1. Introduction
The maxillary sinus is often affected by periapical pathologies because of its proximity to the maxillary posterior teeth. As a result, conditions affecting the maxillary sinuses can imitate dental problems, and vice versa [
1]. Radiographs are frequently used to diagnose diseases of the maxillary sinus ranging from conventional 2D imaging like panoramic radiograph and PA view of sinuses to the more advanced 3D imaging modalities like cone-beam computed tomography (CBCT), computed tomography (CT), and magnetic resonance imaging (MRI). The multiplanar images acquired by CBCT allow radiologists to inspect the entire volume of the acquired image and anatomic variations or abnormalities found in the image volume [
2]. The maxillary sinus area is usually within the imaging field when CBCT is indicated for dental implant site assessment or periapical pathologies3. Hence, maxillofacial radiologists frequently view the incidental findings in the maxillary sinus area and can assess the prevalence, which can be incidental, benign, or detrimental to the treatment plan.
In a study by Cha et al. [
4], using CBCT examinations, the abnormalities found were signs of sinusitis (7.5%), retention cysts (3.5%), and polypoid mucosal thickening (2.3%). In another study, the prevalence of flat mucosal thickening ranged from 23.7% to 38.1%, polypoid mucosal thickening ranged from 6.5% to19.4%, signs of acute sinusitis were 3.6%, and partial and total opacification were 12% and 7%, respectively.
The inability of oral radiologists to detect incidental abnormalities in the maxillary sinus despite being visible in the CBCT volume is often due to their limited experience in interpreting volumetric images and their failure to conduct a thorough visual examination of the entire image [
5]. The European Academy of Dento-MaxilloFacial Radiology (EADMFR) and the American Academy of Oral and Maxillofacial Radiology (AAOMR) outlines that an oral and maxillofacial radiologist should review and interpret the entire volume regardless of the region of interest [
6].
The present study was undertaken to record the prevalence of incidental maxillary sinus abnormalities in CBCT scans, recognize the frequency, type, and location of these findings and correlate the distance between the periapical lesions and the presence of any inflammatory changes in the maxillary sinus.
2. Materials and Methods
The retrospective study was conducted in the Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Mangalore. After receiving approval from the Institutional Ethical Committee, MAHE/MCODSMLR/ 198/2021. A statistician was consulted and considering the power of the study to be 80%, it was advised to include 117 patient scans. Detailed information regarding age, gender, facial asymmetry, trauma, and history of upper respiratory infections was obtained from the patient’s past medical records. Large FOV CBCT scans were included in the study, extended from the roof of the orbits inferiorly to at least the second cervical vertebrae of patients above 18. Scans of edentulous patients, patients referred exclusively for Max sinus abnormalities, young patients with incomplete sinus development, low-resolution images, and those with metallic artifacts which impaired sinus visualization were excluded.
The CBCT images were obtained using standard exposure parameters and patient positioning protocols (field of view= 17×10cm, resolution= 0.16mm, 80–84kvp, 10–12mA) with a CBCT unit (Planmeca, Helsinki, Finland). Romexis version 4.6.2 software (Planmeca, Helsinki, Finland) was used. Exposure parameters were standardized for all the patients. The CBCT scan had panoramic reconstruction and multiplanar reformation views, i.e., axial, sagittal, and coronal planes. Two examiners assessed all images to diagnose and classify them into different abnormality subtypes. In case of a discrepancy between two observers, a third examiner intervened, and a consensus on the radiologic impression was obtained. The presence or absence of sinus abnormalities was identified using a yes/no scale. The radiology reports followed a consistent format and contained a listing of all radiographic findings used to tabulate the data in this study using Microsoft Excel.
Increased or decreased dimension of the sinus
Radiographic density changes in the cortical bone of the sinus
Partial or complete opacification of the sinus cavity
Increased thickening of the mucosa greater than 3 mm.
Congenital changes (aplasia and hypoplasia),
Inflammatory lesions like polyps
Fracture lines
Patients were divided into the following age groups: 1) <20; 2) 20-30; 3)30-40; 4) 40-50; and 5) 50-60; 6)60 years and above.
The location of the diagnosed abnormalities was recorded as affecting either the anterior, posterior, inferior, superior, lateral, or medial walls of the sinus based on the method of Nishimura & Iizuka [
7]. The presence of periapical lesions in upper posterior teeth was recorded. The lesions' proximity to the sinus wall floor was classified using the method followed by Oberli et al. [
8]. They were classified as Class I (near the sinus floor), class II (in contact with the sinus floor), and Class III (overlapping the sinus floor). A periapical lesion was recorded when the lamina dura was imperceptible or had an irregular appearance and when there was a radiolucency indicating bone destruction around the root apex. Only the lesion most closely related to the sinus was recorded in cases of multiple periapical lesions near the sinuses. The above findings were all correlated with the age and gender of the patient.
