Submitted:
28 August 2023
Posted:
30 August 2023
Read the latest preprint version here
Abstract
Keywords:
Introduction
3. Lifestyle Interventions for preventing and treating cancer
3.1. Glucose management and ketogenic diet
3.1.1. Mechanism
3.1.2. Clinical Evidence
3.1.3. Dosing Recommendations
3.2. Exercise
3.3. Stress Reduction and Sleep
4. Recommended Supplements and Medications for the Treatment of Cancer
4.1. Vitamin D
4.1.1. Mechanism
4.1.2. Clinical Evidence
4.1.3. Dosing Recommendation
4.2. Melatonin
4.2.1. Mechanism
4.2.2. Clinical Evidence
4.2.3. Dosing
4.3. Green tea
4.3.1. Mechanism
4.3.2. Clinical Evidence
4.3.3. Dosing
4.4. Metformin
4.4.1. Mechanism
4.4.2. Clinical Evidence
4.4.3. Dosing
4.5. Curcumin
4.5.1. Mechanism
4.5.2. Clinical Evidence
4.5.3. Dosing
4.6. Mebendazole
4.6.1. Mechanism
4.6.2. Clinical Evidence
4.6.3. Dosing
4.7. Omega-3
4.7.1. Mechanism
4.7.2. Clinical Evidence
4.7.3. Dosing
4.8. Berberine
4.8.1. Mechanisms
4.8.2. Clinical Evidence
4.8.3. Dosing
4.9. Atorvastatin
4.9.1. Mechanism
4.9.2. Clinical Evidence
4.9.3. Dosing
4.10. Disulfiram
4.10.1. Mechanism
4.10.2. Clinical Evidence
4.10.3. Dosing
4.11. Cimetidine
4.11.1. Mechanism
4.11.2. Clinical Studies
4.11.3. Dosing
4.12. Mistletoe
4.12.1. Mechanism
4.12.2. Clinical Evidence
4.12.3. Dosing
4.13. Ashwaganda
4.13.3 Dosing
4.14. Phosphodiesterase 5 inhibitors
4.14.1. Mechanism
4.14.2. Clinical Evidence
4.14.3. Dosing
4.15. Itraconazole
4.15.1. Mechanism
4.15.2. Clinical Evidence
4.15.3. Dosing
5.1. Potential Adjunctive Therapies
5.1.1. Tumour Treating Fields
5.1.2. Photodynamic Therapy
5.1.3. Hyperbaric Oxygen
| Intervention | Mechanism | Evidence | Toxicity | Dosage per day |
| METABOLIC AND LIFESTYLE INTERVENTIONS FOR CANCER TREATMENT | ||||
| Glucose management and ketogenic diet | Restricting carbohydrates prevents their conversion to glucose, impacting the body's metabolic and energy functions. [326,327] | Prevent the high glucose spikes that fuel cancer [328] | Some possible complications for select populations | Ketogenic diet (<50g carbohydrates per day) in 8 hour eating window |
| Exercise | Multiple mechanisms[329] | Improved survival outcomes [330,331,332,333,334,335] | Possible overuse | 30 minutes per day |
| Stress Reduction | Multiple mechanisms [336] | Stress associated with higher cancer risk and poorer survival outcome[64,337,338] | No known fatalities | Daily mindfulness |
| Sleep | Multiple mechanisms [339] | Healthy sleep is essential for metabolic regulation [77] | 8 hours per night | |
| TIER ONE REPURPOSED DRUGS – STRONG RECOMMENDATION | ||||
| Vitamin D | Inhibiting Angiogenesis [340] Stimulating adherence of cells [341] Enhancing intercellular communication [342,343] | Statistically significant reductions in cancer mortality [344]. More significant reductions in cancer risk for those with normal BMI (<25) [345] |
Serum 25-hydroxyvitamin D higher than 150ng/mL are hallmark of vitamin D toxicity due to hypercalcemia [346] | 20,000 to 50,000 IU daily |
| Melatonin | Multiple mechanisms [129,130] | Low levels of melatonin increase breast cancer risk [347] Increases cancer remission and survival rates [348] |
Oral LD50 in mice: 1.25g/kg [349] | Start at 1 mg and increase to 20-30 mg at night (extended/slow release) |
| Green tea | Inhibition of mitochondrial glutamate dehydrogenase by epigallocatechin gallate [350]. Suppression of cancer stem cells [351,352] |
Green tea drinkers have lower risk of breast cancer[353]. Lowers risk of multiple cancers [354]. Lower risk of non-Hodgkin’s Lymphoma [355] |
EGCG: Mouse oral LD50 2.2g/kg | 500-1,000 mg daily |
| Metformin | Blood glucose stabilization [160] Inhibition of AMPK/mTOR pathway [356] |
Lower incidence and higher survivability[357] of colorectal cancer [358]. Survival benefit for people with prostate cancer and concurrent diabetes [359]. Lower risk of cancer in people with type 2 diabetes [360]. |
Oral LD50 in rats: 1g/kg [361] | 1,000 mg twice daily |
| Curcumin | Inducing Apoptosis selectively in cancer cells [362]. Multiple mechanisms [175] |
Significant heterogeneity in trials depending on curcumin formulation [363] | Oral LD50 in rats: >5g/kg [364] | 600 mg daily or as per manufacturer’s suggested dosing |
| Mebendazole | Inhibits cancer-associated signaling pathways [365] | Case reports show improvement [366,367]. Case series with related drug fenbendazole show promise in treating genitourinary malignancies [368] | Oral LD50 in mice: >1280 mg/kg [369] | 100-200 mg daily |
| Omega 3 | modulation of cyclooxygenase activity alteration of membrane and cell surface receptor function[206,370] |
Protective against breast cancer in Asian patients [371] Lower levels of Omega 3 relative to Omega 6 associated with higher cancer mortality [372] |
N/A Possible heavy metal toxicity from extreme overuse [373] |
2-4 g/day |
| Berberine | Multiple mechanisms [374,375] | Can reduce risk of colorectal cancer [376]. Reduces tumor volume in animal studies [377] |
Mouse oral LD50: 329 mg/kg [378] | A daily dose of 1000-1500 mg or 500-600 mg two or three times daily |
| Atorvastatin | Multiple mechanisms [379,380] | Improvement [230,381,382,383,384,385,386,387] | oral LD50 in mice: >5g/kg [388] | 40 mg 2x/day‡. |
| Simvastatin | Multiple mechanisms [380,389] | Case series shows simvastatin may increase radiosensitivity of cancer cells [390] Statin use in US population associated with lower cancer mortality[383] |
Oral mouse LD50: 3g/kg [391] | |
| Disulfiram | Multiple mechanisms [235,392] | Reduce tumor activity in breast cancer [393] | Oral rat LD50: 9g/kg [394] | 80mg 3x daily or 500 mg once daily |
| Cimetidine | Interferes with tumor cell adhesion, angiogenesis and proliferation [395] | Improvement in gastric cancer survivability [396] Improvement in survivability of surgical treatment of colorectal cancers [397] |
Oral rat LD50: 5g/kg [398] | 400-800 mg twice daily |
| Mistletoe | protein synthesis interference, cell-cycle inhibition, and induced apoptosis [251,256] | evidence of the efficacy of mistletoe extracts in gastric and female genital cancer [399] | Peritoneal rat LD50: 1-3g/kg for stem aqueous extract [400] | given subcutaneously by an integrative oncologist, Typical dose 600mg 3x/week [401] |
| Sildenafil | Enhances drug sensitivity [402] | N/A | Increase in adverse events above 200mg [403] | 20 mg daily |
| TIER TWO REPURPOSED DRUGS – WEAK RECOMMENDATION | ||||
| Low dose naltrexone (LDN) | Interfering with cell signalling [404] Immunomodulation [405] Anti-inflammatory [406] |
Improvement in tumors including non-small cell lung cancer (NSCLC) [407] suppress human ovarian cancer [408] |
Oral mouse LD50: 1g/kg [409] |
1-4.5mg daily |
| Doxycycline | Inhibiting anti-apoptotic and angiogenic proteins [410] | N/A | Oral rat LD50: 2g/kg [411] | 100 mg daily (for cycles of 2 weeks – use sparingly) |
| Wheatgrass | Inhibition of metastasis and angiogenesis, Induction of apoptosis [412] | N/A | No observed toxicity at >2g/kg oral dose in mice for 14 days [413] | 9g fermented wheat germ extract daily |
| Intervention | Mechanism | Evidence | Toxicity | Dosage per day |
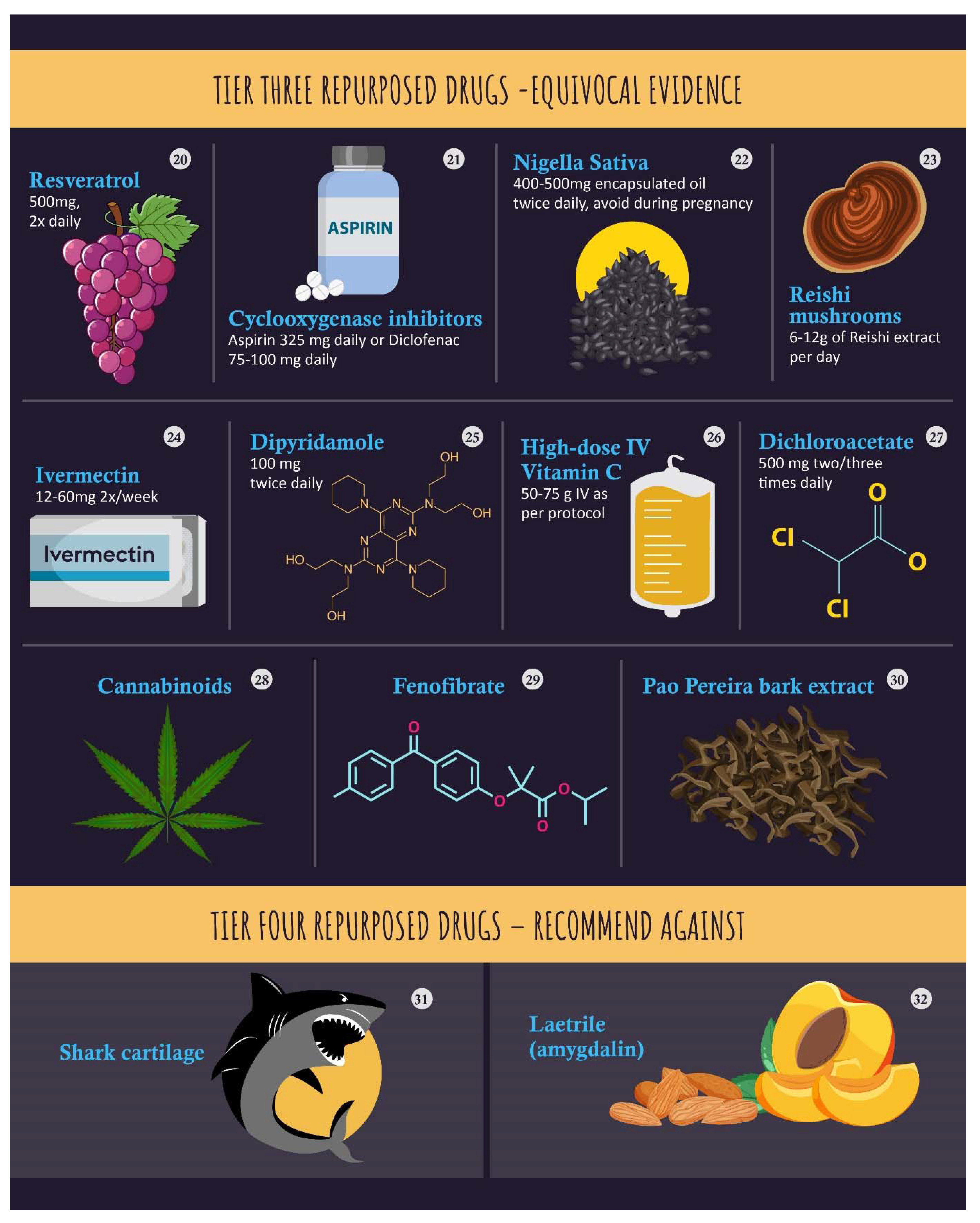
| TIER THREE REPURPOSED DRUGS -EQUIVOCAL EVIDENCE | ||||
| Resveratrol | Induction of apoptosis [414] Inhibition of cancer stem cells [415] |
In vivo evidence for anti-cancer effect, high heterogeneity in humans [416] | Predicted Oral Rat LD50, 48h: 870 mg/kg/day [417] | 500mg, 2x daily |
| Aspirin | Multiple mechanisms [418] | Protective effect on esophageal cancer [419], and other cancers [420] | Oral mouse LD50: 250mg/kg [421] | 325 mg daily |
| Diclofenac | Multiple, mechanisms [422] | Improved disease free survival in breast cancer surgery[423]. Normalizes skin lesions when applied topically [424]. Case studies shows improvement [425,426,427,428,429] |
Mouse oral LD50: 170mg/kg [430] | Diclofenac 75-100 mg daily |
| Nigella Sativa (thymoquinone) | p53, NF-κB, PPARγ, STAT3, MAPK, and PI3K/AKT signaling pathways [431] | improved treatment outcome in acute lymphoblastic leukemia in children[432] | Oral mouse LD50: 29mL/kg [433] | 400-500mg encapsulated oil twice daily, avoid during pregnancy |
| Reishi | Immunomodulation [434,435] | 50% increased effectiveness of cancer chemotherapy [436] | Oral mouse LD50: >10g/kg[437] | 6-12g of Reishi extract per day |
| Ivermectin | Regulates multiple signaling pathways[438,439] | Case series showed improvement in patient symptoms when combined with dichloroacetate [440] | Mouse oral LD50: >27mg/kg [441] | 12-60mg 2x/week |
| Dipyridamole | Increases tumor chemosensitivity [442] | Increases efficacy of other anti-cancer agents [443,444,445] | Rat oral LD50: 8g/kg [446] | 100 mg twice daily |
| Intravenous Vitamin C | Targeted killing (through intracellular generation of H2O2) of cancer cells [447] | Improved life quality in cancer patients [448], lowered inflammation [449] | Rat intravenous LD50 >4g/kg [450] | 50-75 g IV as per protocol |
| Dichloroacetate | Inhibits dehydrogenase kinase to inhibit metabolic reprogramming by cancer cells [451] | Greater treatment response, but no impact on survival [452] | Rat oral LD50 5 g/kg [453] | 500 mg two/three times daily |
| Cannabinoids | induction of cancer cell death by apoptosis and the inhibition of cancer cell proliferation [454] | Useful in treating refractory chemotherapy induced nausea and vomiting Case studies show possible benefit [455] |
THC Mouse oral LD50: 500mg/kg[456] CBD Mouse oral LD50: >100mg/kg [457] |
Daily doses range from 10 to 800mg CBD and 5-8mg THC [458] |
| Fenofibrate | Stimulation of peroxisome proliferator activated receptor α (PPARα) [459] | No clinical data | Mouse oral LD50: 1.6g/kg [460] | N/A |
| Pao Pereira | Inhibition of NF kappa B Signaling [461] | Effectiveness in prostate cancer [462] | Limited information | N/A |
| Potential Adjunctive Therapies | ||||
| Tumor Treating Fields | Multiple mechanisms, induction of apoptosis and autophagy [463] | N/A | N/A | |
| Photodynamic therapy | Direct cellular damage, vascular shutdown and activation of immune response against tumor cells [464] | N/A | N/A | |
| Hyperbaric Oxygen | Elevates levels of reactive oxygen species to signal cell death in cancer cells[465] | N/A | Possible adverse reactions[466] | |
| TIER FOUR REPURPOSED DRUGS – RECOMMEND AGAINST | ||||
| Shark cartilage | inhibition of angiogenesis. sphyrnastatin 1 and 2 have antiangiogenic activity and to inhibit neovascularization [467] | N/A | Gastric adverse events[468], potential neurotoxicity [469] | |
| Laetrile (amygdalin) | Multiple mechanisms [470] | produced few clinical side effects [471] | Rat oral LD50: 0.9g [472] | |
References
- Devic, S. Warburg effect-a consequence or the cause of carcinogenesis? J Cancer 2016, 7, 817. [Google Scholar] [CrossRef] [PubMed]
- Koppenol, W.H.; Bounds, P.L.; Dang, C.V. Otto Warburg's contributions to current concepts of cancer metabolism. Nat Rev Cancer 2011, 11, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, E.K.J.; Ribeiro, M.J.; Stoot, J.H.M.B.; McCready, V.R.; Bourguignon, M.; Mazière, B. FDG Accumulation and Tumor Biology. Nuclear Medicine and Biology 1998, 25, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Bar-Shalom, R.; Valdivia, A.Y.; Blaufox, M.D. PET imaging in oncology. Seminars in Nuclear Medicine 2000, 30, 150–185. [Google Scholar] [CrossRef]
- Smallbone, K.; Gatenby, R.A.; Gillies, R.J.; Maini, P.K.; Gavaghan, D.J. Metabolic changes during carcinogenesis: potential impact on invasiveness. J Theor Biol 2007, 244, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Pugachev, A.; Ruan, S.; Carlin, S.; Larson, S.M.; Campa, J.; Ling, C.C.; Humm, J.L. Dependence of FDG uptake on tumor microenvironment. Int J Radiat Oncol Biol Phys 2005, 62, 545–553. [Google Scholar] [CrossRef]
- Gatenby, R.A.; Gillies, R.J. Why do cancers have high aerobic glycolysis? Nat Rev Cancer 2004, 4, 891–899. [Google Scholar] [CrossRef]
- Seyfried, T. Mitochondria: the ultimate tumor suppressor. In Cancer As a Metabolic Disease: On the Origin, Management, and Prevention of Cancer; 2012; pp. 195–205. [Google Scholar]
- Nebeling, L.C.; Miraldi, F.; Shurin, S.B.; Lerner, E. Effects of a ketogenic diet on tumor metabolism and nutritional status in pediatric oncology patients: two case reports. Journal of the American College of Nutrition 1995, 14, 202–208. [Google Scholar] [CrossRef]
- Schmidt, M.; Pfetzer, N.; Schwab, M.; Strauss, I.; Kämmerer, U. Effects of a ketogenic diet on the quality of life in 16 patients with advanced cancer: A pilot trial. Nutrition & Metabolism 2011, 8, 54. [Google Scholar] [CrossRef]
- Tinguely, D.; Gross, J.; Kosinski, C. Efficacy of Ketogenic Diets on Type 2 Diabetes: a Systematic Review. Curr Diab Rep 2021, 21, 32. [Google Scholar] [CrossRef]
- Poff, A.M.; Ari, C.; Seyfried, T.N.; D’Agostino, D.P. The ketogenic diet and hyperbaric oxygen therapy prolong survival in mice with systemic metastatic cancer. PloS one 2013, 8, e65522. [Google Scholar] [CrossRef] [PubMed]
- Afghahi, A.; Sledge, G.W.J. Targeted Therapy for Cancer in the Genomic Era. The Cancer Journal 2015, 21, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L.; T. Supuran, C.; O. Alfarouk, K. The Warburg Effect and the Hallmarks of Cancer. Anti-Cancer Agents in Medicinal Chemistry- Anti-Cancer Agents) 2017, 17, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Klement, R.J.; Kämmerer, U. Is there a role for carbohydrate restriction in the treatment and prevention of cancer? Nutrition & Metabolism 2011, 8, 75. [Google Scholar] [CrossRef]
- Feng, S.; Wang, H.; Liu, J.; Aa, J.; Zhou, F.; Wang, G. Multi-dimensional roles of ketone bodies in cancer biology: Opportunities for cancer therapy. Pharmacological Research 2019, 150, 104500. [Google Scholar] [CrossRef] [PubMed]
- Ferrere, G.; Alou, M.T.; Liu, P.; Goubet, A.-G.; Fidelle, M.; Kepp, O.; Durand, S.; Iebba, V.; Fluckiger, A.; Daillère, R. Ketogenic diet and ketone bodies enhance the anticancer effects of PD-1 blockade. JCI insight 2021, 6. [Google Scholar] [CrossRef]
- Davies, P.; Demetrius, L.A.; Tuszynski, J.A. Implications of quantum metabolism and natural selection for the origin of cancer cells and tumor progression. AIP Advances 2012, 2. [Google Scholar] [CrossRef]
- T, E.; L, X.; RJ, G.; RA, G. Separation of metabolic supply and demand: aerobic glycolysis as a normal physiological response to fluctuating energetic demands in the membrane. Cancer & metabolism 2014, 2. [Google Scholar] [CrossRef]
- Wittig, R.; Coy, J.F. The Role of Glucose Metabolism and Glucose-Associated Signalling in Cancer. 2017. [Google Scholar] [CrossRef]
- Heiden, M.G.V.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. 2009. [Google Scholar] [CrossRef]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. bmj 2018, 360. [Google Scholar] [CrossRef] [PubMed]
- Barclay, A.W.; Augustin, L.S.A.; Brighenti, F.; Delport, E.; Henry, C.J.; Sievenpiper, J.L.; Usic, K.; Yuexin, Y.; Zurbau, A.; Wolever, T.M.S. Dietary glycaemic index labelling: A global perspective. Nutrients 2021, 13, 3244. [Google Scholar] [CrossRef] [PubMed]
- Matthan, N.R.; Ausman, L.M.; Meng, H.; Tighiouart, H.; Lichtenstein, A.H. Estimating the reliability of glycemic index values and potential sources of methodological and biological variability. The American journal of clinical nutrition 2016, 104, 1004–1013. [Google Scholar] [CrossRef]
- Meidenbauer, J.J.; Mukherjee, P.; Seyfried, T.N. The glucose ketone index calculator: a simple tool to monitor therapeutic efficacy for metabolic management of brain cancer. Nutrition & metabolism 2015, 12, 1–7. [Google Scholar]
