1. Introduction
Boron neutron capture therapy (BNCT) is an innovative non-invasive radiotherapy approach for the treatment of cancers such as high-grade gliomas that utilizes the nuclear reaction of the stable isotope boron-10 (
10B) and thermal neutrons to generate high-linear-energy particles [1-4]. The approved accelerator-based BNCT for head and neck cancers in Japan has marked a significant advancement [
5]; however, current treatments such as 4-borono-L-phenylalanine (L-BPA) are not effective for all patients because of the variability in the expression levels of L-type amino acid transporter 1 (LAT-1), which is responsible for BPA uptake into cancer cells [
6].
The limitations associated with the current boron carriers necessitate the development of novel carriers. Our previous studies introduced a maleimide-functionalized
closo-dodecaborate sodium form (MID) and its albumin conjugate (MID-AC) [
7,
8]. We have previously demonstrated that MID-AC selectively accumulates in tumors and significantly inhibits tumor growth in a mouse colon tumor model [
7,
9,
10]. Importantly, our results revealed the potential of MID-AC to effectively deliver boron for BNCT to treat high-grade gliomas because of its efficient induction of boron neutron capture reactions in the tumor cell nucleus and its prolonged retention in tumor cells [
11]. However, the application of MID-AC is limited by the requirement of high total injection doses [
11].
In the continued pursuit of enhancing the therapeutic potential of BNCT and reducing the total injection dose, attention has been focused on the use of small-molecule albumin ligands [
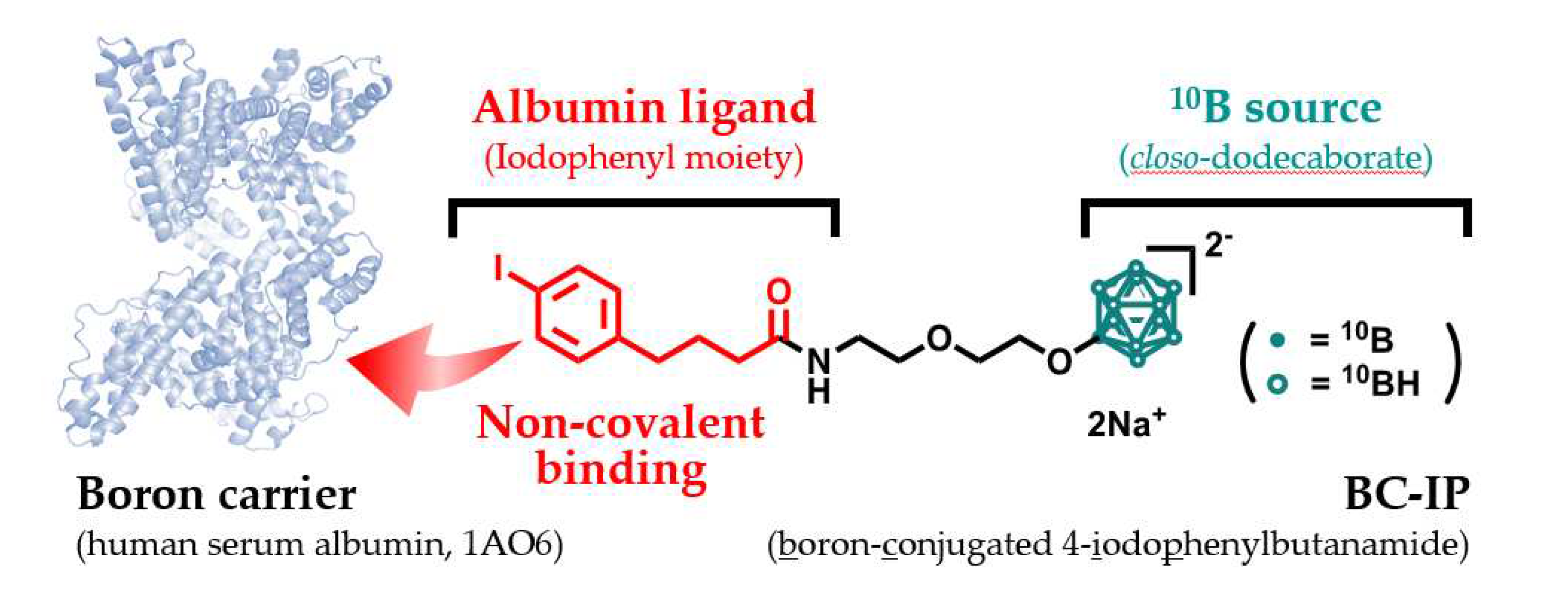
12]. Our strategy is designed to form an albumin-boron conjugate post-injection in the blood, rather than preparing it pre-administration. In this context, boron-conjugated 4-iodophenylbutanamide (BC-IP) is a promising candidate [
13].
This study aimed to further explore the use of BC-IP as a boron carrier in BNCT, with a particular focus on in vivo tumor accumulation and its potential impact on the treatment of high-grade gliomas. The main objective of this study was to validate the enhanced therapeutic potential of BNCT combined with BC-IP, an innovative approach that has been extensively explored through in vivo studies using neutron irradiation. This underscores the commitment of this research to real-world applications and efficacy, moving beyond laboratory settings and animal models to provide meaningful insights relevant to clinical oncology. The insights gained from this study will significantly advance our understanding of the clinical translation of BNCT.
2. Materials and Methods
2.1. Boron Compounds
BC-IP with a molecular weight (MW) of 563 was successfully synthesized according to a previous study [
13]. Briefly, the synthesis of BC-IP involved a series of reactions, starting with
closo-dodecaborate, which was transformed into a 1,4-dioxane-closo-dodecaborate complex. This was further modified by amination and iodination to yield water-soluble BC-IP. The solubility of this compound is a crucial characteristic of potential clinical boron carriers. The chemical structure of BC-IP is shown in
Figure A1. The L-BPA was provided by Interpharma Praha (Prague, Czech Republic). Subsequently, BPA-fructose complex were prepared [
14]. Notably, all compounds used in this study were enriched with boron-10.