A Chi-square test was used to compare the patterns with gender and age. Pearson's correlation coefficient was applied to assess the correlation between dimensions using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) was employed for data analysis. Results were considered significant at a p-value of < 0.05 level.
3. Results
Fifty-five patients (47%) were male, and 62 (53%) were female. The most common indication for CBCT scans was dental implant site assessment, surgical planning, Orthodontic scans, TMJ dysfunction, suspected oral malignancies, and trauma.
68 patients were found to have pathologic findings in one or both sinuses, such as mucosal thickening, retention cysts, opacification, sinus polyps, and antrolith. (58.1%) (
Figure 1,
Figure 2,
Figure 3 and
Figure 4). Of 55 male patients, 33 had pathologies like oroantral communication and Inflammatory cysts in either sinus, whereas only 35 of the 62 scans of female patients revealed radiographically abnormal findings in either sinus. The difference in findings between male and female patients was not statistically significant (
Table 1).
Patients in the 6th decade of life showed a slightly higher prevalence of pathologic findings in the maxillary sinus, which was statistically significant (p=0.017) (
Table 2).
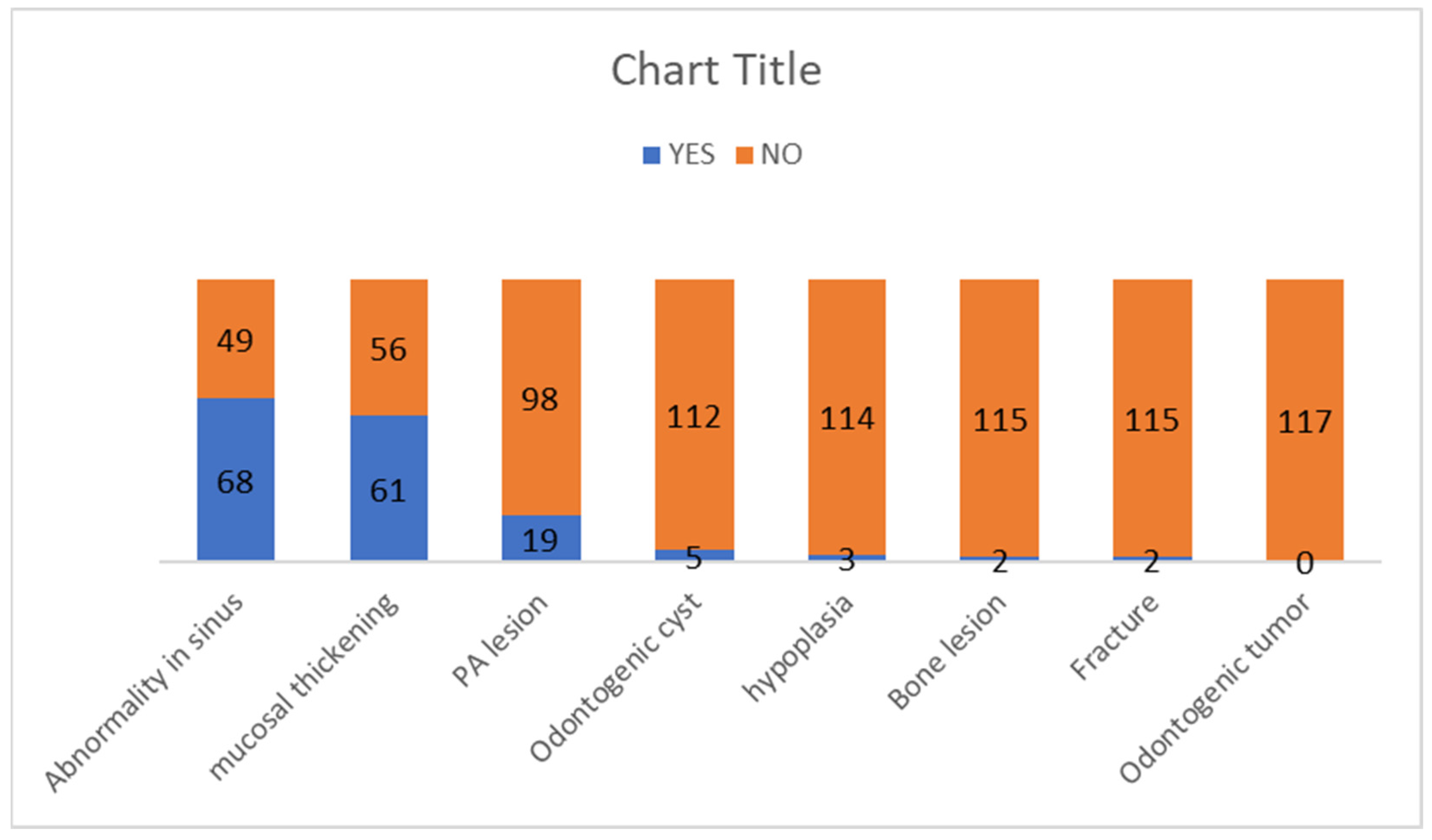
Sixty-one patients were diagnosed with mucosal thickening (52.1%). The sinus wall most affected by mucosal thickening was the maxillary sinus floor, followed by the medial and lateral walls of the maxillary sinus. Of the 19 patients with Odontogenic conditions causing periapical lesions, 15 had maxillary sinus mucosal thickening, and the relation was statistically significant (p=0.004). The odontogenic cyst was diagnosed in 5 patients (4.3%), while a sinus wall fracture was recorded in 2 patients (1.7%). Maxillary sinus hypoplasia was diagnosed in three patients (2.6%). The frequency of the pathologies is represented in Graph 1.
