Submitted:
17 September 2023
Posted:
19 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
- Present a detailed comparison of existing studies, mainly focusing on integrating ICT technologies in healthcare, an important SDG, in terms of sustainable aspects, security and privacy challenges, design and integration challenges, E-health related applications, and future directions.
- Present an overview of the need for digital transformation in healthcare, discuss its significant components, highlight E-health’s importance and benefits, explore its integration and design challenges and categorise the security and privacy challenges.
- Present in-depth discussion on the role of Blockchain technology in E-health, discussing Blockchain technology and its characteristics, highlighting its benefits, and describing the possible types of Blockchain-based E-health use cases.
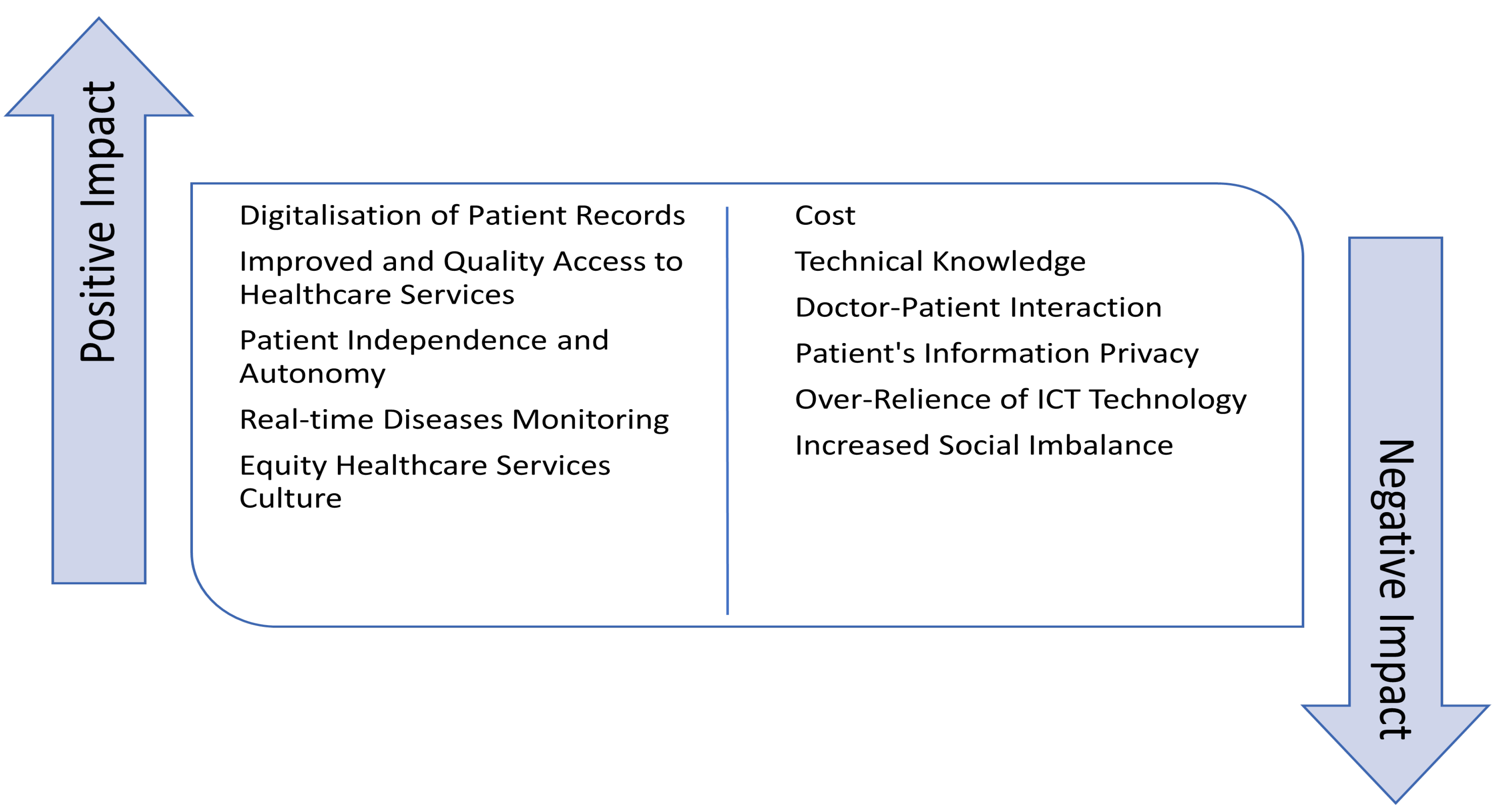
- Discuss the positive and negative impact of ICT integration, including Blockchain technology, into the health systems.
- Identify open issues and challenges of integrating ICT technologies into the healthcare systems and discuss future research directions, which provide the strength for researchers to address the issues in future solutions.
2. Methodology of Our Study
- Development of Study design based on the literature review on healthcare management studies.
- Selection of assessable sources such as Google Scholar to find digital healthcare studies with a sustainability focus.
- Creation of a search query and keyword pursuit for sustainability, SDG3, sustainable development objective, healthcare, blockchain, information technology, security and privacy, design purpose, and economic, social, and environmental considerations.
- Creation of appropriate data sets and data collection using MS Excel. The main headings of the dataset comprised Problem Focused, Sustainability Aspects Focused, ICT Integration, Technology, Security and Privacy Challenges, Design and Integration Challenges, E-Health Related Applications, and Future Directions were created.
- Data evaluation is completed through Textual analysis of the developed records of various studies.
- Assessment of the findings and conclusion is established.
3. Existing Work
4. Digital Transformation in Healthcare
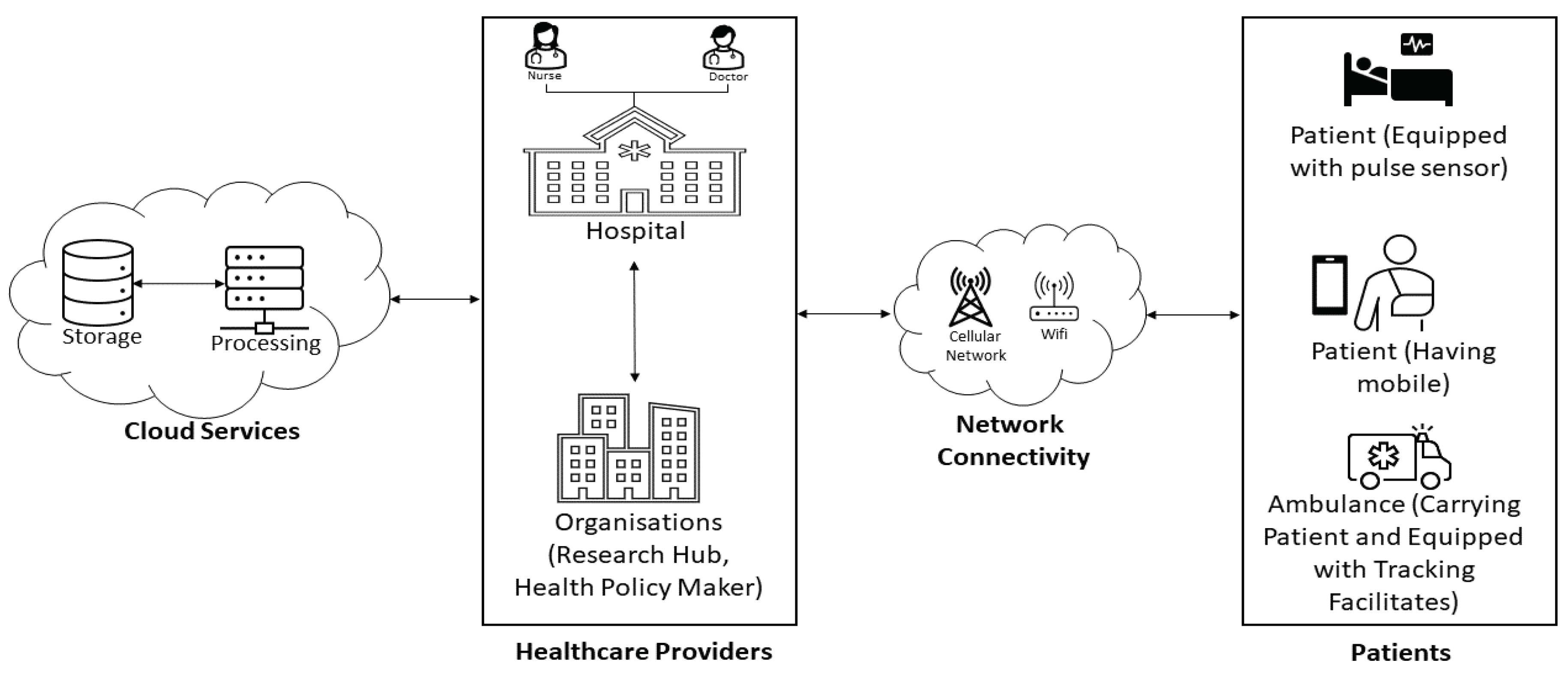
4.1. ICT-Based Healthcare System Components
4.1.1. Patient
4.1.2. Healthcare Provider
4.1.3. Medical Device
4.1.4. Sensor
4.1.5. Network/E-Health Architecture
4.1.6. Data Processing
4.2. E-Health Importance and Benefits
4.2.1. Enhancing Public Health and Medical Facilities
4.2.2. Aiding Medical Professionals
4.2.3. Real-time Monitoring and Management
4.2.4. Improved and Accurate Analysis
4.3. E-Health Challenges
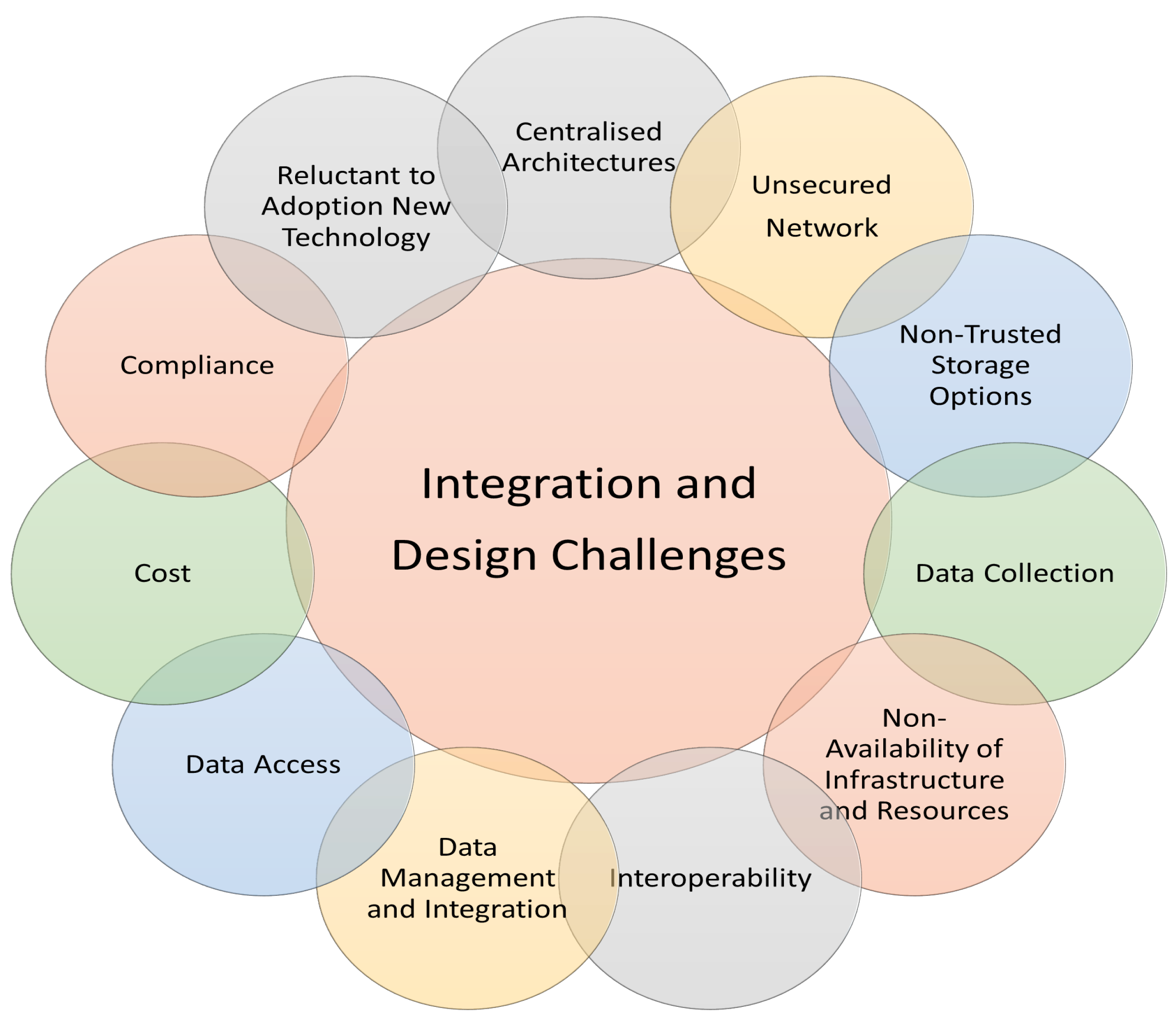
4.3.1. Integration and Design Challenges
- Centralised Architectures: A number of issues, some of which are directly related to the quality of treatment offered to patients, are seen as fundamental design issues in the current healthcare systems, which are based on centralised architectures [46]. For instance, because healthcare systems span many organisations all over the world and are expanding at a larger scale, centralised architecture may be less scalable and less efficient. It may also lead to more error-prone and longer wait times, which can be the reasons for deaths in severe cases [47]. In addition, the single point of failure problem is magnified in a centralised architecture, which means the entire healthcare system might go down and severely impede patient care [48].
- Unsecured networks: When healthcare practitioners transmit or maintain patient information using unprotected Wi-Fi or public networks, they run the risk of making the information accessible to third parties who are not authorised to access it [49].
- Non-trusted Storage Options: There are serious threats to patient privacy and data security posed by using non-trusted storage solutions in healthcare systems [50]. For example, physicians and other healthcare practitioners can keep patients’ data on their local servers without enforcing any security system or on their own devices like smartphones, tablets, and computers. Nevertheless, in either event, it is possible that the gadgets cannot be as secure as the rest of the healthcare system’s infrastructure. On the other hand, there is a larger-scale risk of data breaches, unauthorised access, and data loss when using untrusted public clouds for storage purposes [51].
- Data Collection: Data collection is a prerequisite for every healthcare setup to maintain quality, achieve efficiency, or have a positive outcome improvement process. Various healthcare entities acquire data from various sources, which typically flows in a disjointed or non-standardized fashion across these entities. Therefore, healthcare organizations may encounter numerous challenges when gathering information about patients’ race, ethnicity, and language, requiring careful collection, preparation, and management [52].
- Non-Availability of Infrastructure and Resources: A lack of suitable ICT infrastructure, such as internet access, hardware, and software, might hamper adopting and using ICT solutions in health systems. For instance, many governments might not have the means to invest in ICT technology and infrastructure, making integrating ICT into health systems challenging [53].
- Interoperability: Sharing, storing, and exchanging data across different health systems can be difficult due to the widespread use of multiple ICT solutions and platforms supported by heterogeneous and dispersed network architectures. Thus, interoperability protocols and specifications are required to guarantee appropriate collaboration and interaction across various ICT technologies [54].