2.2. Cell Culture
The rat glioma cell lines F98 and C6 were used in this study. These cells were respectively obtained from Dr. Rolf Barth at Ohio State University (Columbus, Ohio, USA) and the Japan Collection of Research Bioresources (JCRB) Cell Bank, (National Institute of Biomedical Innovation, Osaka, Japan). All cell cultures were maintained in a medium formulation commonly used in our laboratory, as previously described [
11,
15,
16]. This medium was based on Dulbecco’s modified Eagle’s medium (DMEM), supplemented with 10% fetal bovine serum (FBS), the antibiotics penicillin and streptomycin, and the antifungal agent amphotericin B. The culture conditions were maintained at 37℃ within an atmosphere comprising 5% CO
2. All necessary components for the formulation of the culture medium were sourced from Gibco Invitrogen (Grand Island, NY, USA).
2.3. In Vitro Cellular Uptake of Boron
Intracellular uptake of boron was evaluated using F98 and C6 glioma cells. A total of 4×105 cells were plated in a 100-mm dish (Becton, Dickinson, and Company, Franklin Lakes, NJ, USA) and cultured for three days until they reached near-confluency. The culture medium was then replaced with fresh medium containing either 10 µg B/mL of BPA or BC-IP. The cells were subsequently incubated for an additional 3, 6, and 24 h at 37°C. For boron retention studies, the cells were treated with 10 µg B/mL of BPA or BC-IP for 24 hours, after which the medium was replaced with a boron-free medium and incubated for further 1, 3, 6, or 24 hours. Following incubation, the cells were rinsed twice with cold phosphate-buffered saline (PBS). Subsequently, we detached the cells using trypsin-ethylenediamine tetraacetic acid solution. The cells were collected by centrifugation at 200 × g for 5 min and washed with cold PBS. This procedure was performed twice in order to remove boron attached to the cell membrane. The cells were then digested with 1 N nitric acid solution (FUJIFILM Wako Pure Chemical Industries, Osaka, Japan) overnight at room temperature. The boron concentration of the cell lysate was measured via inductively-coupled plasma atomic emission spectroscopy (ICP-AES) (iCAP6300 emission spectrometer, Hitachi High-Technologies, Tokyo, Japan). The boron concentration within the cells was expressed as micrograms of boron (B) per 109 cells.
2.4. Rat Glioma Model Using F98 Cells
This study used male Fischer rats, each approximately 10 weeks old and weighing between 200 and 250 g. The rats were rendered unconscious through intraperitoneal administration of a cocktail of anesthetics: medetomidine (0.4 mg/kg; ZENOAQ, Fukushima, Japan), midazolam (2.0 mg/kg; SANDOZ, Yamagata, Japan), and butorphanol (5.0 mg/kg; Meiji Seika, Tokyo, Japan). The head of each rat was secured using a stereotactic frame (Model 900; David Kopf Instruments, Tujunga, CA, USA). After a head skin incision was made using a scalpel, a 1-mm burr hole was made 1 mm posterior to the bregma and 4 mm to the right lateral side. Subsequently, F98 rat glioma cells were implanted into the right brains of these rats. For therapeutic trials, a suspension of 10
3 F98 rat glioma cells in 10 µL DMEM containing 1.4% agarose (Wako Pure Chemical Industries, Osaka, Japan) was used. For biodistribution investigations, 10
5 F98 rat glioma cells were injected. All injections were conducted at a steady rate of 20 µL/min and regulated by an automated infusion pump. These surgical procedures have been established and regularly used by our research team in previous studies [
11,
15,
16].
All procedures involving animals adhered to "the Guide for the Care and Use of Laboratory Animals" and were approved by two distinct ethical committees: the Animal Use Review Board of Osaka Medical and Pharmaceutical University (Approval No. 2019-029) and the Ethical Committee of the Institute for Integrated Radiation and Nuclear Science at Kyoto University (KURNS; Kumatori, Osaka, Japan) (Approval No. 2019-9).
2.5. Biodistribution Study of Boron Agent in F98 Glioma Model
To assess the biodistribution of boron, the rats were implanted with 105 F98 glioma cells and treated with BC-IP at doses of 5, 10, or 20 mg boron (B) per kg body weight (b.w.) approximately 12-14 days post-implantation, a time window anticipated to allow substantial tumor growth. The animals were subsequently euthanized at predetermined time points and various tissue samples — namely tumor, brain, blood — were harvested and weighed. Each collected tissue sample was then processed by digestion in a 1N nitric acid solution for 1 week, followed by boron quantification using ICP-AES. The boron concentrations obtained from these assays are expressed as micrograms of boron (B) per gram of tissue.
2.6. Survival Analysis of Neutron Irradiation Study for Rat Glioma Models
Survival analysis of in vivo neutron irradiation experiments was performed 15 days after implantation of 103 F98 glioma cells. The study involved a total of 20 rats with F98 glioma, which were randomly assigned into four groups: those left untreated (control, n = 5), those received neutron irradiation only (irradiation only, n = 2), neutron irradiation following 2.5 h after intravenous BPA administration (BNCT with BPA, n = 5), and those subjected to neutron irradiation 3 h after intravenous BC-IP administration (BNCT with BC-IP, n = 8). To ensure experimental consistency, all rats were anesthetized prior to the procedures, and either BPA or BC-IP was administered to the relevant groups according to the study design. To concentrate the neutron irradiation exclusively on their heads, all rat bodies were shielded with a plate lined with 6LiF ceramic tiles to minimize extraneous exposure. Targeted neutron irradiation was then carried out at the Heavy Water Irradiation Facility at KURNS, with a reactor power of 5 MW and neutron flux of 9.6 × 108 neutrons/cm2/s for a duration of 20 min. After irradiation, all rats were monitored until death or euthanasia. The therapeutic effect of the different treatments was evaluated using Kaplan-Meier survival curves, and the percent increase in life span (%ILS) was computed using the following formula: [(Median Survival Time (MST) of each BNCT group – MST of untreated control group) × 100]/MST of the untreated control group.
2.7. Assessing Physical Absorbed Dosages and Compound Biological Effectiveness in In Vivo Neutron Irradiation
The physically-absorbed dose — accounting for thermal, epithermal, and fast neutrons as well as gamma rays — was calculated using the formula D
B + D
N + D
H + D
γ. Here, each component corresponds to the different capture reactions:
10B(n,α)
7Li (D
B),
14N(n,p)
14C (D
N), and
1H(n,n)
1H (D
H), along with gamma-ray (D
γ). Thermal neutron fluence was determined from the radioactivity of gold foil attached to the heads of the irradiated rats. The doses absorbed to the brain and the tumor in the F98 rat glioma model during BNCT (using BPA and BC-IP) were calculated using data from biodistribution experiments. The estimated photon-equivalent dose was calculated using the equation D
B × compound biological effectiveness (CBE) + D
N × relative biological effectiveness of nitrogen (RBE
N) + D
H × relative biological effectiveness of hydrogen (RBE
H) + D
γ [
17], where RBE
N and RBE
H are both assumed to be 3.0 [
5,
18]. The CBEs for normal brain tissue and brain tumor tissue treated with BPA were determined to be 1.35 and 3.8, respectively [18-20]. Since BC-IP is quite similar in structure to MID-AC, the CBE of BC-IP was assumed to be 13.4, the same as MID-AC [
11].
