1. Introduction
Mother´s own milk (MOM) is the gold standard nutritional source during the first months of life in both full-term and premature infants. Milk from mothers of premature newborns is adapted to the moment of the infants´ birth, containing higher levels of immunological and anti-inflammatory factors (e.g. lactoferrin), and of protein, sodium, fat and minerals such as calcium or phosphorus. Premature newborns absorb a very high percentage of lipids from MOM (90%) and have higher energy requirements than full-term newborns (58-70 Kcal/dl vs 48-64 Kcal/dl), with very important contribution of long-chain polyunsaturated fatty acids (LC-PUFA), such as docosahexaenoic acid and arachidonic acid energy intake is higher than in a full-term newborn (58-70 Kcal/dl vs 48-64 Kcal/dl) (1-3). Very preterm infants fed with mother’s own milk (MOM) have lower rates of neonatal morbidity and improved long-term metabolic and neurocognitive outcomes (4-6). Health teams working in neonatal intensive care unit (NICU) should provide support to mothers of premature newborns to facilitate milk consumption, her presence for newborn and establishing the kangaroo method as early as possible (7-11).
The vast majority of premature newborns initially require donated human milk (DHM) probably due to maternal stress from the premature birth. DHM is pasteurized in the donated human milk banks. The potential mechanisms by which DHM reduces necrotizing enterocolitis (NEC) (12) include reduced exposure to bovine antigens and the effects of functional components such as lactoferrin and human milk oligosaccharides, which may act positively on gut microbiota (13-15).
The mother´s microbiota colonizes the child from the intestinal bacteria during pregnancy with bacteria present in the birth canal, including the vaginal and perianal area, and bacteria from the skin and in MOM. This process favors adequate colonization by harmless microorganisms that protect the newborn from pathogens. Adequate and diverse colonization positively influences immune, metabolic, cognitive, and sensory development of the newborn (16-18). The intestinal microbiota of the newborn is influenced by diet. The bacterial phyla most frequently found in MOM include Firmicutes, Bacterioidetes, Actinobacteria, and Proteobacteria, closely resembling the make-up of the mother’s intestinal bacteria. MOM also contains skin bacteria such as Streptococcus and Staphylococcus. Complex carbohydrates present in the MOM promote the development of Bifidobacterium, which are the dominant species in the newborn intestine, and delay the implantation of enterobacteria. Infants fed with artificial formula have higher levels of Enterobacteria and lower levels of Bifidobacterium (19-23).
There is a dearth of studies assessing the effect of maternal stress on the gut microbiota of mothers of very premature newborns: most studies of prenatal stress have been conducted in animal models. Although rarely taken into account, maternal stress is an important factor, whose appearance and inadequate management could lead to a poor establishment of breastfeeding or even alter the production or modify the composition of breast milk. We examined the association between postnatal maternal stress and production and composition of breast milk with the process of bacterial colonization of the intestine of very premature infants. (24-29).
2. Material and methods
2.1. Study design
This prospective observational study was carried out over a 2-year period, from May 1, 2019 to April 30, 2021, at the NICU of the level III Clinical University Hospital of Santiago de Compostela. The study included premature newborns weighing less than 1500 grams and/or less than 32 weeks of gestational age (GA) who were breastfed and their mothers. The follow-up of both mothers and neonates spanned the first 15 days of the newborn’s life. The study was approved by the local ethics committee (registration code 2019/229) and data were collected in an encrypted manner in a database.
2.2. Inclusion and exclusion criteria
The following inclusion criteria were applied: all premature newborns ≤32 weeks GA and/or ≤1500 g body weight and their mothers, who specified the intention of breastfeeding and provided written informed consent (IC) to participate in the study. The exclusion criteria were as follows: newborns whose participation in the study was not compatible due to their very serious pathologies that did not make it possible to receive MOM; mothers who intend to give their own milk but abandoned to breastfeed in the 15 first days of life.
2.3. Study population
Study population consisted of 52 premature newborns with a GA ≤32 weeks and/or bodyweight ≤1500 g, and their 45 mothers, who provided written informed consent and breastfed their newborns (
Supplementary Figure S1). The following data were collected:
- -
Sociodemographic data: mother’s age (≥35 years and <35 years); educational level (primary, secondary, higher); type of delivery (vaginal or cesarean section); GA; twinhood; newborn sex and bodyweight.
- -
Data on the clinical status of premature newborns: respiratory support (invasive mechanical ventilation [IMV], non-invasive mechanical ventilation [NIMV]) required or not; hemodynamically significant patent ductus arteriosus; sepsis; antibiotics received by newborn; antibiotics received by mother prior to delivery; days of parenteral nutrition; complete enteral nutrition; degree of feeding tolerance; start date of milk fortification; and evolution of newborn’s bodyweight.
- -
Initiation of kangaroo method: early (from birth to ≤4 days), intermediate (5-7 days), or late (≥ 8 days).
- -
Exposure to stress in mothers of premature newborns, measured using the parental stress scale (PSS: NICU).
- -
Breast milk parameters, determined by nutritional analysis and study of microbiota.
- -
Fecal calprotectin (FC) and microbiota, evaluated in fecal samples from premature newborns.