3.2. Figures, Tables and Schemes
The frequency of the pathologies seen as incidental findings in the maxillary sinus.
Graph 1.
The frequency of the pathologies seen as incidental findings in the maxillary sinus.
Graph 1.
The frequency of the pathologies seen as incidental findings in the maxillary sinus.
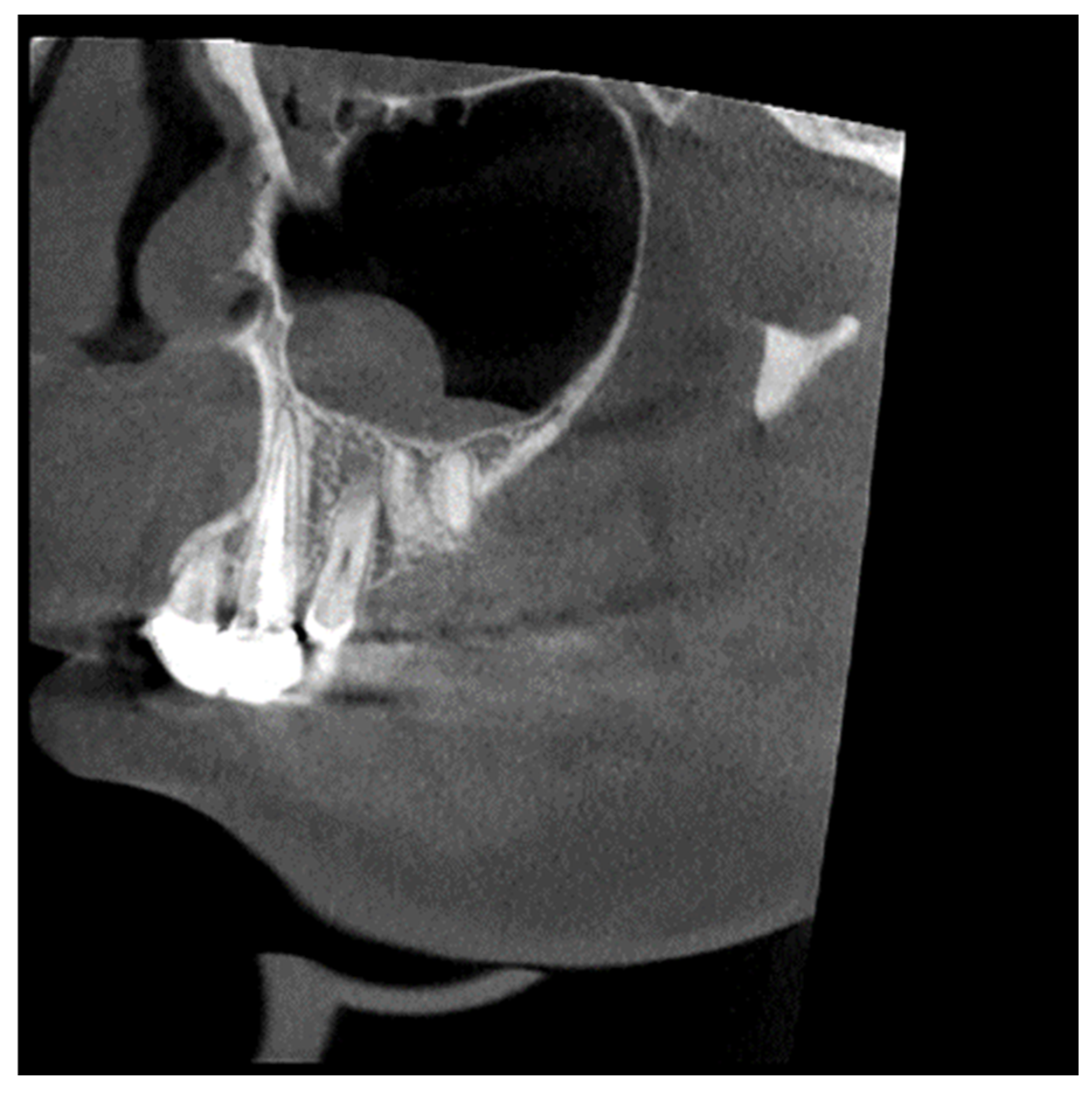