2.8. Statistical Analysis
During the in vitro cellular uptake studies, boron concentrations within different cell lines were analyzed using Student's t-test. Kaplan-Meier curves were used to analyze the survival times. Any significant variance among the groups was determined using log-rank tests. Statistical significance was set at p < 0.05 (and deemed significant). All data were processed using JMP® Pro 16.2.0 software (SAS Institute, Cary, NC, USA).
3. Results
3.1. In Vitro Cellular Uptake of Boron
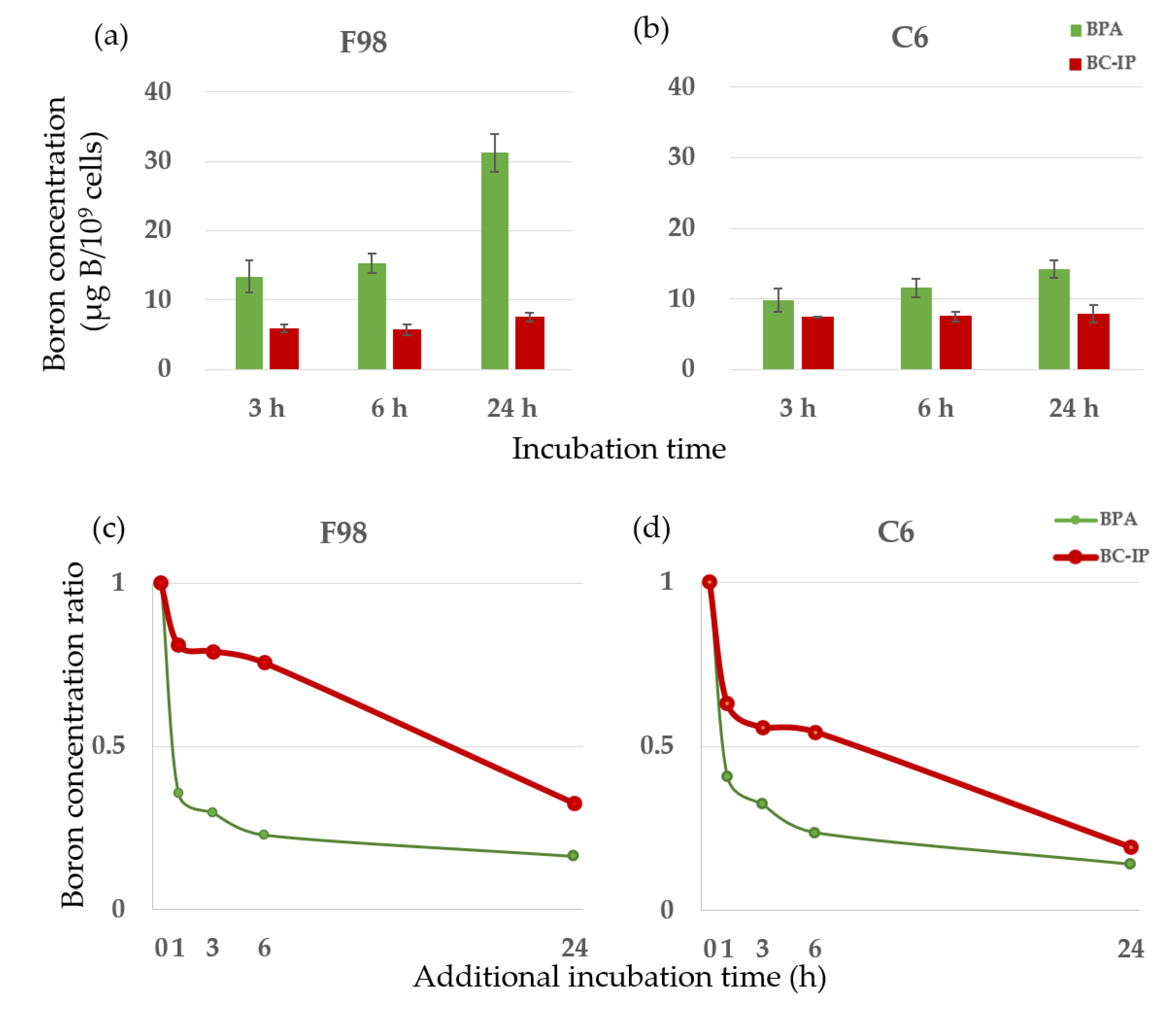
In this study, we used two types of boron carriers — BPA and BC-IP — on F98 and C6 glioma cells. The boron concentrations in both cell types after exposure to either boron carrier from 1 to 24 h showed an increasing trend over time for both BPA and BC-IP. In terms of boron retention, from 1 to 24 h, BPA showed a significantly higher boron concentration in both cell lines compared to BC-IP (
p < 0.05, Student’s t-test). However, from 24+1 h to 24+24 h, the boron retention rate was significantly higher in BC-IP treated cells than in the BPA-treated cells (
p < 0.05, according to Student’s t-test). After switching to a boron-free medium, the boron retention rates for BPA and BC-IP after an additional 1 h of incubation were 35.6% and 81.0% in F98 glioma cells and 40.5% and 63.0% in C6 glioma cells, respectively. After 6 and 24 h of incubation, these rates were 22.8% and 75.6% (6 h) and 16.3% and 32.5% (24 h) in F98 glioma cells, and 23.6% and 54.3% (6 h) and 14.0% and 19.1% (24 h) in C6 glioma cells, respectively. When switched to a boron-free medium, boron retention in BPA-treated cells decreased rapidly, whereas BC-IP-treated cells showed a gradual decrease in boron retention over time. The results are shown in
Figure 1.