- Inchauspé, J. Glucose Revolution: The life-changing power of balancing your blood sugar. Simon and Schuster, 2022. [Google Scholar]
- Maruvada, P.; Leone, V.; Kaplan, L.M.; Chang, E.B. The human microbiome and obesity: moving beyond associations. Cell host & microbe 2017, 22, 589–599. [Google Scholar]
- Nieuwdorp, M.; Gilijamse, P.W.; Pai, N.; Kaplan, L.M. Role of the microbiome in energy regulation and metabolism. Gastroenterology 2014, 146, 1525–1533. [Google Scholar] [CrossRef]
- Pedersen, H.K.; Gudmundsdottir, V.; Nielsen, H.B.; Hyotylainen, T.; Nielsen, T.; Jensen, B.A.H.; Forslund, K.; Hildebrand, F.; Prifti, E.; Falony, G. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 2016, 535, 376–381. [Google Scholar] [CrossRef]
- Rebello, C.J.; Burton, J.; Heiman, M.; Greenway, F.L. Gastrointestinal microbiome modulator improves glucose tolerance in overweight and obese subjects: A randomized controlled pilot trial. Journal of Diabetes and its Complications 2015, 29, 1272–1276. [Google Scholar] [CrossRef]
- Sung, M.M.; Kim, T.T.; Denou, E.; Soltys, C.-L.M.; Hamza, S.M.; Byrne, N.J.; Masson, G.; Park, H.; Wishart, D.S.; Madsen, K.L. Improved glucose homeostasis in obese mice treated with resveratrol is associated with alterations in the gut microbiome. Diabetes 2017, 66, 418–425. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Stratigou, T.; Tsagarakis, S. Microbiome and diabetes: where are we now? Diabetes research and clinical practice 2018, 146, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.W.; Gao, L.; Stastka, P.; Cheney, M.C.; Mahabamunuge, J.; Torres Soto, M.; Ford, C.B.; Bryant, J.A.; Henn, M.R.; Hohmann, E.L. Fecal microbiota transplantation for the improvement of metabolism in obesity: The FMT-TRIM double-blind placebo-controlled pilot trial. PLoS medicine 2020, 17, e1003051. [Google Scholar] [CrossRef]
- Astrup, A.; Teicholz, N.; Magkos, F.; Bier, D.M.; Brenna, J.T.; King, J.C.; Mente, A.; Ordovas, J.M.; Volek, J.S.; Yusuf, S. Dietary saturated fats and health: are the US guidelines evidence-based? Nutrients 2021, 13, 3305. [Google Scholar] [CrossRef] [PubMed]
- Ramsden, C.E.; Zamora, D.; Leelarthaepin, B.; Majchrzak-Hong, S.F.; Faurot, K.R.; Suchindran, C.M.; Ringel, A.; Davis, J.M.; Hibbeln, J.R. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. Bmj 2013, 346, e8707. [Google Scholar] [CrossRef] [PubMed]
- Teicholz, N. The big fat surprise: why butter, meat and cheese belong in a healthy diet; Simon and Schuster, 2014. [Google Scholar]
- Teicholz, N. A short history of saturated fat: the making and unmaking of a scientific consensus. Current Opinion in Endocrinology, Diabetes, and Obesity 2023, 30, 65. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.D.; Aminazdeh-Gohari, S.; Kofler, B. Ketogenic diet in cancer therapy. Aging (Albany NY) 2018, 10, 164–165. [Google Scholar] [CrossRef]
- Augustus, E.; Granderson, I.; Rocke, K.D. The Impact of a Ketogenic Dietary Intervention on the Quality of Life of Stage II and III Cancer Patients: A Randomized Controlled Trial in the Caribbean. Nutrition and Cancer 2021, 73, 1590–1600. [Google Scholar] [CrossRef]
- Kirkpatrick, C.F.; Willard, K.-E.; Maki, K.C. Keto is Trending: Implications for Body Weight and Lipid Management. Current Cardiology Reports 2022, 24, 1093–1100. [Google Scholar] [CrossRef]
- EH, K.; BA, Z.-K.; PE, A.; KR, B.-G.; AG, C.B.; R, B.; JR, B.; RH, C.; J, H.C.; MG, D. , et al. Optimal clinical management of children receiving the ketogenic diet: recommendations of the International Ketogenic Diet Study Group. Epilepsia 2009, 50. [Google Scholar] [CrossRef]
- Cervenka, M.C.; Wood, S.; Bagary, M.; Balabanov, A.; Bercovici, E.; Brown, M.-G.; Devinsky, O.; Lorenzo, C.D.; Doherty, C.P.; Felton, E.; et al. International Recommendations for the Management of Adults Treated With Ketogenic Diet Therapies. 2021. [Google Scholar] [CrossRef]
- K, R.; SL, S. Practice Paper of the Academy of Nutrition and Dietetics: Classic and Modified Ketogenic Diets for Treatment of Epilepsy. Journal of the Academy of Nutrition and Dietetics 2017, 117. [Google Scholar] [CrossRef]
- Martenz, D.M.; Zupec-Kania, B. The Modified Keto Cookbook: Quick, Convenient Great-tasting Recipes for Following a Low-ratio Ketogenic Diet; Springer Publishing Company, 2015. [Google Scholar]
- Lightstone, L.; Shinnar, S.; Callahan, C.M.; O'Dell, C. Reasons for failure of the ketogenic diet. Journal of Neuroscience Nursing 2001, 33, 292. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.J.; Crimarco, A.; Perelman, D.; Durand, L.R.; Petlura, C.; Aronica, L.; Robinson, J.L.; Kim, S.H.; Gardner, C.D. Adherence to ketogenic and mediterranean study diets in a crossover trial: The keto–med randomized trial. Nutrients 2021, 13, 967. [Google Scholar] [CrossRef]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. New England Journal of Medicine 2008, 359, 229–241. [Google Scholar] [CrossRef]
- Mohorko, N.; Černelič-Bizjak, M.; Poklar-Vatovec, T.; Grom, G.; Kenig, S.; Petelin, A.; Jenko-Pražnikar, Z. Weight loss, improved physical performance, cognitive function, eating behavior, and metabolic profile in a 12-week ketogenic diet in obese adults. Nutrition research 2019, 62, 64–77. [Google Scholar] [CrossRef]
- Hamer, J.; Warner, E. Lifestyle modifications for patients with breast cancer to improve prognosis and optimize overall health. Cmaj 2017, 189, E268–E274. [Google Scholar] [CrossRef] [PubMed]
- Montagnese, C.; Porciello, G.; Vitale, S.; Palumbo, E.; Crispo, A.; Grimaldi, M.; Calabrese, I.; Pica, R.; Prete, M.; Falzone, L. Quality of life in women diagnosed with breast cancer after a 12-month treatment of lifestyle modifications. Nutrients 2020, 13, 136. [Google Scholar] [CrossRef]
- Berrino, F.; Villarini, A.; Traina, A.; Bonanni, B.; Panico, S.; Mano, M.P.; Mercandino, A.; Galasso, R.; Barbero, M.; Simeoni, M. Metabolic syndrome and breast cancer prognosis. Breast cancer research and treatment 2014, 147, 159–165. [Google Scholar] [CrossRef]
- Ligibel, J.A.; Bohlke, K.; May, A.M.; Clinton, S.K.; Demark-Wahnefried, W.; Gilchrist, S.C.; Irwin, M.L.; Late, M.; Mansfield, S.; Marshall, T.F. Exercise, diet, and weight management during cancer treatment: ASCO guideline. Journal of Clinical Oncology 2022, 40, 2491–2507. [Google Scholar] [CrossRef]
- Oberoi, S.; Robinson, P.D.; Cataudella, D.; Culos-Reed, S.N.; Davis, H.; Duong, N.; Gibson, F.; Götte, M.; Hinds, P.; Nijhof, S.L. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta-analysis of randomized trials. Critical reviews in oncology/hematology 2018, 122, 52–59. [Google Scholar] [CrossRef]
- Garcia, D.O.; Thomson, C.A. Physical activity and cancer survivorship. Nutrition in Clinical Practice 2014, 29, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.M.; Zabor, E.C.; Schwitzer, E.; Koelwyn, G.J.; Adams, S.C.; Nilsen, T.S.; Moskowitz, C.S.; Matsoukas, K.; Iyengar, N.M.; Dang, C.T. Efficacy of exercise therapy on cardiorespiratory fitness in patients with cancer: a systematic review and meta-analysis. Journal of Clinical Oncology 2018, 36, 2297. [Google Scholar] [CrossRef] [PubMed]
- Aydin, M.; Kose, E.; Odabas, I.; Bingul, B.M.; Demirci, D.; Aydin, Z. The effect of exercise on life quality and depression levels of breast cancer patients. Asian Pacific Journal of Cancer Prevention: APJCP 2021, 22, 725. [Google Scholar] [CrossRef]
- Kenfield, S.A.; Stampfer, M.J.; Giovannucci, E.; Chan, J.M. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. Journal of Clinical Oncology 2011, 29, 726. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.; Galvão, D.A.; Taaffe, D.R.; Newton, R.U.; Souza, G.; Trajano, G.S.; Pinto, R.S. Resistance training in breast cancer patients undergoing primary treatment: a systematic review and meta-regression of exercise dosage. Breast Cancer 2021, 28, 16–24. [Google Scholar] [CrossRef]
- An, K.Y.; Morielli, A.R.; Kang, D.W.; Friedenreich, C.M.; McKenzie, D.C.; Gelmon, K.; Mackey, J.R.; Reid, R.D.; Courneya, K.S. Effects of exercise dose and type during breast cancer chemotherapy on longer-term patient-reported outcomes and health-related fitness: A randomized controlled trial. International journal of cancer 2020, 146, 150–160. [Google Scholar] [CrossRef]
- Beasley, J.M.; Kwan, M.L.; Chen, W.Y.; Weltzien, E.K.; Kroenke, C.H.; Lu, W.; Nechuta, S.J.; Cadmus-Bertram, L.; Patterson, R.E.; Sternfeld, B. Meeting the physical activity guidelines and survival after breast cancer: findings from the after breast cancer pooling project. Breast cancer research and treatment 2012, 131, 637–643. [Google Scholar] [CrossRef]
- Chen, X.; Lu, W.; Zheng, W.; Gu, K.; Matthews, C.E.; Chen, Z.; Zheng, Y.; Shu, X.O. Exercise after diagnosis of breast cancer in association with survival. Cancer Prevention Research 2011, 4, 1409–1418. [Google Scholar] [CrossRef]
- Kelly, P.; Williamson, C.; Niven, A.G.; Hunter, R.; Mutrie, N.; Richards, J. Walking on sunshine: scoping review of the evidence for walking and mental health. British journal of sports medicine 2018, 52, 800–806. [Google Scholar] [CrossRef]
- Lee, I.M.; Buchner, D.M. The importance of walking to public health. Medicine & Science in Sports & Exercise 2008, 40, S512–S518. [Google Scholar]
- Chida, Y.; Hamer, M.; Wardle, J.; Steptoe, A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Rev Clin Oncol 2008, 5, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Metin, Z.G.; Karadas, C.; Izgu, N.; Ozdemir, L.; Demirci, U. Effects of progressive muscle relaxation and mindfulness meditation on fatigue, coping styles, and quality of life in early breast cancer patients: An assessor blinded, three-arm, randomized controlled trial. European Journal of Oncology Nursing 2019, 42, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Greenlee, H.; DuPont-Reyes, M.J.; Balneaves, L.G.; Carlson, L.E.; Cohen, M.R.; Deng, G.; Johnson, J.A.; Mumber, M.; Seely, D.; Zick, S.M. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: a cancer journal for clinicians 2017, 67, 194–232. [Google Scholar] [CrossRef] [PubMed]
- Büttner-Teleagă, A.; Kim, Y.-T.; Osel, T.; Richter, K. Sleep disorders in cancer—a systematic review. International journal of environmental research and public health 2021, 18, 11696. [Google Scholar] [CrossRef]
- Chen, Y.; Tan, F.; Wei, L.; Li, X.; Lyu, Z.; Feng, X.; Wen, Y.; Guo, L.; He, J.; Dai, M. Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose–response relationship. BMC cancer 2018, 18, 1–13. [Google Scholar] [CrossRef]
- Medysky, M.E.; Temesi, J.; Culos-Reed, S.N.; Millet, G.Y. Exercise, sleep and cancer-related fatigue: are they related? Neurophysiologie Clinique/Clinical Neurophysiology 2017, 47, 111–122. [Google Scholar] [CrossRef]
- Lundt, A.; Jentschke, E. Long-term changes of symptoms of anxiety, depression, and fatigue in cancer patients 6 months after the end of yoga therapy. Integrative cancer therapies 2019, 18, 1534735418822096. [Google Scholar] [CrossRef]
- Lopresti, A.L.; Smith, S.J.; Malvi, H.; Kodgule, R. An investigation into the stress-relieving and pharmacological actions of an ashwagandha (Withania somnifera) extract: A randomized, double-blind, placebo-controlled study. Medicine 2019, 98. [Google Scholar] [CrossRef]
- Salve, J.; Pate, S.; Debnath, K.; Langade, D.; Langade, D.G. Adaptogenic and anxiolytic effects of ashwagandha root extract in healthy adults: a double-blind, randomized, placebo-controlled clinical study. Cureus 2019, 11. [Google Scholar] [CrossRef]
- Gopukumar, K.; Thanawala, S.; Somepalli, V.; Rao, T.S.; Thamatam, V.B.; Chauhan, S. Efficacy and safety of ashwagandha root extract on cognitive functions in healthy, stressed adults: a randomized, double-blind, placebo-controlled study. Evidence-Based Complementary and Alternative Medicine 2021, 2021. [Google Scholar] [CrossRef]
- Chandrasekhar, K.; Kapoor, J.; Anishetty, S. A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults. Indian journal of psychological medicine 2012, 34, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Langade, D.; Thakare, V.; Kanchi, S.; Kelgane, S. Clinical evaluation of the pharmacological impact of ashwagandha root extract on sleep in healthy volunteers and insomnia patients: A double-blind, randomized, parallel-group, placebo-controlled study. Journal of ethnopharmacology 2021, 264, 113276. [Google Scholar] [CrossRef] [PubMed]
- Akhgarjand, C.; Asoudeh, F.; Bagheri, A.; Kalantar, Z.; Vahabi, Z.; Shab-bidar, S.; Rezvani, H.; Djafarian, K. Does Ashwagandha supplementation have a beneficial effect on the management of anxiety and stress? A systematic review and meta-analysis of randomized controlled trials. Phytotherapy Research 2022, 36, 4115–4124. [Google Scholar] [CrossRef] [PubMed]
- Vyazovskiy, V.V.; Delogu, A. NREM and REM sleep: complementary roles in recovery after wakefulness. The Neuroscientist 2014, 20, 203–219. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep health 2015, 1, 40–43. [Google Scholar] [CrossRef]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D. National Sleep Foundation's sleep quality recommendations: first report. Sleep health 2017, 3, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Cheah, K.L.; Norhayati, M.N.; Husniati Yaacob, L.; Abdul Rahman, R. Effect of Ashwagandha (Withania somnifera) extract on sleep: A systematic review and meta-analysis. PloS one 2021, 16, e0257843. [Google Scholar] [CrossRef]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep medicine 2017, 32, 246–256. [Google Scholar] [CrossRef]
- Wimalawansa, S.J. Physiological Basis for Using Vitamin D to Improve Health. Biomedicines 2023, 11, 1542. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D Deficiency. New England Journal of Medicine 2002, 357, 266–281. [Google Scholar] [CrossRef]
- Brandi, M.L. Indications on the use of vitamin D and vitamin D metabolites in clinical phenotypes. Clin Cases Miner Bone Metab 2010, 7, 243–250. [Google Scholar] [PubMed]
- Chapuy, M.C.; Preziosi, P.; Maamer, M.; Arnaud, S.; Galan, P.; Hercberg, S.; Meunier, P.J. Prevalence of Vitamin D Insufficiency in an Adult Normal Population. Osteoporosis International 1997, 7, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Vieth, R. Why the optimal requirement for Vitamin D3 is probably much higher than what is officially recommended for adults. The Journal of Steroid Biochemistry and Molecular Biology 2004, 89-90, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Wimalawansa, S.J. Rapidly Increasing Serum 25(OH)D Boosts the Immune System, against Infections—Sepsis and COVID-19. Nutrients 2022, 14. [Google Scholar] [CrossRef]
- Wimalawansa, S.J. Effective and practical ways to overcome vitamin D deficiency. J Family Med Community Health 2021, 8, 1185. [Google Scholar]
- Carlberg, C.; Velleuer, E. Vitamin D and the risk for cancer: A molecular analysis. Biochemical Pharmacology 2022, 196, 114735. [Google Scholar] [CrossRef]
- Baeke, F.; Takiishi, T.; Korf, H.; Gysemans, C.; Mathieu, C. Vitamin D: modulator of the immune system. Current opinion in pharmacology 2010, 10, 482–496. [Google Scholar] [CrossRef]
- Bartley, J. Vitamin D: emerging roles in infection and immunity. Expert review of anti-infective therapy 2010, 8, 1359–1369. [Google Scholar] [CrossRef]
- Chowdhury, R.; Kunutsor, S.; Vitezova, A.; Oliver-Williams, C.; Chowdhury, S.; Kiefte-de-Jong, J.C.; Khan, H.; Baena, C.P.; Prabhakaran, D.; Hoshen, M.B. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. Bmj 2014, 348. [Google Scholar] [CrossRef]