- Data Management and Integration: The capacity to combine and manage diverse types of data collected from many sources is a recurring IT challenge to the healthcare industry, primarily as clinics and hospitals digital their work operations. Notes or transcripts from patient visits, information about insurance, treatment plans, laboratory results, referrals, medical history, and vital data from remote monitoring gadgets, such as wearables, are some of the various types of data collected in e-health. Other types of data collected in e-health include health history and referrals [55]. Since patients frequently see a variety of experts at facilities that are partnered with one another, each category of data in a patient’s file may originate from a different source. To compile all pertinent medical information about a patient in one location, healthcare providers require electronic health records (EHR) software designed to collect, integrate, and manage patients’ data efficiently. This results in improved diagnostic procedures, treatment approaches, and patient outcomes [56].
- Data Access: Data accessibility promotes access to the patient healthcare record and prompt reaction in an emergency, both crucial in sustaining the high standards of healthcare services. In addition, it benefits patients since doctors may quickly access their complete medical histories, lab findings, and related notes from other practitioners [57]. The capacity to quickly retrieve relevant information from a patient’s record can significantly enhance clinical efficiency by minimising the number of times a doctor has to switch between programs to finish a consultation and diagnose a patient. However, the exponential growth of data in the field of E-healthcare highlights the pressing necessity for enhanced data accessibility practices and information and communication technology (ICT) models. Despite the numerous advantages of this expansion, ensuring the availability of high-quality care data remains a significant challenge [58].
- Cost: Building health systems based on ICT infrastructure and technologies may be impossible in low-income or other areas with few funds. For example, there can be a sizable financial burden associated with the purchase, implementation, and support of ICT infrastructure to form a complete healthcare system and the expenditure of training healthcare staff to use the new technologies used to train before the manual methods [59].
- Compliance: The regulatory landscape is continuously shifting, as evidenced by the standards for billing, the maintenance of equipment, and software updates, to name just a few instances. Even though compliance controls are in place to protect patients and the data they provide, it still creates a legal minefield that chief information officers in the healthcare industry need to avoid [60]. Solution providers like Ta and Cervey help healthcare organisations and medical practices remotely. For instance, Arena provides a specialised quality management system to the medical device manufacturing industry. This system assists medical device manufacturers in ensuring that their equipment complies with specific regulations such as ISO 3485 [61].
- Reluctant to Adoption New Technology: Many healthcare workers may be reluctant to accept new technology because of the potential disruption to their practices that ICT integration into health systems may cause. For example, the adoption and use of ICT in health systems may be hampered because health workers may lack the technical experience and skills necessary to utilise and maintain ICT solutions efficiently [62].
4.3.2. Security and Privacy Challenges
-
Security ChallengesSecurity in E-health is defined as the access to sensitive patient information strictly regulated using security rules and processes to prevent misuse of sensitive patient information. In many countries, patients’ individual health records (PHI) are recorded, communicated, and kept electronically for later use.
- ★
- Physical Access to Resources: One of the most critical security challenges in healthcare systems is ensuring the safety of the resources used to implement the healthcare infrastructure. This is especially true in situations where patient data is stored or accessible. To prevent theft or unauthorised access to patient information, healthcare organisations must ensure that physical access controls are in place and functioning properly [63].
- ★
- Third-Party Untrusted Manufacturers/Devices: While the increasing use of IoT devices within healthcare systems promises to bring about much-needed beneficial change, this development also raises new security concerns. As a result of its potential to facilitate data operations and enhance the treatment process, IoT has been adopted by many organisations working in the health sector [64]. Nevertheless, due to the fact that most IoT devices are designed and manufactured by unreliable vendors, they frequently lack security patches and suitable built-in security protections, which in turn creates security concerns for entire healthcare systems [65].
- ★
- Cyber Attacks: Cyber-attacks, such as ransomware, phishing, spoofing, and malware attacks, are increasingly targeting the healthcare industry [66]. In addition to disrupting healthcare operations, these cyberattacks might result in the theft or disclosure of private patient data. For example, the healthcare industry is becoming vulnerable to ransomware attacks, in which hackers encrypt sensitive patient information and demand a ransom in exchange for decrypting it [67].
- ★
- Insider Threats: When it comes to data security threats, many businesses neglect the possibility of insider threats because they focus instead on external attacks, despite the fact that insider threats are typically related to overlooked basic design or security vulnerabilities [68]. The healthcare industry has recently seen an upsurge in insider threats, which are just as dangerous as those from the outside. In most cases involving E-health, insider threats might come from within the organisation itself, whether they be former or current staff, suppliers, company associates, healthcare officers, doctors, or incompetent staff [69].