3.2. Biodistribution Study of the Boron Agent in F98 Glioma Model
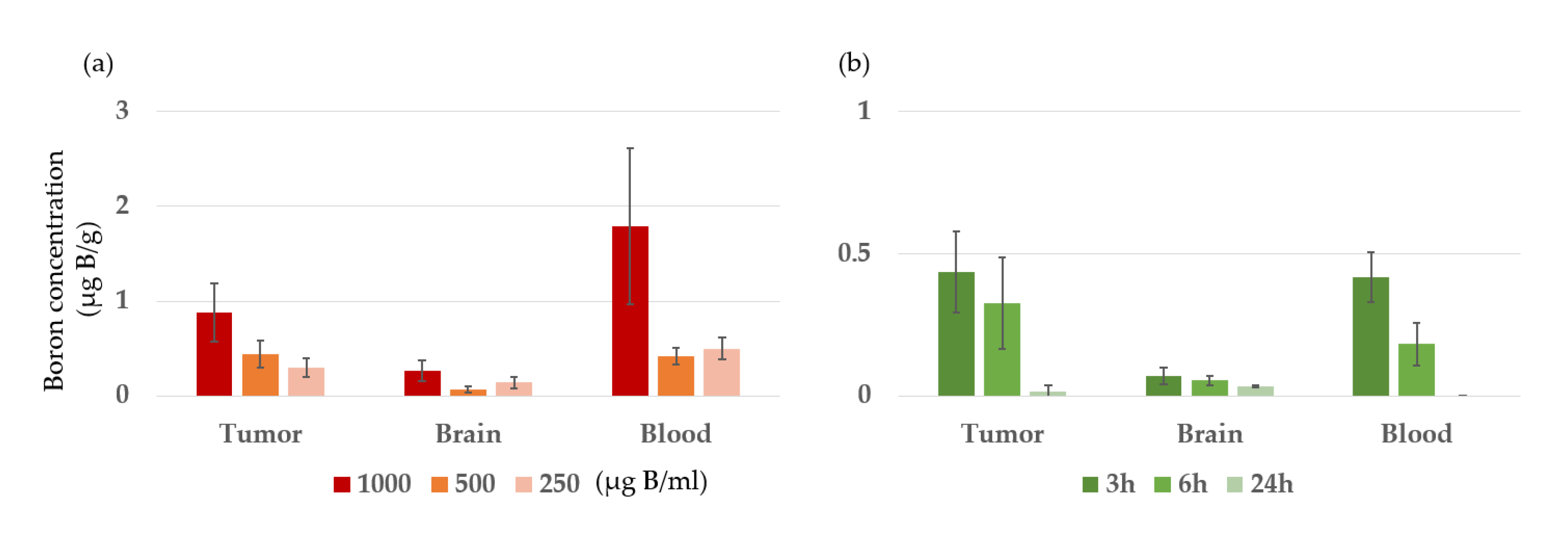
Boron concentrations in tumors, normal brain tissue, and blood of F98 glioma-bearing rats were measured 3 hours after intravenous (i.v.) administration of BC-IP at 1,000, 500, and 250 µg B/ml (20 mg B/kg). In addition, BC-IP was administered at 500 µg B/ml (20 mg B/kg) and then boron concentrations were measured 3, 6, and 24 hours later. The results are shown in
Figure 2 and
Table 1. In the former, the boron concentration increased in a concentration-dependent manner. The tumor-to-normal brain ratios at 1,000, 500, and 250 µg B/ml were found to be 3.3, 6.4, and 2.1, respectively, while the tumor-to-blood ratios were 0.5, 1.04, and 0.6, respectively. For the latter, boron concentrations were highest 3 h after BC-IP administration and then decreased over time.
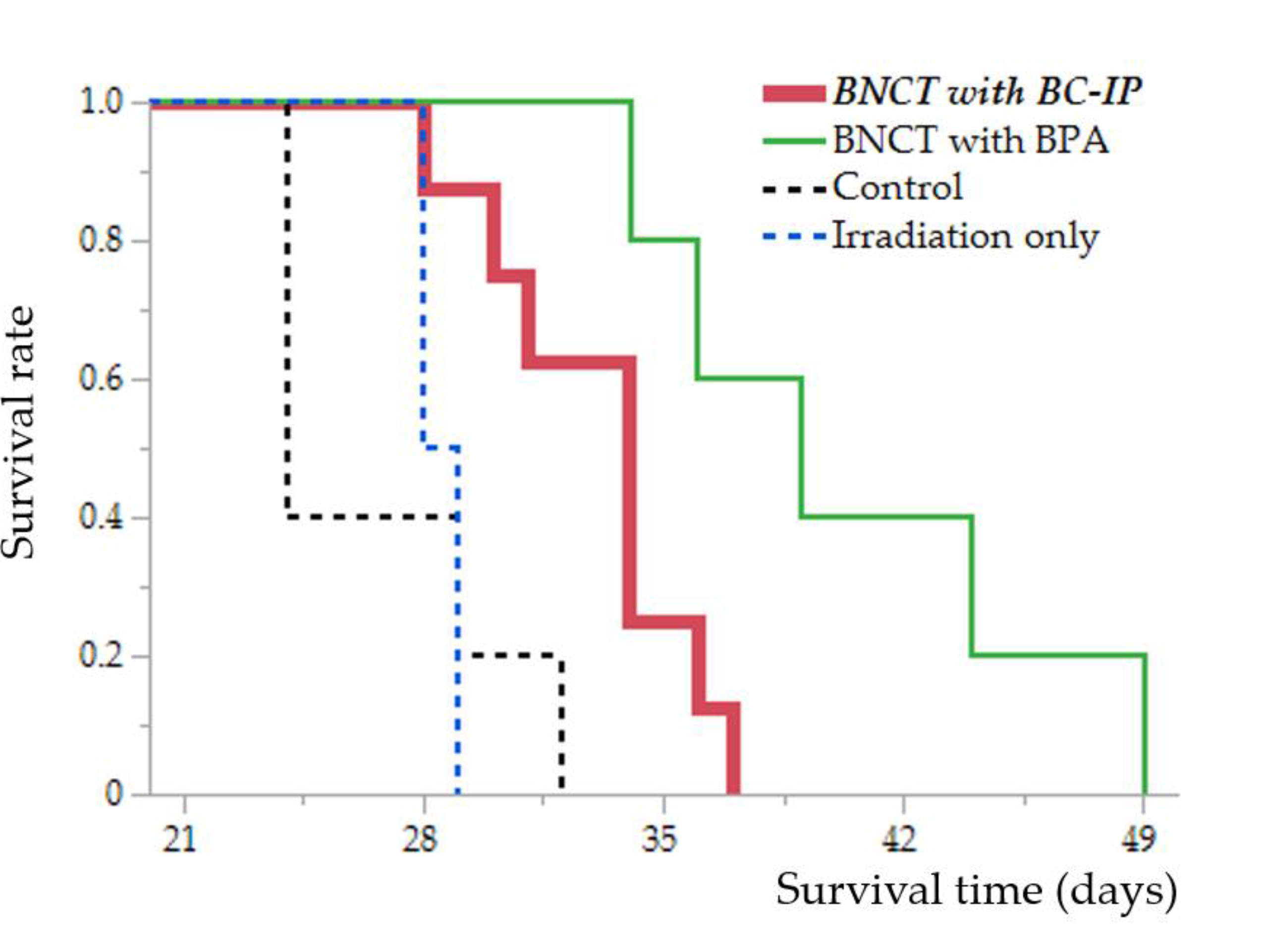
3.3. In Vivo Survival Analysis of the Neutron Irradiation Study
The MSTs for each group are as follows: control group, 24 days [95% Confidence Interval (CI), 24–32 days]; irradiation only group, 28.5 days [95% CI, 28–29 days]; BNCT with BPA group, 39 days [95% CI, 34–49 days]; and BNCT with BC-IP group, 34 days [95% CI, 28–37 days].