Data were collected from mothers and newborns on days 3, 7 and 15 after birth.
2.4. Outcome measures
2.4.1. Anthropometric assessment
Weight was measured accurate to the nearest 10 g. Measurements were taken by the same researcher in duplicate to minimize intra-observer bias. Weight percentiles were calculated using the Fenton scale.
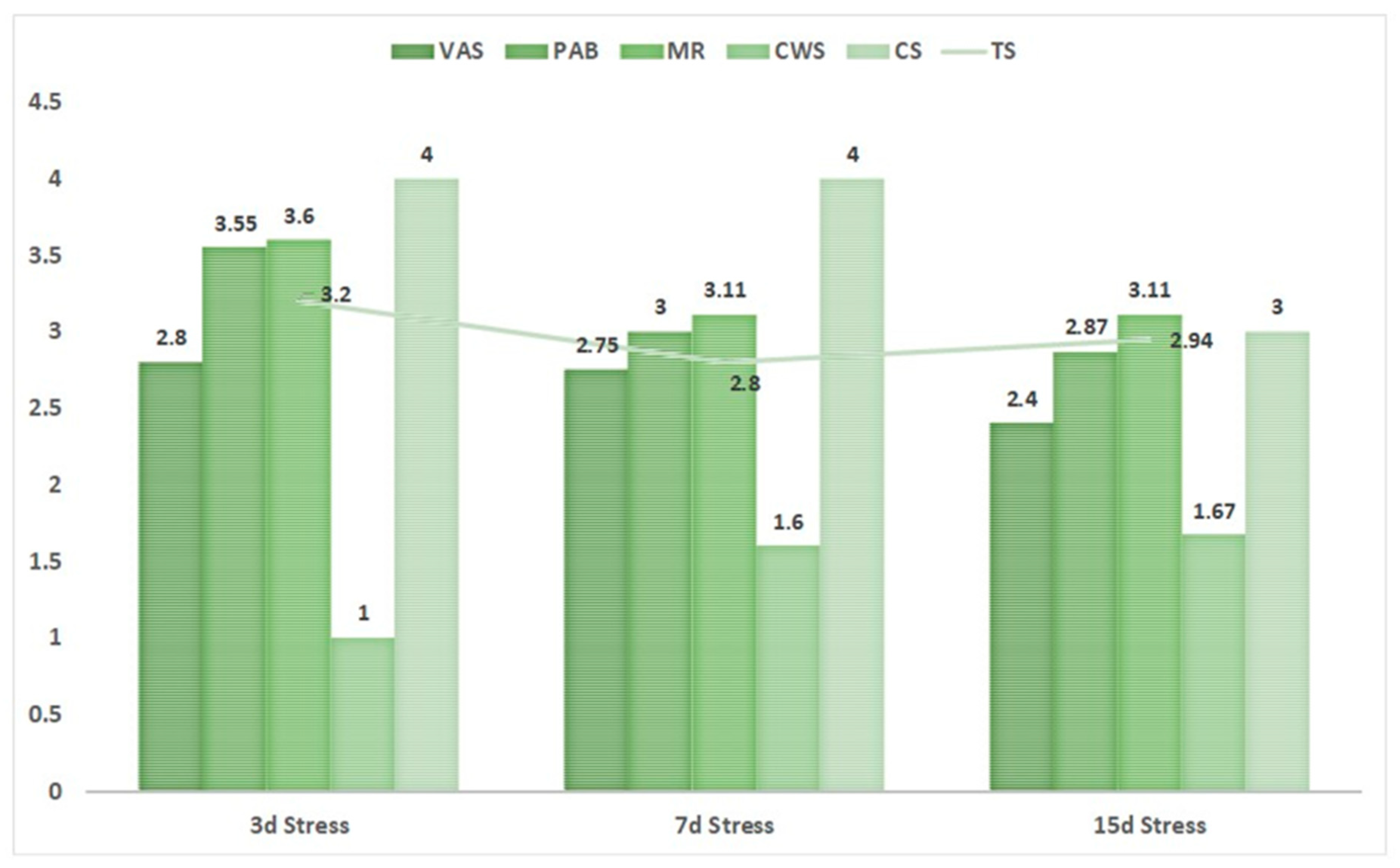
2.4.2. Parental Stress Scale
To quantify stress in mothers of preterm infants, the PSS:NICU (30-33) was used. This consists of 5 subscales: (i) visual and auditory stimuli (VAS) in the NICU which is the stress generated by what they see and hear; (ii) physical appearance and behavior of the newborn (PAB) which is the stress generated by the physical appearance and behavior of the newborn; (iii) mother’s relationship with the newborn and maternal role (MR) defined as the stress caused by the individual perception of her role as mother and the establishment of the maternal bond; (iv) communication with health personnel (CWS) which is the stress generated by the relationship with the health personnel; (v) common stress (CS) defined as the individual perception of stress to which the mother is subjected. The complete scale consists of a total of 46 items, each of which is rated by the user using a 5-point Likert scale, where 1 corresponds to no stress and 5 to extremely stressful. The overall score of the 46 items is weighted to obtain a total stress (TS) rating. The total stress experienced by the mother was defined as high or low depending on whether it was above or below the median value on 3, 7, and 15 days after birth of the newborn.
