Submitted:
19 July 2023
Posted:
21 July 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Case Reports
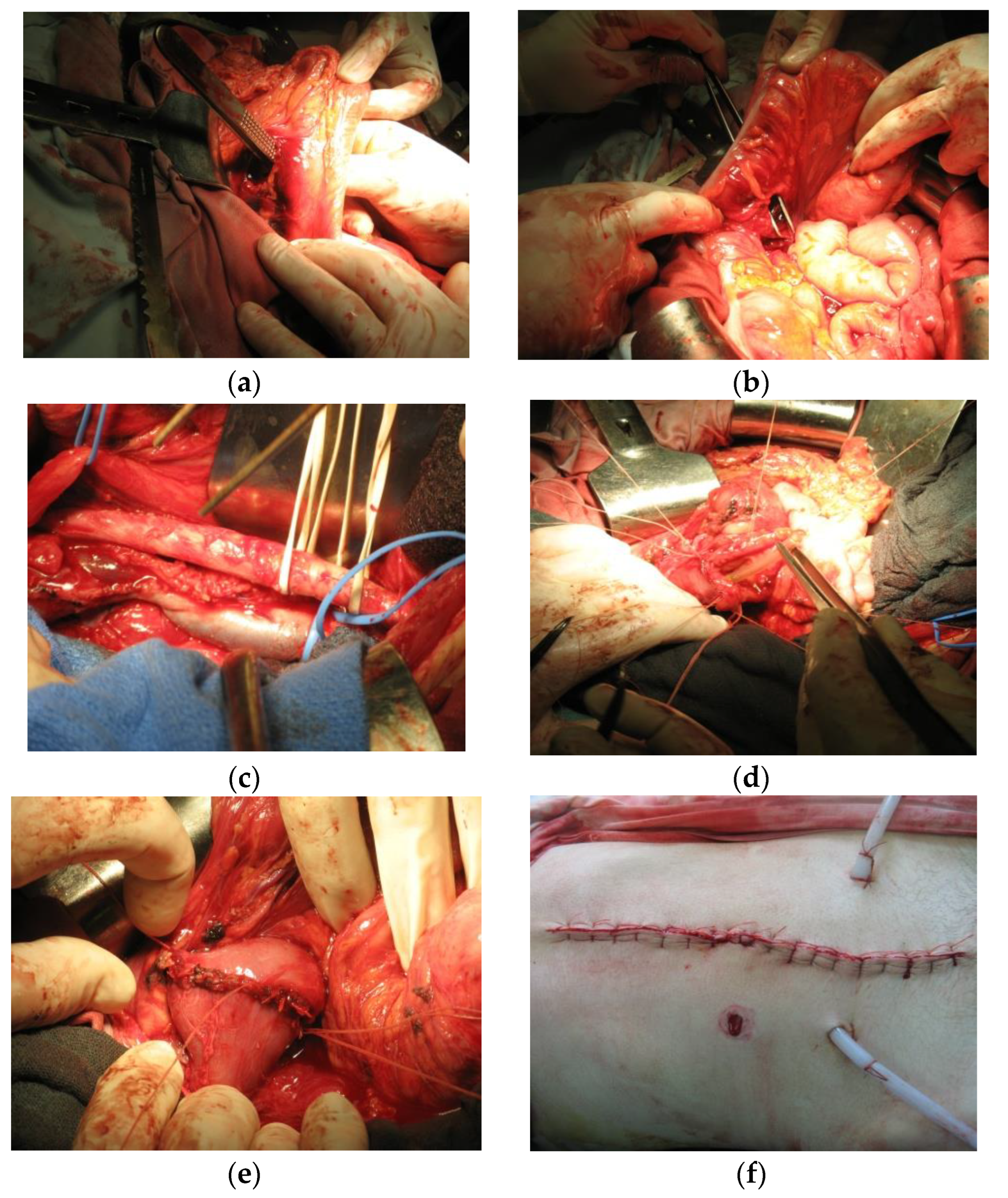
Case Report 1
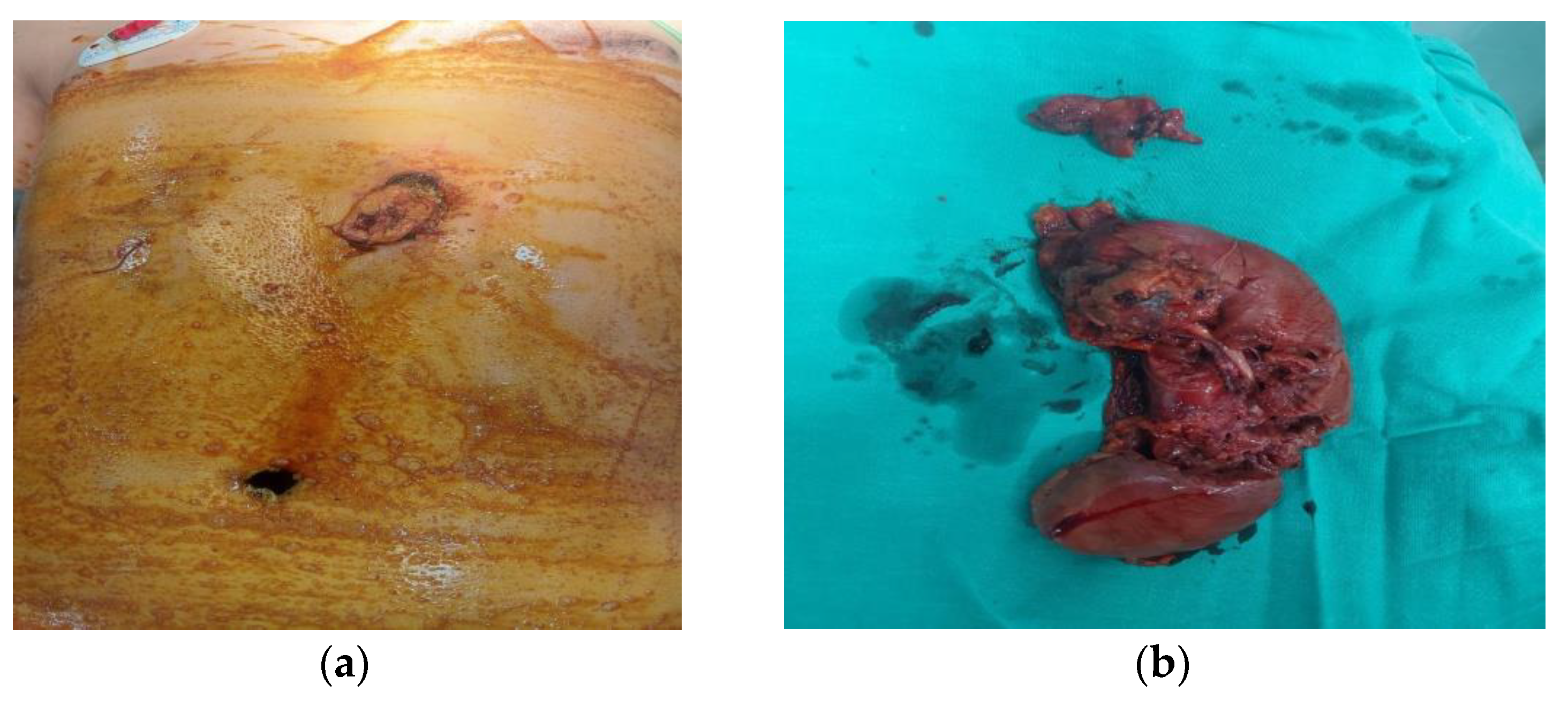
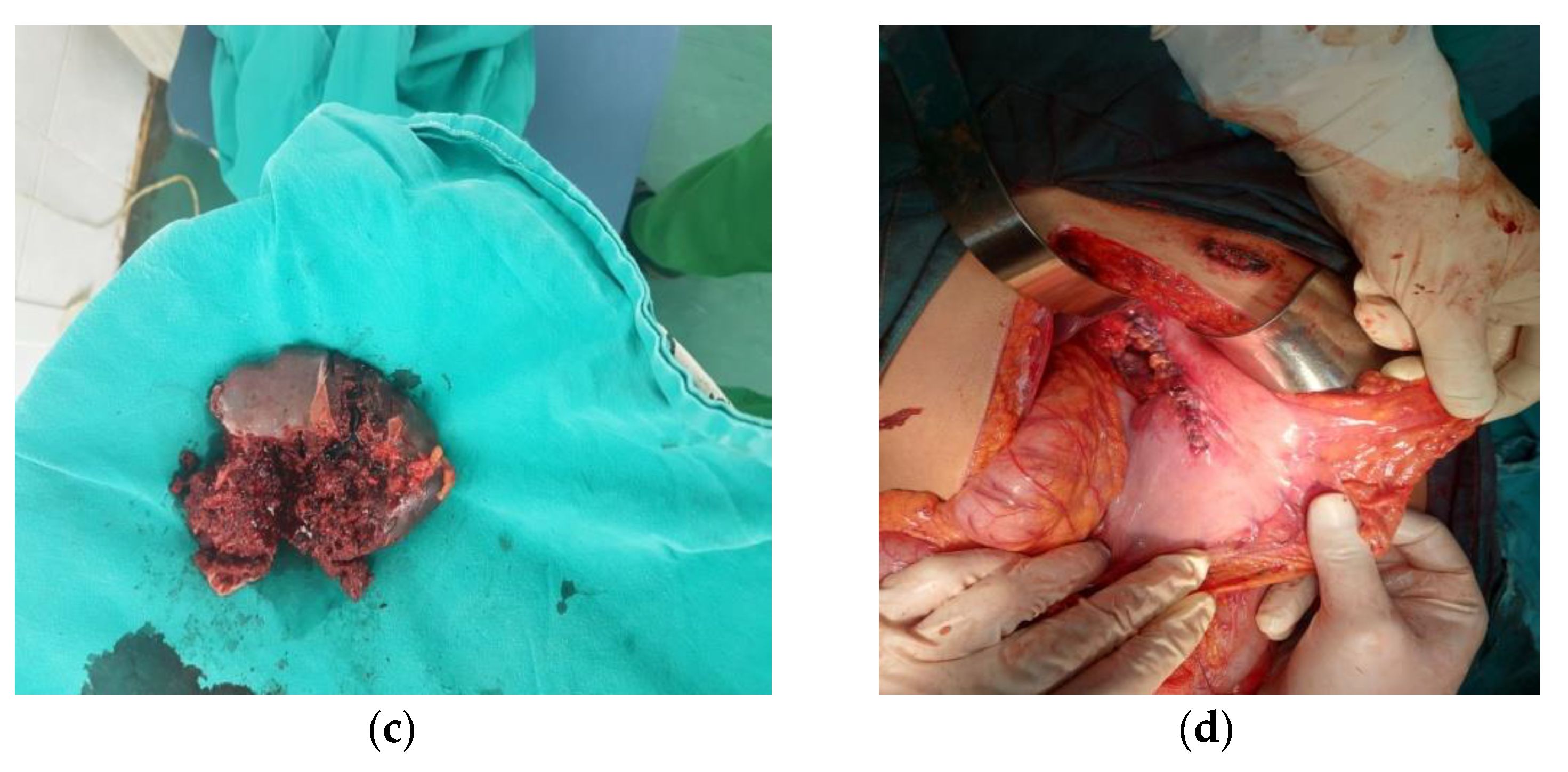
Case Report 2
Discussion
Conclusions
Conflicts of Interest
References
- Beraldo, R.F.; Forlin, E. Firearm-Related Musculoskeletal Injuries in Brazilian Children and Teenagers. Rev Bras Ortop (Sao Paulo). 2019, 54, 685–691. [Google Scholar] [PubMed]
- Drexel, S.; Azarow, K.; Jafri, M. Abdominal Trauma Evaluation for the Pediatric Surgeon. Surg Clin N Am 2017, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Amick, L.F. Penetrating trauma in the pediatric patient. Clin PediatrEmerg Med 2001, 2, 63–70. [Google Scholar] [CrossRef]
- Stefanopoulos, P.; Tsiatis, N.; Herbstein, J. Gunshot wounds. Encyclopedia of Forensic Sciences, Third Edition 2023, 3, 75–98. [Google Scholar]
- Murray, C.J.; Lopez, A.D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997, 349, 1269–1276. [Google Scholar] [CrossRef]