Although the BNCT with BC-IP group had a significantly shorter survival extension than the BNCT with BPA group (
p = 0.016, according to the log-rank test), they had a significantly longer survival extension than the untreated control and irradiation only group (compared to the control group,
p = 0.0086; compared to the irradiation only group,
p = 0.019, respectively, log-rank test) (
Figure 3).
The %ILS values were as follows: BNCT with BC-IP, 41.7%, and BNCT with BPA, 62.5%. A detailed description of these results is presented in
Table 2.
3.4. Assessing Physical Dosages and Compound Biological Effectiveness of In Vivo Neutron Irradiation
The physical and photon-equivalent doses delivered to the brains and tumors during neutron irradiation experiments were estimated using the CBE factor for each boron carrier, which was derived from reference data [
11]. This estimation also considered the average tumor boron concentrations obtained from in vivo biodistribution studies [
16]. The estimated photon-equivalent doses delivered to the tumor during BPA-BNCT at 2 h was 13.7 Gy-Eq. In contrast, for BNCT with BC-IP at 3 h, the doses were 4.6 Gy-Eq (
Table 3).
4. Discussion
This study focused on the application of BC-IP, a novel boron carrier, in BNCT for the treatment of high-grade gliomas. Through extensive in vivo studies, including neutron irradiation, we observed promising results, highlighting the potential of BC-IP to enhance the therapeutic potential of BNCT.
Human serum albumin (HSA) is the most abundant polypeptide protein in blood plasma. HSA, which weighs 66.5 kDa and consists of 585 amino acids, is present in the plasma at concentrations of 35-50 g/L [21-23]. It has many important physiological functions. For example, it significantly contributes to the regulation of plasma oncotic pressure and fluid distribution. It also functions as a transport molecule for various internal and external substances due to its remarkable ligand-binding capacity [
24]. In addition, HSA accumulates in malignant tumor and inflammatory tissues because of the enhanced permeability and retention (EPR) effect [
9,
25]. Furthermore, rapidly-growing tumor cells significantly take up significant amounts of extracellular proteins, including serum albumin, which represents to the total volume of extracellular proteins in the tumor cytoplasm. This is due to the fact that serum albumin serves as an important nutrient source for tumors to grow [
26,
27]. Hence, HSA has been studied as a potential drug delivery system. As an example, nab-paclitaxel — an albumin-paclitaxel nanoparticles complex — was first approved in the United States for the treatment of metastatic breast cancer in 2005 [
28,
29]. Thereafter, FDA expanded approval to other type of cancers, such as non-small cell lung cancer and pancreatic cancer [
30,
31]. Upon intravenous administration, nab-paclitaxel transforms into soluble albumin-bound complexes that accumulate in tumors via mechanisms such as transcytosis and the EPR effect [
32]. Some albumin-drug conjugates are currently under clinical study, including the methotrexate-albumin conjugate (MTX-HSA) and the doxorubicin maleimide derivative (INNO-206) [10,33-38]. Considering these factors, we believe that albumin can serve as an effective boron carrier for BNCT. Accordingly, we have been engaged in the development and research of albumin-related drugs for BNCT in recent years [
7,
11,
13,
15].
Recently, we reported that BNCT with MID-AC was effective in the F98 glioma rat model [
11]. This study demonstrated that the drug remained in the tumor for an extended period, suggesting its potential for a stable and sustained boron capture reaction through neutron irradiation. However, a challenge with this drug is its increased molecular weight due to the conjugation of albumin during the synthesis stage, leading to the requirement for a larger dosage. For the MID albumin conjugates, a boron dose of 7.5 mg/kg body weight was equivalent to a total dose of 420 mg/kg body weight [
10,
39]. To address this issue, we developed BC-IP, a compound that can bind to albumin in the blood after intravenous administration [
13].
In the in vitro drug exposure experiments, BC-IP exhibited significantly lower intracellular boron uptake than BPA, with only a slight increase in uptake as the exposure time was extended (
Figure 1-a, b). In contrast, in terms of clearance, a large proportion of BPA was expelled one hour after exposure, whereas BC-IP displayed superior retention (
Figure 1-c, d). Because BC-IP was originally designed to bind with albumin in the blood after intravenous administration, its precise behavior in this in vitro experiment is unclear. Although the boron concentration in BC-IP was lower than that in BPA, this may be attributed to the unique characteristics of the drug. However, the high retention rate of BC-IP indicates its potential suitability as a boron carrier for BNCT. This property is particularly significant, considering the current limitations of BPA, the sole boron compound approved for clinical use. Our in vitro results indicated that BPA was rapidly eliminated from the blood upon cessation of administration. Other studies also showed that BPA was quickly cleared after exposure was terminated [
40,
41]. Therefore, in current clinical BNCT, patients must be continuously administered large amounts of BPA to maintain the necessary concentration of boron in the blood throughout neutron irradiation [
42]. The superior retention rate of BC-IP could alleviate this issue, indicating its potential as a novel boron carrier for BNCT.