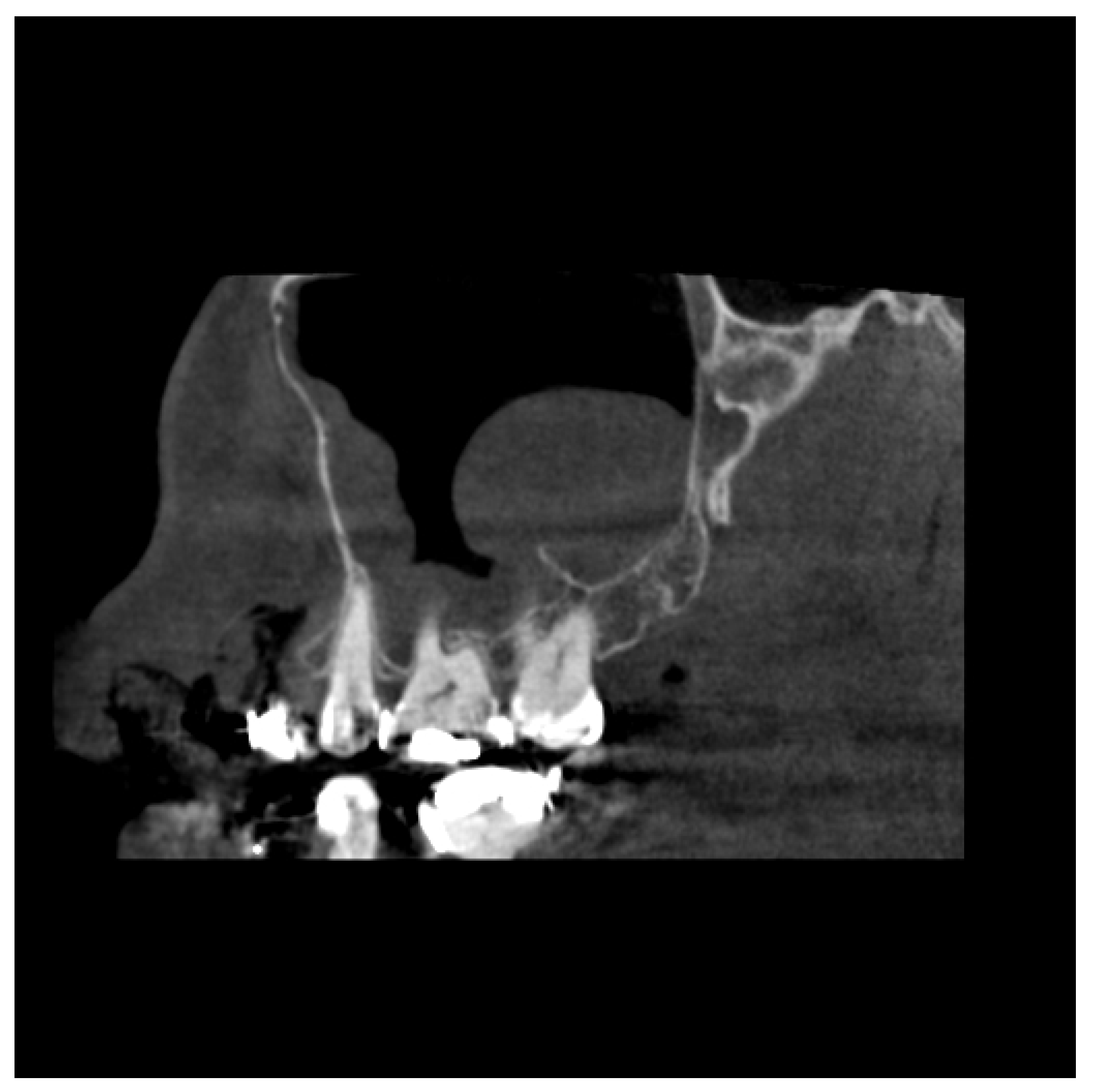
Figure 1.
View from the Sagittal plane. The maxillary sinus floor shows a thickening of the mucous boundaries of the maxillary sinuses.
Figure 1.
View from the Sagittal plane. The maxillary sinus floor shows a thickening of the mucous boundaries of the maxillary sinuses.