- Ng, K.; Venook, A.P.; Sato, K.; Yuan, C.; Hollis, B.W.; Niedzwiecki, D.; Ye, C.; Chang, I.W.; O'Neil, B.H.; Innocenti, F. Vitamin D status and survival of metastatic colorectal cancer patients: Results from CALGB/SWOG 80405 (Alliance); American Society of Clinical Oncology, 2015. [Google Scholar]
- Hossain, S.; Beydoun, M.A.; Beydoun, H.A.; Chen, X.; Zonderman, A.B.; Wood, R.J. Vitamin D and breast cancer: A systematic review and meta-analysis of observational studies. Clinical nutrition ESPEN 2019, 30, 170–184. [Google Scholar] [CrossRef]
- Zhang, Y.; Fang, F.; Tang, J.; Jia, L.; Feng, Y.; Xu, P.; Faramand, A. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. Bmj 2019, 366. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, A.; Grant, W.B. Vitamin D and cancer: an historical overview of the epidemiology and mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.; Nimeiri, H.S.; McCleary, N.J.; Abrams, T.A.; Yurgelun, M.B.; Cleary, J.M.; Rubinson, D.A.; Schrag, D.; Miksad, R.; Bullock, A.J. Effect of high-dose vs standard-dose vitamin D3 supplementation on progression-free survival among patients with advanced or metastatic colorectal cancer: the SUNSHINE randomized clinical trial. Jama 2019, 321, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- Díaz, G.D.; Paraskeva, C.; Thomas, M.G.; Binderup, L.; Hague, A. Apoptosis is induced by the active metabolite of vitamin D3 and its analogue EB1089 in colorectal adenoma and carcinoma cells: possible implications for prevention and therapy. Cancer research 2000, 60, 2304–2312. [Google Scholar] [PubMed]
- Feldman, D.; Krishnan, A.V.; Swami, S.; Giovannucci, E.; Feldman, B.J. The role of vitamin D in reducing cancer risk and progression. Nature reviews cancer 2014, 14, 342–357. [Google Scholar] [CrossRef]
- Mathieu, C.; Adorini, L. The coming of age of 1, 25-dihydroxyvitamin D3 analogs as immunomodulatory agents. Trends in molecular medicine 2002, 8, 174–179. [Google Scholar] [CrossRef]
- Yang, E.S.; Burnstein, K.L. Vitamin D inhibits G1 to S progression in LNCaP prostate cancer cells through p27Kip1 stabilization and Cdk2 mislocalization to the cytoplasm. Journal of Biological Chemistry 2003, 278, 46862–46868. [Google Scholar] [CrossRef]
- Larriba, M.J.; García de Herreros, A.; Muñoz, A. Vitamin D and the epithelial to mesenchymal transition. Stem cells international 2016, 2016. [Google Scholar] [CrossRef]
- Bernardi, R.J.; Johnson, C.S.; Modzelewski, R.A.; Trump, D.L. Antiproliferative effects of 1α, 25-dihydroxyvitamin D3 and vitamin D analogs on tumor-derived endothelial cells. Endocrinology 2002, 143, 2508–2514. [Google Scholar] [CrossRef]
- Ng, K.; Meyerhardt, J.A.; Wu, K.; Feskanich, D.; Hollis, B.W.; Giovannucci, E.L.; Fuchs, C.S. Circulating 25-hydroxyvitamin d levels and survival in patients with colorectal cancer. Journal of Clinical Oncology 2008, 26, 2984–2991. [Google Scholar] [CrossRef]
- Johansson, H.; Spadola, G.; Tosti, G.; Mandalà, M.; Minisini, A.M.; Queirolo, P.; Aristarco, V.; Baldini, F.; Cocorocchio, E.; Albertazzi, E. Vitamin D supplementation and disease-free survival in stage II melanoma: a randomized placebo controlled trial. Nutrients 2021, 13, 1931. [Google Scholar] [CrossRef] [PubMed]
- Yuan, C.; Sato, K.; Hollis, B.W.; Zhang, S.; Niedzwiecki, D.; Ou, F.-S.; Chang, I.W.; O'Neil, B.H.; Innocenti, F.; Lenz, H.-J. Plasma 25-hydroxyvitamin D levels and survival in patients with advanced or metastatic colorectal cancer: findings from CALGB/SWOG 80405 (Alliance). Clinical Cancer Research 2019, 25, 7497–7505. [Google Scholar] [CrossRef] [PubMed]
- Mezawa, H.; Sugiura, T.; Watanabe, M.; Norizoe, C.; Takahashi, D.; Shimojima, A.; Tamez, S.; Tsutsumi, Y.; Yanaga, K.; Urashima, M. Serum vitamin D levels and survival of patients with colorectal cancer: post-hoc analysis of a prospective cohort study. BMC cancer 2010, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zgaga, L.; Theodoratou, E.; Farrington, S.M.; Din, F.V.; Ooi, L.Y.; Glodzik, D.; Johnston, S.; Tenesa, A.; Campbell, H.; Dunlop, M.G. Plasma vitamin D concentration influences survival outcome after a diagnosis of colorectal cancer. J Clin Oncol 2014, 32, 2430–2439. [Google Scholar] [CrossRef]
- Toriola, A.T.; Nguyen, N.; Scheitler-Ring, K.; Colditz, G.A. Circulating 25-hydroxyvitamin D levels and prognosis among cancer patients: a systematic review. Cancer epidemiology, biomarkers & prevention 2014, 23, 917–933. [Google Scholar]
- Tretli, S.; Schwartz, G.G.; Torjesen, P.A.; Robsahm, T.E. Serum levels of 25-hydroxyvitamin D and survival in Norwegian patients with cancer of breast, colon, lung, and lymphoma: a population-based study. Cancer Causes & Control 2012, 23, 363–370. [Google Scholar]
- Chen, Q.-Y.; Kim, S.; Lee, B.; Jeong, G.; Lee, D.H.; Keum, N.; Manson, J.E.; Giovannucci, E.L. Post-diagnosis vitamin D supplement use and survival among cancer patients: a meta-analysis. Nutrients 2022, 14, 3418. [Google Scholar] [CrossRef]
- Vaughan-Shaw, P.G.; Buijs, L.F.; Blackmur, J.P.; Theodoratou, E.; Zgaga, L.; Din, F.V.N.; Farrington, S.M.; Dunlop, M.G. The effect of vitamin D supplementation on survival in patients with colorectal cancer: systematic review and meta-analysis of randomised controlled trials. British journal of cancer 2020, 123, 1705–1712. [Google Scholar] [CrossRef]
- Kuznia, S.; Zhu, A.; Akutsu, T.; Buring, J.E.; Camargo Jr, C.A.; Cook, N.R.; Chen, L.-J.; Cheng, T.-Y.D.; Hantunen, S.; Lee, I.M. Efficacy of vitamin D3 supplementation on cancer mortality: Systematic review and individual patient data meta-analysis of randomised controlled trials. Ageing research reviews 2023, 101923. [Google Scholar] [CrossRef]
- Wang, L.; Wang, C.; Wang, J.; Huang, X.; Cheng, Y. Longitudinal, observational study on associations between postoperative nutritional vitamin D supplementation and clinical outcomes in esophageal cancer patients undergoing esophagectomy. Scientific Reports 2016, 6, 38962. [Google Scholar] [CrossRef]
- Madden, J.M.; Murphy, L.; Zgaga, L.; Bennett, K. De novo vitamin D supplement use post-diagnosis is associated with breast cancer survival. Breast cancer research and treatment 2018, 172, 179–190. [Google Scholar] [CrossRef]
- Marshall, D.T.; Savage, S.J.; Garrett-Mayer, E.; Keane, T.E.; Hollis, B.W.; Horst, R.L.; Ambrose, L.H.; Kindy, M.S.; Gattoni-Celli, S. Vitamin D3 supplementation at 4000 international units per day for one year results in a decrease of positive cores at repeat biopsy in subjects with low-risk prostate cancer under active surveillance. The Journal of Clinical Endocrinology & Metabolism 2012, 97, 2315–2324. [Google Scholar]
- Wagner, D.; Trudel, D.; Van der Kwast, T.; Nonn, L.; Giangreco, A.A.; Li, D.; Dias, A.; Cardoza, M.; Laszlo, S.; Hersey, K. Randomized clinical trial of vitamin D3 doses on prostatic vitamin D metabolite levels and ki67 labeling in prostate cancer patients. The Journal of Clinical Endocrinology & Metabolism 2013, 98, 1498–1507. [Google Scholar]
- Abu el Maaty, M.A.; Wölfl, S. Effects of 1, 25 (OH) 2D3 on cancer cells and potential applications in combination with established and putative anti-cancer agents. Nutrients 2017, 9, 87. [Google Scholar] [CrossRef] [PubMed]
- Zeichner, S.B.; Koru-Sengul, T.; Shah, N.; Liu, Q.; Markward, N.J.; Montero, A.J.; Glück, S.; Silva, O.; Ahn, E.R. Improved clinical outcomes associated with vitamin D supplementation during adjuvant chemotherapy in patients with HER2+ nonmetastatic breast cancer. Clinical breast cancer 2015, 15, e1–e11. [Google Scholar] [CrossRef] [PubMed]
- Amon, U.; Yaguboglu, R.; Ennis, M.; Holick, M.F.; Amon, J. Safety Data in Patients with Autoimmune Diseases during Treatment with High Doses of Vitamin D3 According to the “Coimbra Protocol”. Nutrients 2022, 14, 1575. [Google Scholar] [CrossRef] [PubMed]
- Finamor, D.C.; Sinigaglia-Coimbra, R.; Neves, L.C.M.; Gutierrez, M.; Silva, J.J.; Torres, L.D.; Surano, F.; Neto, D.J.; Novo, N.F.; Juliano, Y. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermato-endocrinology 2013, 5, 222–234. [Google Scholar] [CrossRef]
- Biancatelli, R.M.L.C.; Berrill, M.; Mohammed, Y.H.; Marik, P.E. Melatonin for the treatment of sepsis: the scientific rationale. Journal of thoracic disease 2020, 12, S54. [Google Scholar] [CrossRef] [PubMed]
- Jockers, R.; Delagrange, P.; Dubocovich, M.L.; Markus, R.P.; Renault, N.; Tosini, G.; Cecon, E.; Zlotos, D.P. Update on melatonin receptors: IUPHAR Review 20. British journal of pharmacology 2016, 173, 2702–2725. [Google Scholar] [CrossRef]
- Jung, B.; Ahmad, N. Melatonin in cancer management: progress and promise. Cancer research 2006, 66, 9789–9793. [Google Scholar] [CrossRef]
- Yeager, R.L.; Oleske, D.A.; Sanders, R.A.; Watkins Iii, J.B.; Eells, J.T.; Henshel, D.S. Melatonin as a principal component of red light therapy. Medical hypotheses 2007, 69, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.-X.; Reiter, R.J.; Zimmerman, S.; Hardeland, R. Melatonin: Both a messenger of darkness and a participant in the cellular actions of non-visible solar radiation of near infrared light. Biology 2023, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Manouchehri, E.; Taghipour, A.; Ghavami, V.; Ebadi, A.; Homaei, F.; Latifnejad Roudsari, R. Night-shift work duration and breast cancer risk: an updated systematic review and meta-analysis. BMC women's health 2021, 21, 1–16. [Google Scholar] [CrossRef]
- Wise, J. Danish night shift workers with breast cancer awarded compensation; British Medical Journal Publishing Group, 2009. [Google Scholar]
- Reiter, R.J.; Rosales-Corral, S.A.; Tan, D.-X.; Acuna-Castroviejo, D.; Qin, L.; Yang, S.-F.; Xu, K. Melatonin, a Full Service Anti-Cancer Agent: Inhibition of Initiation, Progression and Metastasis. International Journal of Molecular Sciences 2017, 18, 843. [Google Scholar] [CrossRef] [PubMed]
- Talib, W.H.; Alsayed, A.R.; Abuawad, A.; Daoud, S.; Mahmod, A.I. Melatonin in Cancer Treatment: Current Knowledge and Future Opportunities. Molecules 2021, 26, 2506. [Google Scholar] [CrossRef] [PubMed]
- Akbarzadeh, M.; Movassaghpour, A.A.; Ghanbari, H.; Kheirandish, M.; Fathi Maroufi, N.; Rahbarghazi, R.; Nouri, M.; Samadi, N. The potential therapeutic effect of melatonin on human ovarian cancer by inhibition of invasion and migration of cancer stem cells. Scientific reports 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sharma, R.; Ma, Q.; Rosales-Corral, S.; Acuna-Castroviejo, D.; Escames, G. Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy. Melatonin Research 2019, 2, 105–119. [Google Scholar] [CrossRef]
- Sanchez-Sanchez, A.M.; Antolin, I.; Puente-Moncada, N.; Suarez, S.; Gomez-Lobo, M.; Rodriguez, C.; Martin, V. Melatonin cytotoxicity is associated to Warburg effect inhibition in Ewing sarcoma cells. PLoS One 2015, 10, e0135420. [Google Scholar] [CrossRef]
- Perfilyeva, Y.V.; Ostapchuk, Y.O.; Abdolla, N.; Tleulieva, R.; Krasnoshtanov, V.C.; Belyaev, N.N. Exogenous melatonin up-regulates expression of CD62L by lymphocytes in aged mice under inflammatory and non-inflammatory conditions. Immunological Investigations 2019, 48, 632–643. [Google Scholar] [CrossRef]
- Liu, H.; Xu, L.; Wei, J.E.; Xie, M.R.; Wang, S.E.; Zhou, R.X. Role of CD4+ CD25+ regulatory T cells in melatonin-mediated inhibition of murine gastric cancer cell growth in vivo and in vitro. The anatomical record: advances in integrative anatomy and evolutionary biology 2011, 294, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Shiu, S.Y.W.; Law, I.C.; Lau, K.W.; Tam, P.C.; Yip, A.W.C.; Ng, W.T. Melatonin slowed the early biochemical progression of hormone-refractory prostate cancer in a patient whose prostate tumor tissue expressed MT1 receptor subtype. Journal of pineal research 2003, 35, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Tomov, B.; Popov, D.; Tomova, R.; Vladov, N.; Den Otter, W.; Krastev, Z. Therapeutic response of untreatable hepatocellular carcinoma after application of the immune modulators IL-2, BCG and melatonin. Anticancer Research 2013, 33, 4531–4535. [Google Scholar]
- Mills, E.; Wu, P.; Seely, D.; Guyatt, G. Melatonin in the treatment of cancer: a systematic review of randomized controlled trials and meta-analysis. Journal of pineal research 2005, 39, 360–366. [Google Scholar] [CrossRef]
- Seely, D.; Wu, P.; Fritz, H.; Kennedy, D.A.; Tsui, T.; Seely, A.J.E.; Mills, E. Melatonin as adjuvant cancer care with and without chemotherapy: a systematic review and meta-analysis of randomized trials. Integrative cancer therapies 2012, 11, 293–303. [Google Scholar] [CrossRef]
- Li, X.-X.; Liu, C.; Dong, S.-L.; Ou, C.-S.; Lu, J.-L.; Ye, J.-H.; Liang, Y.-R.; Zheng, X.-Q. Anticarcinogenic potentials of tea catechins. Frontiers in Nutrition 2022, 9, 3024. [Google Scholar] [CrossRef]
- Caccamo, A.E.; Scaltriti, M.; Caporali, A.; D'Arca, D.; Scorcioni, F.; Astancolle, S.; Mangiola, M.; Bettuzzi, S. Cell detachment and apoptosis induction of immortalized human prostate epithelial cells are associated with early accumulation of a 45 kDa nuclear isoform of clusterin. Biochemical Journal 2004, 382, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Scaltriti, M.; Santamaria, A.; Paciucci, R.; Bettuzzi, S. Intracellular clusterin induces G2-M phase arrest and cell death in PC-3 prostate cancer cells1. Cancer research 2004, 64, 6174–6182. [Google Scholar] [CrossRef]
- Liao, S.; Umekita, Y.; Guo, J.; Kokontis, J.M.; Hiipakka, R.A. Growth inhibition and regression of human prostate and breast tumors in athymic mice by tea epigallocatechin gallate. Cancer letters 1995, 96, 239–243. [Google Scholar] [CrossRef]
- Li, C.; Allen, A.; Kwagh, J.; Doliba, N.M.; Qin, W.; Najafi, H.; Collins, H.W.; Matschinsky, F.M.; Stanley, C.A.; Smith, T.J. Green tea polyphenols modulate insulin secretion by inhibiting glutamate dehydrogenase. Journal of biological chemistry 2006, 281, 10214–10221. [Google Scholar] [CrossRef]
- Rashidi, B.; Malekzadeh, M.; Goodarzi, M.; Masoudifar, A.; Mirzaei, H. Green tea and its anti-angiogenesis effects. Biomedicine & Pharmacotherapy 2017, 89, 949–956. [Google Scholar]
- Song, Q.; Zhang, G.; Wang, B.; Cao, G.; Li, D.; Wang, Y.; Zhang, Y.; Geng, J.; Li, H.; Li, Y. Reinforcing the combinational immuno-oncotherapy of switching “cold” tumor to “hot” by responsive penetrating nanogels. ACS Applied Materials & Interfaces 2021, 13, 36824–36838. [Google Scholar]
- McCarty, M.F.; Iloki-Assanga, S.; Lujany, L.M.L. Nutraceutical targeting of TLR4 signaling has potential for prevention of cancer cachexia. Medical Hypotheses 2019, 132, 109326. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-H.; Shen, Y.-A.; Hung, P.-H.; Yu, Y.-B.; Chen, Y.-J. Epigallocathechin gallate, polyphenol present in green tea, inhibits stem-like characteristics and epithelial-mesenchymal transition in nasopharyngeal cancer cell lines. BMC Complementary and Alternative Medicine 2012, 12, 1–12. [Google Scholar] [CrossRef]
- Bonuccelli, G.; Sotgia, F.; Lisanti, M.P. Matcha green tea (MGT) inhibits the propagation of cancer stem cells (CSCs), by targeting mitochondrial metabolism, glycolysis and multiple cell signalling pathways. Aging (Albany NY) 2018, 10, 1867. [Google Scholar] [CrossRef] [PubMed]
- El-Nashar, H.A.S.; Aly, S.H.; Ahmadi, A.; El-Shazly, M. The Impact of Polyphenolics in the Management of Breast Cancer: Mechanistic Aspects and Recent Patents. Recent Patents on Anti-Cancer Drug Discovery 2022, 17, 358–379. [Google Scholar] [CrossRef]