In the in vivo biodistribution study, we evaluated boron concentrations in the tumor, normal brain, and blood of F98 glioma-bearing rats following the intravenous administration of the boron compound BC-IP at various concentrations. The results showed that the boron concentration increased with the administered dose. In addition, boron concentrations peaked at 3 h after BC-IP administration and gradually decreased over time. Therefore, we performed our in vivo neutron irradiation experiment 3 h after the administration of BC-IP concentration of 1000 µg B/ml (20mg B/kg). However, boron accumulation in the tumor was quite low, which may explain the shorter survival time in the irradiation experiment compared to BNCT with BPA group. By time, boron accumulation in tumors decreased over time, and boron accumulation was almost completely cleared 24 h after administration; however, the T/Br ratio was high at both 3 and 6 h after administration. Although boron accumulation needs to be improved, based on the in vitro boron clearance results, irradiation at 6 h after BC-IP administration may provide a survival benefit equivalent to 3 h after administration because of the relatively high retention rate up to the 6-hour time point. The high retention rate may avoid the need for a continuous infusion of boron compounds, as mentioned earlier, and may allow for a variety of the irradiation plans such as adjusting the irradiation time and flexible scheduling.
In our in vivo neutron irradiation study, although the prolonged survival in the BC-IP group that received BNCT was not as favorable as that in the BPA group, it was still significantly longer than the prolonged survival observed in both the untreated control and irradiation-only group. It is worth noting that although boron accumulation in the tumor was low in BC-IP in our biodistribution study, the results were better than those of the control groups. BPA enters the tumor mainly via LAT-1 [
6], whereas the novel compound BC-IP enters the tumor via the EPR effect [
25]. In other words, these agents are taken up through different mechanisms. Therefore, BC-IP alone is not sufficiently effective. However, when used in combination with BPA, it may contribute to solving the problem of BPA-negative cells.
However, glioma cells infiltrate the normal brain parenchyma where the blood-brain barrier (BBB) remains intact. Therefore, the delivery of these agents remains a major challenge. Our solution to overcome this challenge may be convection-enhanced delivery (CED), which allows for the direct administration of therapeutic agents into the tumor or brain parenchyma. This technique bypasses the BBB using pressure-driven bulk flow, offering significant pharmacokinetic advantages over traditional IV administration [43-45]. Therefore, the combination of CED and novel boron carriers such as BC-IP could potentially enhance the effectiveness of BNCT treatment for high-grade gliomas. However, this would require the use of molecular targets or other modifications to BC-IP. We suggest that bevacizumab (BEV), an anti-vascular endothelial growth factor (VEGF) antibody, is another option. In clinical practice, the addition of bevacizumab to BNCT has already been shown to prolong survival [
46], and is expected to be an effective treatment regimen in the future.
5. Conclusions
Our research illustrates the potential of BC-IP as an alternative boron carrier for BNCT, specifically within the context of an F98 glioma model. Despite BC-IP displaying lower intracellular boron uptake in comparison to BPA, it exhibits superior retention, highlighting its potential for future BNCT applications. Continued research is crucial to optimize these methodologies, promising significant advancements in BNCT for glioma treatment.
Author Contributions
Conceptualization, S.K.; methodology, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo), K.T., H.K., R.H., N.N., M.F. and S.K.; validation, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo), K.T. and S.K.; formal analysis, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo) and K.T.; investigation, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo), K.T. and S.K.; resources, K.N., H.N., T.T. (Takushi Takata), H.T., N.H., T.W., M.S., T.T. (Toshihiro Takami) and S.K.; data curation, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo) and K.T.; writing—original draft preparation, Y.F. (Yoshiki Fujikawa) and Y.F. (Yusuke Fukuo); writing—review and editing, S.K.; visualization, Y.F. (Yoshiki Fujikawa), Y.F. (Yusuke Fukuo), K.T. and S.K.; supervision, S.K., S.-I.M. and M.W.; project administration, S.K.; funding acquisition, S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Japan Society for the Promotion of Science (JSPS) KAKENHI, grant number JP23H03024 to S.K. [Grants-in-Aid for Science Research (B)].
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Animal Use Review Board and Ethical Committee of Osaka Medical and Pharmaceutical University (No. 2019-029) and the Institute for Integrated Radiation and Nuclear Science, Kyoto University (KURNS; Kumatori, Osaka, Japan) (No. 2019-9).
Informed Consent Statement
Not applicable.
Data Availability Statement
All data analyzed in this study are available upon reasonable request from corresponding author. The JMP Pro version 16.2.0. software (SAS, Cary, NC, USA) was used for the statistical analysis.
Acknowledgments
The authors would like to acknowledge Dr. Rolf Barth (Ohio State University, Columbus, Ohio, USA) for providing cells line: F98. The authors also thank Aya Sunamura for her secretarial work, and Itsuko Inoue for her technical assistance.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Figure A1.
The chemical structure and synthetic scheme of BC-IP.
Figure A1.
The chemical structure and synthetic scheme of BC-IP.