-
Privacy ChallengesWhen discussing health information, "privacy" refers to preventing unwanted access to an individual’s medical records and keeping those records private [70]. It is possible to achieve this goal by strictly enforcing the relevant policies and laws. Patients have the right to know who has access to their medical records, how those records are being used, whether or not they will be shared with a third party and the circumstances under which such information may be shared. For instance, the Health Insurance Portability and Accountability Act (HIPAA) protects patients’ health information confidentiality [71].In E-health scenarios, the following are the privacy issues /challenges that patients and healthcare service providers (such as doctors) might face.
- ★
- Device Privacy: In the E-health patient scenario, device privacy is a major concern due to the enforcement of the device anonymity principle, which states that the patient has the right to know who is authorised to configure and install the device, what kind of medical device the patient is equipping, and who is interacting with and responsible for managing the devices [72].
- ★
- Data Privacy: Personal and medical information are two highly sensitive data that must be safeguarded to ensure data privacy. Data privacy in healthcare systems refers to protecting individual patients’ health information against misuse [73].
5. The Role of Blockchain in E-Health
5.1. Blockchain Technology
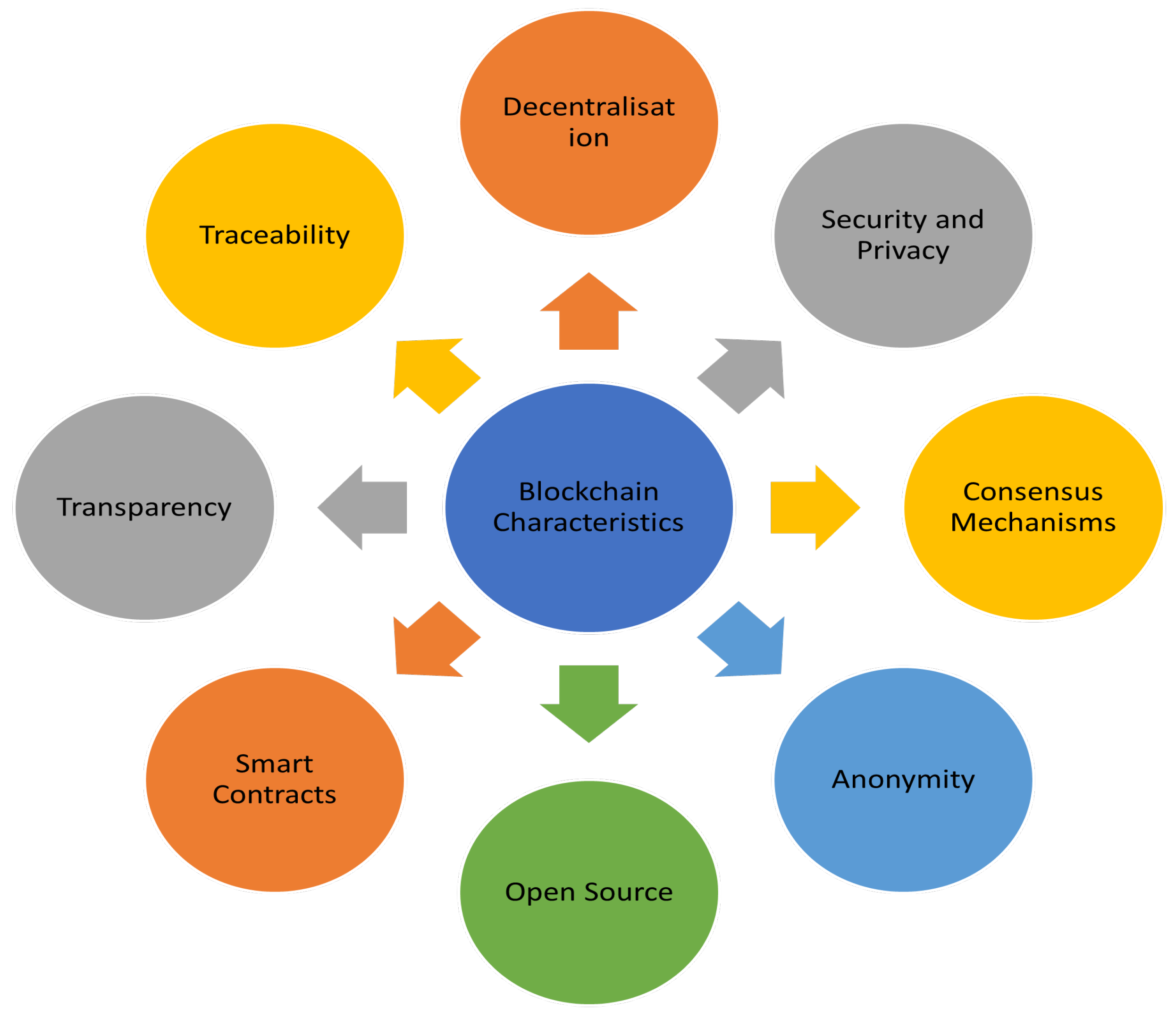
5.2. Characteristics
- Decentralisation: In a decentralised network, rather than having a central authority controlling everything, a group of nodes organises themselves in a P2P fashion and takes on responsibility for maintaining the network’s general structure [79].
- Immutability: Immutability (or tamper-proof) in the context of Blockchain technology refers to the fact that once a significant number of miner nodes have confirmed a block of data, the block and its associated data are irrevocably secured. Therefore, the immutability characteristic of Blockchain data provides assurances of data integrity and authenticity and can be used to trace its history [85].
- Security and Privacy: Utilising cutting-edge cryptographic techniques, blockchain technology ensures the security and immutability of all transactions created and stored in its distributed ledger. Using consensus protocols, for instance, Blockchain transactions are recorded in the distributed ledger after being generated by the encryption and digital signature mechanism. Encrypting and hashing each block in the chain with the hashing methods creates a verifiable chain [86].
- Consensus Mechanism: The consensus mechanism is a fundamental characteristic of Blockchain technology that ensures that only valid transactions and blocks are added to the distributed ledger, which requires the agreement of all network nodes. The consensus method is an agreement or set of rules that are given as a challenging problem or puzzle that all network participants must solve and agree upon [84].
- Anonymity: Blockchain’s anonymity feature could be transformative in terms of user and data privacy and security. Implementing anonymity in Blockchain is a promising new step towards preserving users’ privacy and fostering trust in the veracity of data and transactions, especially in high-stakes situations involving the exchange of financial or personally identifying information [87].
- Open Source: Using some of the available coding attributes incorporated into Blockchain technology, this open-source feature enables developers to create decentralised and secure applications to establish trust between network nodes and their data. This characteristic also gives you the freedom to create efficient and automated applications for a wide range of social and business use cases [88].
- Smart Contracts: Smart contracts are an intriguing use case for Blockchain technology since they are self-managing and self-executing pieces of code that execute on the Blockchain. Smart contracts automate the process of obtaining an agreement between a sender and a recipient on a set of established conditions by using predefined rules. Smart contracts are a facilitator, confirming and implementing contract rules to facilitate contract negotiations and achieve autonomy. Furthermore, smart contracts are used to ensure that all parties in the Blockchain are held accountable for their activities, as their conditions are public and can be viewed by any node in the network [89].
- Transparency: Transparency is yet another essential characteristic of Blockchain technology, as it enables anyone with network access to keep track of and validate transactions in the distributed ledger. In a public blockchain, for instance, users can record and manage transactions in a public ledger that is accessible to everyone on the network [90].
- Traceability: For audit purposes, the blockchain’s traceability feature and the usage of security guidelines ensure that transactions can’t be altered after they’ve been added to the ledger. As a result, it is possible to trace the history of any transaction in detail [91].
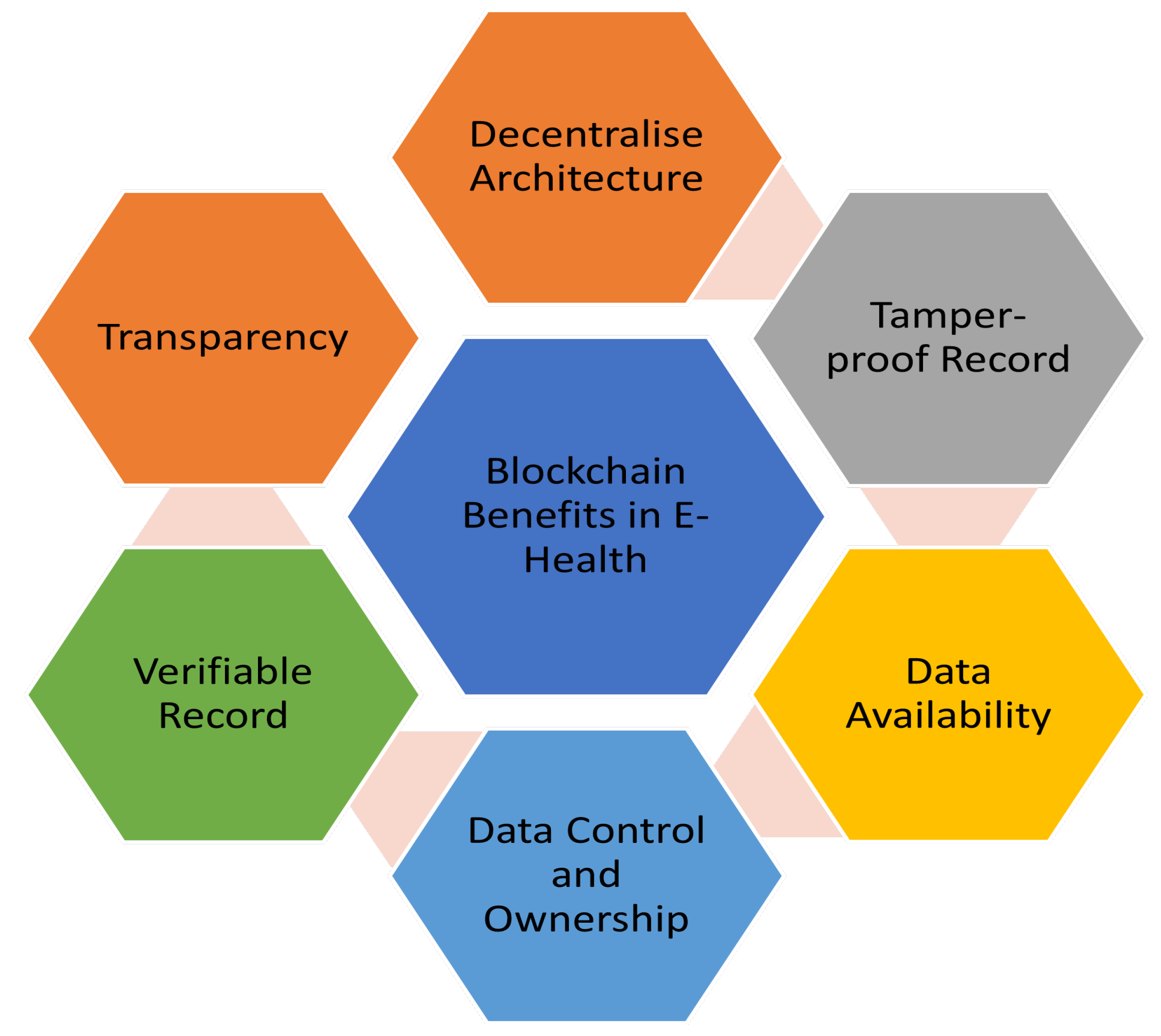
5.3. Blockchain Benefits in E-Health
- Decentralise Architecture: These days, a decentralised management system is necessary for processing, managing, and storing health data due to the nature of E-healthcare systems worldwide. In such scenarios, participants worldwide, including doctors, patients, hospitals, healthcare stakeholders, drug distributors, and so on, seek remote access to the system to carry out the abovementioned tasks [92]. To make this a reality, Blockchain has the potential to serve as the decentralised health data management infrastructure from which all stakeholders can enjoy secure access to identical medical records without anyone acting as the global health data authority [93].