2.4.3. Nutritional analysis of macronutrients in MOM
A 5-ml sample of fresh MOM was collected on days 3, 7, and 15 after birth of the newborn and its nutritional content (proteins, fats, and carbohydrates) was analyzed using the human milk analyzer with FTIR technology (MilkoSkan Mars, FOSS, Denmark) (34). MOM samples were collected directly from milk expressed by the mother in the morning when she attended the neonatal intensive care unit (NICU) using a breast pump. MOM that is extracted manually can have a higher fat content than milk extracted using a breast pump (35). This was taken into account when collecting the samples, and the same process was used to collect all samples to avoid variation. MOM was collected in a sterile bottle, homogenized by shaking it several times and heated in a water bath for immediate analysis. The analyzer used for the measurement underwent daily calibration before carrying out the macronutrient analysis.
2.4.4. FC
Stool samples for FC analysis were collected from the newborn’s diaper on days 3, 7, and 15 days after birth, and the sample immediately stored in a refrigerator for subsequent analysis by solid phase microplate enzyme immunoassay (ELISA).
2.4.5. Analysis of microbiota in newborn stool and MOM
Stool samples were collected directly from the diaper using a spatula and placed in a sterile recipient. To collect MOM samples, the nipple area of the breast was washed with soap and water and approximately 1 ml of milk extracted using a breast pump and collected in sterile plastic jar. The samples were frozen at -80ºC in tubes with screw caps for subsequent processing and analysis. Nucleic acid extraction was carried out using the Maxwell® RSC instrument with the Maxwell® RSC PureFood GMO and Authentication kit. Once genomic material was obtained, DNA was quantified using Qubit DNA Assay (Thermo Fisher®). The microbiota was analyzed using the MiSeq sequencer to carry out the 16s microbiome protocol. The results were analyzed using Illumina BaseSpace together with the 16S Metagenomics application (36-38).
The Shannon index was used as an indicator to quantify biodiversity. A value of zero indicates the presence of a single species: the higher the index, the greater the diversity of species (39,40).
2.5. Statistical analyses
Data were analyzed using the statistical package IBM SPSS Statistics version 20.0. The normality of the quantitative variables was assessed using the Shapiro-Wilk test. Variables are presented as the median and interquartile range.
Statistical analyses were carried out using the non-parametric Mann-Whitney U test for quantitative variables, the chi-squared test for qualitative variables, and the non-parametric Kruskal Wallis test for comparison of 3 or more variables. The possible relationship between variables was studied using the Spearman correlation test or through univariate or multivariate linear regression studies.
In all the comparisons of variables, statistical significance was set at p ≤ 0.05.
3. Results
3.1. Characteristics of the study participants
Table 1 shows data for participating mothers and their infants. The study population consisted of 45 mothers and 52 very preterm newborns (24 females and 28 males) who met the inclusion criteria for the study. In newborns, there were no significant differences in sex distribution between groups. The mean percentile of weight decreased from P33 at birth to P15 at 3 days of life, after which bodyweight increased on the 15th percentile. Implementation of the kangaroo method was early or intermediate in 69.23% (36/52) of cases. Tolerance to enteral feeding among neonates was generally good, with complete enteral nutrition established at 15 days of life in 92.31% (48/52) of newborns.
Median FC levels decreased with age and were higher at 7 days of life in newborns who did not receive antibiotics (p=0.027) and newborns weighing <1000 g at birth (p=0.044).
F, female; FC, fecal calprotectin; g, grams; M, male; n, number; y, years; w, week.
The common stress (CS) was 4 at days 3 and 7, indicating a very stressful situation, and decreased to 3 at day 15. Analysis of the individual subscales showed the highest stress scores for the MR subscale (
Figure 1).
Table 2 shows significant associations between stress scores and other mother or newborn-related variables.
The earlier the kangaroo method was established, the greater the reduction in stress. Stress levels among mothers were very high over the first 3 days post-delivery, while MOM production over this period was very low. On day 7 post-delivery, stress levels decreased, and milk production increased, and continued to do so over the following days, although stress levels increased slightly.
Stress management was poorer in the group of mothers that had completed only primary education versus those that had completed secondary or higher education. In the latter group, stress levels decreased sooner after delivery, with significant decreases observed at 7 and 15 versus 3 days (
Table 2).
3.2. Macronutrient content in MOM
As expected, median levels of MOM macronutrients increased over time, especially fats and carbohydrates. Lipid levels were 1.79 g/dl, 3.16 g/dl, and 3.27 g/dl at 3, 7, and 15 days, respectively, and carbohydrates levels were 6.55 g/dl, 6.85 g/dl, and 7.19 g/dl at 3, 7, and 15 days, respectively. We observed no association between the levels of macronutrients and maternal stress during the study period.