- Kim, T.L.; Jeong, G.H.; Yang, J.W.; Lee, K.H.; Kronbichler, A.; Van Der Vliet, H.J.; Grosso, G.; Galvano, F.; Aune, D.; Kim, J.Y. Tea consumption and risk of cancer: an umbrella review and meta-analysis of observational studies. Advances in Nutrition 2020, 11, 1437–1452. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Call, T.G.; Zent, C.S.; LaPlant, B.; Bowen, D.A.; Roos, M.; Secreto, C.R.; Ghosh, A.K.; Kabat, B.F.; Lee, M.-J. Phase I trial of daily oral Polyphenon E in patients with asymptomatic Rai stage 0 to II chronic lymphocytic leukemia. Journal of Clinical Oncology 2009, 27, 3808. [Google Scholar] [CrossRef]
- Lemanne, D.; Block, K.I.; Kressel, B.R.; Sukhatme, V.P.; White, J.D. A case of complete and durable molecular remission of chronic lymphocytic leukemia following treatment with epigallocatechin-3-gallate, an extract of green tea. Cureus 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Kubatka, P.; Mazurakova, A.; Samec, M.; Koklesova, L.; Zhai, K.; Al-Ishaq, R.; Kajo, K.; Biringer, K.; Vybohova, D.; Brockmueller, A. Flavonoids against non-physiologic inflammation attributed to cancer initiation, development, and progression—3PM pathways. Epma Journal 2021, 1–29. [Google Scholar] [CrossRef]
- Bettuzzi, S.; Brausi, M.; Rizzi, F.; Castagnetti, G.; Peracchia, G.; Corti, A. Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer research 2006, 66, 1234–1240. [Google Scholar] [CrossRef] [PubMed]
- Sarma, D.N.; Barrett, M.L.; Chavez, M.L.; Gardiner, P.; Ko, R.; Mahady, G.B.; Marles, R.J.; Pellicore, L.S.; Giancaspro, G.I.; Dog, T.L. Safety of green tea extracts: a systematic review by the US Pharmacopeia. Drug safety 2008, 31, 469–484. [Google Scholar] [CrossRef]
- Mazzanti, G.; Di Sotto, A.; Vitalone, A. Hepatotoxicity of green tea: an update. Archives of toxicology 2015, 89, 1175–1191. [Google Scholar] [CrossRef] [PubMed]
- Dowling, R.J.; Niraula, S.; Stambolic, V.; Goodwin, P.J. Metformin in cancer: translational challenges. Journal of molecular endocrinology 2012, 48, R31–43. [Google Scholar] [CrossRef]
- Dowling, R.J.O.; Zakikhani, M.; Fantus, I.G.; Pollak, M.; Sonenberg, N. Metformin inhibits mammalian target of rapamycin–dependent translation initiation in breast cancer cells. Cancer research 2007, 67, 10804–10812. [Google Scholar] [CrossRef]
- Andrzejewski, S.; Siegel, P.M.; St-Pierre, J. Metabolic Profiles Associated With Metformin Efficacy in Cancer. Frontiers in Endocrinology 2018, 9, 372. [Google Scholar] [CrossRef]
- Saraei, P.; Asadi, I.; Kakar, M.A.; Moradi-Kor, N. The beneficial effects of metformin on cancer prevention and therapy: a comprehensive review of recent advances. Cancer management and research 2019, 3295–3313. [Google Scholar] [CrossRef]
- Barrios-Bernal, P.; Zatarain-Barrón, Z.L.; Hernández-Pedro, N.; Orozco-Morales, M.; Olivera-Ramírez, A.; Ávila-Moreno, F.; Colín-González, A.L.; Cardona, A.F.; Rosell, R.; Arrieta, O. Will We Unlock the Benefit of Metformin for Patients with Lung Cancer? Lessons from Current Evidence and New Hypotheses. Pharmaceuticals 2022, 15, 786. [Google Scholar] [CrossRef]
- Shi, P.; Liu, W.; Wang, H.; Li, F.; Zhang, H.; Wu, Y.; Kong, Y.; Zhou, Z.; Wang, C.; Chen, W. Metformin suppresses triple-negative breast cancer stem cells by targeting KLF5 for degradation. Cell discovery 2017, 3, 1–13. [Google Scholar] [CrossRef]
- Gandini, S.; Puntoni, M.; Heckman-Stoddard, B.M.; Dunn, B.K.; Ford, L.; DeCensi, A.; Szabo, E. Metformin and cancer risk and mortality: a systematic review and meta-analysis taking into account biases and confounders. Cancer prevention research 2014, 7, 867–885. [Google Scholar] [CrossRef]
- Zhang, P.; Li, H.; Tan, X.; Chen, L.; Wang, S. Association of metformin use with cancer incidence and mortality: a meta-analysis. Cancer epidemiology 2013, 37, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Lega, I.C.; Shah, P.S.; Margel, D.; Beyene, J.; Rochon, P.A.; Lipscombe, L.L. The effect of metformin on mortality following cancer among patients with diabetes. Cancer Epidemiology, Biomarkers & Prevention 2014, 23, 1974–1984. [Google Scholar]
- Mei, Z.-B.; Zhang, Z.-J.; Liu, C.-Y.; Liu, Y.; Cui, A.; Liang, Z.-L.; Wang, G.-H.; Cui, L. Survival benefits of metformin for colorectal cancer patients with diabetes: a systematic review and meta-analysis. PLoS One 2014, 9, e91818. [Google Scholar] [CrossRef]
- Yin, M.; Zhou, J.; Gorak, E.J.; Quddus, F. Metformin is associated with survival benefit in cancer patients with concurrent type 2 diabetes: a systematic review and meta-analysis. The oncologist 2013, 18, 1248–1255. [Google Scholar] [CrossRef] [PubMed]
- Coyle, C.; Cafferty, F.H.; Vale, C.; Langley, R.E. Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Annals of Oncology 2016, 27, 2184–2195. [Google Scholar] [CrossRef]
- Eibl, G.; Rozengurt, E. Metformin: review of epidemiology and mechanisms of action in pancreatic cancer. Cancer and Metastasis Reviews 2021, 40, 865–878. [Google Scholar] [CrossRef]
- Jiménez-Vacas, J.M.; Herrero-Aguayo, V.; Montero-Hidalgo, A.J.; Sáez-Martínez, P.; Gómez-Gómez, E.; León-González, A.J.; Fuentes-Fayos, A.C.; Yubero-Serrano, E.M.; Requena-Tapia, M.J.; López, M. Clinical, cellular, and molecular evidence of the additive antitumor effects of biguanides and statins in prostate cancer. The Journal of Clinical Endocrinology & Metabolism 2021, 106, e696–e710. [Google Scholar]
- Buczyńska, A.; Sidorkiewicz, I.; Krętowski, A.J.; Zbucka-Krętowska, M.; Adamska, A. Metformin intervention—A panacea for cancer treatment? Cancers 2022, 14, 1336. [Google Scholar] [CrossRef]
- Stopsack, K.H.; Ziehr, D.R.; Rider, J.R.; Giovannucci, E.L. Metformin and prostate cancer mortality: a meta-analysis. Cancer causes & control 2016, 27, 105–113. [Google Scholar]
- Wang, Y.; Liu, G.; Tong, D.; Parmar, H.; Hasenmayer, D.; Yuan, W.; Zhang, D.; Jiang, J. Metformin represses androgen-dependent and androgen-independent prostate cancers by targeting androgen receptor. The Prostate 2015, 75, 1187–1196. [Google Scholar] [CrossRef]
- Giordano, A.; Tommonaro, G. Curcumin and Cancer. Nutrients 2019, 11, 2376. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, K.; Rasoulpoor, S.; Daneshkhah, A.; Abolfathi, S.; Salari, N.; Mohammadi, M.; Rasoulpoor, S.; Shabani, S. Clinical effects of curcumin in enhancing cancer therapy: A systematic review. BMC cancer 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.-W.; Lee, K.-S.; Kim, C.-W. Curcumin attenuates the expression of IL-1β, IL-6, and TNF-α as well as cyclin E in TNF-α-treated HaCaT cells; NF-κB and MAPKs as potential upstream targets. International journal of molecular medicine 2007, 19, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Darvishi, B.; Ghanei, M.; Jowzi, N.; Beiraghdar, F.; Varnamkhasti, B.S. Molecular mechanisms of curcumins suppressing effects on tumorigenesis, angiogenesis and metastasis, focusing on NF-κB pathway. Cytokine & growth factor reviews 2016, 28, 21–29. [Google Scholar]
- Alexandrow, M.G.; Song, L.J.; Altiok, S.; Gray, J.; Haura, E.B.; Kumar, N.B. Curcumin: a novel stat 3 pathway inhibitor for chemoprevention of lung cancer. European Journal of Cancer Prevention 2012, 21, 407. [Google Scholar] [CrossRef]
- Yim-Im, W.; Sawatdichaikul, O.; Semsri, S.; Horata, N.; Mokmak, W.; Tongsima, S.; Suksamrarn, A.; Choowongkomon, K. Computational analyses of curcuminoid analogs against kinase domain of HER2. BMC bioinformatics 2014, 15, 1–13. [Google Scholar] [CrossRef]
- Starok, M.; Preira, P.; Vayssade, M.; Haupt, K.; Salomé, L.; Rossi, C. EGFR inhibition by curcumin in cancer cells: a dual mode of action. Biomacromolecules 2015, 16, 1634–1642. [Google Scholar] [CrossRef]
- James, M.I.; Iwuji, C.; Irving, G.; Karmokar, A.; Higgins, J.A.; Griffin-Teal, N.; Thomas, A.; Greaves, P.; Cai, H.; Patel, S.R. Curcumin inhibits cancer stem cell phenotypes in ex vivo models of colorectal liver metastases, and is clinically safe and tolerable in combination with FOLFOX chemotherapy. Cancer letters 2015, 364, 135–141. [Google Scholar] [CrossRef]
- Wang, J.Y.; Wang, X.; Wang, X.J.; Zheng, B.Z.; Wang, Y.; Liang, B. Curcumin inhibits the growth via Wnt/β-catenin pathway in non-small-cell lung cancer cells. European Review for Medical & Pharmacological Sciences 2018, 22. [Google Scholar]
- Zoi, V.; Galani, V.; Lianos, G.D.; Voulgaris, S.; Kyritsis, A.P.; Alexiou, G.A. The role of curcumin in cancer treatment. Biomedicines 2021, 9, 1086. [Google Scholar] [CrossRef]
- Santosa, D.; Suharti, C.; Riwanto, I.; Dharmana, E.; Pangarsa, E.A.; Setiawan, B.; Suyono, S.; Tobing, M.L.; Suhartono, S.; Hadisapurto, S. Curcumin as adjuvant therapy to improve remission in myeloma patients: A pilot randomized clinical trial. Caspian Journal of Internal Medicine 2022, 13, 375. [Google Scholar] [PubMed]
- Pastorelli, D.; Fabricio, A.S.C.; Giovanis, P.; D'Ippolito, S.; Fiduccia, P.; Soldà, C.; Buda, A.; Sperti, C.; Bardini, R.; Da Dalt, G. Phytosome complex of curcumin as complementary therapy of advanced pancreatic cancer improves safety and efficacy of gemcitabine: Results of a prospective phase II trial. Pharmacological research 2018, 132, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, N.; Aggarwal, B.B.; Newman, R.A.; Wolff, R.A.; Kunnumakkara, A.B.; Abbruzzese, J.L.; Ng, C.S.; Badmaev, V.; Kurzrock, R. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clinical cancer research 2008, 14, 4491–4499. [Google Scholar] [CrossRef]
- Saghatelyan, T.; Tananyan, A.; Janoyan, N.; Tadevosyan, A.; Petrosyan, H.; Hovhannisyan, A.; Hayrapetyan, L.; Arustamyan, M.; Arnhold, J.; Rotmann, A.-R. Efficacy and safety of curcumin in combination with paclitaxel in patients with advanced, metastatic breast cancer: A comparative, randomized, double-blind, placebo-controlled clinical trial. Phytomedicine 2020, 70, 153218. [Google Scholar] [CrossRef]
- Panahi, Y.; Saadat, A.; Beiraghdar, F.; Nouzari, S.M.H.; Jalalian, H.R.; Sahebkar, A. Antioxidant effects of bioavailability-enhanced curcuminoids in patients with solid tumors: A randomized double-blind placebo-controlled trial. Journal of Functional Foods 2014, 6, 615–622. [Google Scholar] [CrossRef]
- Desai, P.; Ann, D.; Wang, J.; Prabhu, S. Pancreatic cancer: Recent advances in nanoformulation-based therapies. Critical Reviews™ in therapeutic drug carrier systems 2019, 36. [Google Scholar] [CrossRef]
- Fda, F. Notice to US Food and Drug Administration of the Conclusion That the Intended Use of Curcumin is Generally Recognized as Safe. Food and Drug Administration, GRAS Notice 2018, 822. [Google Scholar]
- Kim, D.-C.; Ku, S.-K.; Bae, J.-S. Anticoagulant activities of curcumin and its derivative. BMB reports 2012, 45, 221–226. [Google Scholar] [CrossRef]
- Pantziarka, P.; Bouche, G.; Meheus, L.; Sukhatme, V.; Sukhatme, V.P. Repurposing Drugs in Oncology (ReDO)—mebendazole as an anti-cancer agent. ecancermedicalscience 2014, 8. [Google Scholar] [CrossRef]
- Guerini, A.E.; Triggiani, L.; Maddalo, M.; Bonù, M.L.; Frassine, F.; Baiguini, A.; Alghisi, A.; Tomasini, D.; Borghetti, P.; Pasinetti, N. Mebendazole as a candidate for drug repurposing in oncology: An extensive review of current literature. Cancers 2019, 11, 1284. [Google Scholar] [CrossRef]
- Larsen, A.R.; Bai, R.-Y.; Chung, J.H.; Borodovsky, A.; Rudin, C.M.; Riggins, G.J.; Bunz, F. Repurposing the antihelmintic mebendazole as a hedgehog inhibitor. Molecular cancer therapeutics 2015, 14, 3–13. [Google Scholar] [CrossRef]
- Fong, D.; Christensen, C.T.; Chan, M.M. Targeting cancer stem cells with repurposed drugs to improve current therapies. Recent patents on anti-cancer drug discovery 2021, 16, 136–160. [Google Scholar] [PubMed]
- Mukherjee, P.; Greenwood, B.; Henao, J.; Kiebish, M.A.; Seyfried, T.N. Ketogenic diet as a metabolic vehicle for enhancing the therapeutic efficacy of mebendazole and devimistat in preclinical pediatric glioma. bioRxiv 2023, 2023–2006. [Google Scholar]
- Meco, D.; Attinà, G.; Mastrangelo, S.; Navarra, P.; Ruggiero, A. Emerging Perspectives on the Antiparasitic Mebendazole as a Repurposed Drug for the Treatment of Brain Cancers. International Journal of Molecular Sciences 2023, 24, 1334. [Google Scholar] [CrossRef]
- Nygren, P.; Larsson, R. Drug repositioning from bench to bedside: tumour remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta oncologica 2014, 53, 427–428. [Google Scholar] [CrossRef]
- Dobrosotskaya, I.Y.; Hammer, G.D.; Schteingart, D.E.; Maturen, K.E.; Worden, F.P. Mebendazole monotherapy and long-term disease control in metastatic adrenocortical carcinoma. Endocrine practice 2011, 17, e59–e62. [Google Scholar] [CrossRef] [PubMed]
- Chiang, R.S.; Syed, A.B.; Wright, J.L.; Montgomery, B.; Srinlavs, S. Fenbendazole enhancing anti-tumor effect: a case series. Clin. Oncol. Case Rep 2021, 4, 2–5. [Google Scholar]
- Agrawal, S.; Vamadevan, P.; Mazibuko, N.; Bannister, R.; Swery, R.; Wilson, S.; Edwards, S. A new method for ethical and efficient evidence generation for off-label medication use in oncology (a case study in glioblastoma). Frontiers in Pharmacology 2019, 681. [Google Scholar] [CrossRef]
- Dach, J. Cracking Cancer Toolkit: Using Repurposed Drugs for Cancer Treatment; Amazon Digital Services LLC - KDP Print US, 2020. [Google Scholar]
- Williamson, T.; Bai, R.-Y.; Staedtke, V.; Huso, D.; Riggins, G.J. Mebendazole and a non-steroidal anti-inflammatory combine to reduce tumor initiation in a colon cancer preclinical model. Oncotarget 2016, 7, 68571. [Google Scholar] [CrossRef]
- Nabavi, S.F.; Bilotto, S.; Russo, G.L.; Orhan, I.E.; Habtemariam, S.; Daglia, M.; Devi, K.P.; Loizzo, M.R.; Tundis, R.; Nabavi, S.M. Omega-3 polyunsaturated fatty acids and cancer: lessons learned from clinical trials. Cancer and Metastasis Reviews 2015, 34, 359–380. [Google Scholar] [CrossRef]
- Cockbain, A.J.; Toogood, G.J.; Hull, M.A. Omega-3 polyunsaturated fatty acids for the treatment and prevention of colorectal cancer. Gut 2012, 61, 135–149. [Google Scholar] [CrossRef]
- Corsetto, P.A.; Montorfano, G.; Zava, S.; Jovenitti, I.E.; Cremona, A.; Berra, B.; Rizzo, A.M. Effects of n-3 PUFAs on breast cancer cells through their incorporation in plasma membrane. Lipids in health and disease 2011, 10, 1–16. [Google Scholar] [CrossRef] [PubMed]
- De Carlo, F.; Witte, T.R.; Hardman, W.E.; Claudio, P.P. Omega-3 eicosapentaenoic acid decreases CD133 colon cancer stem-like cell marker expression while increasing sensitivity to chemotherapy. PLoS One 2013, 8, e69760. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Wang, Q.; Zhao, J.; Dong, L.; Ge, Y.; Hou, L.; Liu, Y.; Zheng, Z. Docosahexaenoic acid inhibited the Wnt/β-catenin pathway and suppressed breast cancer cells in vitro and in vivo. The Journal of nutritional biochemistry 2014, 25, 104–110. [Google Scholar] [CrossRef]
- Vasudevan, A.; Yu, Y.; Banerjee, S.; Woods, J.; Farhana, L.; Rajendra, S.G.; Patel, A.; Dyson, G.; Levi, E.; Maddipati, K.R. Omega-3 fatty acid is a potential preventive agent for recurrent colon cancer. Cancer Prevention Research 2014, 7, 1138–1148. [Google Scholar] [CrossRef]
- Aucoin, M.; Cooley, K.; Knee, C.; Fritz, H.; Balneaves, L.G.; Breau, R.; Fergusson, D.; Skidmore, B.; Wong, R.; Seely, D. Fish-derived omega-3 fatty acids and prostate cancer: a systematic review. Integrative cancer therapies 2017, 16, 32–62. [Google Scholar] [CrossRef]
- Zheng, J.-S.; Hu, X.-J.; Zhao, Y.-M.; Yang, J.; Li, D. Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. Bmj 2013, 346, f3706. [Google Scholar] [CrossRef]
- Pot, G.K.; Geelen, A.; van Heijningen, E.M.B.; Siezen, C.L.E.; van Kranen, H.J.; Kampman, E. Opposing associations of serum n-3 and n-6 polyunsaturated fatty acids with colorectal adenoma risk: An endoscopy-based case–control study. International journal of cancer 2008, 123, 1974–1977. [Google Scholar] [CrossRef]