- Tamper-proof Record: Since the data in a distributed ledger are encrypted, hashed, time-stamped, and appended in chronological order in the form of a chain, the immutability attribute of the distributed ledger used in blockchain considerably improves the security of the health data recorded on it [94]. Once data has been recorded to blockchain technology, it cannot be tampered with, edited, or recovered by any other means. In addition, patient health records are encrypted before being saved on blockchain technology using cryptographic keys, which helps protect patients’ identities as well as their privacy [95].
- Data Availability: Patient information in traditional healthcare systems is regularly shared between several providers without any security measure, increasing the risk of data leakage and unauthorised access. Due to the distributed nature and immutable feature of the blockchain, records are duplicated across numerous nodes, making the system highly resistant to data loss, illicit activities, and an array of security attacks that target data availability [96].
- Data Control and Ownership: Considering patient data in E-health systems contain sensitive and essential information, patients must retain ownership of their data and have insight into how the healthcare system utilises it [97]. In addition, it makes it clear that patients have a right to the certainty that the information about their health that other parties hold will not be mishandled. Blockchain technology fulfils these needs through its secure cryptographic techniques and the practical application of its smart contracts functionality [98]. By using such available features of Blockchain, Patients can decide who has access to their medical records and can grant or revoke access as needed. Furthermore, blockchain’s built-in privacy mechanisms allow patients to control who is entitled to their health information and cease access at any time [99].
- Verifiable Record: One of the advantages of using blockchain technology in electronic health care is that it makes it possible to verify the accuracy of medical records about patients and healthcare providers without actually accessing the records stored on the blockchain. For instance, the supply chain management process of medications and the processing of insurance claims both use this capability to provide the verifiability of records recorded on a temper-proof ledger in the event that a discrepancy occurs. Therefore, This is a crucial requirement to ensure data integrity [100].
- Transparency: In terms of E-health transparency, Blockchain technology makes use of a decentralised ledger to record all of the transactions and patient data using a consensus process [101]. This feature introduces and assures an additional level of difficulty for anyone working in the healthcare system to change or manipulate the data in any way. In addition to this, transparency means that all parties involved, such as patients, medical professionals, healthcare facilities, and insurance companies, have access to identical information and can validate the credibility of the data [102].
5.4. Blockchain-based E-health Use Cases/Applications
5.4.1. Management of Electronic Health Record (EHR)
5.4.2. Medical Bill/Insurance Claims
5.4.3. Remotely Analysing/Monitoring Patients
5.4.4. Health Data Analysis
5.4.5. Clinical Trials/Data
6. Impact of ICT Integration into Health Systems
6.1. Positive Impacts
6.1.1. Digitalisation of Patient Records
6.1.2. Improved and Quality Access to Healthcare Services
6.1.3. Patient Independence and Autonomy
6.1.4. Real-Time Diseases Monitoring
6.1.5. Equity Healthcare Services Culture
6.2. Blockchain Technology Impacts on Sustainability
6.2.1. Environmental Impact
6.2.2. Social Impact
6.2.3. Economical Impact
6.3. Negative Impacts
6.3.1. Cost
6.3.2. Technical Knowledge
6.3.3. Doctor-Patient Interaction
6.3.4. Patient’s Information Privacy
6.3.5. Over-Relience of ICT Technology
6.3.6. Increased Social Imbalance
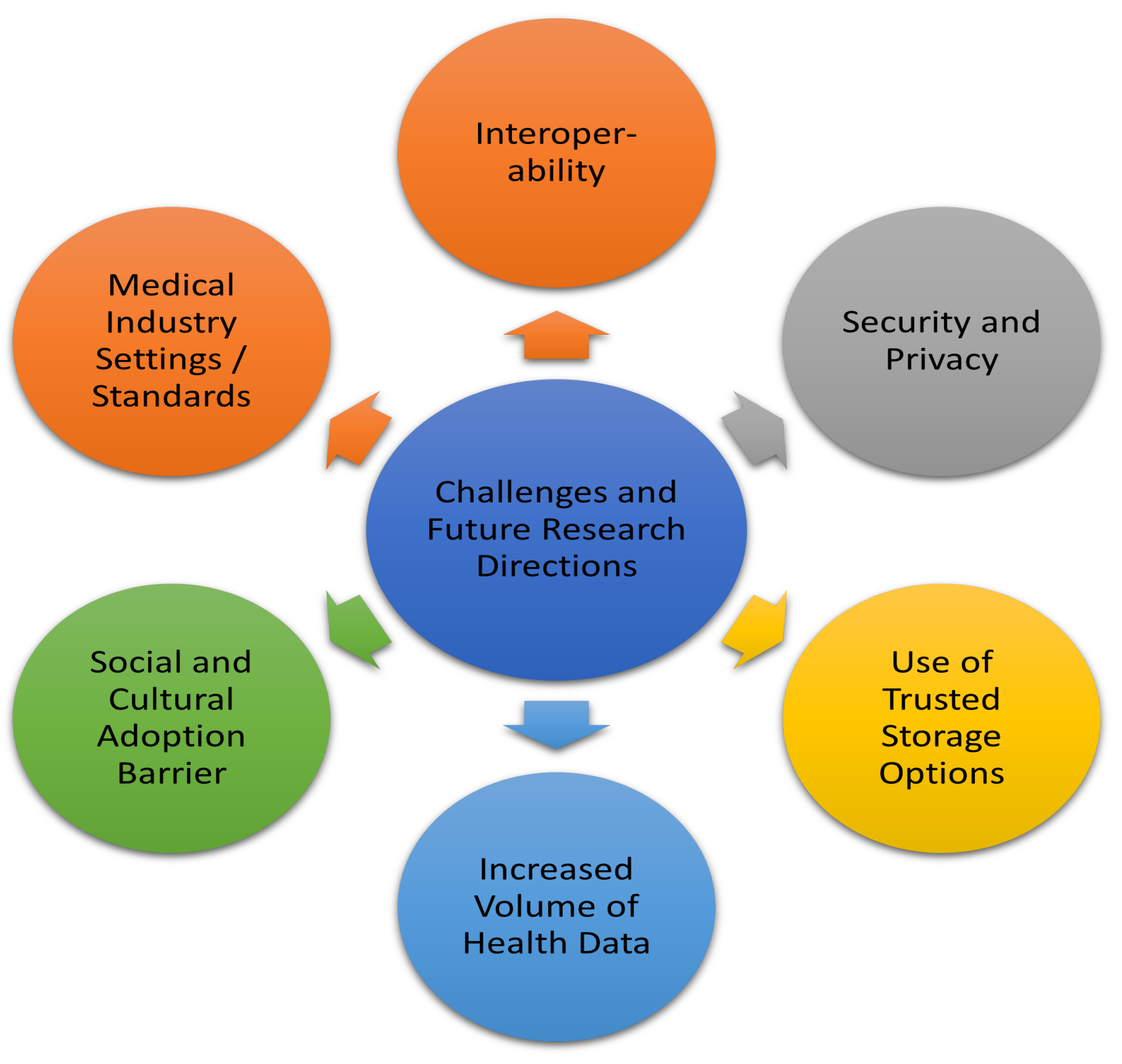
7. Challenges and Future Research Directions
7.1. Interoperability
7.2. Security and Privacy
7.3. Use of Trusted Storage Options
7.4. Increased Volume of Health Data
7.5. Social and Cultural Adoption Barrier
7.6. Medical Industry Settings/Standards
8. Implications of Our Study
8.1. Security and Privacy Implications
8.2. Stakeholder Implications
8.3. Research and Development
9. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| SDG | Sustainable Development Goal |
| IoT | Internet of Things |
| AI | Artificial Intelligence |
| BC | Blockchain |
| WHO | World Health Organisation |
References
- Berniak-Woźny, J.; Rataj, M. Towards Green and Sustainable Healthcare: A Literature Review and Research Agenda for Green Leadership in the Healthcare Sector. International Journal of Environmental Research and Public Health 2023, 20, 908. [Google Scholar] [CrossRef] [PubMed]
- Mhlanga, D. The role of artificial intelligence and machine learning amid the COVID-19 pandemic: What lessons are we learning on 4IR and the sustainable development goals. International Journal of Environmental Research and Public Health 2022, 19, 1879. [Google Scholar] [CrossRef] [PubMed]
- Ekwebelem, O.C.; Ofielu, E.S.; Nnorom-Dike, O.V.; Iweha, C.; Ekwebelem, N.C.; Obi, B.C.; Ugbede-Ojo, S.E. Threats of COVID-19 to achieving United Nations sustainable development goals in Africa. The American Journal of Tropical Medicine and Hygiene 2021, 104, 457. [Google Scholar] [CrossRef] [PubMed]
- Kontoangelos, K.; Economou, M.; Papageorgiou, C. Mental health effects of COVID-19 pandemia: a review of clinical and psychological traits. Psychiatry investigation 2020, 17, 491. [Google Scholar] [CrossRef] [PubMed]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC public health 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chandan, A.; John, M.; Potdar, V. Achieving UN SDGs in Food Supply Chain Using Blockchain Technology. Sustainability 2023, 15, 2109. [Google Scholar] [CrossRef]
- Medaglia, R.; Damsgaard, J. Blockchain and the United Nations Sustainable Development Goals: Towards an Agenda for IS Research. PACIS, 2020, p. 36.