3.3. Microbiota in MOM and neonatal stool samples
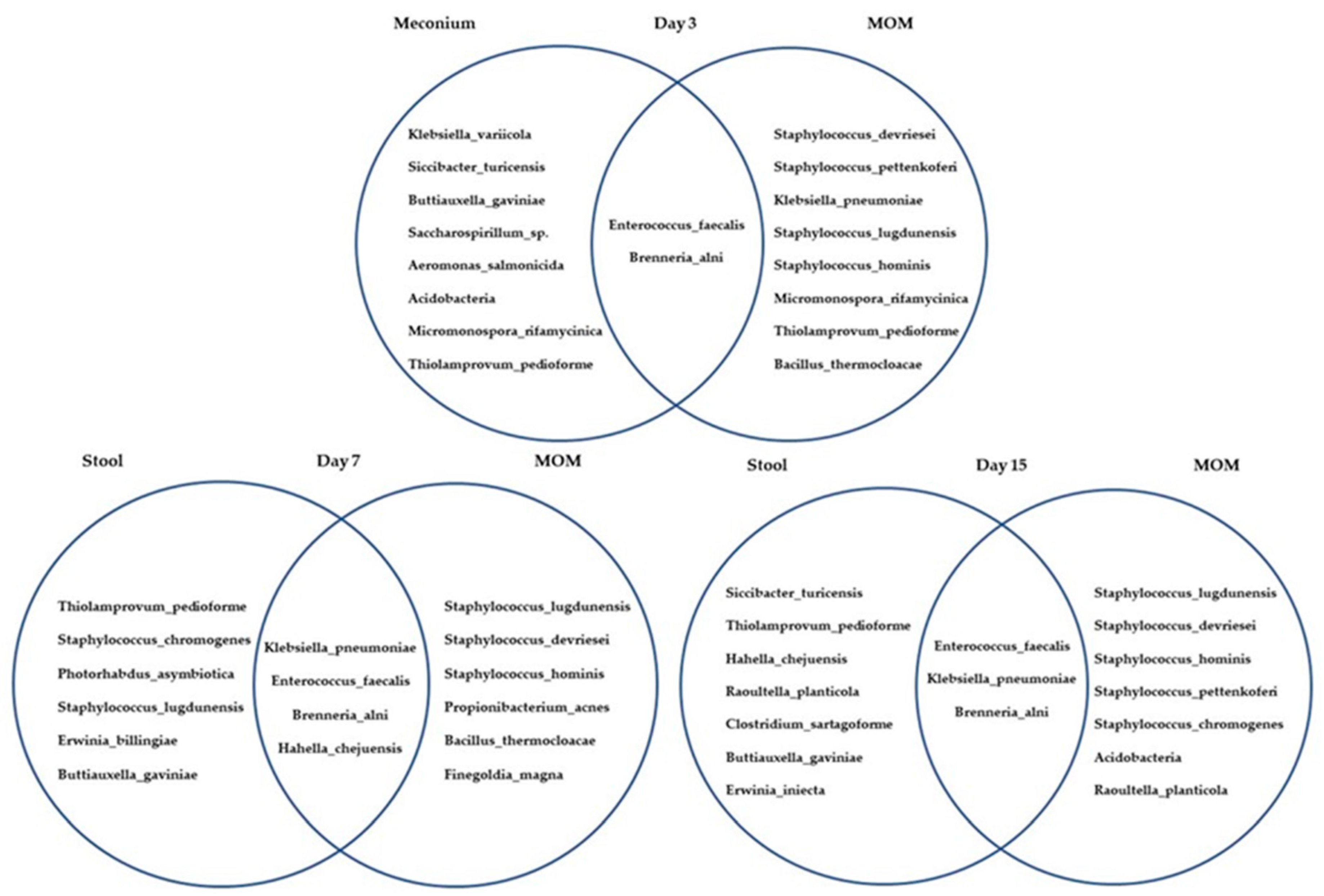
The Venn diagrams in
Figure 2 depict the microbiota of MOM and neonatal stool samples collected at days 3, 7, and 15 post-delivery.
The bacteria detected in MOM samples included microorganisms commonly found on the skin
(Staphylococcus,
Streptococcus,
Bacillus) and in the intestinal microbiota (
Klebsiella,
Clostridium or
Enterococcus). Bacteria found in neonatal fecal samples primarily consisted of species commonly found in the intestinal microbiota (
Clostridium,
Enterobacter,
Enterococcus,
Klebsiella). We investigated the association between microbial diversity in MOM and neonatal stool samples with maternal stress at days 3, 7, and 15 post-delivery (
Table 3). Stress was defined as low or high according to the median value at each day. Although the results were not statistically significant, a trend towards greater microbial diversity (i.e. a higher Shannon index) was observed in milk from mothers with continually decreasing maternal stress over the study. The pattern observed for fecal samples was more erratic, although we observed a similar trend to that of breast milk at 15 days.
The proportion of Proteobacteria, Firmicutes, Actinobacteria and Bacteroidetes was analyzed in the MOM and neonatal fecal samples 3, 7, and 15 days post-delivery (
Table 4).
Although the effect was not significant, we observed a greater proportion of Proteobacteria in neonatal fecal samples. Species of the phylum Firmicutes predominated in MOM. In milk samples from high-stress mothers we observed a trend over the course of the study period towards decreasing proportions of Firmicutes (87.5%, 62.5%, and 55.6% on days 3, 7, and 15, respectively) and increasing proportions of Proteobacteria (12.5%, 37 .5%, and 44.4% on days 3, 7, and 15, respectively). The opposite effect was observed in MOM samples from low-stress mothers (
Table 5).