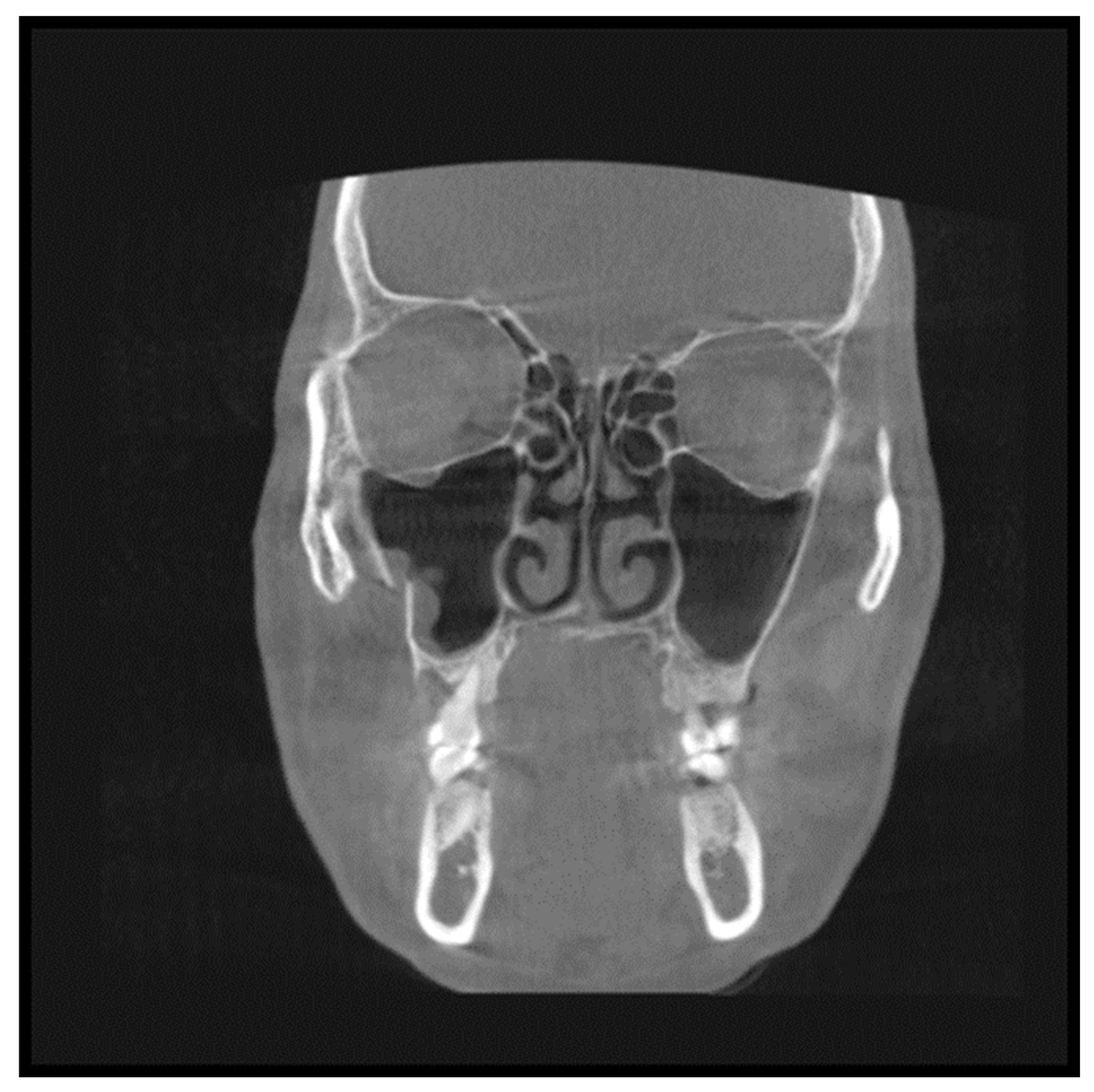
Figure 2.
View from the Coronal plane. The maxillary sinus floor shows a fracture line along the floor of the maxillary sinuses.
Figure 2.
View from the Coronal plane. The maxillary sinus floor shows a fracture line along the floor of the maxillary sinuses.