- Nowak, A. The Cost of Living: The Impact of the Increasing Cost of Pharmaceutical Drugs on Public Health 2019.
- Organization, W.H. ; others. Is the Eastern Mediterranean Region ready for digitalizing health? implications from the global strategy on digital health (2020–2025) 2021.
- Abbas, H.S.M.; Qaisar, Z.H.; Ali, G.; Alturise, F.; Alkhalifah, T. Impact of cybersecurity measures on improving institutional governance and digitalization for sustainable healthcare. Plos one 2022, 17, e0274550. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Pinglu, C.; Ullah, S.; Abbas, H.S.M.; Khan, S. The role of e-governance in combating COVID-19 and promoting sustainable development: a comparative study of China and Pakistan. Chinese Political Science Review 2021, 6, 86–118. [Google Scholar] [CrossRef]
- Verdejo Espinosa, Á.; López, J.L.; Mata Mata, F.; Estevez, M.E. Application of IoT in healthcare: keys to implementation of the sustainable development goals. Sensors 2021, 21, 2330. [Google Scholar] [CrossRef]
- Cabanillas-Carbonell, M.; Pérez-Martínez, J.A.; Yáñez, J. 5G Technology in the Digital Transformation of Healthcare, a Systematic Review. Sustainability 2023, 15, 3178. [Google Scholar] [CrossRef]
- Joshi, S.; Sharma, M.; Das, R.P.; Rosak-Szyrocka, J.; Żywiołek, J.; Muduli, K.; Prasad, M. Modeling Conceptual Framework for Implementing Barriers of AI in Public Healthcare for Improving Operational Excellence: Experiences from Developing Countries. Sustainability 2022, 14, 11698. [Google Scholar] [CrossRef]
- Thayyib, P.; Mamilla, R.; Khan, M.; Fatima, H.; Asim, M.; Anwar, I.; Shamsudheen, M.; Khan, M.A. State-of-the-Art of Artificial Intelligence and Big Data Analytics Reviews in Five Different Domains: A Bibliometric Summary. Sustainability 2023, 15, 4026. [Google Scholar] [CrossRef]
- Soltysik-Piorunkiewicz, A.; Morawiec, P. The Sustainable e-Health System Development in COVID 19 Pandemic–The Theoretical Studies of Knowledge Management Systems and Practical Polish Healthcare Experience. J. e-Health Manag 2022, 2022, 1–12. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. International journal of environmental research and public health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Fragão-Marques, M.; Ozben, T. Digital transformation and sustainability in healthcare and clinical laboratories. Clinical Chemistry and Laboratory Medicine (CCLM) 2023, 61, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Hadjiat, Y. Healthcare inequity and digital health–A bridge for the divide, or further erosion of the chasm? PLOS Digital Health 2023, 2, e0000268. [Google Scholar] [CrossRef]
- Ngongoni, C.N.; Wasswa, W.; Chibi, M. Legacy of COVID-19 Innovations: Strengthening African Primary Health Care through Pandemic Innovations. Sustainability 2023, 15, 12073. [Google Scholar] [CrossRef]
- Alajlan, A.; Baslyman, M. Toward a Comprehensive Understanding and Evaluation of the Sustainability of E-Health Solutions. Applied Sciences 2023, 13, 5811. [Google Scholar] [CrossRef]
- Cheshmehzangi, A.; Su, Z.; Zou, T. ICT applications and the COVID-19 pandemic: Impacts on the individual’s digital data, digital privacy, and data protection. Frontiers in Human Dynamics 2023, 5, 971504. [Google Scholar] [CrossRef]
- Butt, J. A conceptual framework to support digital transformation in manufacturing using an integrated business process management approach. Designs 2020, 4, 17. [Google Scholar] [CrossRef]
- Badidi, E. Edge AI and blockchain for smart sustainable cities: Promise and potential. Sustainability 2022, 14, 7609. [Google Scholar] [CrossRef]
- Clark, S.; MacLachlan, M.; Marshall, K.; Morahan, N.; Carroll, C.; Hand, K.; Boyle, N.; O’Sullivan, K. Including digital connection in the united nations sustainable development goals: A systems thinking approach for achieving the SDGs. Sustainability 2022, 14, 1883. [Google Scholar] [CrossRef]
- Stark, H.E.; Graudins, L.V.; McGuire, T.M.; Lee, C.Y.Y.; Duguid, M.J. Implementing a sustainable medication reconciliation process in Australian hospitals: The World Health Organization High 5s project. Research in Social and Administrative Pharmacy 2020, 16, 290–298. [Google Scholar] [CrossRef]
- Tajpour, M.; Hosseini, E.; Mohammadi, M.; Bahman-Zangi, B. The effect of knowledge management on the sustainability of technology-driven businesses in emerging markets: The mediating role of social media. Sustainability 2022, 14, 8602. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Braithwaite, J. Will information and communication technology disrupt the health system and deliver on its promise? Medical Journal of Australia 2010, 193, 399–400. [Google Scholar] [CrossRef]
- Celik, A.; Romdhane, I.; Kaddoum, G.; Eltawil, A.M. A top-down survey on optical wireless communications for the internet of things. IEEE Communications Surveys & Tutorials 2022. [Google Scholar]
- Yuehong, Y.; Zeng, Y.; Chen, X.; Fan, Y. The internet of things in healthcare: An overview. Journal of Industrial Information Integration 2016, 1, 3–13. [Google Scholar]
- Lupiáñez-Villanueva, F.; Hardey, M.; Torrent, J.; Ficapal, P. The integration of Information and Communication Technology into medical practice. International journal of medical informatics 2010, 79, 478–491. [Google Scholar] [CrossRef]
- Ksibi, S.; Jaidi, F.; Bouhoula, A. A Comprehensive Study of Security and Cyber-Security Risk Management within e-Health Systems: Synthesis, Analysis and a Novel Quantified Approach. Mobile Networks and Applications 2022, 1–21. [Google Scholar] [CrossRef]
- Islam, M.R.; Kabir, M.M.; Mridha, M.F.; Alfarhood, S.; Safran, M.; Che, D. Deep Learning-Based IoT System for Remote Monitoring and Early Detection of Health Issues in Real-Time. Sensors 2023, 23, 5204. [Google Scholar] [CrossRef]
- Grimson, J. Delivering the electronic healthcare record for the 21st century. International journal of medical informatics 2001, 64, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Butpheng, C.; Yeh, K.H.; Xiong, H. Security and privacy in IoT-cloud-based e-health systems—A comprehensive review. Symmetry 2020, 12, 1191. [Google Scholar] [CrossRef]
- Tahir, A.; Chen, F.; Khan, H.U.; Ming, Z.; Ahmad, A.; Nazir, S.; Shafiq, M. A systematic review on cloud storage mechanisms concerning e-healthcare systems. Sensors 2020, 20, 5392. [Google Scholar] [CrossRef] [PubMed]
- Mathews, S.C.; McShea, M.J.; Hanley, C.L.; Ravitz, A.; Labrique, A.B.; Cohen, A.B. Digital health: a path to validation. NPJ digital medicine 2019, 2, 38. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Kim, D.H. Design and implementation of e-health system based on semantic sensor network using IETF YANG. Sensors 2018, 18, 629. [Google Scholar] [CrossRef]
- Benhlima, L.; others. Big data management for healthcare systems: architecture, requirements, and implementation. Advances in bioinformatics 2018, 2018. [Google Scholar]
- Ross, M.; Wei, W.; Ohno-Machado, L. “Big data” and the electronic health record. Yearbook of medical informatics 2014, 23, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical care 2012, 50, 217. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Chen, W.; Zhao, J.; Yang, G.Z. Medical robotics: opportunities in China. Annual Review of Control, Robotics, and Autonomous Systems 2022, 5, 361–383. [Google Scholar] [CrossRef]
- Chan, M.; Estève, D.; Fourniols, J.Y.; Escriba, C.; Campo, E. Smart wearable systems: Current status and future challenges. Artificial intelligence in medicine 2012, 56, 137–156. [Google Scholar] [CrossRef]
- Chen, M.; Decary, M. Artificial intelligence in healthcare: An essential guide for health leaders. Healthcare management forum. SAGE Publications Sage CA: Los Angeles, CA, 2020, Vol. 33, pp. 10–18.
- Hameed, K.; Barika, M.; Garg, S.; Amin, M.B.; Kang, B. A taxonomy study on securing Blockchain-based Industrial applications: An overview, application perspectives, requirements, attacks, countermeasures, and open issues. Journal of Industrial Information Integration 2022, 26, 100312. [Google Scholar] [CrossRef]
- Wen, H.; Wu, Y.; Yang, C.; Duan, H.; Yu, S. A unified federated learning framework for wireless communications: Towards privacy, efficiency, and security. IEEE INFOCOM 2020-IEEE Conference on Computer Communications Workshops (INFOCOM WKSHPS). IEEE, 2020, pp. 653–658.
- Daglish, D.; Archer, N. Electronic personal health record systems: a brief review of privacy, security, and architectural issues. 2009 world congress on privacy, security, Trust and the Management of e-Business. IEEE, 2009, pp. 110–120.
- Thota, C.; Sundarasekar, R.; Manogaran, G.; Varatharajan, R.; Priyan, M. Centralized fog computing security platform for IoT and cloud in healthcare system. In Fog computing: Breakthroughs in research and practice; IGI global, 2018; pp. 365–378.