We observed a trend towards greater biodiversity in stool samples collected 7 days post-delivery from neonates who received complete enteral nutrition. Relative proportions of bacteria from the phyla Proteobacteria, Firmicutes, Actinobacteria and Bacteroidetes (52.94%, 35.29%, 5.88%, 5.88%, respectively) were higher in neonates who received complete enteral nutrition compared to those who did not. Indeed, in the latter group bacteria from the phyla Actinobacteria and Bacteroidetes were completely absent.
4. Discussion
This study of very premature newborns and their mothers describes the negative effects of maternal stress on MOM production and on the bacterial biodiversity of both milk and the neonatal intestinal microbiota, but shows that stress does not affect the macronutrient composition of milk.
4.1. Parental stress and MOM
Parental stress, if improperly managed, can lead to states of anxiety and depression in mothers, with significant negative impacts at both the personal and family level. High levels of parental stress following the birth of a very premature child can result in suboptimal bonding between mother and child, and is a risk factor for poor behavioral and social development in childhood (3, 7, 8, 9). In our study population, total stress in mothers of preterm infants decreased between 3 and 7 days post-delivery, subsequently increasing slightly at 15 days, possibly coinciding with the appearance of prematurity-associated complications in the newborn. In line with previously reported findings (33), the stress subscale for which the highest scores were observed was MR, with mean scores of 3.6 (day 3), 3.11 (day 7), and 3.11 (day 15). This subscale assesses stress related to the mother-child bond, including stress resulting from mother-child separation. It should also be noted that this study was carried out during the COVID-19 pandemic, and the resulting impact on hospital care in particular and society in general may have contributed to additional stress among mothers of premature newborns (41,42).
Situations of stress lead to increases in cortisol, adrenaline, dopamine, and other mediators of stress, and inhibition of prolactin and oxytocin, hormones central to the production and secretion of milk (43,44). We observed a statistically significant inverse relationship between stress and milk production 3 days post-delivery. However, this effect was not significant at 7 or 15 days post-delivery, possibly because the initial stress caused by preterm labor decreases, and mothers focus on breastfeeding their newborn, which in turn has a stress-reducing effect as it favors the release of hormones such as oxytocin (44). We show that maternal stress is significantly reduced if the kangaroo method is established early (≤4 days post-delivery). Provision of psychological and emotional support to mothers of premature newborns should be implemented in all NICUs.
Our findings indicate better stress management in mothers with a higher educational level, possibly because they have access to greater social and emotional support, which allows them to better manage their stress levels (45).
In line with the results of other studies (46,47), maternal stress did not alter the macronutrient content of MOM (46,47). Other authors have reported that in conditions of acute stress, in which cortisol levels increase, milk contains lower levels of carbohydrates and higher levels of fat, while in chronic stress conditions, fat levels in milk decrease (48).
4.2. FC, microbiota, MOM and maternal stress
FC is a protein that reflects the migration of neutrophils to the intestinal lumen and can serve as a biomarker of intestinal inflammation in adults, although in children conclusive FC values to establish a reference range are lacking (49,50). FC levels appear to be linked to the maturity of the digestive system, resulting in higher levels in full-term and preterm newborns than in adults but with similar values between preterm and term newborn (51). Multiple factors could explain the elevation of FC in the first days of life, including the intrauterine environment, immaturity of the intestine, possible hypoxic-ischemic damage to the intestinal mucosa, and even bacterial colonization of the intestine (52). FC levels decrease over the following days, often due to the antibiotic treatment that preterm newborns undergo, which may delay intestinal colonization. When enteral feeding is established, FC concentrations rise again, and subsequently decrease within a few days in the absence of any pathology (53,54). It is difficult to specify FC levels that are indicative of intestinal disease in premature infants owing to the marked variability in this parameter, which is influenced by multiple factors. However, research continues to investigate how FC could serve as a marker to facilitate detection of potentially fatal gastrointestinal disorders of premature newborns, such as NEC.
Bacteria found in the MOM microbiota included skin microorganisms (Staphylococcus, Streptococcus, Bacillus) and bacteria present in the intestinal microbiota (Klebsiella, Clostridium, or Enterococcus), while those found in newborn fecal samples largely corresponded to the intestinal microbiota (Clostridium, Enterobacter, Enterococcus, Klebsiella). The species that predominate in newborn fecal samples were Enterococcus faecalis, E. coli, Klebsiella spp and Staphylococcus spp, with Lactobacillus and Bifidobacteria detected in small amounts. Prenatal or postnatal stress can also influence the newborn intestinal microbiota, and it is also likely that individual genetic factors modulate the effects of this stress (19-23).