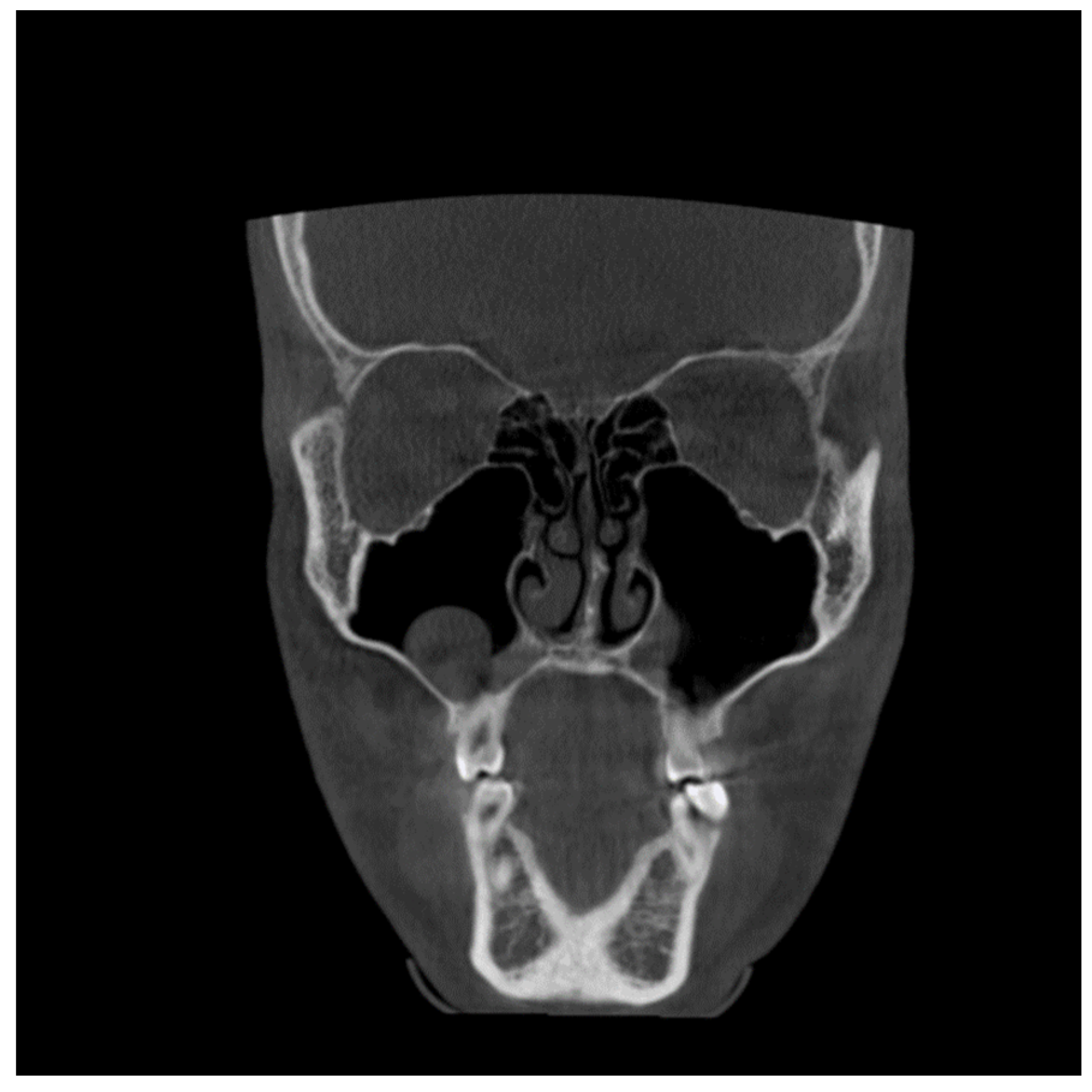
Figure 3.
View from the Coronal plane. The maxillary sinus floor shows a polypoid growth along the floor of the right maxillary sinuses.
Figure 3.
View from the Coronal plane. The maxillary sinus floor shows a polypoid growth along the floor of the right maxillary sinuses.
Figure 4.
View from the sagittal plane. The maxillary sinus floor shows thickening along the maxillary sinus floor associated with periapical infection in the maxillary molar.
Figure 4.
View from the sagittal plane. The maxillary sinus floor shows thickening along the maxillary sinus floor associated with periapical infection in the maxillary molar.
4. Discussion
CBCT, a new 3D imaging modality, could be of clinical value in screening and planning paranasal surgery. Studies reported the valuable application of CBCT for intraoperative imaging of the paranasal sinus [
9]. One of the benefits of applying CBCT for imaging of the paranasal sinuses could be the lower dose compared with CT imaging. Moreover, CBCT delivers an isotropic volume resolution facilitating the diagnosis of delicate structures in multiplanar reconstructions [
10]. The study assessed the prevalence of incidental findings in the Maxillary Sinus using cone-beam computerized tomography scans of patients referred to the department. The study showed a high prevalence of abnormalities in the Maxillary Sinus, highlighting the need to thoroughly examine the entire volume of the CBCT image, which includes the Maxillary Sinus and its associated regions.