- Brasky, T.M.; Lampe, J.W.; Potter, J.D.; Patterson, R.E.; White, E. Specialty supplements and breast cancer risk in the VITamins And Lifestyle (VITAL) Cohort. Cancer epidemiology, biomarkers & prevention 2010, 19, 1696–1708. [Google Scholar]
- Murphy, R.A.; Mourtzakis, M.; Chu, Q.S.C.; Baracos, V.E.; Reiman, T.; Mazurak, V.C. Supplementation with fish oil increases first-line chemotherapy efficacy in patients with advanced nonsmall cell lung cancer. Cancer 2011, 117, 3774–3780. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Xu, X.-T.; Tian, M.-X.; Dai, Z. N-3 polyunsaterated fatty acids improve quality of life and survival, but not body weight in cancer cachexia: A systematic review and meta-analysis of controlled trials. Nutrition Research 2022. [Google Scholar] [CrossRef] [PubMed]
- West, N.J.; Clark, S.K.; Phillips, R.K.S.; Hutchinson, J.M.; Leicester, R.J.; Belluzzi, A.; Hull, M.A. Eicosapentaenoic acid reduces rectal polyp number and size in familial adenomatous polyposis. Gut 2010, 59, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Bougnoux, P.; Hajjaji, N.; Ferrasson, M.N.; Giraudeau, B.; Couet, C.; Le Floch, O. Improving outcome of chemotherapy of metastatic breast cancer by docosahexaenoic acid: a phase II trial. British journal of cancer 2009, 101, 1978–1985. [Google Scholar] [CrossRef] [PubMed]
- Xiong, R.-G.; Huang, S.-Y.; Wu, S.-X.; Zhou, D.-D.; Yang, Z.-J.; Saimaiti, A.; Zhao, C.-N.; Shang, A.O.; Zhang, Y.-J.; Gan, R.-Y. Anticancer effects and mechanisms of berberine from medicinal herbs: An update review. Molecules 2022, 27, 4523. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Zhang, F.; Zhao, Y.; Shao, D.; Zheng, X.; Chen, Y.; He, K.; Li, J.; Chen, L. Berberine enhances chemosensitivity and induces apoptosis through dose-orchestrated AMPK signaling in breast cancer. Journal of Cancer 2017, 8, 1679. [Google Scholar] [CrossRef] [PubMed]
- Kou, Y.; Tong, B.; Wu, W.; Liao, X.; Zhao, M. Berberine improves chemo-sensitivity to cisplatin by enhancing cell apoptosis and repressing PI3K/AKT/mTOR signaling pathway in gastric cancer. Frontiers in pharmacology 2020, 11, 616251. [Google Scholar] [CrossRef]
- Zhu, C.; Li, J.; Hua, Y.; Wang, J.; Wang, K.; Sun, J. Berberine inhibits the expression of SCT through miR-214-3p stimulation in breast cancer cells. Evidence-Based Complementary and Alternative Medicine 2020, 2020. [Google Scholar] [CrossRef]
- Li, S.; Wang, N.; Tan, H.Y.; Chueng, F.; Zhang, Z.J.; Yuen, M.F.; Feng, Y. Modulation of gut microbiota mediates berberine-induced expansion of immuno-suppressive cells to against alcoholic liver disease. Clinical and Translational Medicine 2020, 10, e112. [Google Scholar] [CrossRef]
- You, H.-Y.; Xie, X.-M.; Zhang, W.-J.; Zhu, H.-L.; Jiang, F.-Z. Berberine modulates cisplatin sensitivity of human gastric cancer cells by upregulation of miR-203. In Vitro Cellular & Developmental Biology-Animal 2016, 52, 857–863. [Google Scholar]
- Chen, Y.-X.; Gao, Q.-Y.; Zou, T.-H.; Wang, B.-M.; Liu, S.-D.; Sheng, J.-Q.; Ren, J.-L.; Zou, X.-P.; Liu, Z.-J.; Song, Y.-Y. Berberine versus placebo for the prevention of recurrence of colorectal adenoma: a multicentre, double-blinded, randomised controlled study. The Lancet Gastroenterology & Hepatology 2020, 5, 267–275. [Google Scholar]
- Cruz, P.M.R.; Mo, H.; McConathy, W.J.; Sabnis, N.; Lacko, A.G. The role of cholesterol metabolism and cholesterol transport in carcinogenesis: a review of scientific findings, relevant to future cancer therapeutics. Frontiers in pharmacology 2013, 4, 119. [Google Scholar] [CrossRef] [PubMed]
- Parrales, A.; Thoenen, E.; Iwakuma, T. The interplay between mutant p53 and the mevalonate pathway. Cell Death & Differentiation 2018, 25, 460–470. [Google Scholar]
- Borgquist, S.; Bjarnadottir, O.; Kimbung, S.; Ahern, T.P. Statins: a role in breast cancer therapy? Journal of internal medicine 2018, 284, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.Y.-H.; Lee, F.-P.; Chang, C.-L.; Wu, S.-Y. Statin-based palliative therapy for hepatocellular carcinoma. Medicine 2015, 94. [Google Scholar] [CrossRef]
- Zhong, S.; Zhang, X.; Chen, L.; Ma, T.; Tang, J.; Zhao, J. Statin use and mortality in cancer patients: Systematic review and meta-analysis of observational studies. Cancer Treat Rev 2015, 41, 554–567. [Google Scholar] [CrossRef]
- Lin, J.J.; Ezer, N.; Sigel, K.; Mhango, G.; Wisnivesky, J.P. The effect of statins on survival in patients with stage IV lung cancer. Lung cancer 2016, 99, 137–142. [Google Scholar] [CrossRef]
- Manthravadi, S.; Shrestha, A.; Madhusudhana, S. Impact of statin use on cancer recurrence and mortality in breast cancer: A systematic review and meta-analysis. International journal of cancer 2016, 139, 1281–1288. [Google Scholar] [CrossRef]
- Demierre, M.-F.; Higgins, P.D.R.; Gruber, S.B.; Hawk, E.; Lippman, S.M. Statins and cancer prevention. Nat Rev Cancer 2005, 5, 930–942. [Google Scholar] [CrossRef]
- Lu, C.; Li, X.; Ren, Y.; Zhang, X. Disulfiram: a novel repurposed drug for cancer therapy. Cancer Chemotherapy and Pharmacology 2021, 87, 159–172. [Google Scholar] [CrossRef]
- Kang, X.; Jadhav, S.; Annaji, M.; Huang, C.-H.; Amin, R.; Shen, J.; Ashby Jr, C.R.; Tiwari, A.K.; Babu, R.J.; Chen, P. Advancing Cancer Therapy with Copper/Disulfiram Nanomedicines and Drug Delivery Systems. Pharmaceutics 2023, 15, 1567. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Wang, Z.; Brown, S.; Kannappan, V.; Tawari, P.E.; Jiang, W.; Irache, J.M.; Tang, J.Z.; Britland, S.; Armesilla, A.L. Liposome encapsulated Disulfiram inhibits NFκB pathway and targets breast cancer stem cells in vitro and in vivo. Oncotarget 2014, 5, 7471. [Google Scholar] [CrossRef] [PubMed]
- Yip, N.C.; Fombon, I.S.; Liu, P.; Brown, S.; Kannappan, V.; Armesilla, A.L.; Xu, B.; Cassidy, J.; Darling, J.L.; Wang, W. Disulfiram modulated ROS–MAPK and NFκB pathways and targeted breast cancer cells with cancer stem cell-like properties. British journal of cancer 2011, 104, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.M.; Go, Y.Y.; Shin, S.H.; Cho, J.-G.; Woo, J.-S.; Song, J.-J. Anti-cancer effects of disulfiram in head and neck squamous cell carcinoma via autophagic cell death. PLoS One 2018, 13, e0203069. [Google Scholar] [CrossRef]
- Triscott, J.; Lee, C.; Hu, K.; Fotovati, A.; Berns, R.; Pambid, M.; Luk, M.; Kast, R.E.; Kong, E.; Toyota, E. Disulfiram, a drug widely used to control alcoholism, suppresses self-renewal of glioblastoma and overrides resistance to temozolomide. Oncotarget 2012, 3, 1112. [Google Scholar] [CrossRef]
- Dufour, P.; Lang, J.M.; Giron, C.; Duclos, B.; Haehnel, P.; Jaeck, D.; Jung, J.M.; Oberling, F. Sodium ditiocarb as adjuvant immunotherapy for high risk breast cancer: a randomized study. Biotherapy 1993, 6, 9–12. [Google Scholar] [CrossRef]
- Huang, J.; Campian, J.L.; Gujar, A.D.; Tran, D.D.; Lockhart, A.C.; DeWees, T.A.; Tsien, C.I.; Kim, A.H. A phase I study to repurpose disulfiram in combination with temozolomide to treat newly diagnosed glioblastoma after chemoradiotherapy. Journal of neuro-oncology 2016, 128, 259–266. [Google Scholar] [CrossRef]
- Nechushtan, H.; Hamamreh, Y.; Nidal, S.; Gotfried, M.; Baron, A.; Shalev, Y.I.; Nisman, B.; Peretz, T.; Peylan-Ramu, N. A phase IIb trial assessing the addition of disulfiram to chemotherapy for the treatment of metastatic non-small cell lung cancer. The oncologist 2015, 20, 366–367. [Google Scholar] [CrossRef]
- Huang, J.; Campian, J.L.; Gujar, A.D.; Tsien, C.; Ansstas, G.; Tran, D.D.; DeWees, T.A.; Lockhart, A.C.; Kim, A.H. Final results of a phase I dose-escalation, dose-expansion study of adding disulfiram with or without copper to adjuvant temozolomide for newly diagnosed glioblastoma. Journal of neuro-oncology 2018, 138, 105–111. [Google Scholar] [CrossRef]
- Ghosh, A.K.; Hirasawa, N.; Ohuchi, K. Enhancement by histamine of vascular endothelial growth factor production in granulation tissue via H2 receptors. British journal of pharmacology 2001, 134, 1419. [Google Scholar] [CrossRef]
- Ibrahim, S.S.A.; El-Aal, S.A.A.; Reda, A.M.; Achy, S.E.; Shahine, Y. Anti-neoplastic action of Cimetidine/Vitamin C on histamine and the PI3K/AKT/mTOR pathway in Ehrlich breast cancer. Scientific Reports 2022, 12, 11514. [Google Scholar] [CrossRef] [PubMed]
- Deva, S.; Jameson, M. Histamine type 2 receptor antagonists as adjuvant treatment for resected colorectal cancer. Cochrane Database of Systematic Reviews 2012. [Google Scholar] [CrossRef] [PubMed]
- Flodgren, P.; Borgström, S.; Jönsson, P.E.; Lindström, C.; Sjögren, H.O. Metastatic malignant melanoma: Regression induced by combined treatment with interferon [HuIFN-α (Le)] and cimetidine. International journal of cancer 1983, 32, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Tønnesen, H.; Bülow, S.; Fischerman, K.; Hjortrup, A.; Pedersen, V.M.; Svendsen, L.B.; Knigge, U.; Damm, P.; Hesselfeldt, P.; Pedersen, I.K. Effect of cimetidine on survival after gastric cancer. The Lancet 1988, 332, 990–992. [Google Scholar] [CrossRef]
- Florence, L.; Syril, J.; Isabelle, C.; Jean-Fran, G.; Francis, D.; Jacques, B. Combined cimetidine and temozolomide, compared with temozolomide alone: significant increases in survival in nud mice bearing U373 human glioblastoma multiforme orthotopic xenografts. J Neurosurg 2005, 102, 706–714. [Google Scholar]
- Thronicke, A.; Schad, F.; Debus, M.; Grabowski, J.; Soldner, G. Viscum album L. therapy in oncology: An update on current evidence. Complementary Medicine Research 2022, 29, 362–368. [Google Scholar] [CrossRef]
- Harmsma, M.; Grommé, M.; Ummelen, M.; Dignef, W.; Tusenius, K.J.; Ramaekers, F. Differential effects of Viscum album extract Iscador® Qu on cell cycle progression and apoptosis in cancer cells. International Journal of Oncology 2004, 25, 1521–1529. [Google Scholar] [CrossRef]
- Huber, R.; Rostock, M.; Goedl, R.; Ludtke, R.; Urech, K.; Buck, S.; Klein, R. Mistletoe treatment induces GM-CSF-and IL-5 production by PBMC and increases blood granulocyte-and eosinophil counts: a placebo controlled randomized study in healthy subjects. European journal of medical research 2005, 10, 411. [Google Scholar]
- Loef, M.; Walach, H. Quality of life in cancer patients treated with mistletoe: a systematic review and meta-analysis. BMC Complementary Medicine and Therapies 2020, 20, 1–14. [Google Scholar] [CrossRef]
- Oei, S.L.; Thronicke, A.; Schad, F. Mistletoe and immunomodulation: insights and implications for anticancer therapies. Evidence-Based Complementary and Alternative Medicine 2019, 2019. [Google Scholar] [CrossRef]
- Ben-Arye, E.; Lavie, O.; Samuels, N.; Khamaisie, H.; Schiff, E.; Raz, O.G.; Mahajna, J. Safety of herbal medicine use during chemotherapy in patients with ovarian cancer: a “bedside-to-bench” approach. Medical Oncology 2017, 34, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.-S.; Chun, S.-Y.; Kim, M.-K.; Nan, H.-Y.; Lee, C.; Kim, S. Mistletoe extract targets the STAT3-FOXM1 pathway to induce apoptosis and inhibits metastasis in breast cancer cells. The American Journal of Chinese Medicine 2021, 49, 487–504. [Google Scholar] [CrossRef] [PubMed]
- Horneber, M.; van Ackeren, G.; Linde, K.; Rostock, M. Mistletoe therapy in oncology. Cochrane Database of Systematic Reviews 2008. [Google Scholar]
- Loef, M.; Walach, H. Survival of Cancer Patients Treated with Non-Fermented Mistletoe Extract: A Systematic Review and Meta-Analysis. Integrative Cancer Therapies 2022, 21, 15347354221133561. [Google Scholar] [CrossRef]
- Paller, C.J.; Wang, L.; Fu, W.; Kumar, R.; Durham, J.N.; Azad, N.S.; Laheru, D.A.; Browner, I.; Kachhap, S.K.; Boyapati, K. Phase I trial of intravenous mistletoe extract in advanced cancer. Cancer Research Communications 2023, 3, 338–346. [Google Scholar] [CrossRef]
- Kienle, G.S.; Mussler, M.; Fuchs, D.; Kiene, H. Intravenous mistletoe treatment in integrative cancer care: a qualitative study exploring the procedures, concepts, and observations of expert doctors. Evidence-Based Complementary and Alternative Medicine 2016, 2016. [Google Scholar] [CrossRef]
- Dutta, R.; Khalil, R.; Green, R.; Mohapatra, S.S.; Mohapatra, S. Withania somnifera (Ashwagandha) and withaferin A: Potential in integrative oncology. International journal of molecular sciences 2019, 20, 5310. [Google Scholar] [CrossRef]
- Mikulska, P.; Malinowska, M.; Ignacyk, M.; Szustowski, P.; Nowak, J.; Pesta, K.; Szeląg, M.; Szklanny, D.; Judasz, E.; Kaczmarek, G. Ashwagandha (Withania somnifera)—Current research on the health-promoting activities: a narrative review. Pharmaceutics 2023, 15, 1057. [Google Scholar] [CrossRef]
- Nagy, Z.; Cheung, B.B.; Tsang, W.; Tan, O.; Herath, M.; Ciampa, O.C.; Shadma, F.; Carter, D.R.; Marshall, G.M. Withaferin A activates TRIM16 for its anti-cancer activity in melanoma. Scientific reports 2020, 10, 19724. [Google Scholar] [CrossRef]
- Jawarneh, S.; Talib, W.H. Combination of ashwagandha water extract and intermittent fasting as a therapy to overcome cisplatin resistance in breast cancer: an in vitro and in vivo study. Frontiers in Nutrition 2022, 9, 863619. [Google Scholar] [CrossRef]
- Tang, Q.; Ren, L.; Liu, J.; Li, W.; Zheng, X.; Wang, J.; Du, G. Withaferin A triggers G2/M arrest and intrinsic apoptosis in glioblastoma cells via ATF4-ATF3-CHOP axis. Cell Proliferation 2020, 53, e12706. [Google Scholar] [CrossRef]
- Widodo, N.; Priyandoko, D.; Shah, N.; Wadhwa, R.; Kaul, S.C. Selective killing of cancer cells by Ashwagandha leaf extract and its component Withanone involves ROS signaling. PloS one 2010, 5, e13536. [Google Scholar] [CrossRef]
- Choi, B.Y.; Kim, B.-W. Withaferin-A inhibits colon cancer cell growth by blocking STAT3 transcriptional activity. Journal of cancer prevention 2015, 20, 185. [Google Scholar] [CrossRef]
- Koduru, S.; Kumar, R.; Srinivasan, S.; Evers, M.B.; Damodaran, C. Notch-1 inhibition by Withaferin-A: a therapeutic target against colon carcinogenesis. Molecular cancer therapeutics 2010, 9, 202–210. [Google Scholar] [CrossRef]
- Sikandan, A.; Shinomiya, T.; Nagahara, Y. Ashwagandha root extract exerts anti-inflammatory effects in HaCaT cells by inhibiting the MAPK/NF-κB pathways and by regulating cytokines. International journal of molecular medicine 2018, 42, 425–434. [Google Scholar] [CrossRef]
- Biswal, B.M.; Sulaiman, S.A.; Ismail, H.C.; Zakaria, H.; Musa, K.I. Effect of Withania somnifera (Ashwagandha) on the development of chemotherapy-induced fatigue and quality of life in breast cancer patients. Integrative cancer therapies 2013, 12, 312–322. [Google Scholar] [CrossRef]
- Chen, L.; Liu, Y.; Becher, A.; Diepold, K.; Schmid, E.; Fehn, A.; Brunner, C.; Rouhi, A.; Chiosis, G.; Cronauer, M. Sildenafil triggers tumor lethality through altered expression of HSP90 and degradation of PKD2. Carcinogenesis 2020, 41, 1421–1431. [Google Scholar] [CrossRef]
- Chhonker, S.K.; Rawat, D.; Koiri, R.K. Repurposing PDE5 inhibitor tadalafil and sildenafil as anticancer agent against hepatocellular carcinoma via targeting key events of glucose metabolism and multidrug resistance. Journal of Biochemical and Molecular Toxicology 2022, 36, e23100. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Burgos, M.; Losada-Garcia, A.; Cruz-Hernández, C.D.; Cortés-Ramírez, S.A.; Camacho-Arroyo, I.; Gonzalez-Covarrubias, V.; Morales-Pacheco, M.; Trujillo-Bornios, S.I.; Rodríguez-Dorantes, M. New approaches in oncology for repositioning drugs: the case of PDE5 inhibitor sildenafil. Frontiers in Oncology 2021, 11, 627229. [Google Scholar] [CrossRef] [PubMed]