The present study describes the effects of maternal stress on the diversity of microorganisms in MOM, and points to a trend towards reduced biodiversity with a lower Shannon index, in situations of greater stress. However, at days 3 and 7 post-delivery, when maternal stress levels were higher, microbial diversity in neonatal fecal samples was increased. This may be explained by intestinal dysbiosis resulting from stress, which allow bacteria not typically found in the normal microbiota to proliferate abnormally, hence increasing diversity. In infants born to mothers with higher stress levels from days 3 to 15, we observed a progressive increase in the proportion of Proteobacteria species (33.3%, 40%, and 70% on days 3, 7, and 15, respectively), while the opposite effect was observed for Firmicutes species ((66.7%, 40%, and 20% on days 3, 7, and 15, respectively). In milk from mothers who experienced high levels of stress, the proportion of Firmicutes species was greater than that of Proteobacteria species at all 3 timepoints studied, but progressively decreased over time (87.5%, 62.5%, and 55.6%, respectively), while the proportion of Proteobacteria species increased (12.5%, 37.5%, and 44.4%, respectively).
Some limitations of the present study should be noted. The study was carried out during the COVID pandemic, which may have affected the reported outcomes: fear of contagion may have influenced perceived levels of maternal stress and decreased rates of breastfeeding. In some cases, it was impossible to obtain complete data for all study participants. The study’s main strength is its analysis of how stress influences establishment of correct breastfeeding and intestinal colonization of the premature newborn.
5. Conclusions
We show that maternal stress clearly influences the bacterial biodiversity in the milk of mothers and in fecal samples from their premature newborns. This in turn affects the establishment of a healthy intestinal microbiota, which is required for adequate development and health of the premature newborn. Maternal stress, particularly that relating to the role of the mother, is a variable that must be taken into account in NICUs to ensure appropriate control and management, thereby increasing the production of milk and the bacterial biodiversity of both milk and the intestinal microbiota of the newborn.
Measures must be established to control maternal stress during the perinatal period. Although certain independent social variables (e.g. higher educational level) favor better stress control, additional measures can be applied in the NICU: as shown here, early initiation of the kangaroo method allows more rapid control of stress caused by the separation from their prematurely newborn.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org, (Supplementary Figure S1: Flow chart depicting recruitment of the study cohort)
Author Contributions
MCFT designed the study, collected data, carried out the statistical analyses, and drafted the manuscript. APM designed the study, collected and analyzed the data, and drafted the manuscript. MLC designed the study, obtained funding and revised the manuscript. RTP and MLPM carried out the microbiological analyses and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This research was funded by Next Generation EU funds, Maternal and Child Health and Development Research Network (RICORS-SAMID), Institute of Health Carlos III (ISCIII), under the framework of the Project: "Primary Care Interventions to prevent maternal and child chronic diseases of perinatal and developmental origin" (Ref: RD21/ 0012)
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am 2013; 60(1): 49-74. [CrossRef]
- Kramer, MS. "Breast is best": The evidence. Early Hum Dev 2010; 86(11): 729-32. [CrossRef]
- Kim SY, Yi DY. Components of human breast milk: from macronutrient to microbiome and microRNA. Clin Exp Pediatr 2020; 63(8): 301-309. [CrossRef]
- Sadauskaite-Kuehne V, Ludvigsson J, Padaiga Z, Jasinskiene E, Samuelsson U. Longer Breastfeeding in an independent predictive factor against development of type 1 diabetes in chilhood. Diabetes Metab Res Rev. 1: 2004; 20 (2), 2004.
- Hatmal MM, Al-Hatamleh MAI, Olaimat AN, Alshaer W, Hasan H, Albakri KA, et al. Immunomodulatory Properties of Human Breast Milk: MicroRNA Contents and Potential Epigenetic Effects. Biomedicines 2022; 10(6): 1219. [CrossRef]
- Shah KB, Chernausek SD, Garman LD, Pezant NP, Plows JF, Kharoud HK, et al. Human Milk Exosomal MicroRNA: Associations with Maternal Overweight/Obesity and Infant Body Composition at 1 Month of Life. Nutrients 2021; 13(4): 1091. [CrossRef]
- Sivanandan S, Sankar MJ. Kangaroo mother care for preterm or low birthweight infants: a systematic review and meta-analysis. BMJ Glob Health 2023; 8(6): e010728. [CrossRef]
- Conde-Agudelo A, Díaz-Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2016 Aug 23; 2016(8): CD002771. [CrossRef]