Many studies have acknowledged that interpreting CBCT images necessitates familiarity with the anatomy of the area being investigated, comprehension of the spatial relationships within the image volume, a deep understanding of the potential diseases, anatomical variations, and abnormalities that impact the maxillofacial region, and the ability to formulate a differential diagnosis with expertise [
11].
For dental implant site assessment in the maxilla, the configuration and status of the maxillary sinus are essential to assess the available amount of bone. If a sinus lift is indicated, the visualization is helpful because the success rate of sinus lift procedures is crucially dependent on the configuration and status of the maxillary sinus [
12]. Any disease arising from dental or dentoalveolar structures could damage the floor of the maxillary sinus leading to sinusitis, known as odontogenic maxillary sinusitis (OMS). The maxillary sinus and the associated teeth are better revealed in CBCT than in periapical radiography [
13,
14].
Several studies have reported significant variability in the prevalence of incidental findings in the maxillary sinuses of asymptomatic subjects in multiplanar images [
15,
16,
17]. The CT is considered the gold standard for adequate maxillary sinus imaging because of its high resolution and ability to discern bone and soft tissue and detect sinus inflammation in approximately 30% of cases18. CBCT studies reported a prevalence of 24.6% to 56.3% [
19], whereas our research saw incidental abnormalities in 68.3%. Discrepancies in these variations may be due to several factors, such as dissimilarities in the sampling criteria, variations in image interpretation, and diagnostic criteria used.
Our study covered a wide range of age distribution; it did not include patients under 12 years since the formation of their maxillary sinus is still incomplete and specific abnormalities such as mucosal thickening and opacification are common findings in early childhood and are not indicative of sinus disease. The most detected abnormality was mucosal thickening, observed in 52.1% of cases, especially among individuals under 20 and between 20-30 years old. A study done by Rege [
20] also had a similar finding and was associated with irritation, such as odontogenic pathology or allergic phenomena.15 Nonvital posterior maxillary teeth, periodontal abscesses, retained roots, embedded, or impacted teeth, extensively carious teeth, and oroantral fistulae could be etiological factors in pathologies of odontogenic origin causing mucosal thickening [
6].
The proximity between the maxillary molar roots associated with periapical lesions and the sinus floor could influence maxillary sinus irritation [
17]. Our study demonstrated a significant relationship between periapical lesions and sinus pathology (p=0.04). The lower sinus wall was the most affected location within the sinus, which suggests a possible odontogenic involvement [
17]. The results of our study correlate with the study by Hauman et al. [
17], who demonstrated a positive correlation between periapical lesions and sinus opacification.
Odontogenic cysts were the second most frequently found inflammatory abnormality (4.3%). This result is comparable to the findings of Bosio et al. [
21] and Rhodus NL [
19] studies. These studies examined general dental patients using plain panoramic radiography and reported a prevalence ranging from 1.4% to 9.6%.
The third most frequent finding was sinus opacification, observed in six patients. The deviated nasal septum was observed in 6.3% of patients; this finding is consistent with Smith et al. 22, who found that 19.4% of their patients had a deviated septum, and 50.0% had mucosal thickening and sinus opacification, which was consistent with maxillary sinusitis.
Considering the clinical implications of sinus inflammation when installing dental implants, particularly in patients with nasal septum deviation, is essential [
23,
24]. It is crucial to carefully assess the presence or absence of opacifications in the maxillary sinus. However, it is essential to note that opacification can also result from other abnormalities such as mechanical trauma, barotraumas, and hemorrhage. Raghav M et al. [
25]. reported that opacification could even be found in asymptomatic patients as an incidental finding in 67% of cases.
One limitation of this study is the limited sample size and the need for prospective studies. We also recommend a multidisciplinary approach toward the management of such incidental findings. The present study stresses the importance of radiologists being alert and observing alterations that may not be related to the reasons for the initial examination. It is also important to note that incidental findings on radiographs should be assessed clinically as a part of proactive patient care.
5. Conclusions
The high occurrence of incidental findings in the maxillary sinus emphasizes the importance for the dentomaxillofacial radiologist to comprehensively interpret the whole volume acquired in CBCT images, including the entire sinus, while analyzing the images of routine patients. Two-dimensional imaging techniques suffer from the superimposition of anatomic structures making documentation of incidental findings in the maxillary sinus difficult. Incidental findings may be considered in the individual clinical context of signs and symptoms, reducing the risk of overestimating the real impact of radiographic findings.
6. Patents
No Patents have been filed from this study
Author Contributions
Dr. Junaid Ahmed, Dr Nandita Shenoy - "Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND Drafting the work or revising it critically for important intellectual content; AND Final approval of the version to be published; AND Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved." . Dr Aditya Gupta, Dr Sujir, Dr Archana-Drafting the work or revising it critically for important intellectual content; AND Final approval of the version to be published; AND Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of MCODS Mangalore (protocol code 14142).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of Interest
The authors declare no conflict of interest.
