Submitted:
14 July 2023
Posted:
17 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Background and Notation
2.1. Related Works
2.2. Care and Rehabilitation of Patients with Mobility Impairments and Risk of Falls
2.2.1. Falls Risk Factors Can Be Divided into Internal and External Factors
2.2.2 Strategies for Mitigating the Risk of Falling Incidents:
3. Methods
3.1. Data Exploration and System Requirements
3.1.1. Software
- Conduct a thorough examination of the Arduino Integrated Development Environment (IDE) software, which serves as the programming platform for Arduino. Delve into the essential command syntax relevant to variable declaration, sensor integration, and function invocation to enable seamless sensor operation. Additionally, explore the utilization of libraries to leverage pre-existing functions and variables.
- Investigate the intricacies of transmitting messages via Line Notify using the NodeMCU ESP8266. This entails understanding the API-driven HTTP POST method to facilitate the delivery of textual content, stickers, or images to smartphones through the Line messaging application.
3.1.2. Hardware
- Scrutinize the underlying principles governing the control board's functionality and the intricate workings of each individual sensor. This includes comprehending the interconnections between various pins, the permissible voltage ranges for both the board and sensors, and the configuration settings necessary for optimal sensor performance.
- The structure and functioning of the system can be described as follows:
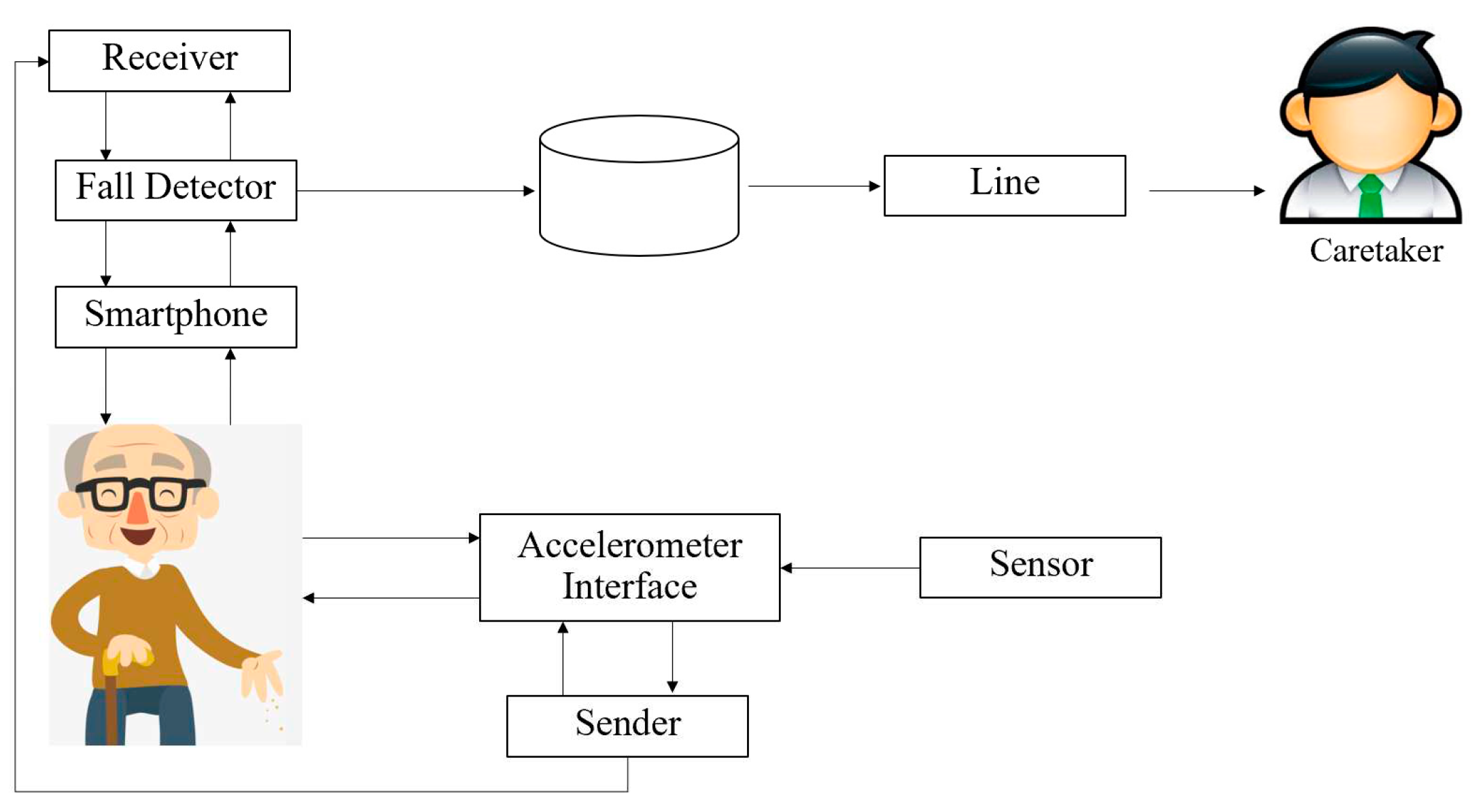
- Initialization of the Decision Tree:
- The program initiates the decision-making process by scrutinizing the occurrence of falls via data derived from the accelerometer sensor.