- Adejuyigbe EA, Agyeman I, Anand P, Anyabolu HC, Arya S, Assenga EN, et al. Evaluation of the impact of continuous Kangaroo Mother Care (KMC) initiated immediately after birth compared to KMC initiated after stabilization in newborns with birthweight 1.0 to . [CrossRef]
- Cristóbal-Cañadas D, Parrón-Carreño T, Nievas-Soriano BJ. Effect of the Kangaroo Mother Method after Preterm Delivery on Maternal Stress and Anxiety in the Context of the COVID-19 Pandemic-A Cohort Study. Int J Environ Res Public Health 2022; 19(24): 16432. [CrossRef]
- Samsudin S, Chui PL, Kamar ABA, Abdullah KL. Maternal Kangaroo care education program in the neonatal intensive care unit improved mothers’ perceptions, knowledge, perceived barriers and stress relates to premature infant. Nurs Open 2023; 10(1): 349-357. [CrossRef]
- Cañizo Vázquez D, Salas García S, Izquierdo Renau M, Iglesias-Platas I. Availability of Donor Milk for Very Preterm Infants Decreased the Risk of Necrotizing Enterocolitis without Adversely Impacting Growth or Rates of Breastfeeding. Nutrients 2019; 11(8): 1895. [CrossRef]
- Charbonneau MR, O’Donnell D, Blanton LV, Totten SM, Davis JC, Barratt MJ, et al. Sialylated Milk Oligosaccharides Promote Microbiota-Dependent Growth in Models of Infant Undernutrition. Cell 2016; 164(5): 859-71. [CrossRef]
- Masi AC, Embleton ND, Lamb CA, Young G, Granger CL, Najera J, et al. Human milk oligosaccharide DSLNT and gut microbiome in preterm infants predicts necrotising enterocolitis. Gut 2021; 70(12): 2273-2282. [CrossRef]
- Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol 2017; 44(1): 193-207. [CrossRef]
- Ahearn-Ford S, Berrington JE, Stewart CJ. Development of the gut microbiome in early life. Exp Physiol 2022; 107(5): 415-421. [CrossRef]
- Neves LL, Hair AB, Preidis GA. A systematic review of associations between gut microbiota composition and growth failure in preterm neonates. Gut Microbes 2023; 15(1): 2190301. [CrossRef]
- Stricker S, Hain T, Chao CM, Rudloff S. Respiratory and Intestinal Microbiota in Pediatric Lung Diseases-Current Evidence of the Gut-Lung Axis. Int J Mol Sci 2022; 23(12): 6791. [CrossRef]
- Wang K, Xia X, Sun L, Wang H, Li Q, Yang Z, et al. Microbial Diversity and Correlation between Breast Milk and the Infant Gut. Foods 2023; 12(9): 1740. [CrossRef]
- Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol Mol Biol Rev 2017; 81(4): e00036-17. [CrossRef]
- Vandenplas Y, Carnielli VP, Ksiazyk J, Luna MS, Migacheva N, Mosselmans JM, et al. Factors affecting early-life intestinal microbiota development. Nutrition 2020; 78: 110812. [CrossRef]
- Notarbartolo V, Giuffrè M, Montante C, Corsello G, Carta M. Composition of Human Breast Milk Microbiota and Its Role in Children’s Health. Pediatr Gastroenterol Hepatol Nutr 2022; 25(3): 194-210. [CrossRef]
- Li Y, Ren L, Wang Y, Li J, Zhou Q, Peng C, et al. The Effect of Breast Milk Microbiota on the Composition of Infant Gut Microbiota: A Cohort Study. Nutrients 2022; 14(24): 5397. [CrossRef]
- Weiss SJ, Hamidi M. Maternal stress during the third trimester of pregnancy and the neonatal microbiome. J Matern Fetal Neonatal Med 2023; 36(1): 2214835. [CrossRef]
- Yeramilli V, Cheddadi R, Shah J, Brawner K, Martin C. A Review of the Impact of Maternal Prenatal Stress on Offspring Microbiota and Metabolites. Metabolites 2023; 13(4): 535. [CrossRef]
- Ziomkiewicz A, Apanasewicz A, Danel DP, Babiszewska M, Piosek M, Orczyk-Pawiłowicz M. Maternal Distress and Social Support Are Linked to Human Milk Immune Properties. Nutrients 2021; 13(6): 1857. [CrossRef]
- Juncker HG, Naninck EFG, Schipper L, Lucassen PJ, van Goudoever JB, de Rooij SR, et al. Maternal stress in the postpartum period is associated with altered human milk fatty acid composition. Clin Nutr 2022; 41(11): 2517-2528. [CrossRef]
- Nagel EM, Howland MA, Pando C, Stang J, Mason SM, Fields DA, et al. Maternal Psychological Distress and Lactation and Breastfeeding Outcomes: a Narrative Review. Clin Ther 2022; 44(2): 215-227. [CrossRef]
- Zijlmans MA, Korpela K, Riksen-Walraven JM, de Vos WM, de Weerth C. Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology 2015; 53: 233-45. [CrossRef]
- Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. 1: Nurs Res 1993; 42(3), 1993.
- Kubicka Z, Fiascone J, Williams D, Zahr E, Ditzel A, Perry D, et al. Implementing modified family integrated care in a U.S. neonatal intensive care unit: nursing perspectives and effects on parents. J Perinatol 2023; 43(4): 503-509. [CrossRef]
- Dudek-Shriber, L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occup Ther 2004; 58(5): 509-20. [CrossRef]
- Caruso A, Mikulic IM. El estrés en padres de bebés prematuros internados en la Unidad de Cuidados Intensivos Neonatales: traducción y adaptación de la escala Parental Stressor Scale: Neonatal Intensive Care Unit (PSS: NICU - M.S. Miles y D. Holditch Davis, 1987; M.S. Miles y S.G. Funk, 1998). Anuario de Investigaciones [Internet]. 2012; XIX:19-26. https://www.redalyc.org/articulo.oa? 3691.
- Fusch G, Rochow N, Choi A, Fusch S, Poeschl S, Obianuju Ubah A, et al. Rapid measurement of macronutrients in breast milk: How reliable are infrared milk analyzers? 4: Clin Nutrition 2015; 34, 2015.