- Booth, L.; Roberts, J.L.; Cruickshanks, N.; Conley, A.; Durrant, D.E.; Das, A.; Fisher, P.B.; Kukreja, R.C.; Grant, S.; Poklepovic, A. Phosphodiesterase 5 inhibitors enhance chemotherapy killing in gastrointestinal/genitourinary cancer cells. Molecular Pharmacology 2014, 85, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Domvri, K.; Zarogoulidis, K.; Zogas, N.; Zarogoulidis, P.; Petanidis, S.; Porpodis, K.; Kioseoglou, E.; Hohenforst-Schmidt, W. Potential synergistic effect of phosphodiesterase inhibitors with chemotherapy in lung cancer. Journal of Cancer 2017, 8, 3648. [Google Scholar] [CrossRef]
- Tai, L.-H.; Alkayyal, A.A.; Leslie, A.L.; Sahi, S.; Bennett, S.; Tanese de Souza, C.; Baxter, K.; Angka, L.; Xu, R.; Kennedy, M.A. Phosphodiesterase-5 inhibition reduces postoperative metastatic disease by targeting surgery-induced myeloid derived suppressor cell-dependent inhibition of Natural Killer cell cytotoxicity. Oncoimmunology 2018, 7, e1431082. [Google Scholar] [CrossRef] [PubMed]
- Serafini, P.; Meckel, K.; Kelso, M.; Noonan, K.; Califano, J.; Koch, W.; Dolcetti, L.; Bronte, V.; Borrello, I. Phosphodiesterase-5 inhibition augments endogenous antitumor immunity by reducing myeloid-derived suppressor cell function. The Journal of experimental medicine 2006, 203, 2691–2702. [Google Scholar] [CrossRef] [PubMed]
- Sutton, S.S.; Magagnoli, J.; Cummings, T.H.; Hardin, J.W. The association between phosphodiesterase-5 inhibitors and colorectal cancer in a national cohort of patients. Clinical and translational gastroenterology 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Weed, D.T.; Vella, J.L.; Reis, I.M.; De la Fuente, A.C.; Gomez, C.; Sargi, Z.; Nazarian, R.; Califano, J.; Borrello, I.; Serafini, P. Tadalafil reduces myeloid-derived suppressor cells and regulatory T cells and promotes tumor immunity in patients with head and neck squamous cell carcinoma. Clinical cancer research 2015, 21, 39–48. [Google Scholar] [CrossRef]
- Califano, J.A.; Khan, Z.; Noonan, K.A.; Rudraraju, L.; Zhang, Z.; Wang, H.; Goodman, S.; Gourin, C.G.; Ha, P.K.; Fakhry, C. Tadalafil augments tumor specific immunity in patients with head and neck squamous cell carcinoma. Clinical cancer research 2015, 21, 30–38. [Google Scholar] [CrossRef]
- Huang, W.; Sundquist, J.; Sundquist, K.; Ji, J. Phosphodiesterase-5 inhibitors use and risk for mortality and metastases among male patients with colorectal cancer. Nature Communications 2020, 11, 3191. [Google Scholar] [CrossRef]
- Danley, K.T.; Tan, A.; Catalona, W.J.; Leikin, R.; Helenowski, I.; Jovanovic, B.; Gurley, M.; Kuzel, T.M. The association of phosphodiesterase-5 inhibitors with the biochemical recurrence-free and overall survival of patients with prostate cancer following radical prostatectomy. 2022, 57-e51. [Google Scholar] [CrossRef]
- Tsubamoto, H.; Ueda, T.; Inoue, K.; Sakata, K.; Shibahara, H.; Sonoda, T. Repurposing itraconazole as an anticancer agent. Oncology letters 2017, 14, 1240–1246. [Google Scholar] [CrossRef]
- Ali, T.; Rahman, S.U.; Hao, Q.; Li, W.; Liu, Z.; Ali Shah, F.; Murtaza, I.; Zhang, Z.; Yang, X.; Liu, G. Melatonin prevents neuroinflammation and relieves depression by attenuating autophagy impairment through FOXO3a regulation. Journal of pineal research 2020, 69, e12667. [Google Scholar] [CrossRef]
- Pounds, R.; Leonard, S.; Dawson, C.; Kehoe, S. Repurposing itraconazole for the treatment of cancer. Oncology letters 2017, 14, 2587–2597. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.J.; Kim, J.; Spaunhurst, K.; Montoya, J.; Khodosh, R.; Chandra, K.; Fu, T.; Gilliam, A.; Molgó Novell, M. Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. 2014. [Google Scholar] [CrossRef]
- Kim, J.; Tang, J.Y.; Gong, R.; Kim, J.; Lee, J.J.; Clemons, K.V.; Chong, C.R.; Chang, K.S.; Fereshteh, M.; Gardner, D. Itraconazole, a commonly used antifungal that inhibits Hedgehog pathway activity and cancer growth. Cancer cell 2010, 17, 388–399. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Dong, X.; Liu, Y.; Ni, B.; Sai, N.; You, L.; Sun, M.; Yao, Y.; Qu, C.; Yin, X. Itraconazole exerts anti-liver cancer potential through the Wnt, PI3K/AKT/mTOR, and ROS pathways. Biomedicine & Pharmacotherapy 2020, 131, 110661. [Google Scholar]
- Antonarakis, E.S.; Heath, E.I.; Smith, D.C.; Rathkopf, D.; Blackford, A.L.; Danila, D.C.; King, S.; Frost, A.; Ajiboye, A.S.; Zhao, M. Repurposing itraconazole as a treatment for advanced prostate cancer: a noncomparative randomized phase II trial in men with metastatic castration-resistant prostate cancer. The oncologist 2013, 18, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhang, W. Itraconazole alters the stem cell characteristics of A549 and NCI-H460 human lung cancer cells by suppressing Wnt signaling. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 2019, 25, 9509. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.R.; Xu, J.; Lu, J.; Bhat, S.; Sullivan Jr, D.J.; Liu, J.O. Inhibition of angiogenesis by the antifungal drug itraconazole. ACS chemical biology 2007, 2, 263–270. [Google Scholar] [CrossRef]
- Mamtani, R.; Yang, Y.-X.; Scott, F.I.; Lewis, J.D.; Boursi, B. Association of itraconazole, a hedgehog inhibitor, and bladder cancer. The Journal of urology 2016, 196, 343–348. [Google Scholar] [CrossRef]
- Marastoni, S.; Madariaga, A.; Pesic, A.; Nair, S.N.; Li, Z.J.; Shalev, Z.; Ketela, T.; Colombo, I.; Mandilaras, V.; Cabanero, M. Repurposing itraconazole and hydroxychloroquine to target lysosomal homeostasis in epithelial ovarian cancer. Cancer Research Communications 2022, 2, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Nacev, B.A.; Grassi, P.; Dell, A.; Haslam, S.M.; Liu, J.O. The antifungal drug itraconazole inhibits vascular endothelial growth factor receptor 2 (VEGFR2) glycosylation, trafficking, and signaling in endothelial cells. Journal of Biological Chemistry 2011, 286, 44045–44056. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Bhagwath, A.S.; Ramzan, Z.; Williams, T.A.; Subramaniyan, I.; Edpuganti, V.; Kallem, R.R.; Dunbar, K.B.; Ding, P.; Gong, K. Itraconazole exerts its antitumor effect in esophageal cancer by suppressing the HER2/AKT signaling pathway. Molecular cancer therapeutics 2021, 20, 1904–1915. [Google Scholar] [CrossRef] [PubMed]
- Tsubamoto, H.; Sonoda, T.; Yamasaki, M.; Inoue, K. Impact of combination chemotherapy with itraconazole on survival of patients with refractory ovarian cancer. Anticancer Research 2014, 34, 2481–2487. [Google Scholar]
- Lan, K.; Yan, R.; Zhu, K.; Li, W.; Xu, Z.; Dang, C.; Li, K. Itraconazole inhibits the proliferation of gastric cancer cells in vitro and improves patient survival. Oncology Letters 2018, 16, 3651–3657. [Google Scholar] [CrossRef] [PubMed]
- Rudin, C.M.; Brahmer, J.R.; Juergens, R.A.; Hann, C.L.; Ettinger, D.S.; Sebree, R.; Smith, R.; Aftab, B.T.; Huang, P.; Liu, J.O. Phase 2 study of pemetrexed and itraconazole as second-line therapy for metastatic nonsquamous non–small-cell lung cancer. Journal of Thoracic Oncology 2013, 8, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.-W.; Chou, Y.-M.; Li, C.-L.; Liao, E.-C.; Huang, H.-S.; Yin, C.-H.; Chen, C.-L.; Yu, S.-J. Itraconazole improves survival outcomes in patients with colon cancer by inducing autophagic cell death and inhibiting transketolase expression. Oncology Letters 2021, 22, 1–11. [Google Scholar] [CrossRef]
- Tsubamoto, H.; Sonoda, T.; Ikuta, S.; Tani, S.; Inoue, K.; Yamanaka, N. Combination chemotherapy with itraconazole for treating metastatic pancreatic cancer in the second-line or additional setting. Anticancer Research 2015, 35, 4191–4196. [Google Scholar]
- Tsubamoto, H.; Sonoda, T.; Inoue, K. Impact of itraconazole on the survival of heavily pre-treated patients with triple-negative breast cancer. Anticancer Research 2014, 34, 3839–3844. [Google Scholar]
- Gerber, D.E.; Putnam, W.C.; Fattah, F.J.; Kernstine, K.H.; Brekken, R.A.; Pedrosa, I.; Skelton, R.; Saltarski, J.M.; Lenkinski, R.E.; Leff, R.D. Concentration-dependent Early Antivascular and Antitumor Effects of Itraconazole in Non–Small Cell Lung Cancer. Clinical Cancer Research 2021, 26, 6017–6027. [Google Scholar] [CrossRef]
- Tsubamoto, H.; Sonoda, T.; Ikuta, S.; Tani, S.; Inoue, K.; Yamanaka, N. Impact of itraconazole after first-line chemotherapy on survival of patients with metastatic biliary tract cancer. Anticancer Research 2015, 35, 4923–4927. [Google Scholar] [CrossRef]
- Ringshausen, I.; Feuerstacke, Y.; Krainz, P.; den Hollander, J.; Hermann, K.; Buck, A.; Peschel, C.; Meyer zum Bueschenfelde, C. Antifungal therapy with itraconazole impairs the anti-lymphoma effects of rituximab by inhibiting recruitment of CD20 to cell surface lipid rafts. Cancer Research 2010, 70, 4292–4296. [Google Scholar] [CrossRef]
- Yang, B.R.; Seong, J.-M.; Choi, N.-K.; Shin, J.-Y.; Lee, J.; Kim, Y.-J.; Kim, M.-S.; Park, S.; Song, H.J.; Park, B.-J. Co-medication of statins with contraindicated drugs. PLoS One 2015, 10, e0125180. [Google Scholar] [CrossRef]
- Kinzel, A.; Ambrogi, M.; Varshaver, M.; Kirson, E.D. Tumor treating fields for glioblastoma treatment: Patient satisfaction and compliance with the second-generation Optune® system. Clinical Medicine Insights: Oncology 2019, 13, 1179554918825449. [Google Scholar] [CrossRef]
- Moser, J.C.; Salvador, E.; Deniz, K.; Swanson, K.; Tuszynski, J.; Carlson, K.W.; Karanam, N.K.; Patel, C.B.; Story, M.; Lou, E. The mechanisms of action of Tumor Treating Fields. Cancer research 2022, 82, 3650–3658. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.M.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K. Effect of tumor-treating fields plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a randomized clinical trial. Jama 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Ghiaseddin, A.P.; Shin, D.; Melnick, K.; Tran, D.D. Tumor treating fields in the management of patients with malignant gliomas. Current Treatment Options in Oncology 2020, 21, 1–19. [Google Scholar] [CrossRef]
- National Comprehensive Cancer, N. NCCN clinical practice guidelines in oncology. Availabe online: https://www.nccn.org/login?returnURL=https://www.nccn.org/professionals/physician_gls/pdf/ (accessed on.
- Yanovsky, R.L.; Bartenstein, D.W.; Rogers, G.S.; Isakoff, S.J.; Chen, S.T. Photodynamic therapy for solid tumors: A review of the literature. Photodermatology, photoimmunology & photomedicine 2019, 35, 295–303. [Google Scholar]
- dos Santos, A.F.; de Almeida, D.R.Q.; Terra, L.F.; Baptista, M.S.; Labriola, L. Photodynamic therapy in cancer treatment-an update review. J. Cancer Metastasis Treat 2019, 5, 10–20517. [Google Scholar] [CrossRef]
- Reiter, R.J.; Ma, Q.; Sharma, R. Melatonin in mitochondria: mitigating clear and present dangers. Physiology 2020. [Google Scholar] [CrossRef]
- Zimmerman, S.; Reiter, R.J. Melatonin and the optics of the human body. Melatonin Research 2019, 2, 138–160. [Google Scholar] [CrossRef]
- Hobday, R.A.; Cason, J.W. The open-air treatment of pandemic influenza. American journal of public health 2009, 99, S236–S242. [Google Scholar] [CrossRef]
- Lindqvist, P.G.; Epstein, E.; Landin-Olsson, M.; Ingvar, C.; Nielsen, K.; Stenbeck, M.; Olsson, H. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. Journal of internal medicine 2014, 276, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.M.; Nathan, T.R.; Lees, W.R.; Mosse, C.A.; Freeman, A.; Emberton, M.; Bown, S.G. Photodynamic therapy using meso tetra hydroxy phenyl chlorin (mTHPC) in early prostate cancer. Lasers in Surgery and Medicine: The Official Journal of the American Society for Laser Medicine and Surgery 2006, 38, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Kostron, H. Photodynamic diagnosis and therapy and the brain. Photodynamic Therapy: Methods and Protocols 2010, 261–280. [Google Scholar]
- Windahl, T.; Andersson, S.-O.; Lofgren, L. Photodynamic therapy of localised prostatic cancer. The Lancet 1990, 336, 1139. [Google Scholar] [CrossRef]
- Bredell, M.G.; Besic, E.; Maake, C.; Walt, H. The application and challenges of clinical PD–PDT in the head and neck region: A short review. Journal of Photochemistry and Photobiology B: Biology 2010, 101, 185–190. [Google Scholar] [CrossRef]
- Moen, I.; Stuhr, L.E.B. Hyperbaric oxygen therapy and cancer—a review. Targeted oncology 2012, 7, 233–242. [Google Scholar] [CrossRef]
- Raa, A.; Stansberg, C.; Steen, V.M.; Bjerkvig, R.; Reed, R.K.; Stuhr, L.E.B. Hyperoxia retards growth and induces apoptosis and loss of glands and blood vessels in DMBA-induced rat mammary tumors. BMC cancer 2007, 7, 1–10. [Google Scholar] [CrossRef]
- Stuhr, L.E.B.; Raa, A.; Øyan, A.M.; Kalland, K.H.; Sakariassen, P.O.; Petersen, K.; Bjerkvig, R.; Reed, R.K. Hyperoxia retards growth and induces apoptosis, changes in vascular density and gene expression in transplanted gliomas in nude rats. Journal of neuro-oncology 2007, 85, 191–202. [Google Scholar] [CrossRef]
- Gore, A.; Muralidhar, M.; Espey, M.G.; Degenhardt, K.; Mantell, L.L. Hyperoxia sensing: from molecular mechanisms to significance in disease. Journal of immunotoxicology 2010, 7, 239–254. [Google Scholar] [CrossRef]
- Bennett, M.H.; Feldmeier, J.; Smee, R.; Milross, C. Hyperbaric oxygenation for tumour sensitisation to radiotherapy. Cochrane Database of Systematic Reviews 2018. [Google Scholar] [CrossRef]
- Mohammadifard, N.; Haghighatdoost, F.; Rahimlou, M.; Rodrigues, A.P.S.; Gaskarei, M.K.; Okhovat, P.; de Oliveira, C.; Silveira, E.A.; Sarrafzadegan, N. The Effect of Ketogenic Diet on Shared Risk Factors of Cardiovascular Disease and Cancer. Nutrients 2022, 14, 3499. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Kumari, S.; Singh, D. Insights into the Cellular Interactions and Molecular Mechanisms of Ketogenic Diet for Comprehensive Management of Epilepsy. Current Neuropharmacology 2022, 20, 2034. [Google Scholar]
- Talib, W.H.; Mahmod, A.I.; Kamal, A.; Rashid, H.M.; Alashqar, A.M.; Khater, S.; Jamal, D.; Waly, M. Ketogenic diet in cancer prevention and therapy: molecular targets and therapeutic opportunities. Current issues in molecular biology 2021, 43, 558–589. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhou, W. Roles and molecular mechanisms of physical exercise in cancer prevention and treatment. J Sport Health Sci 2021, 10, 201–210. [Google Scholar] [CrossRef]
- Friedenreich, C.M.; Stone, C.R.; Cheung, W.Y.; Hayes, S.C. Physical Activity and Mortality in Cancer Survivors: A Systematic Review and Meta-Analysis. JNCI Cancer Spectr 2020, 4, pkz080. [Google Scholar] [CrossRef] [PubMed]
- Kenfield, S.A.; Stampfer, M.J.; Giovannucci, E.; Chan, J.M. Physical Activity and Survival After Prostate Cancer Diagnosis in the Health Professionals Follow-Up Study. JCO 2011, 29, 726–732. [Google Scholar] [CrossRef]
- Lopez, P.; Galvão, D.A.; Taaffe, D.R.; Newton, R.U.; Souza, G.; Trajano, G.S.; Pinto, R.S. Resistance training in breast cancer patients undergoing primary treatment: a systematic review and meta-regression of exercise dosage. Breast Cancer 2021, 28, 16–24. [Google Scholar] [CrossRef]
- Lahart, I.M.; Metsios, G.S.; Nevill, A.M.; Carmichael, A.R. Physical activity, risk of death and recurrence in breast cancer survivors: A systematic review and meta-analysis of epidemiological studies. Acta Oncol 2015, 54, 635–654. [Google Scholar] [CrossRef]
- Beasley, J.M.; Kwan, M.L.; Chen, W.Y.; Weltzien, E.K.; Kroenke, C.H.; Lu, W.; Nechuta, S.J.; Cadmus-Bertram, L.; Patterson, R.E.; Sternfeld, B. , et al. Meeting the physical activity guidelines and survival after breast cancer: findings from the after breast cancer pooling project. Breast Cancer Res Treat 2012, 131, 637–643. [Google Scholar] [CrossRef]