- Papaioannou, M.; Karageorgou, M.; Mantas, G.; Sucasas, V.; Essop, I.; Rodriguez, J.; Lymberopoulos, D. A survey on security threats and countermeasures in internet of medical things (IoMT). Transactions on Emerging Telecommunications Technologies 2022, 33, e4049. [Google Scholar] [CrossRef]
- Ekonomou, E.; Fan, L.; Buchanan, W.; Thuemmler, C. An integrated cloud-based healthcare infrastructure. 2011 IEEE third international conference on cloud computing technology and science. IEEE, 2011, pp. 532–536.
- Newaz, A.I.; Sikder, A.K.; Rahman, M.A.; Uluagac, A.S. A Survey on Security and Privacy Issues in Modern Healthcare Systems: Attacks and Defenses. ACM Trans. Comput. Healthcare 2021, 2. [Google Scholar] [CrossRef]
- Rolim, C.O.; Koch, F.L.; Westphall, C.B.; Werner, J.; Fracalossi, A.; Salvador, G.S. A cloud computing solution for patient’s data collection in health care institutions. 2010 Second International Conference on eHealth, Telemedicine, and Social Medicine. IEEE, 2010, pp. 95–99.
- Garavand, A.; Behmanesh, A.; Aslani, N.; Sadeghsalehi, H.; Ghaderzadeh, M.; others. Towards Diagnostic Aided Systems in Coronary Artery Disease Detection: A Comprehensive Multiview Survey of the State of the Art. International Journal of Intelligent Systems 2023, 2023. [Google Scholar] [CrossRef]
- Sadhu, P.K.; Yanambaka, V.P.; Abdelgawad, A.; Yelamarthi, K. Prospect of internet of medical things: A review on security requirements and solutions. Sensors 2022, 22, 5517. [Google Scholar] [CrossRef] [PubMed]
- Ghaderzadeh, M.; Aria, M.; Hosseini, A.; Asadi, F.; Bashash, D.; Abolghasemi, H. A fast and efficient CNN model for B-ALL diagnosis and its subtypes classification using peripheral blood smear images. International Journal of Intelligent Systems 2022, 37, 5113–5133. [Google Scholar] [CrossRef]
- Ghaderzadeh, M.; Aria, M. Management of covid-19 detection using artificial intelligence in 2020 pandemic. Proceedings of the 5th International Conference on Medical and Health Informatics, 2021, pp. 32–38.
- Roy, S.; Das, A.K.; Chatterjee, S.; Kumar, N.; Chattopadhyay, S.; Rodrigues, J.J. Provably secure fine-grained data access control over multiple cloud servers in mobile cloud computing based healthcare applications. IEEE Transactions on Industrial Informatics 2018, 15, 457–468. [Google Scholar] [CrossRef]
- Rosenbaum, S. Data governance and stewardship: designing data stewardship entities and advancing data access. Health services research 2010, 45, 1442–1455. [Google Scholar] [CrossRef]
- Garavand, A.; Salehnasab, C.; Behmanesh, A.; Aslani, N.; Zadeh, A.H.; Ghaderzadeh, M.; others. Efficient model for coronary artery disease diagnosis: a comparative study of several machine learning algorithms. Journal of Healthcare Engineering 2022, 2022. [Google Scholar] [CrossRef]
- Elsharkawy, N.B.; Abdelaziz, E.M.; Ouda, M.M.; Oraby, F.A. Effectiveness of health information package program on knowledge and compliance among pregnant women with anemia: a randomized controlled trial. International Journal of Environmental Research and Public Health 2022, 19, 2724. [Google Scholar] [CrossRef]
- Ghaderzadeh, M.; Asadi, F.; Hosseini, A.; Bashash, D.; Abolghasemi, H.; Roshanpour, A. Machine learning in detection and classification of leukemia using smear blood images: a systematic review. Scientific Programming 2021, 2021, 1–14. [Google Scholar] [CrossRef]
- Gheisari, M.; Ebrahimzadeh, F.; Rahimi, M.; Moazzamigodarzi, M.; Liu, Y.; Dutta Pramanik, P.K.; Heravi, M.A.; Mehbodniya, A.; Ghaderzadeh, M.; Feylizadeh, M.R.; others. Deep learning: Applications, architectures, models, tools, and frameworks: A comprehensive survey. CAAI Transactions on Intelligence Technology 2023. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Medical 4.0 technologies for healthcare: Features, capabilities, and applications. Internet of Things and Cyber-Physical Systems 2022. [Google Scholar] [CrossRef]
- Al Alkeem, E.; Yeun, C.Y.; Zemerly, M.J. Security and privacy framework for ubiquitous healthcare IoT devices. 2015 10th International Conference for Internet Technology and Secured Transactions (ICITST). IEEE, 2015, pp. 70–75.
- Xu, T.; Wendt, J.B.; Potkonjak, M. Security of IoT systems: Design challenges and opportunities. 2014 IEEE/ACM International Conference on Computer-Aided Design (ICCAD). IEEE, 2014, pp. 417–423.
- Dogaru, D.I.; Dumitrache, I. Cyber security in healthcare networks. 2017 E-Health and Bioengineering Conference (EHB). IEEE, 2017, pp. 414–417.
- AlZubi, A.A.; Al-Maitah, M.; Alarifi, A. Cyber-attack detection in healthcare using cyber-physical system and machine learning techniques. Soft Computing 2021, 25, 12319–12332. [Google Scholar] [CrossRef]
- Zafar, F.; Khan, A.; Suhail, S.; Ahmed, I.; Hameed, K.; Khan, H.M.; Jabeen, F.; Anjum, A. Trustworthy data: A survey, taxonomy and future trends of secure provenance schemes. Journal of network and computer applications 2017, 94, 50–68. [Google Scholar] [CrossRef]
- Walker-Roberts, S.; Hammoudeh, M.; Dehghantanha, A. A systematic review of the availability and efficacy of countermeasures to internal threats in healthcare critical infrastructure. IEEE Access 2018, 6, 25167–25177. [Google Scholar] [CrossRef]
- Price, W.N.; Cohen, I.G. Privacy in the age of medical big data. Nature medicine 2019, 25, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.M.; Rajput, A. Threats to patients’ privacy in smart healthcare environment. In Innovation in Health Informatics; Elsevier, 2020; pp. 375–393.
- Ali, M.; Naeem, F.; Tariq, M.; Kaddoum, G. Federated learning for privacy preservation in smart healthcare systems: A comprehensive survey. IEEE journal of biomedical and health informatics 2022, 27, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Shahid, J.; Ahmad, R.; Kiani, A.K.; Ahmad, T.; Saeed, S.; Almuhaideb, A.M. Data protection and privacy of the internet of healthcare things (IoHTs). Applied Sciences 2022, 12, 1927. [Google Scholar] [CrossRef]
- Battula, S.K.; Garg, S.; Naha, R.; Amin, M.B.; Kang, B.; Aghasian, E. A blockchain-based framework for automatic SLA management in fog computing environments. The Journal of Supercomputing 2022, 78, 16647–16677. [Google Scholar] [CrossRef]
- Swan, M. Blockchain: Blueprint for a new economy; " O’Reilly Media, Inc.", 2015.
- Nofer, M.; Gomber, P.; Hinz, O.; Schiereck, D. Blockchain. Business & Information Systems Engineering 2017, 59, 183–187. [Google Scholar]
- Maleh, Y.; Shojafar, M.; Alazab, M.; Romdhani, I. Blockchain for cybersecurity and privacy: architectures, challenges, and applications 2020.
- Crosby, M.; Pattanayak, P.; Verma, S.; Kalyanaraman, V.; others. Blockchain technology: Beyond bitcoin. Applied Innovation 2016, 2, 71. [Google Scholar]
- Zheng, Z.; Xie, S.; Dai, H.; Chen, X.; Wang, H. An overview of blockchain technology: Architecture, consensus, and future trends. 2017 IEEE international congress on big data (BigData congress). Ieee, 2017, pp. 557–564.
- Gervais, A.; Karame, G.O.; Wüst, K.; Glykantzis, V.; Ritzdorf, H.; Capkun, S. On the security and performance of proof of work blockchains. Proceedings of the 2016 ACM SIGSAC conference on computer and communications security, 2016, pp. 3–16.
- Gaži, P.; Kiayias, A.; Zindros, D. Proof-of-stake sidechains. 2019 IEEE Symposium on Security and Privacy (SP). IEEE, 2019, pp. 139–156.
- Castro, M.; Liskov, B. ; others. Practical byzantine fault tolerance. OsDI, 1999, Vol. 99, pp. 173–186.
- Larimer, D. Delegated proof-of-stake (dpos). Bitshare whitepaper 2014, 81, 85. [Google Scholar]
- Mingxiao, D.; Xiaofeng, M.; Zhe, Z.; Xiangwei, W.; Qijun, C. A review on consensus algorithm of blockchain. 2017 IEEE international conference on systems, man, and cybernetics (SMC). IEEE, 2017, pp. 2567–2572.
- Zheng, B.K.; Zhu, L.H.; Shen, M.; Gao, F.; Zhang, C.; Li, Y.D.; Yang, J. Scalable and privacy-preserving data sharing based on blockchain. Journal of Computer Science and Technology 2018, 33, 557–567. [Google Scholar] [CrossRef]
- Zhang, R.; Xue, R.; Liu, L. Security and privacy on blockchain. ACM Computing Surveys (CSUR) 2019, 52, 1–34. [Google Scholar] [CrossRef]
- Khalilov, M.C.K.; Levi, A. A survey on anonymity and privacy in bitcoin-like digital cash systems. IEEE Communications Surveys & Tutorials 2018, 20, 2543–2585. [Google Scholar]
- Muzammal, M.; Qu, Q.; Nasrulin, B. Renovating blockchain with distributed databases: An open source system. Future generation computer systems 2019, 90, 105–117. [Google Scholar] [CrossRef]
- Mohanta, B.K.; Panda, S.S.; Jena, D. An overview of smart contract and use cases in blockchain technology. 2018 9th international conference on computing, communication and networking technologies (ICCCNT). IEEE, 2018, pp. 1–4.