- Mangel L, Ovental A, Batscha N, Arnon M, Yarkoni I, Dollberg S. Higher fat content in Breastmilk expressed manually: a randomized trial. 3: Breastfeeding Medicine 2015; 10 (7), 2015.
- Alarcón Cavero T, Dauria G, Delgado Palacio S, Del Campo Moreno R, Ferrer Martínez M. Microbiota. Procedimientos en Microbiología Clínica. Recomendaciones de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica [Internet]. Madrid: Cercenado Mansilla E; 2016 [revised 2016; cited 2023]. Available from: https://seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimientomicrobiologia59mod.
- López Causapé C, González Candelas F, Tomás Carmona M, Oliver Palomo A. Aplicaciones de las técnicas de secuenciación masiva en la Microbiología Clínica. Recomendaciones de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica [Internet]. Madrid: Cercenado Mansilla E; 2021 [revised 2021; cited 2023]. Available from: https://seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimiento71.
- 16S Metagenomic Sequencing Library Preparation [Internet]. 2013 [cited 2023]. Available from: https://support.illumina.com/documents/documentation/chemistry_documentation/16s/16s-metagenomic-library-prep-guide-15044223-b.
- Pla, L. Biodiversidad: Inferencia basada en el índice de Shannon y la riqueza. INCI [Internet]. 2006 [cited 2023]; 31 (8): 583-590. Available from: http://ve.scielo.org/scielo.php? 0378. [Google Scholar]
- Haegeman B, Hamelin J, Moriarty J, Neal P, Dushoff J, Weitz JS. Robust estimation of microbial diversity in theory and in practice. ISME J 2013; 7(6): 1092-101. [CrossRef]
- Ionio C, Ciuffo G, Landoni M. Parent-Infant Skin-to-Skin Contact and Stress Regulation: A Systematic Review of the Literature. Int J Environ Res Public Health 2021; 18(9): 4695. [CrossRef]
- Cristóbal-Cañadas D, Parrón-Carreño T, Nievas-Soriano BJ. Effect of the Kangaroo Mother Method after Preterm Delivery on Maternal Stress and Anxiety in the Context of the COVID-19 Pandemic-A Cohort Study. Int J Environ Res Public Health 2022; 19(24): 16432. [CrossRef]
- Dewey, KG. Maternal and fetal stress are associated with impaired lactogenesis in humans. J Nutr 2001; 131(11): 3012S-5S. [CrossRef]
- Nagel EM, Howland MA, Pando C, Stang J, Mason SM, Fields DA, et al. Maternal Psychological Distress and Lactation and Breastfeeding Outcomes: a Narrative Review. Clin Ther 2022; 44(2): 215-227. [CrossRef]
- Fang Y, Boelens M, Windhorst DA, Raat H, van Grieken A. Factors associated with parenting self-efficacy: A systematic review. J Adv Nurs 2021; 77(6): 2641-2661. [CrossRef]
- Palnizky Soffer G, Siri M, Mangel L, Mandel D, Lubetzky R. Impact of Maternal Anxiety on Human Milk Macronutrients Content: A Prospective Observational Study. Breastfeed Med 2020; 15(9): 572-575. [CrossRef]
- Ryoo CJ, Kang NM. Maternal Factors Affecting the Macronutrient Composition of Transitional Human Milk. Int J Environ Res Public Health 2022; 19(6): 3308. [CrossRef]
- Ziomkiewicz A, Babiszewska M, Apanasewicz A, Piosek M, Wychowaniec P, Cierniak A, et al. Psychosocial stress and cortisol stress reactivity predict breast milk composition. Sci Rep 2021; 11(1): 11576. [CrossRef]
- Li F, Ma J, Geng S, Wang J, Liu J, Zhang J, Sheng X. Fecal calprotectin concentrations in healthy children aged 1-18 months. PLoS One 2015; 10(3): e0119574. [CrossRef]
- Campeotto F, Butel MJ, Kalach N, Derrieux S, Aubert-Jacquin C, Barbot L, et al. High faecal calprotectin concentrations in newborn infants. Arch Dis Child Fetal Neonatal Ed 2004; 89(4): F353-5. [CrossRef]
- Kapel N, Campeotto F, Kalach N, Baldassare M, Butel MJ, Dupont C. Faecal calprotectin in term and preterm neonates. J Pediatr Gastroenterol Nutr 2010; 51(5): 542-7. [CrossRef]
- Rougé C, Butel MJ, Piloquet H, Ferraris L, Legrand A, Vodovar M, et al. Fecal calprotectin excretion in preterm infants during the neonatal period. PLoS One 2010; 5(6): e11083. [CrossRef]
- Groer M, Ashmeade T, Louis-Jacques A, Beckstead J, Ji M. Relationships of Feeding and Mother’s Own Milk with Fecal Calprotectin Levels in Preterm Infants. Breastfeed Med 2016; 11(4): 207-12. [CrossRef]
- Park JS, Cho JY, Chung C, Oh SH, Do HJ, Seo JH, et al. Dynamic Changes of Fecal Calprotectin and Related Clinical Factors in Neonates. Front Pediatr 2020; 8: 326. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).