- Shrestha R, Kanchan T, Krishan K. Gunshot Wounds Forensic Pathology. [Updated 2022 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556119/.
- Roberts, B.; James, D.; Haft, J.; Balakrishnan, N.; Prince, J.; Sathya, C. Wounding patterns in pediatric firearm fatalities. Injury. 2023, 54, 154–159. [Google Scholar] [CrossRef]
- DiScala, C.; Sege, R. Outcomes in Children and Young Adults Who Are Hospitalized for Firearms-Related Injuries. Pediatrics 2004, 113, 1306–12. [Google Scholar] [CrossRef]
- Chugtai, B.R.; Uraizy, S.M.A.; Rashid, M.A.; Chaudary, T.H.; Ahmed, B.; Qureshi, G.A.A. Incidence of Homicidal Deaths. The Professional. 2002, 9, 316–319. [Google Scholar]
- Renz, B.M.; Feliciano, D.V. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. 1995, 38, 350–6. [Google Scholar] [CrossRef]
- Gaines, B.A.; Rutkoski, J.D. The role of laparoscopy in pediatric trauma. Semin Pediatr Surg. 2010, 19, 300–3. [Google Scholar] [CrossRef]
- Cotton, B.A.; Nance, M.L. Penetrating trauma in children. Semin Pediatr Surg. 2004, 13, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Lynch, T.; Kilgar, J.; Al Shibli, A. Pediatric Abdominal Trauma. CurrPediatr Rev. 2018, 14, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Deakin, C.D. Early fluid resuscitation in hemorrhagic shock. EurJEmerg Med 1994, 1, 83–8. [Google Scholar]
- Polites, S.F.; Habermann, E.B.; Glasgow, A.E.; et al. Damage control laparotomy for abdominal trauma in children. Pediatr Surg Int 2017, 33, 587–92. [Google Scholar] [CrossRef] [PubMed]
- Tyburski, J.G.; Wilson, R.F.; Dente, C.; Steffes, C.; Carlin, A.M. Factors affecting mortality rates in patients with abdominal vascular injuries. J Trauma. 2001, 50, 1020–6. [Google Scholar] [CrossRef] [PubMed]
- Kincaid, E.H.; Chang, M.C.; Letton, R.W.; Chen, J.G.; Meredith, J.W. Admission base deficit in pediatric trauma: a study using the National Trauma Data Bank. J Trauma. 2001, 51, 332–5. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