- Wang, Z.; Lin, J.; Cai, Q.; Wang, Q.; Zha, D.; Jing, J. Blockchain-based certificate transparency and revocation transparency. IEEE Transactions on Dependable and Secure Computing 2020, 19, 681–697. [Google Scholar] [CrossRef]
- Galvez, J.F.; Mejuto, J.C.; Simal-Gandara, J. Future challenges on the use of blockchain for food traceability analysis. TrAC Trends in Analytical Chemistry 2018, 107, 222–232. [Google Scholar] [CrossRef]
- Shahnaz, A.; Qamar, U.; Khalid, A. Using blockchain for electronic health records. IEEE access 2019, 7, 147782–147795. [Google Scholar] [CrossRef]
- Abu-Elezz, I.; Hassan, A.; Nazeemudeen, A.; Househ, M.; Abd-Alrazaq, A. The benefits and threats of blockchain technology in healthcare: A scoping review. International Journal of Medical Informatics 2020, 142, 104246. [Google Scholar] [CrossRef] [PubMed]
- Cerchione, R.; Centobelli, P.; Riccio, E.; Abbate, S.; Oropallo, E. Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem. Technovation 2023, 120, 102480. [Google Scholar] [CrossRef]
- Abunadi, I.; Kumar, R.L. BSF-EHR: blockchain security framework for electronic health records of patients. Sensors 2021, 21, 2865. [Google Scholar] [CrossRef] [PubMed]
- Tagde, P.; Tagde, S.; Bhattacharya, T.; Tagde, P.; Chopra, H.; Akter, R.; Kaushik, D.; Rahman, M.H. Blockchain and artificial intelligence technology in e-Health. Environmental Science and Pollution Research 2021, 28, 52810–52831. [Google Scholar] [CrossRef] [PubMed]
- Jabbar, R.; Fetais, N.; Krichen, M.; Barkaoui, K. Blockchain technology for healthcare: Enhancing shared electronic health record interoperability and integrity. 2020 IEEE International Conference on Informatics, IoT, and Enabling Technologies (ICIoT). IEEE, 2020, pp. 310–317.
- Ray Chawdhuri, D. Patient privacy and ownership of electronic health records on a blockchain. Blockchain–ICBC 2019: Second International Conference, Held as Part of the Services Conference Federation, SCF 2019, San Diego, CA, USA, June 25–30, 2019, Proceedings 2. Springer, 2019, pp. 95–111.
- Biswas, S.; Sharif, K.; Li, F.; Mohanty, S. Blockchain for e-health-care systems: Easier said than done. Computer 2020, 53, 57–67. [Google Scholar] [CrossRef]
- Hameed, K.; Garg, S.; Amin, M.B.; Kang, B.; Khan, A. A context-aware information-based clone node attack detection scheme in Internet of Things. Journal of Network and Computer Applications 2022, 197, 103271. [Google Scholar] [CrossRef]
- Li, S.; Zhang, Y.; Xu, C.; Cheng, N.; Liu, Z.; Du, Y.; Shen, X. HealthFort: A Cloud-Based Ehealth System With Conditional Forward Transparency and Secure Provenance Via Blockchain. IEEE Transactions on Mobile Computing 2022. [Google Scholar] [CrossRef]
- Sharma, Y.; Balamurugan, B. Preserving the privacy of electronic health records using blockchain. Procedia Computer Science 2020, 173, 171–180. [Google Scholar] [CrossRef]
- Chenthara, S.; Ahmed, K.; Wang, H.; Whittaker, F.; Chen, Z. Healthchain: A novel framework on privacy preservation of electronic health records using blockchain technology. Plos one 2020, 15, e0243043. [Google Scholar] [CrossRef]
- Cachin, C. ; others. Architecture of the hyperledger blockchain fabric. Workshop on distributed cryptocurrencies and consensus ledgers. Chicago, IL, 2016, Vol. 310, pp. 1–4.
- Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustainable cities and society 2018, 39, 283–297. [Google Scholar] [CrossRef]
- Dubovitskaya, A.; Xu, Z.; Ryu, S.; Schumacher, M.; Wang, F. Secure and trustable electronic medical records sharing using blockchain. AMIA annual symposium proceedings. American Medical Informatics Association, 2017, Vol. 2017, p. 650.
- Zheng, H.; You, L.; Hu, G. A novel insurance claim blockchain scheme based on zero-knowledge proof technology. Computer Communications 2022, 195, 207–216. [Google Scholar] [CrossRef]
- Griggs, K.N.; Ossipova, O.; Kohlios, C.P.; Baccarini, A.N.; Howson, E.A.; Hayajneh, T. Healthcare blockchain system using smart contracts for secure automated remote patient monitoring. Journal of medical systems 2018, 42, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. Continuous patient monitoring with a patient centric agent: A block architecture. IEEE Access 2018, 6, 32700–32726. [Google Scholar] [CrossRef]
- Ji, Y.; Zhang, J.; Ma, J.; Yang, C.; Yao, X. BMPLS: Blockchain-based multi-level privacy-preserving location sharing scheme for telecare medical information systems. Journal of medical systems 2018, 42, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, W.; Raghupathi, V. Big data analytics in healthcare: promise and potential. Health information science and systems 2014, 2, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zaabar, B.; Cheikhrouhou, O.; Jamil, F.; Ammi, M.; Abid, M. HealthBlock: A secure blockchain-based healthcare data management system. Computer Networks 2021, 200, 108500. [Google Scholar] [CrossRef]
- Odeh, A.; Keshta, I.; Al-Haija, Q.A. Analysis of Blockchain in the Healthcare Sector: Application and Issues. Symmetry 2022, 14, 1760. [Google Scholar] [CrossRef]
- Wong, D.R.; Bhattacharya, S.; Butte, A.J. Prototype of running clinical trials in an untrustworthy environment using blockchain. Nature communications 2019, 10, 917. [Google Scholar] [CrossRef]
- Nugent, T.; Upton, D.; Cimpoesu, M. Improving data transparency in clinical trials using blockchain smart contracts. F1000Research 2016, 5. [Google Scholar] [CrossRef]
- Ahmad, R.W.; Salah, K.; Jayaraman, R.; Yaqoob, I.; Ellahham, S.; Omar, M. Blockchain and COVID-19 pandemic: Applications and challenges. Cluster Computing 2023, 1–26. [Google Scholar] [CrossRef]
- Wyatt, D.; Lampon, S.; McKevitt, C. Delivering healthcare’s ‘triple aim’: Electronic health records and the health research participant in the UK National Health Service. Sociology of health & illness 2020, 42, 1312–1327. [Google Scholar]
- Shaharul, N.A.; Ahmad Zamzuri, M.I.; Ariffin, A.A.; Azman, A.Z.F.; Mohd Ali, N.K. Digitalisation Medical Records: Improving Efficiency and Reducing Burnout in Healthcare. International Journal of Environmental Research and Public Health 2023, 20, 3441. [Google Scholar] [CrossRef]
- Nundy, S.; Cooper, L.A.; Mate, K.S. The quintuple aim for health care improvement: a new imperative to advance health equity. JAMA 2022, 327, 521–522. [Google Scholar] [CrossRef]
- Deutschbein, T.; Reimondo, G.; Di Dalmazi, G.; Bancos, I.; Patrova, J.; Vassiliadi, D.A.; Nekić, A.B.; Debono, M.; Lardo, P.; Ceccato, F.; others. Age-dependent and sex-dependent disparity in mortality in patients with adrenal incidentalomas and autonomous cortisol secretion: an international, retrospective, cohort study. The Lancet Diabetes & Endocrinology 2022, 10, 499–508. [Google Scholar]
- Chakraborty, C.; Kishor, A. Real-time cloud-based patient-centric monitoring using computational health systems. IEEE transactions on computational social systems 2022, 9, 1613–1623. [Google Scholar] [CrossRef]
- Karidakis, M.; Woodward-Kron, R.; Amorati, R.; Hu, B.; Pym, A.; Hajek, J. Enhancing COVID-19 public health communication for culturally and linguistically diverse communities: An Australian interview study with community representatives. Qualitative Health Communication 2022, 1, 61–83. [Google Scholar] [CrossRef]
- Kaihlanen, A.M.; Virtanen, L.; Buchert, U.; Safarov, N.; Valkonen, P.; Hietapakka, L.; Hörhammer, I.; Kujala, S.; Kouvonen, A.; Heponiemi, T. Towards digital health equity-a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC health services research 2022, 22, 188. [Google Scholar] [CrossRef]
- Martine, G.; Alves, J.E.D. Economy, society and environment in the 21st century: three pillars or trilemma of sustainability? Revista Brasileira de Estudos de População 2015, 32, 433–460. [Google Scholar] [CrossRef]
- Agarwal, B.; Gautam, R.S.; Jain, P.; Rastogi, S.; Bhimavarapu, V.M.; Singh, S. Impact of Environmental, Social, and Governance Activities on the Financial Performance of Indian Health Care Sector Firms: Using Competition as a Moderator. Journal of Risk and Financial Management 2023, 16, 109. [Google Scholar] [CrossRef]
- Pentescu, A.; Cetină, I.; Orzan, G. Social media’s impact on healthcare services. Procedia Economics and Finance 2015, 27, 646–651. [Google Scholar] [CrossRef]
- Raghupathi, V.; Raghupathi, W. Healthcare expenditure and economic performance: insights from the United States data. Frontiers in public health 2020, 8, 156. [Google Scholar] [CrossRef]
- ŞENKARDEŞ, İ.Ç.G. A Discussion On The Effects Of Blockchain Technology Within The Context Of Sustainable Development. Bilgi ve İletişim Teknolojileri Dergisi 2021, 3, 243–262. [Google Scholar] [CrossRef]
- Schmitt, T.; Haarmann, A. Financing health promotion, prevention and innovation despite the rising healthcare costs: How can the new German government square the circle? Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen 2023, 177, 95–103. [Google Scholar] [CrossRef]
- Popov, V.V.; Kudryavtseva, E.V.; Kumar Katiyar, N.; Shishkin, A.; Stepanov, S.I.; Goel, S. Industry 4.0 and digitalisation in healthcare. Materials 2022, 15, 2140. [Google Scholar] [CrossRef]
- Konttila, J.; Siira, H.; Kyngäs, H.; Lahtinen, M.; Elo, S.; Kääriäinen, M.; Kaakinen, P.; Oikarinen, A.; Yamakawa, M.; Fukui, S.; others. Healthcare professionals’ competence in digitalisation: A systematic review. Journal of clinical nursing 2019, 28, 745–761. [Google Scholar] [CrossRef]
- Botrugno, C. Information technologies in healthcare: Enhancing or dehumanising doctor–patient interaction? Health 2021, 25, 475–493. [Google Scholar] [CrossRef]