- Chen, X.; Lu, W.; Zheng, W.; Gu, K.; Matthews, C.E.; Chen, Z.; Zheng, Y.; Shu, X.O. Exercise after diagnosis of breast cancer in association with survival. Cancer Prev Res (Phila) 2011, 4, 1409–1418. [Google Scholar] [CrossRef]
- Eckerling, A.; Ricon-Becker, I.; Sorski, L.; Sandbank, E.; Ben-Eliyahu, S. Stress and cancer: mechanisms, significance and future directions. Nat Rev Cancer 2021, 21, 767–785. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Saito, E.; Sawada, N.; Abe, S.K.; Hidaka, A.; Shimazu, T.; Yamaji, T.; Goto, A.; Iwasaki, M.; Sasazuki, S. , et al. Perceived stress level and risk of cancer incidence in a Japanese population: the Japan Public Health Center (JPHC)-based Prospective Study. Sci Rep 2017, 7, 12964. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, N.; Nishiyama, T.; Sawada, T.; Wang, C.; Lin, Y.; Watanabe, Y.; Tamakoshi, A.; Kikuchi, S. Perceived Stress and Colorectal Cancer Incidence: The Japan Collaborative Cohort Study. Sci Rep 2017, 7, 40363. [Google Scholar] [CrossRef] [PubMed]
- Walker, W.H.; Borniger, J.C. Molecular mechanisms of cancer-induced sleep disruption. International journal of molecular sciences 2019, 20, 2780. [Google Scholar] [CrossRef]
- Iseki, K.; Tatsuta, M.; Uehara, H.; Iishi, H.; Yano, H.; Sakai, N.; Ishiguro, S. Inhibition of angiogenesis as a mechanism for inhibition by Lα-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 of colon carcinogenesis induced by azoxymethane in Wistar rats. International Journal of Cancer 1999, 81, 730–733. [Google Scholar] [CrossRef]
- Pálmer, H.G.; González-Sancho, J.M.; Espada, J.; Berciano, M.T.; Puig, I.; Baulida, J.; Quintanilla, M.; Cano, A.; de Herreros, A.G.; Lafarga, M. , et al. Vitamin D(3) promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of beta-catenin signaling. J Cell Biol 2001, 154, 369–387. [Google Scholar] [CrossRef]
- Garland, C.F.; Garland, F.C.; Gorham, E.D.; Lipkin, M.; Newmark, H.; Mohr, S.B.; Holick, M.F. The Role of Vitamin D in Cancer Prevention. Am J Public Health 2006, 96, 252–261. [Google Scholar] [CrossRef]
- Fujioka, T.; Suzuki, Y.; Okamoto, T.; Mastushita, N.; Hasegawa, M.; Omori, S. Prevention of renal cell carcinoma by active vitamin D3. World J Surg 2000, 24, 1205–1210. [Google Scholar] [CrossRef]
- Keum, N.; Lee, D.H.; Greenwood, D.C.; Manson, J.E.; Giovannucci, E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Annals of Oncology 2019, 30, 733–743. [Google Scholar] [CrossRef]
- Chandler, P.D.; Chen, W.Y.; Ajala, O.N.; Hazra, A.; Cook, N.; Bubes, V.; Lee, I.M.; Giovannucci, E.L.; Willett, W.; Buring, J.E. , et al. Effect of Vitamin D3 Supplements on Development of Advanced Cancer: A Secondary Analysis of the VITAL Randomized Clinical Trial. JAMA Network Open 2020, 3, e2025850. [Google Scholar] [CrossRef]
- Marcinowska-Suchowierska, E.; Kupisz-Urbańska, M.; Łukaszkiewicz, J.; Płudowski, P.; Jones, G. Vitamin D Toxicity–A Clinical Perspective. Frontiers in Endocrinology 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Veiga, E.C.d.A.; Simões, R.; Valenti, V.E.; Cipolla-Neto, J.; Abreu, L.C.; Barros, E.P.M.; Sorpreso, I.C.E.; Baracat, M.C.P.; Baracat, E.C.; Soares, J.M. Repercussions of melatonin on the risk of breast cancer: a systematic review and meta-analysis. Rev. Assoc. Med. Bras. 2019, 65, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Park, S.; Koyanagi, A.; Yang, J.W.; Jacob, L.; Yon, D.K.; Lee, S.W.; Kim, M.S.; Il Shin, J.; Smith, L. Effects of exogenous melatonin supplementation on health outcomes: An umbrella review of meta-analyses based on randomized controlled trials. Pharmacological Research 2022, 176, 106052. [Google Scholar] [CrossRef] [PubMed]
- Sugden, D. Psychopharmacological effects of melatonin in mouse and rat. J Pharmacol Exp Ther 1983, 227, 587–591. [Google Scholar]
- Rehman, H.; Krishnasamy, Y.; Haque, K.; Thurman, R.G.; Lemasters, J.J.; Schnellmann, R.G.; Zhong, Z. Green Tea Polyphenols Stimulate Mitochondrial Biogenesis and Improve Renal Function after Chronic Cyclosporin A Treatment in Rats. PLOS ONE 2013, 8, e65029. [Google Scholar] [CrossRef]
- Lin, C.-H.; Shen, Y.-A.; Hung, P.-H.; Yu, Y.-B.; Chen, Y.-J. Epigallocathechin gallate, polyphenol present in green tea, inhibits stem-like characteristics and epithelial-mesenchymal transition in nasopharyngeal cancer cell lines. BMC Complement Altern Med 2012, 12, 201. [Google Scholar] [CrossRef]
- Bonuccelli, G.; Sotgia, F.; Lisanti, M.P. Matcha green tea (MGT) inhibits the propagation of cancer stem cells (CSCs), by targeting mitochondrial metabolism, glycolysis and multiple cell signalling pathways. Aging (Albany NY) 2018, 10, 1867–1883. [Google Scholar] [CrossRef]
- Yu, S.; Zhu, L.; Wang, K.; Yan, Y.; He, J.; Ren, Y. Green tea consumption and risk of breast cancer. Medicine (Baltimore) 2019, 98, e16147. [Google Scholar] [CrossRef]
- Abe, S.K.; Inoue, M. Green tea and cancer and cardiometabolic diseases: a review of the current epidemiological evidence. Eur J Clin Nutr 2021, 75, 865–876. [Google Scholar] [CrossRef]
- Mirtavoos-Mahyari, H.; Salehipour, P.; Parohan, M.; Sadeghi, A. Effects of Coffee, Black Tea and Green Tea Consumption on the Risk of Non-Hodgkin’s Lymphoma: A Systematic Review and Dose–Response Meta-Analysis of Observational Studies. Nutrition and Cancer 2019, 71, 887–897. [Google Scholar] [CrossRef]
- Dowling, R.J.O.; Zakikhani, M.; Fantus, I.G.; Pollak, M.; Sonenberg, N. Metformin inhibits mammalian target of rapamycin-dependent translation initiation in breast cancer cells. Cancer Research 2007, 67, 10804–10812. [Google Scholar] [CrossRef]
- He, K.; Hu, H.; Ye, S.; Wang, H.; Cui, R.; Yi, L. The effect of metformin therapy on incidence and prognosis in prostate cancer: A systematic review and meta-analysis. Sci Rep 2019, 9, 2218. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.-A.W.; Jiang, A.A.; Toh, E.M.S.; Ng, C.H.; Ong, Z.H.; Peng, S.; Tham, H.Y.; Sundar, R.; Chong, C.S.; Khoo, C.M. Metformin and colorectal cancer: a systematic review, meta-analysis and meta-regression. Int J Colorectal Dis 2020, 35, 1501–1512. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.-Q.; Zhou, X.-C.; Du, P.; Yin, M.-Y.; Xu, L.; Chen, W.-J.; Xu, C.-F. Relationships are between metformin use and survival in pancreatic cancer patients concurrent with diabetes. Medicine (Baltimore) 2020, 99, e21687. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Bai, P.; Dai, H.; Deng, Z. Metformin and risk of cancer among patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Primary Care Diabetes 2021, 15, 52–58. [Google Scholar] [CrossRef] [PubMed]
- PubChem. Metformin.
- Kunwar, A.; Barik, A.; Mishra, B.; Rathinasamy, K.; Pandey, R.; Priyadarsini, K.I. Quantitative cellular uptake, localization and cytotoxicity of curcumin in normal and tumor cells. Biochimica et Biophysica Acta (BBA)-General Subjects 2008, 1780, 673–679. [Google Scholar] [CrossRef] [PubMed]
- de Waure, C.; Bertola, C.; Baccarini, G.; Chiavarini, M.; Mancuso, C. Exploring the Contribution of Curcumin to Cancer Therapy: A Systematic Review of Randomized Controlled Trials. Pharmaceutics 2023, 15, 1275. [Google Scholar] [CrossRef]
- Opdyke, D.J.L.; Letizia, C. Monographs. Food and Chemical Toxicology 1983, 21, 833–875. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, L.; Zhang, J.; He, F.; Wang, H.; Liu, Q.; Shi, D.; Ni, N.; Wagstaff, W.; Chen, C. , et al. Antiparasitic mebendazole (MBZ) effectively overcomes cisplatin resistance in human ovarian cancer cells by inhibiting multiple cancer-associated signaling pathways. Aging (Albany NY) 2021, 13, 17407–17427. [Google Scholar] [CrossRef]
- Nygren, P.; Larsson, R. Drug repositioning from bench to bedside: tumour remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta Oncol 2014, 53, 427–428. [Google Scholar] [CrossRef]
- Dobrosotskaya, I.Y.; Hammer, G.D.; Schteingart, D.E.; Maturen, K.E.; Worden, F.P. Mebendazole monotherapy and long-term disease control in metastatic adrenocortical carcinoma. Endocr Pract 2011, 17, e59–62. [Google Scholar] [CrossRef]
- Chiang, R.S.; Syed, A.B.; Wright, J.L.; Montgomery, B.; Srinivas, Y. Fenbendazole Enhancing Anti-Tumor Effect: A Case Series. Clinical Oncology: Case Reports 2021, 2021. [Google Scholar]
- Marsboom, R. Toxicologic studies on mebendazole. Toxicology and Applied Pharmacology 1973, 24, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Fabian, C.J.; Kimler, B.F.; Hursting, S.D. Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Res 2015, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Nindrea, R.D.; Aryandono, T.; Lazuardi, L.; Dwiprahasto, I. Protective Effect of Omega-3 Fatty Acids in Fish Consumption Against Breast Cancer in Asian Patients: A Meta-Analysis. Asian Pac J Cancer Prev 2019, 20, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Sun, Y.; Yu, Q.; Song, S.; Brenna, J.T.; Shen, Y.; Ye, K. Higher ratio of plasma omega-6/omega-3 fatty acids is associated with greater risk of all-cause, cancer, and cardiovascular mortality: a population-based cohort study in UK Biobank. 2023. [Google Scholar] [CrossRef]
- Bays, H.E. Safety Considerations with Omega-3 Fatty Acid Therapy. The American Journal of Cardiology 2007, 99, S35–S43. [Google Scholar] [CrossRef]
- Zhang, C.; Sheng, J.; Li, G.; Zhao, L.; Wang, Y.; Yang, W.; Yao, X.; Sun, L.; Zhang, Z.; Cui, R. Effects of Berberine and Its Derivatives on Cancer: A Systems Pharmacology Review. Frontiers in Pharmacology 2020, 10. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Y.; Du, X.; Ma, H.; Yao, J. The Anti-Cancer Mechanisms of Berberine: A Review. Cancer Manag Res 2020, 12, 695–702. [Google Scholar] [CrossRef]
- Fang, S.; Guo, S.; Du, S.; Cao, Z.; Yang, Y.; Su, X.; Wei, W. Efficacy and safety of berberine in preventing recurrence of colorectal adenomas: A systematic review and meta-analysis. Journal of Ethnopharmacology 2022, 282, 114617. [Google Scholar] [CrossRef]
- Xu, J.; Long, Y.; Ni, L.; Yuan, X.; Yu, N.; Wu, R.; Tao, J.; Zhang, Y. Anticancer effect of berberine based on experimental animal models of various cancers: a systematic review and meta-analysis. BMC Cancer 2019, 19, 589. [Google Scholar] [CrossRef] [PubMed]
- Haginiwa, J.; Harada, M. Pharmacological Studies on Crude Drugs. V. Yakugaku Zasshi 1962, 82, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Hu, J.-W.; He, X.-R.; Jin, W.-L.; He, X.-Y. Statins: a repurposed drug to fight cancer. J Exp Clin Cancer Res 2021, 40, 241. [Google Scholar] [CrossRef]
- Carter, P.; Vithayathil, M.; Kar, S.; Potluri, R.; Mason, A.M.; Larsson, S.C.; Burgess, S. Predicting the effect of statins on cancer risk using genetic variants from a Mendelian randomization study in the UK Biobank. Elife 2020, 9, e57191. [Google Scholar] [CrossRef] [PubMed]
- Yu, O.; Eberg, M.; Benayoun, S.; Aprikian, A.; Batist, G.; Suissa, S.; Azoulay, L. Use of Statins and the Risk of Death in Patients With Prostate Cancer. JCO 2014, 32, 5–11. [Google Scholar] [CrossRef]
- Manthravadi, S.; Shrestha, A.; Madhusudhana, S. Impact of statin use on cancer recurrence and mortality in breast cancer: A systematic review and meta-analysis. International Journal of Cancer 2016, 139, 1281–1288. [Google Scholar] [CrossRef]
- Ahern, T.P.; Pedersen, L.; Tarp, M.; Cronin-Fenton, D.P.; Garne, J.P.; Silliman, R.A.; Sørensen, H.T.; Lash, T.L. Statin Prescriptions and Breast Cancer Recurrence Risk: A Danish Nationwide Prospective Cohort Study. J Natl Cancer Inst 2011, 103, 1461–1468. [Google Scholar] [CrossRef]
- Lash, T.L.; Riis, A.H.; Ostenfeld, E.B.; Erichsen, R.; Vyberg, M.; Ahern, T.P.; Thorlacius-Ussing, O. Associations of Statin Use With Colorectal Cancer Recurrence and Mortality in a Danish Cohort. Am J Epidemiol 2017, 186, 679–687. [Google Scholar] [CrossRef]
- Shao, J.Y.-H.; Lee, F.-P.; Chang, C.-L.; Wu, S.-Y. Statin-Based Palliative Therapy for Hepatocellular Carcinoma. Medicine (Baltimore) 2015, 94, e1801. [Google Scholar] [CrossRef]
- Gray, R.T.; Coleman, H.G.; Hughes, C.; Murray, L.J.; Cardwell, C.R. Statin use and survival in colorectal cancer: Results from a population-based cohort study and an updated systematic review and meta-analysis. Cancer Epidemiol 2016, 45, 71–81. [Google Scholar] [CrossRef]
- Lin, J.J.; Ezer, N.; Sigel, K.; Mhango, G.; Wisnivesky, J.P. The effect of statins on survival in patients with stage IV lung cancer. Lung Cancer 2016, 99, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Elseweidy, M.; Asker, E.-S.; Atteia, H.; Mohamed, S.; Hegazy, S. Atorvastatin and Fenofibrate Modulate Certain Steroidal Hormones, Vitamin D and Bile Acids in Diabetic Dyslipidemic Rats. 2015, 7, 426-434.
- Jiang, W.; Hu, J.-W.; He, X.-R.; Jin, W.-L.; He, X.-Y. Statins: a repurposed drug to fight cancer. Journal of Experimental & Clinical Cancer Research 2021, 40, 1–33. [Google Scholar]
- Baas, J.M.; Krens, L.L.; ten Tije, A.J.; Erdkamp, F.; van Wezel, T.; Morreau, H.; Gelderblom, H.; Guchelaar, H.J. Safety and efficacy of the addition of simvastatin to cetuximab in previously treated KRAS mutant metastatic colorectal cancer patients. Invest New Drugs 2015, 33, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- PubChem. Simvastatin. Availabe online: https://www.ncbi.nlm.nih.gov/pubmed/.
- Liu, P.; Kumar, I.; Brown, S.; Kannappan, V.; Tawari, P.; Tang, J.; Jiang, W.; Armesilla, A.; Darling, J.; Wang, W. Disulfiram targets cancer stem-like cells and reverses resistance and cross-resistance in acquired paclitaxel-resistant triple-negative breast cancer cells. British journal of cancer 2013, 109, 1876–1885. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, K.; Wang, Y.; Li, M.; Sun, X.; Liang, Z.; Wang, L.; Chen, L.; Yang, H.; Zhu, L. Disulfiram chelated with copper promotes apoptosis in human breast cancer cells by impairing the mitochondria functions. Scanning 2016, 38, 825–836. [Google Scholar] [CrossRef]
- PubChem. Disulfiram. Availabe online: https://www.ncbi.nlm.nih.
- Kubecova, M.; Kolostova, K.; Pinterova, D.; Kacprzak, G.; Bobek, V. Cimetidine: an anticancer drug? Eur J Pharm Sci 2011, 42, 439–444. [Google Scholar] [CrossRef]
- Tonnesen, H.; Bülow, S.; Fischerman, K.; Hjortrup, A.; Møller Pedersen, V.; Bo Svendsen, L.; Knigge, U.; Damm, P.; Hesselfeldt, P.; Krogh Pedersen, I. , et al. Effect of Cimetidine on Survival after gastric cancer. The Lancet 1988, 332, 990–992. [Google Scholar] [CrossRef]
- Deva, S.; Jameson, M. Histamine type 2 receptor antagonists as adjuvant treatment for resected colorectal cancer. Cochrane Database Syst Rev, 1002; CD007814. [Google Scholar] [CrossRef]
- Brimblecombe, R.W.; Duncan, W.A.M.; Durant, G.J.; Emmett, J.C.; Ganellin, C.R.; Parsons, M.E. Cimetidine—A Non-Thiourea H2-Receptor Antagonist. J Int Med Res 1975, 3, 86–92. [Google Scholar] [CrossRef]
- Kleijnen, J.; Knipschild, P. Mistletoe treatment for cancer review of controlled trials in humans. Phytomedicine 1994, 1, 255–260. [Google Scholar] [CrossRef]
- John Wasagwa, B.B.L.; Biu Abubakar Abdullahi, Luka Joshua, Ngulde Ibrahim Saidu, Onyiche Emmanuel Thank God. Phytochemistry and Toxicity Studies on Aqueous Extracts of Leaf and Stem of Mistletoe (Science Publishing Group 2018, 4, 1. [CrossRef]
- Phase I Trial of Intravenous Mistletoe Extract in Advanced Cancer | Cancer Research Communications | American Association for Cancer Research. 2023. [CrossRef]
- Shi, Z.; Tiwari, A.K.; Patel, A.S.; Fu, L.-W.; Chen, Z.-S. Roles of sildenafil in enhancing drug sensitivity in cancer. Cancer Research 2011, 71, 3735–3738. [Google Scholar] [CrossRef]
- PubChem. Sildenafil.