References
- Migas K, Kozłowski R, Sierocka A, Marczak M. Healing of Unilateral Maxillary Sinusitis by Endodontic and Periodontal Treatment of Maxillary Teeth. Medicina (Kaunas). 2022 Sep 18;58(9):1302. [CrossRef]
- Cağlayan F, Tozoğlu U. Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol. 2012 Mar-Apr;18(2):159-63. [CrossRef]
- Farman AG, Scarfe WC, van Genuchten M. Multidimensional imaging: immediate and imminent issues. Compend Contin Educ Dent 2010; 31:648–651.
- Cha JY, Mah J, Sinclair P. Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofacial Orthop 2007; 132:7–14. [CrossRef]
- Scarfe, WC. Incidental findings on cone beam computed tomographic images: A pandora’s box? Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 117(5):537-40. [CrossRef]
- Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC; American Academy of Oral and Maxillofacial Radiology. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Jun;113(6):817-26. [CrossRef]
- Nishimura T, Iizuka T: Evaluation of the pathophysiology of odontogenic maxillary sinusitis using bone scintigraphy. Int J Oral MaxillofacSurg 2002, 31:389–396. [CrossRef]
- Oberli K, Bornstein MM, Von Arx T: Periapical surgery and the maxillary sinus: radiographic parameters for clinical outcome. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 2007, 103:848–853. [CrossRef]
- Bozdemir E, Gormez O, Yıldırım D, Aydogmus Erik A. Paranasal sinus pathoses on cone beam computed tomography. J Istanb Univ Fac Dent. 2016 Jan 12;50(1):27-34. [CrossRef]
- Min CK, Kim KA. Quantitative analysis of metal artefacts of dental implant in CBCT image by correlation analysis to micro-CT: A microstructural study. Dentomaxillofac Radiol. 2021 Mar 1;50(3):20200365. [CrossRef]
- Scarfe WC, Levin MD, Gane D, Farman AG. Use of cone beam computed tomography in endodontics. Int J Dent. 2009;2009:634567. [CrossRef]
- Ulm CW, Solar P, Krennmair G, Matejka M, Watzek G. Incidence and suggested surgical management of septa in sinus-lift procedures. Int J Oral Maxillofac Implants 1995;10:462-5.
- Little R.E., Long C.M., Loehrl T.A., Poetker D.M. Odontogenic sinusitis: a review of the current literature. Laryngoscope Investig Otolaryngol. 2018;3:110–114. [CrossRef]
- Nair U.P., Nair M.K. Maxillary sinusitis of odontogenic origin: cone-beam volumetric computerized tomography-aided diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e53–e57. [CrossRef]
- Madani G, Beale TJ: Sinonasal inflammatory disease. Semin Ultrasound CT MRI 2009, 30:17–24. [CrossRef]
- Vallo J, Taipale LS, Huumonen S, Soikkonen K, Norblad A: Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Hearth Examination Survery. Oral Surg Oral Med Oral Pahtol Oral Radiol Endod 2010, 109:e80–e87. [CrossRef]
- Hauman CHJ, Chandler NP, Tong DC: Endodontic implications of the maxillary sinus: a review. Int Endod J 2002, 35:127–141. [CrossRef]
- Noorian V, Motaghi A. Assessment of the Diagnostic Accuracy of Limited CT Scan of Paranasal Sinuses in the Identification of Sinusitis. Iran Red Crescent Med J. 2012 Nov;14(11):709-12. [CrossRef]
- Rhodus NL: The prevalence and clinical significance of maxillary sinus mucous retention cysts in a general clinic population. Ear Nose Throat J 1990, 69:82–87.
- Rege IC, Sousa TO, Leles CR, Mendonça EF. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health. 2012 Aug 10;12:30. [CrossRef]
- Bósio JA, Tanaka O, Rovigatti E, Gruner SK: The incidence of maxillary sinus retention cysts in orthodontic patients. World J Orthod 2009, 10:e7–e8.
- Smith KD, Edwards PC, Saini TS, Norton NS. The prevalence of concha bullosa and nasal septal deviation and their relationship to maxillary sinusitis by volumetric tomography. Int J Dent. 2010;2010:404982. [CrossRef]
- Little R.E., Long C.M., Loehrl T.A., Poetker D.M. Odontogenic sinusitis: a review of the current literature. Laryngoscope Investig Otolaryngol. 2018;3:110–114. [CrossRef]
- Nair U.P., Nair M.K. Maxillary sinusitis of odontogenic origin: cone-beam volumetric computerized tomography-aided diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e53–e57. [CrossRef]
- Raghav M, Karjodkar FR, Sontakke S, Sansare K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp Clin Dent. 2014 Jul;5(3):361-5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).