- Bertakis, K.D. The influence of gender on the doctor–patient interaction. Patient education and counseling 2009, 76, 356–360. [Google Scholar] [CrossRef]
- Kabanda, G. Cybersecurity risk management plan for a blockchain application model. Trans Eng Comput Sci 2021, 2, 221. [Google Scholar]
- Mahgoub, I.M.; Abdelrahman, A.; Abdallah, T.A.; Mohamed Ahmed, K.A.H.; Omer, M.E.A.; Abdelrahman, E.; Salih, Z.M.A. Psychological effects of the COVID-19 pandemic: Perceived stress, anxiety, work–family imbalance, and coping strategies among healthcare professionals in Khartoum state hospitals, Sudan, 2021. Brain and Behavior 2021, 11, e2318. [Google Scholar] [CrossRef]
- Torab-Miandoab, A.; Samad-Soltani, T.; Jodati, A.; Rezaei-Hachesu, P. Interoperability of heterogeneous health information systems: a systematic literature review. BMC Medical Informatics and Decision Making 2023, 23, 18. [Google Scholar] [CrossRef] [PubMed]
- Reegu, F.A.; Abas, H.; Gulzar, Y.; Xin, Q.; Alwan, A.A.; Jabbari, A.; Sonkamble, R.G.; Dziyauddin, R.A. Blockchain-Based Framework for Interoperable Electronic Health Records for an Improved Healthcare System. Sustainability 2023, 15, 6337. [Google Scholar] [CrossRef]
- Shakeel, T.; Habib, S.; Boulila, W.; Koubaa, A.; Javed, A.R.; Rizwan, M.; Gadekallu, T.R.; Sufiyan, M. A survey on COVID-19 impact in the healthcare domain: worldwide market implementation, applications, security and privacy issues, challenges and future prospects. Complex & intelligent systems 2023, 9, 1027–1058. [Google Scholar]
- Zubaydi, H.D.; Varga, P.; Molnár, S. Leveraging Blockchain Technology for Ensuring Security and Privacy Aspects in Internet of Things: A Systematic Literature Review. Sensors 2023, 23, 788. [Google Scholar] [CrossRef]
- Qahtan, S.; Yatim, K.; Zulzalil, H.; Osman, M.H.; Zaidan, A.; Alsattar, H. Review of healthcare industry 4.0 application-based blockchain in terms of security and privacy development attributes: Comprehensive taxonomy, open issues and challenges and recommended solution. Journal of Network and Computer Applications 2023, 209, 103529. [Google Scholar] [CrossRef]
- Albahri, A.; Duhaim, A.M.; Fadhel, M.A.; Alnoor, A.; Baqer, N.S.; Alzubaidi, L.; Albahri, O.; Alamoodi, A.; Bai, J.; Salhi, A. ; others. A systematic review of trustworthy and explainable artificial intelligence in healthcare: Assessment of quality, bias risk, and data fusion. Information Fusion 2023. [Google Scholar] [CrossRef]
- Mahajan, H.B.; Rashid, A.S.; Junnarkar, A.A.; Uke, N.; Deshpande, S.D.; Futane, P.R.; Alkhayyat, A.; Alhayani, B. Integration of Healthcare 4.0 and blockchain into secure cloud-based electronic health records systems. Applied Nanoscience 2023, 13, 2329–2342. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Jindal, N.; Singh, H.; Rana, P.S. Applications and Challenges in Healthcare Big Data: A Strategic Review. Current Medical Imaging 2023, 19, 27–36. [Google Scholar] [CrossRef]
- Guo, C.; Chen, J. Big data analytics in healthcare. In Knowledge Technology and Systems: Toward Establishing Knowledge Systems Science; Springer, 2023; pp. 27–70.
- El Khatib, M.; Hamidi, S.; Al Ameeri, I.; Al Zaabi, H.; Al Marqab, R. Digital Disruption and Big Data in Healthcare-Opportunities and Challenges. ClinicoEconomics and Outcomes Research 2022, 563–574. [Google Scholar] [CrossRef]
- Khan, M.I.; Loh, J. Benefits, challenges, and social impact of health care providers’ adoption of social media. Social Science Computer Review 2022, 40, 1631–1647. [Google Scholar] [CrossRef]
- Jacob, C.; Sezgin, E.; Sanchez-Vazquez, A.; Ivory, C. Sociotechnical factors affecting patients’ adoption of mobile health tools: systematic literature review and narrative synthesis. JMIR mHealth and uHealth 2022, 10, e36284. [Google Scholar] [CrossRef]
- Siyal, A.A.; Junejo, A.Z.; Zawish, M.; Ahmed, K.; Khalil, A.; Soursou, G. Applications of blockchain technology in medicine and healthcare: Challenges and future perspectives. Cryptography 2019, 3, 3. [Google Scholar] [CrossRef]

| Ref | Publisher and Year | Paper Title | Problem Focused | Sustainability Aspects Focused | ICT Integration Technology | Security and Privacy Challenges | Design and Integration Challenges | E-Health Related Applications | Future Directions |
|---|---|---|---|---|---|---|---|---|---|
| [10] | PLOS ONE 2022 | Impact of cybersecurity measures on improving institutional governance and digitalization for sustainable healthcare | To assess the relationship between digitalization and security for healthcare | Social and Economic | N/A | N/A | N/A | N/A | Proposed model can be applied to other SDGs |
| [11] | Springer 2021 | The role of E-Governance in combating COVID-19 and promoting sustainable development: A comparative study of China and Pakistan | To investigate the role of e-governance in combating COVID-19 | Social and Economic | N/A | N/A | N/A | N/A | Financial technology can provide solutions to health crises such as the COVID-19 pandemic |
| [12] | MDPI 2021 | Application of IoT in Healthcare: Keys to Implementation of the SDGs | (a) Are IoT applications key to the improvement of people’s health and the environment? (b) Are there research and case studies implemented in cities or territories that demonstrate the effectiveness of IoT applications and their benefits to public health? (c) What sustainable development indicators and objectives can be assessed in the applications and projects analyzed | Environment | IoT | N/A | N/A | Intelligent Solutions (Vaccine and drug manufacturing, logistics, population vaccination planning and management, data management, and patient monitoring at home) | Security for management of intelligent systems IoT-based framework for SDGs |
| [13] | MDPI 2023 | 5G Technology in the Digital Transformation of Healthcare, a Systematic Review | Analyse the impact of the 5G network on the use of apps to improve healthcare | N/A | 5G | N /A | N/A | Telemedicine | 5G-based technologies to facilitate monitoring and tracking for better healthcare |
| [14] | MDPI 2022 | Modeling Conceptual Framework for Implementing Barriers of AI in Public Healthcare for Improving Operational Excellence: Experiences from Developing Countries | To understand the significance of AI and its implementation barriers in the healthcare systems in developing countries | Social and Economic | AI | Privacy | Governance, Scalability | N/A | various perspectives on the design and development of the conceptual framework can be further expanded and empirically developed from the viewpoint of sustainable public healthcare systems |
| [15] | MDPI 2023 | State-of-the-Art of AI and Big Data Analytics Reviews in Five Different Domains: A Bibliometric Summary | To explore the AI and Big data technologies for different emerging fields (Business, Engineering, Healthcare, Sustainable Operations, and Hospitality Tourism) | N/A | AI and Big data | N/A | N/A | N/A | Specialization in AI sub-domains and BDA tools, AI and BDA in selected management domains, contributing to Smaller thematic areas, Empirical research base, Legal and ethical concerns |
| [16] | IBIMA 2022 | The Sustainable e-Health System Development in COVID-19 Pandemic - The Theoretical Studies of Knowledge Management Systems and Practical Polish Healthcare Experience | To describe the theoretical issues of sustainable development in e-health, and to show practical issues of ICT | N/A | AI | N/A | N/A | Electronic Cards (Insurance, Verification, Prescription, Medical Events, Drug monitoring, network patient information) | Barriers of ICT implementation in the healthcare system. |
| [17] | MDPI 2023 | Digital Transformation in Healthcare: Technology Acceptance and Its Applications | To examine the effects of digital transformation on the healthcare industry | N/A | IoT | Security | N/A | Telemedicine | N/A |
| [18] | De Gruyter 2023 | Digital Transformation and Sustainability in Healthcare and Clinical Laboratories | Study examines the existing data about the influence of digital technology on healthcare and clinical labs | Environmental | N/A | N/A | N/A | Telemedicine and Teleworking | N/A |
| [19] | Plos Digital Health 2023 | Healthcare inequity and digital health–A bridge for the divide, or further erosion of the chasm? | The present state of disparity and inequity to assess the ramifications of digital health | N/A | N/A | N/A | N/A | N/A | N/A |
| [20] | MDPI 2023 | Legacy of COVID-19 Innovations: Strengthening African Primary Health Care through Pandemic Innovations | How are technologies that were originally created for the purpose of addressing the COVID-19 pandemic being employed to enhance the capacity and effectiveness of Primary Health Care? | N/A | N/A | Security | Minimalistic Design, Cross Functional Innovations, Modular Designs, Offgrid Capabilities, Interoperability | N/A | N/A |
| [21] | MDPI 2023 | Toward a Comprehensive Understanding and Evaluation of the Sustainability of E-Health Solutions | Evaluate the long-term viability and ecological impact of recently suggested or currently implemented electronic health (e-health) solutions | Social, Economics | N/A | N/A | N/A | N/A | N/A |
| [22] | Frontiers 2023 | ICT applications and the COVID-19 pandemic: Impacts on the individual’s digital data, digital privacy, and data protection | The use of ICT technologies and Users personal data | N/A | Big Data | Privacy and Data Accessibility | N/A | N/A | The present discourse concerns matters pertaining to digital privacy, data-driven methodologies, and legislation governing the protection of data. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