References
- Yamamoto, T.; Nakai, K.; Matsumura, A. Boron neutron capture therapy for glioblastoma. Cancer Lett 2008, 262, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Soloway, A.H.; Tjarks, W.; Barnum, B.A.; Rong, F.G.; Barth, R.F.; Codogni, I.M.; Wilson, J.G. The Chemistry of Neutron Capture Therapy. Chem Rev 1998, 98, 1515–1562. [Google Scholar] [CrossRef] [PubMed]
- Kato, I.; Ono, K.; Sakurai, Y.; Ohmae, M.; Maruhashi, A.; Imahori, Y.; Kirihata, M.; Nakazawa, M.; Yura, Y. Effectiveness of BNCT for recurrent head and neck malignancies. Appl Radiat Isot 2004, 61, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Kageji, T.; Nagahiro, S.; Mizobuchi, Y.; Matsuzaki, K.; Nakagawa, Y.; Kumada, H. Boron neutron capture therapy (BNCT) for newly-diagnosed glioblastoma: comparison of clinical results obtained with BNCT and conventional treatment. J Med Invest 2014, 61, 254–263. [Google Scholar] [CrossRef]
- Suzuki, M.; Kato, I.; Aihara, T.; Hiratsuka, J.; Yoshimura, K.; Niimi, M.; Kimura, Y.; Ariyoshi, Y.; Haginomori, S.; Sakurai, Y.; et al. Boron neutron capture therapy outcomes for advanced or recurrent head and neck cancer. J Radiat Res 2014, 55, 146–153. [Google Scholar] [CrossRef]
- Detta, A.; Cruickshank, G.S. L-amino acid transporter-1 and boronophenylalanine-based boron neutron capture therapy of human brain tumors. Cancer Res 2009, 69, 2126–2132. [Google Scholar] [CrossRef]
- Kikuchi, S.; Kanoh, D.; Sato, S.; Sakurai, Y.; Suzuki, M.; Nakamura, H. Maleimide-functionalized closo-dodecaborate albumin conjugates (MID-AC): Unique ligation at cysteine and lysine residues enables efficient boron delivery to tumor for neutron capture therapy. J Control Release 2016, 237, 160–167. [Google Scholar] [CrossRef]
- Ishii, S.; Sato, S.; Asami, H.; Hasegawa, T.; Kohno, J.Y.; Nakamura, H. Design of S-S bond containing maleimide-conjugated closo-dodecaborate (SSMID): identification of unique modification sites on albumin and investigation of intracellular uptake. Org Biomol Chem 2019, 17, 5496–5499. [Google Scholar] [CrossRef]
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res 1986, 46, 6387–6392. [Google Scholar]
- Elsadek, B.; Kratz, F. Impact of albumin on drug delivery--new applications on the horizon. J Control Release 2012, 157, 4–28. [Google Scholar] [CrossRef]
- Kashiwagi, H.; Kawabata, S.; Yoshimura, K.; Fukuo, Y.; Kanemitsu, T.; Takeuchi, K.; Hiramatsu, R.; Nishimura, K.; Kawai, K.; Takata, T.; et al. Boron neutron capture therapy using dodecaborated albumin conjugates with maleimide is effective in a rat glioma model. Invest New Drugs 2022, 40, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Chen, X. Simple bioconjugate chemistry serves great clinical advances: albumin as a versatile platform for diagnosis and precision therapy. Chem Soc Rev 2016, 45, 1432–1456. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, K.; Harrison, S.; Kawai, K.; Morita, T.; Miura, K.; Okada, S.; Nakamura, H. Iodophenyl-conjugated closo-dodecaborate as a promising small boron molecule that binds to serum albumin and accumulates in tumor. Bioorg Med Chem Lett 2022, 72, 128869. [Google Scholar] [CrossRef] [PubMed]
- Coderre, J.A.; Button, T.M.; Micca, P.L.; Fisher, C.D.; Nawrocky, M.M.; Liu, H.B. Neutron capture therapy of the 9L rat gliosarcoma using the p-boronophenylalanine-fructose complex. Int J Radiat Oncol Biol Phys 1994, 30, 643–652. [Google Scholar] [CrossRef]
- Tsujino, K.; Kashiwagi, H.; Nishimura, K.; Kayama, R.; Yoshimura, K.; Fukuo, Y.; Shiba, H.; Hiramatsu, R.; Nonoguchi, N.; Furuse, M.; et al. Improved Boron Neutron Capture Therapy Using Integrin αvβ3-Targeted Long-Retention-Type Boron Carrier in a F98 Rat Glioma Model. Biology (Basel) 2023, 12. [Google Scholar] [CrossRef]
- Fukuo, Y.; Hattori, Y.; Kawabata, S.; Kashiwagi, H.; Kanemitsu, T.; Takeuchi, K.; Futamura, G.; Hiramatsu, R.; Watanabe, T.; Hu, N.; et al. The Therapeutic Effects of Dodecaborate Containing Boronophenylalanine for Boron Neutron Capture Therapy in a Rat Brain Tumor Model. Biology (Basel) 2020, 9. [Google Scholar] [CrossRef] [PubMed]
- Kumada, H.; Takada, K. Treatment planning system and patient positioning for boron neutron capture therapy. Ther Radiol Oncol 2018, 2, 50. [Google Scholar] [CrossRef]
- Coderre, J.A.; Morris, G.M. The radiation biology of boron neutron capture therapy. Radiat Res 1999, 151, 1–18. [Google Scholar] [CrossRef]
- Coderre, J.A.; Makar, M.S.; Micca, P.L.; Nawrocky, M.M.; Liu, H.B.; Joel, D.D.; Slatkin, D.N.; Amols, H.I. Derivations of relative biological effectiveness for the high-let radiations produced during boron neutron capture irradiations of the 9L rat gliosarcoma in vitro and in vivo. Int J Radiat Oncol Biol Phys 1993, 27, 1121–1129. [Google Scholar] [CrossRef]
- Yamamoto, T.; Matsumura, A.; Yamamoto, K.; Kumada, H.; Hori, N.; Torii, Y.; Shibata, Y.; Nose, T. Characterization of neutron beams for boron neutron capture therapy: in-air radiobiological dosimetry. Radiat Res 2003, 160, 70–76. [Google Scholar] [CrossRef]
- Executive Committee of the German Medical Association on the Recommendation of the Scientific Advisory, B. Executive Committee of the German Medical Association on the Recommendation of the Scientific Advisory, B. Cross-Sectional Guidelines for Therapy with Blood Components and Plasma Derivatives: Chapter 5 Human Albumin - Revised. In Transfus Med Hemother; Switzerland, 2016; Volume 43, pp. 223–232.
