRef]
- Bergman, F.O.; Blom, S.E.; Stenström, S.J. Radical excision of a fibro-fatty proliferation of the median nerve, with no neurological loss symptoms. Plastic and reconstructive surgery 1970, 46, 375–380. [Google Scholar] [CrossRef]
- Sondergaard, G.; Mikkelsen, S. Fibrolipomatous hamartoma of the median nerve. Journal of hand surgery (Edinburgh, Scotland) 1987, 12, 224–226. [Google Scholar] [CrossRef]
- Langa, V.; Posner, M.A.; Steiner, G.E. Lipofibroma of the median nerve: a report of two cases. Journal of hand surgery (Edinburgh, Scotland) 1987, 12, 221–223. [Google Scholar] [CrossRef]
- Walker, C.W.; Adams, B.D.; Barnes, C.L.; Roloson, G.J.; FitzRandolph, R.L. Case report 667. Fibrolipomatous hamartoma of the median nerve. Skeletal radiology 1991, 20, 237–239. [Google Scholar] [CrossRef]
- Camilleri, I.G.; Milner, R.H. Intraneural lipofibroma of the median nerve. Journal of hand surgery (Edinburgh, Scotland) 1998, 23, 120–122. [Google Scholar] [CrossRef]
- Brodwater, B.K.; Major, N.M.; Goldner, R.D.; Layfield, L.J. Macrodystrophia lipomatosa with associated fibrolipomatous hamartoma of the median nerve. Pediatric surgery international 2000, 16, 216–218. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Chen, D.J.; Chen, H.C. Lipofibromatous hamartoma of the median nerve with long-term follow-up. Chang Gung medical journal 2005, 28, 111–116. [Google Scholar]
- De Smet, L. Lipofibromatous hamartoma of the median nerve and macrodactyly. Genetic counseling (Geneva, Switzerland) 2008, 19, 341–343. [Google Scholar] [PubMed]
- Liaw, K.; Kan, J.H. Lipofibromatous hamartoma. Pediatric radiology 2008, 38, 1032. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, D.; Ulrich, F.; Schroeder, M.; Pallua, N. Lipofibromatous hamartoma of the median nerve in patients with macrodactyly: diagnosis and treatment of a rare disease causing carpal tunnel syndrome. Archives of orthopaedic and trauma surgery 2009, 129, 1219–1224. [Google Scholar] [CrossRef]
- Jain, T.P.; Srivastava, D.N.; Mittal, R.; Gamanagatti, S. Fibrolipomatous hamartoma of median nerve. Australasian radiology 2007, 51 Spec No., B98–b100. [Google Scholar] [CrossRef]
- Nardella, D.; Sohawon, S.; Carlier, A. Lipofibromatous hamartoma of the median nerve. Three case reports. Journal of plastic, reconstructive & aesthetic surgery : JPRAS 2009, 62, e314–317. [Google Scholar] [CrossRef]
- Okubo, T.; Saito, T.; Mitomi, H.; Takagi, T.; Torigoe, T.; Suehara, Y.; Katagiri, H.; Murata, H.; Takahashi, M.; Ito, I.; et al. Intraneural lipomatous tumor of the median nerve: Three case reports with a review of literature. International journal of surgery case reports 2012, 3, 407–411. [Google Scholar] [CrossRef]
- Senger, J.L.; Classen, D.; Bruce, G.; Kanthan, R. Fibrolipomatous hamartoma of the median nerve: A cause of acute bilateral carpal tunnel syndrome in a three-year-old child: A case report and comprehensive literature review. Plastic surgery (Oakville, Ont.) 2014, 22, 201–206. [Google Scholar] [CrossRef]
- Kini, J.R.; Kini, H.; Rau, A.; Kamath, J.; Kini, A. Lipofibromatous Hamartoma of the Median Nerve in Association with or without Macrodactyly. Turk patoloji dergisi 2018, 34, 87–91. [Google Scholar] [CrossRef]
- Hoellwarth, J.S.; Goitz, R.J. Lipofibromatous Hamartoma of the Palmar Cutaneous Branch of the Median Nerve. Journal of hand and microsurgery 2018, 10, 109–112. [Google Scholar] [CrossRef]
- Kitridis, D.; Dionellis, P.; Xarchas, K.; Givissis, P. Giant Median Nerve Due to Hamartoma Causing Severe Carpal Tunnel Syndrome. Journal of orthopaedic case reports 2018, 8, 57–60. [Google Scholar] [CrossRef]
- Mohammed Saeed, M.A.; Dawood, A.A.; Mahmood, H.M. Lipofibromatous hamartoma of the median nerve with macrodactyly of middle finger. Journal of clinical orthopaedics and trauma 2019, 10, 1077–1081. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Feng, S.Q.; Mao, Z.M.; Li, L. Microsurgical interfascicular dissection operation is a viable treatment of carpal tunnel syndrome caused by Lipofibromatous hamartoma: A case report. International journal of surgery case reports 2023, 102, 107818. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).