- Liu, N.; Yan, L.; Shan, F.; Wang, X.; Qu, N.; Handley, M.K.; Ma, M. Low-dose naltrexone plays antineoplastic role in cervical cancer progression through suppressing PI3K/AKT/mTOR pathway. Translational Oncology 2021, 14, 101028. [Google Scholar] [CrossRef]
- WM, L.; AG, D. Naltrexone at low doses (LDN) and its relevance to cancer therapy. Expert review of anticancer therapy 2022, 22. [Google Scholar] [CrossRef]
- L, P.; J, Y. Reduced Pro-Inflammatory Cytokines after Eight Weeks of Low-Dose Naltrexone for Fibromyalgia. Biomedicines 2017, 5. [Google Scholar] [CrossRef]
- Miskoff, J.A.; Chaudhri, M. Low dose naltrexone and lung cancer: a case report and discussion. Cureus 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Donahue, R.N.; McLaughlin, P.J.; Zagon, I.S. The opioid growth factor (OGF) and low dose naltrexone (LDN) suppress human ovarian cancer progression in mice. Gynecologic Oncology 2011, 122, 382–388. [Google Scholar] [CrossRef]
- PubChem. Naltrexone. Availabe online: https://www.ncbi.nlm.nih.gov/pubmed/.
- Ghasemi, K.; Ghasemi, K. A Brief look at antitumor effects of doxycycline in the treatment of colorectal cancer and combination therapies. Eur J Pharmacol 2022, 916, 174593. [Google Scholar] [CrossRef]
- Tkachenko, E.M.; Grintsov, E.F.; Zupanets, I.A.; Shebeko, S.K. Study of the acute toxicity of the combination of doxycycline with glucosamine hydrochloride. 2014.
- Bar-Sela, G.; Cohen, M.; Ben-Arye, E.; Epelbaum, R. The medical use of wheatgrass: review of the gap between basic and clinical applications. Mini reviews in medicinal chemistry 2015, 15, 1002–1010. [Google Scholar] [CrossRef]
- Das, P.; Mukhopadhyay, S.; Mandal, S.; Chakraborty, A.; Pal, A.; Sarkar, N.K.; Mukhopadhyay, A. Acute toxicity test of a natural iron chelator and an antioxidant, extracted from Triticum aestivum Linn. (wheat grass). 2014; 901321. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Sethi, G.; Vadhan-Raj, S.; Bueso-Ramos, C.; Takada, Y.; Gaur, U.; Nair, A.S.; Shishodia, S.; Aggarwal, B.B. Resveratrol inhibits proliferation, induces apoptosis, and overcomes chemoresistance through down-regulation of STAT3 and nuclear factor-kappaB-regulated antiapoptotic and cell survival gene products in human multiple myeloma cells. Blood 2007, 109, 2293–2302. [Google Scholar] [CrossRef]
- Zhang, L.; Wen, X.; Li, M.; Li, S.; Zhao, H. Targeting cancer stem cells and signaling pathways by resveratrol and pterostilbene. Biofactors 2018, 44, 61–68. [Google Scholar] [CrossRef]
- Ko, J.-H.; Sethi, G.; Um, J.-Y.; Shanmugam, M.K.; Arfuso, F.; Kumar, A.P.; Bishayee, A.; Ahn, K.S. The Role of Resveratrol in Cancer Therapy. International Journal of Molecular Sciences 2017, 18, 2589. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, S.D.; Diderich, R.; Sobanski, T.; Pavlov, T.S.; Chankov, G.V.; Chapkanov, A.S.; Karakolev, Y.H.; Temelkov, S.G.; Vasilev, R.A.; Gerova, K.D. , et al. QSAR Toolbox - workflow and major functionalities. SAR QSAR Environ Res 2016, 27, 203–219. [Google Scholar] [CrossRef] [PubMed]
- Tao, D.L.; Tassi Yunga, S.; Williams, C.D.; McCarty, O.J.T. Aspirin and antiplatelet treatments in cancer. Blood 2021, 137, 3201–3211. [Google Scholar] [CrossRef]
- Corley, D.A.; Kerlikowske, K.; Verma, R.; Buffler, P. Protective association of aspirin/NSAIDs and esophageal cancer: A systematic review and meta-analysis. Gastroenterology 2003, 124, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Yang, T.; Gan, Y.; Li, W.; Wang, C.; Gong, Y.; Lu, Z. Associations between aspirin use and the risk of cancers: a meta-analysis of observational studies. BMC Cancer 2018, 18, 288. [Google Scholar] [CrossRef]
- Bekemeier, H. [Salicylamide and salicylic acid poisoning in cats, in comparison with other animals. I]. Arzneimittelforschung 1955, 5, 572–575. [Google Scholar]
- Amanullah, A.; Upadhyay, A.; Dhiman, R.; Singh, S.; Kumar, A.; Ahirwar, D.K.; Gutti, R.K.; Mishra, A. Development and Challenges of Diclofenac-Based Novel Therapeutics: Targeting Cancer and Complex Diseases. Cancers 2022, 14, 4385. [Google Scholar] [CrossRef]
- Forget, P.; Bentin, C.; Machiels, J.P.; Berliere, M.; Coulie, P.G.; De Kock, M. Intraoperative use of ketorolac or diclofenac is associated with improved disease-free survival and overall survival in conservative breast cancer surgery. British Journal of Anaesthesia 2014, 113, i82–i87. [Google Scholar] [CrossRef]
- Singer, K.; Dettmer, K.; Unger, P.; Schönhammer, G.; Renner, K.; Peter, K.; Siska, P.J.; Berneburg, M.; Herr, W.; Oefner, P.J. , et al. Topical Diclofenac Reprograms Metabolism and Immune Cell Infiltration in Actinic Keratosis. Front Oncol 2019, 9, 605. [Google Scholar] [CrossRef]
- Tao, Y.-L.; Wang, Z.-J.; Han, J.-G.; Wei, P. Inflammatory myofibroblastic tumor successfully treated with chemotherapy and nonsteroidals: A case report. World J Gastroenterol 2012, 18, 7100–7103. [Google Scholar] [CrossRef]
- Teshima, M.; Iwae, S.; Hirayama, Y.; Furukawa, T. Nonsteroidal anti-inflammatory drug treatment for desmoid tumor recurrence after surgery. Otolaryngol Head Neck Surg 2012, 147, 978–979. [Google Scholar] [CrossRef]
- Lackner, H.; Urban, C.; Benesch, M.; Raith, J.; Moser, A.; Sovinz, P.; Schwinger, W.; Dornbusch, H.J.; Triebl-Roth, K. Multimodal treatment of children with unresectable or recurrent desmoid tumors: an 11-year longitudinal observational study. J Pediatr Hematol Oncol 2004, 26, 518–522. [Google Scholar] [CrossRef]
- Lackner, H.; Urban, C.; Kerbl, R.; Schwinger, W.; Beham, A. Noncytotoxic drug therapy in children with unresectable desmoid tumors. Cancer 1997, 80, 334–340. [Google Scholar] [CrossRef]
- Breuer, S.; Maimon, O.; Appelbaum, L.; Peretz, T.; Hubert, A. TL-118-anti-angiogenic treatment in pancreatic cancer: a case report. Med Oncol 2013, 30, 585. [Google Scholar] [CrossRef] [PubMed]
- Schumann, S.; Mann, G.; Wilde, H.; Ploen, U.; Mager, P.P. [Biological effects of 3-substituted acetic acid derivatives of 1,2,4-benzotriazines]. Pharmazie 1982, 37, 148–149. [Google Scholar] [CrossRef]
- Majdalawieh, A.F.; Fayyad, M.W.; Nasrallah, G.K. Anti-cancer properties and mechanisms of action of thymoquinone, the major active ingredient of Nigella sativa. Critical Reviews in Food Science and Nutrition 2017, 57, 3911–3928. [Google Scholar] [CrossRef] [PubMed]
- Dogar, M.; Adnan, H.; Akhtar, M.S.; Sheikh, M.A. Preliminary assessment of efficacy of Nigella sativa seeds in acute lymphoblastic leukemia local children. Pharmacologyonline 2009, 2, 769–777. [Google Scholar]
- Zaoui, A.; Cherrah, Y.; Mahassini, N.; Alaoui, K.; Amarouch, H.; Hassar, M. Acute and chronic toxicity of Nigella sativa fixed oil. Phytomedicine 2002, 9, 69–74. [Google Scholar] [CrossRef]
- Ayeka, P.A. Potential of Mushroom Compounds as Immunomodulators in Cancer Immunotherapy: A Review. Evid Based Complement Alternat Med 2018, 2018, 7271509. [Google Scholar] [CrossRef]
- Cao, Y.; Xu, X.; Liu, S.; Huang, L.; Gu, J. Ganoderma: A Cancer Immunotherapy Review. Frontiers in Pharmacology 2018, 9, 1217. [Google Scholar] [CrossRef]
- Jin, X.; Beguerie, J.R.; Sze, D.M.-y.; Chan, G.C.F. Ganoderma lucidum (Reishi mushroom) for cancer treatment. Cochrane Database of Systematic Reviews, 2012. [Google Scholar] [CrossRef]
- Li, Y.; Zhiyong, X.; Wei, L.; Birong, Z. Study on acute toxicity and genetic toxicity test of Ganoderma Lucidum Spore Powder Capsule. Tianjin Pharmacy 2007, 2, 14–23. [Google Scholar]
- Juarez, M.; Schcolnik-Cabrera, A.; Dueñas-Gonzalez, A. The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug. Am J Cancer Res 2018, 8, 317–331. [Google Scholar]
- Tang, M.; Hu, X.; Wang, Y.; Yao, X.; Zhang, W.; Yu, C.; Cheng, F.; Li, J.; Fang, Q. Ivermectin, a potential anticancer drug derived from an antiparasitic drug. Pharmacological Research 2021, 163, 105207. [Google Scholar] [CrossRef] [PubMed]
- Ishiguro, T.; Ishiguro, R.H.; Ishiguro, M.; Toki, A.; Terunuma, H. Synergistic Anti-tumor Effect of Dichloroacetate and Ivermectin. Cureus 2022, 14, e21884. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.K.; Chu, L.; Mrozik, H.; Slayton, L.; Rafalko, B.; Goldmann, M.L.; Shoop, W.L.; Margiatto, G.; Fisher, M.H. Synthesis and Biological Activity of 4a,4"-Disubstituted Avermectins. J. Agric. Food Chem. 1994, 42, 1786–1790. [Google Scholar] [CrossRef]
- Spano, D.; Marshall, J.-C.; Marino, N.; De Martino, D.; Romano, A.; Scoppettuolo, M.N.; Bello, A.M.; Di Dato, V.; Navas, L.; De Vita, G. , et al. Dipyridamole prevents triple-negative breast-cancer progression. Clin Exp Metastasis 2013, 30, 47–68. [Google Scholar] [CrossRef]
- Budd, G.T.; Herzog, P.; Bukowski, R.M. Phase I/II trial of dipyridamole, 5-fluorouracil, leukovorin, and mitoxantrone in metastatic breast cancer. Invest New Drugs 1994, 12, 283–287. [Google Scholar] [CrossRef]
- Kohnoe, S.; Maehara, Y.; Takahashi, I.; Emi, Y.; Baba, H.; Sugimachi, K. Treatment of advanced gastric cancer with 5-fluorouracil and cisplatin in combination with dipyridamole. Int J Oncol 1998, 13, 1203–1206. [Google Scholar] [CrossRef]
- Raschko, J.W.; Synold, T.W.; Chow, W.; Coluzzi, P.; Hamasaki, V.; Leong, L.A.; Margolin, K.A.; Morgan, R.J.; Shibata, S.I.; Somlo, G. , et al. A phase I study of carboplatin and etoposide administered in conjunction with dipyridamole, prochlorperazine and cyclosporine A. Cancer Chemotherapy and Pharmacology 2000, 46, 403–410. [Google Scholar] [CrossRef]
- Takenaka, F.; Takeya, N.; Ishihara, T.; Higuchi, M.; Hayashi, H. Toxicological studies on dipyridamole in the rat. Arzneimittelforschung 1972, 22, 892–895. [Google Scholar]
- Benade, L.; Howard, T.; Burk, D. Synergistic killing of Ehrlich ascites carcinoma cells by ascorbate and 3-amino-1,2,4,-triazole. Oncology 1969, 23, 33–43. [Google Scholar] [CrossRef]
- Takahashi, H.; Mizuno, H.; Yanagisawa, A. High-dose intravenous vitamin C improves quality of life in cancer patients. Personalized Medicine Universe 2012, 1, 49–53. [Google Scholar] [CrossRef]
- Mikirova, N.; Casciari, J.; Rogers, A.; Taylor, P. Effect of high-dose intravenous vitamin C on inflammation in cancer patients. Journal of Translational Medicine 2012, 10, 189. [Google Scholar] [CrossRef]
- PubChem. Ascorbic Acid.
- Stacpoole, P.W. Therapeutic Targeting of the Pyruvate Dehydrogenase Complex/Pyruvate Dehydrogenase Kinase (PDC/PDK) Axis in Cancer. J Natl Cancer Inst 2017, 109. [Google Scholar] [CrossRef] [PubMed]
- Powell, S.F.; Mazurczak, M.; Dib, E.G.; Bleeker, J.S.; Geeraerts, L.H.; Tinguely, M.; Lohr, M.M.; McGraw, S.C.; Jensen, A.W.; Ellison, C.A. , et al. Phase II study of dichloroacetate, an inhibitor of pyruvate dehydrogenase, in combination with chemoradiotherapy for unresected, locally advanced head and neck squamous cell carcinoma. Invest New Drugs 2022, 40, 622–633. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, V.; Bonomi, M.; Marinelli, L.; Gervasio, F.L.; Cavalli, A.; Novellino, E.; Parrinello, M. Molecular basis of cyclooxygenase enzymes (COXs) selective inhibition. Proceedings of the National Academy of Sciences 2010, 107, 5411–5416. [Google Scholar] [CrossRef]
- Velasco, G.; Sánchez, C.; Guzmán, M. Anticancer mechanisms of cannabinoids. Current oncology (Toronto, Ont.) 2016, 23, S23–32. [Google Scholar] [CrossRef] [PubMed]
- Sarfaraz, S.; Adhami, V.M.; Syed, D.N.; Afaq, F.; Mukhtar, H. Cannabinoids for cancer treatment: progress and promise. Cancer research 2008, 68, 339–342. [Google Scholar] [CrossRef] [PubMed]
- RN, P.; RF, T.; RB, F. Acute toxicity of delta-9-tetrahydrocannabinol in rats and mice. Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine (New York, N.Y.) 1971, 136. [Google Scholar] [CrossRef]
- NIDA Research Monograph, 2023.
- Guggisberg, J.; Schumacher, M.; Gilmore, G.; Zylla, D.M. Cannabis as an Anticancer Agent: A Review of Clinical Data and Assessment of Case Reports. https://home.liebertpub.com/can. 2022. [Google Scholar] [CrossRef]
- Lian, X.; Wang, G.; Zhou, H.; Zheng, Z.; Fu, Y.; Cai, L. Anticancer properties of fenofibrate: a repurposing use. Journal of Cancer 2018, 9, 1527. [Google Scholar] [CrossRef]
- Kumar, M.; Patidar, S.; Singh, R.; Dhiman, V. Fenofibrate inhibit the development of malaria in Plasmodium berghei-infected mice. World Journal of Pharmaceutical Sciences 2014, 1273–1276. [Google Scholar]
- Chang, C.; Zhao, W.; Xie, B.; Deng, Y.; Han, T.; Cui, Y.; Dai, Y.; Zhang, Z.; Gao, J.; Guo, H. Pao pereira extract suppresses castration-resistant prostate cancer cell growth, survival, and invasion through inhibition of NFκB signaling. Integrative Cancer Therapies 2014, 13, 249–258. [Google Scholar] [CrossRef]
- Bemis, D.L.; Capodice, J.L.; Desai, M.; Katz, A.E.; Buttyan, R. beta-carboline alkaloid-enriched extract from the amazonian rain forest tree pao pereira suppresses prostate cancer cells. Journal of the Society for Integrative Oncology 2009, 7, 59–65. [Google Scholar] [PubMed]
- Moser, J.C.; Salvador, E.; Deniz, K.; Swanson, K.; Tuszynski, J.; Carlson, K.W.; Karanam, N.K.; Patel, C.B.; Story, M.; Lou, E. , et al. The Mechanisms of Action of Tumor Treating Fields. Cancer Research 2022, 82, 3650–3658. [Google Scholar] [CrossRef] [PubMed]
- Juarranz, Á.; Jaén, P.; Sanz-Rodríguez, F.; Cuevas, J.; González, S. Photodynamic therapy of cancer. Basic principles and applications. Clinical and Translational Oncology 2008, 10, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Moen, I.; Stuhr, L.E.B. Hyperbaric oxygen therapy and cancer--a review. Target Oncol 2012, 7, 233–242. [Google Scholar] [CrossRef]
- Manning, E.P. Central Nervous System Oxygen Toxicity and Hyperbaric Oxygen Seizures. 2016. [Google Scholar] [CrossRef]
- Gonzalez, R.P.; Leyva, A.; Moraes, M.O. Shark cartilage as source of antiangiogenic compounds: from basic to clinical research. Biological and Pharmaceutical Bulletin 2001, 24, 1097–1101. [Google Scholar] [CrossRef]
- Miller, D.R.; Anderson, G.T.; Stark, J.J.; Granick, J.L.; Richardson, D. Phase I/II trial of the safety and efficacy of shark cartilage in the treatment of advanced cancer. 2016, 9817287. [Google Scholar] [CrossRef] [PubMed]
- Mondo, K.; Hammerschlag, N.; Basile, M.; Pablo, J.; Banack, S.A.; Mash, D.C. Cyanobacterial Neurotoxin β-N-Methylamino-L-alanine (BMAA) in Shark Fins. Marine Drugs 2012, 10, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Liczbiński, P.; Bukowska, B. Molecular mechanism of amygdalin action in vitro: review of the latest research. Immunopharmacology and Immunotoxicology 2018, 40, 212–218. [Google Scholar] [CrossRef]
- Shi, J.; Chen, Q.; Xu, M.; Xia, Q.; Zheng, T.; Teng, J.; Li, M.; Fan, L. Recent updates and future perspectives about amygdalin as a potential anticancer agent: A review. Cancer Medicine 2019, 8, 3004–3011. [Google Scholar] [CrossRef] [PubMed]
- Adewusi, S.R.A.; Oke, O.L. On the metabolism of amygdalin. 1. The LD50 and biochemical changes in rats. 2011. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