- Yang, X.; Bolsa-Ferruz, M.; Marichal, L.; Porcel, E.; Salado-Leza, D.; Lux, F.; Tillement, O.; Renault, J.P.; Pin, S.; Wien, F.; et al. Human Serum Albumin in the Presence of AGuIX Nanoagents: Structure Stabilisation without Direct Interaction. Int J Mol Sci 2020, 21. [Google Scholar] [CrossRef]
- Jahanban-Esfahlan, A.; Ostadrahimi, A.; Jahanban-Esfahlan, R.; Roufegarinejad, L.; Tabibiazar, M.; Amarowicz, R. Recent developments in the detection of bovine serum albumin. Int J Biol Macromol 2019, 138, 602–617. [Google Scholar] [CrossRef]
- Fanali, G.; di Masi, A.; Trezza, V.; Marino, M.; Fasano, M.; Ascenzi, P. Human serum albumin: from bench to bedside. Mol Aspects Med 2012, 33, 209–290. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Stehle, G.; Sinn, H.; Wunder, A.; Schrenk, H.H.; Stewart, J.C.; Hartung, G.; Maier-Borst, W.; Heene, D.L. Plasma protein (albumin) catabolism by the tumor itself--implications for tumor metabolism and the genesis of cachexia. Crit Rev Oncol Hematol 1997, 26, 77–100. [Google Scholar] [CrossRef] [PubMed]
- Sinn, H.; Schrenk, H.H.; Friedrich, E.A.; Schilling, U.; Maier-Borst, W. Design of compounds having an enhanced tumour uptake, using serum albumin as a carrier. Part I. Int J Rad Appl Instrum B 1990, 17, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Elzoghby, A.O.; Samy, W.M.; Elgindy, N.A. Albumin-based nanoparticles as potential controlled release drug delivery systems. J Control Release 2012, 157, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Gradishar, W.J.; Tjulandin, S.; Davidson, N.; Shaw, H.; Desai, N.; Bhar, P.; Hawkins, M.; O'Shaughnessy, J. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol 2005, 23, 7794–7803. [Google Scholar] [CrossRef]
- Gradishar, W.J.; Krasnojon, D.; Cheporov, S.; Makhson, A.N.; Manikhas, G.M.; Clawson, A.; Bhar, P. Significantly longer progression-free survival with nab-paclitaxel compared with docetaxel as first-line therapy for metastatic breast cancer. J Clin Oncol 2009, 27, 3611–3619. [Google Scholar] [CrossRef]
- Hawkins, M.J.; Soon-Shiong, P.; Desai, N. Protein nanoparticles as drug carriers in clinical medicine. Adv Drug Deliv Rev 2008, 60, 876–885. [Google Scholar] [CrossRef]
- Schnitzer, J.E. gp60 is an albumin-binding glycoprotein expressed by continuous endothelium involved in albumin transcytosis. Am J Physiol 1992, 262, H246–H254. [Google Scholar] [CrossRef]
- Hartung, G.; Stehle, G.; Sinn, H.; Wunder, A.; Schrenk, H.H.; Heeger, S.; Kränzle, M.; Edler, L.; Frei, E.; Fiebig, H.H.; et al. Phase I trial of methotrexate-albumin in a weekly intravenous bolus regimen in cancer patients. Phase I Study Group of the Association for Medical Oncology of the German Cancer Society. Clin Cancer Res 1999, 5, 753–759. [Google Scholar] [PubMed]
- Vis, A.N.; van der Gaast, A.; van Rhijn, B.W.; Catsburg, T.K.; Schmidt, C.; Mickisch, G.H. A phase II trial of methotrexate-human serum albumin (MTX-HSA) in patients with metastatic renal cell carcinoma who progressed under immunotherapy. Cancer Chemother Pharmacol 2002, 49, 342–345. [Google Scholar] [CrossRef]
- Stehle, G.; Sinn, H.; Wunder, A.; Schrenk, H.H.; Schütt, S.; Maier-Borst, W.; Heene, D.L. The loading rate determines tumor targeting properties of methotrexate-albumin conjugates in rats. Anticancer Drugs 1997, 8, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Kratz, F.; Müller-Driver, R.; Hofmann, I.; Drevs, J.; Unger, C. A novel macromolecular prodrug concept exploiting endogenous serum albumin as a drug carrier for cancer chemotherapy. J Med Chem 2000, 43, 1253–1256. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, E.; Li, M.; Wang, C.; Nichols, C.M.; Li, J.; Chen, H.; Berenson, J.R. Anti-myeloma effects of the novel anthracycline derivative INNO-206. Clin Cancer Res 2012, 18, 3856–3867. [Google Scholar] [CrossRef]
- Cho, H.; Jeon, S.I.; Ahn, C.H.; Shim, M.K.; Kim, K. Emerging Albumin-Binding Anticancer Drugs for Tumor-Targeted Drug Delivery: Current Understandings and Clinical Translation. Pharmaceutics 2022, 14. [Google Scholar] [CrossRef]
- Axtell, J.C.; Saleh, L.M.A.; Qian, E.A.; Wixtrom, A.I.; Spokoyny, A.M. Synthesis and Applications of Perfunctionalized Boron Clusters. Inorg Chem 2018, 57, 2333–2350. [Google Scholar] [CrossRef]
- Fukuda, H. Boron Neutron Capture Therapy (BNCT) for Cutaneous Malignant Melanoma Using (10)B-p-Boronophenylalanine (BPA) with Special Reference to the Radiobiological Basis and Clinical Results. Cells 2021, 10. [Google Scholar] [CrossRef]
- Lin, Y.C.; Lee, Y.J.; Chen, Y.W.; Wang, S.Y.; Chou, F.I. Evaluation of the Key Advantages between Two Modalities of Boronophenylalanine Administration for Clinical Boron Neutron Capture Therapy Using an Animal Model. Cells 2022, 11. [Google Scholar] [CrossRef]
- Malouff, T.D.; Seneviratne, D.S.; Ebner, D.K.; Stross, W.C.; Waddle, M.R.; Trifiletti, D.M.; Krishnan, S. Boron Neutron Capture Therapy: A Review of Clinical Applications. Front Oncol 2021, 11, 601820. [Google Scholar] [CrossRef] [PubMed]
- Barth, R.F.; Mi, P.; Yang, W. Boron delivery agents for neutron capture therapy of cancer. Cancer Commun (Lond) 2018, 38, 35. [Google Scholar] [CrossRef] [PubMed]
- Lewis, O.; Woolley, M.; Johnson, D.; Rosser, A.; Barua, N.U.; Bienemann, A.S.; Gill, S.S.; Evans, S. Chronic, intermittent convection-enhanced delivery devices. J Neurosci Methods 2016, 259, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.F.; Thomas, M.G.; Lind, C.R. Neurosurgical convection-enhanced delivery of treatments for Parkinson's disease. J Clin Neurosci 2011, 18, 1163–1167. [Google Scholar] [CrossRef]
- Furuse, M.; Kawabata, S.; Wanibuchi, M.; Shiba, H.; Takeuchi, K.; Kondo, N.; Tanaka, H.; Sakurai, Y.; Suzuki, M.; Ono, K.; et al. Boron neutron capture therapy and add-on bevacizumab in patients with recurrent malignant glioma. Jpn J Clin Oncol 2022, 52, 433–440. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).