- 2.
- Branching:
- Crucial conditions or attributes, such as the tri-axial acceleration values (X, Y, and Z) obtained from the accelerometer sensor, are employed by the program to partition the data into distinct clusters based on fall characteristics.
- 3.
- Decision-Making:
- Each tier of the decision tree embodies a decision node predicated on the identified fall characteristics, encompassing forward, backward, leftward, or rightward falls.
- 4.
- Termination of Decision-Making:
- Upon reaching a juncture where further decisions are infeasible, the program proceeds to store the fall data, encompassing temporal, spatial, and contextual details regarding the fall incident.
- Subsequently, the program disseminates a notification message, comprising comprehensive fall characteristics, geographical information, and auditory prompts, to the designated emergency contact via the smartphone interface.
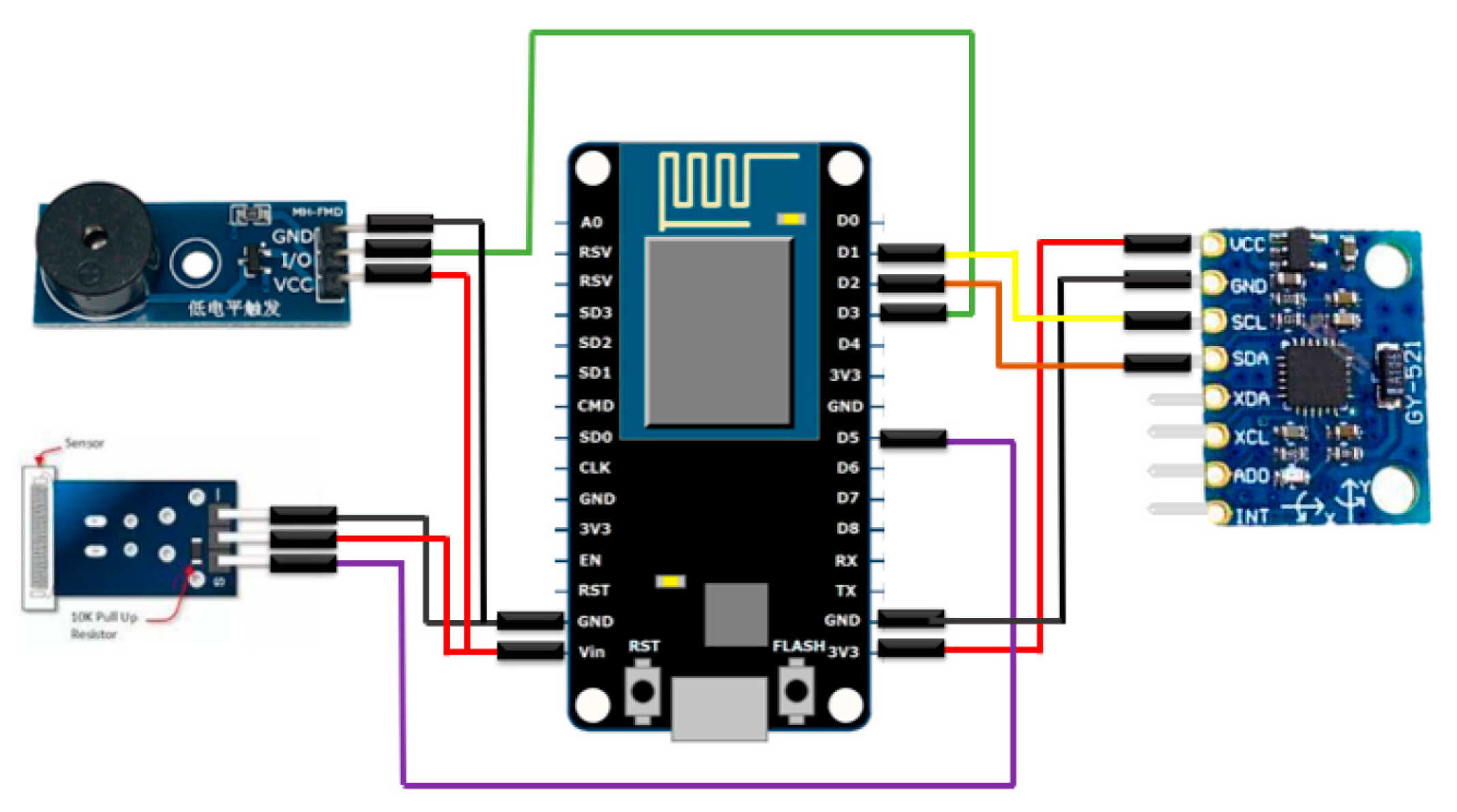
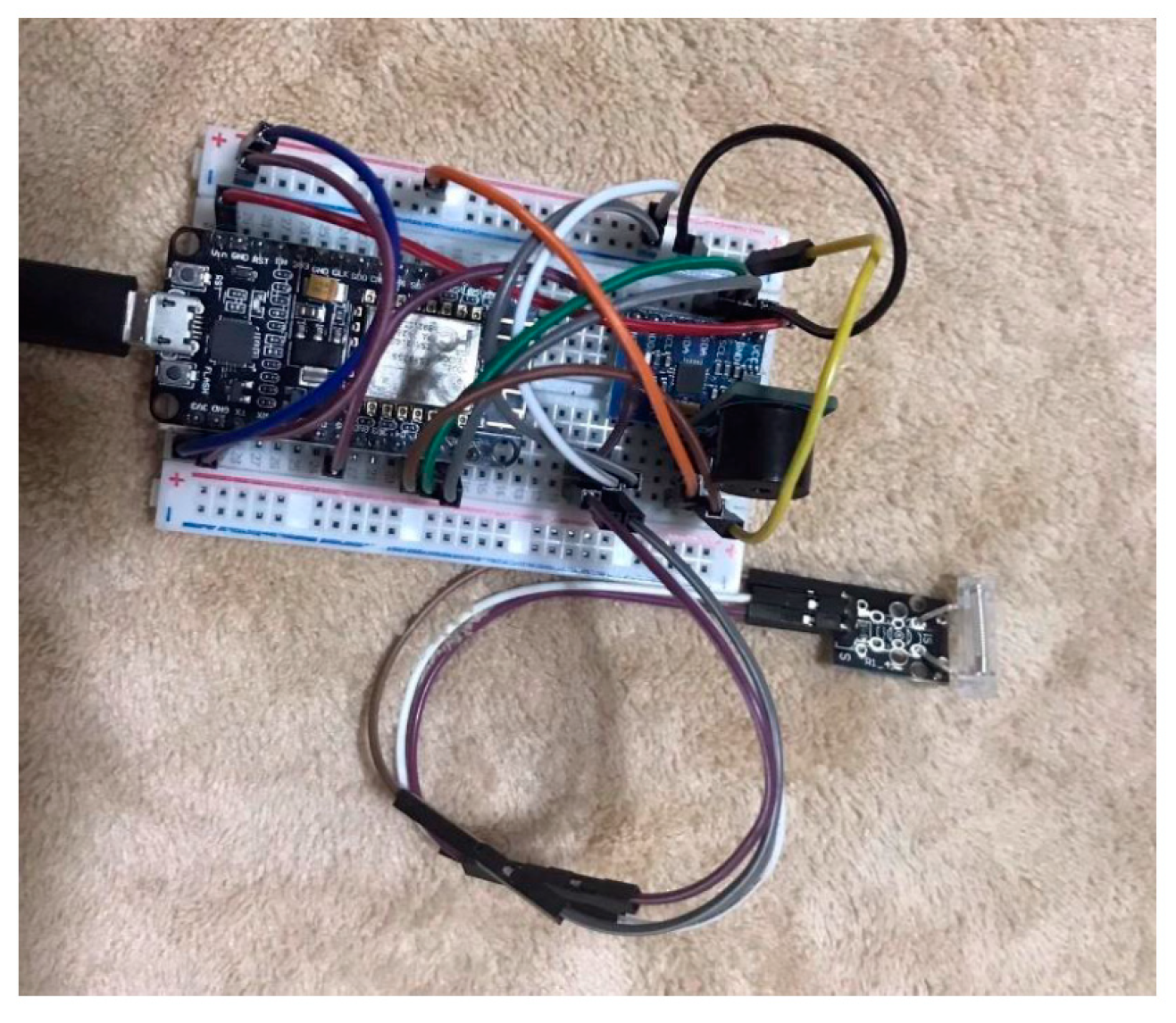
3.2. HARDWARE Development
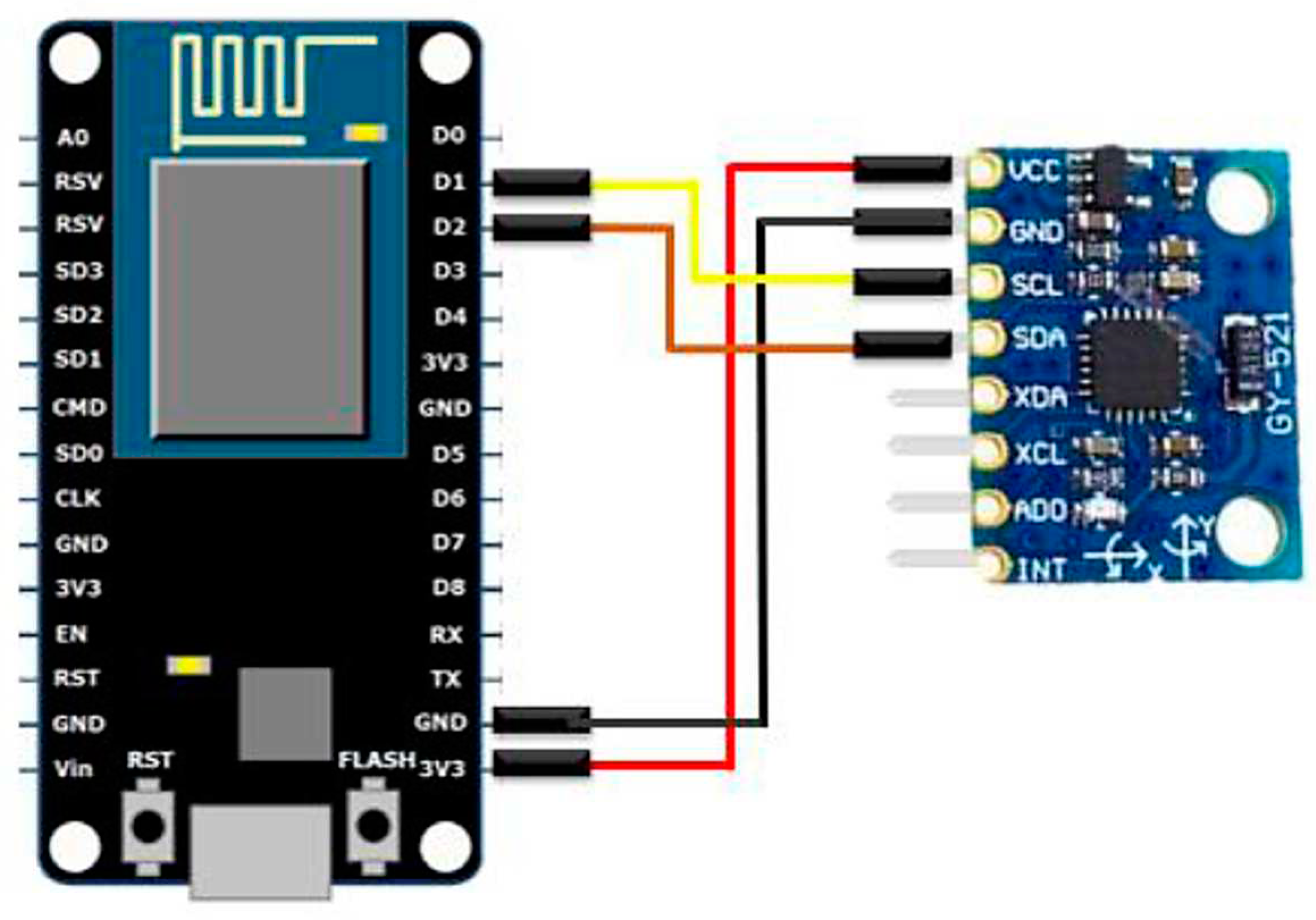
- The ground (GND) pin of the NodeMCU board is meticulously linked to the corresponding ground pin of the GY-521 module, ensuring a robust grounding connection.
- The power supply voltage (VCC) pin of the NodeMCU board is judiciously connected to the designated voltage input pin of the GY-521 module, thereby providing a reliable power source.
- Pin D1 of the NodeMCU board, which serves as the data transmission line for the serial clock (SCL) signal, is methodically linked to the corresponding SCL pin of the GY-521 module, facilitating synchronized data communication.
- Likewise, pin D2 of the NodeMCU board, serving as the data transmission line for the serial data (SDA) signal, is meticulously connected to the respective SDA pin of the GY-521 module, enabling the exchange of data packets.
- Equations for determining the acceleration in the X, Y, and Z axes:
- Acceleration_X = ax
- Acceleration_Y = ay
- Acceleration_Z = az
- 2.
- Equation for calculating the overall acceleration:
- Total_Acceleration = √(ax² + ay² + az²)
- 3.
- Equations for assessing the inclination along the Roll (X) and Pitch (Y) axes:
- Roll = atan2(ay, az)
- Pitch = atan2(-ax, √(ay² + az²))
- 4.
- Equations for evaluating the angular rates of rotation around the Roll (X), Pitch (Y), and Yaw (Z) axes:
- Gyro_Rate_X = gx
- Gyro_Rate_Y = gy
- Gyro_Rate_Z = gz
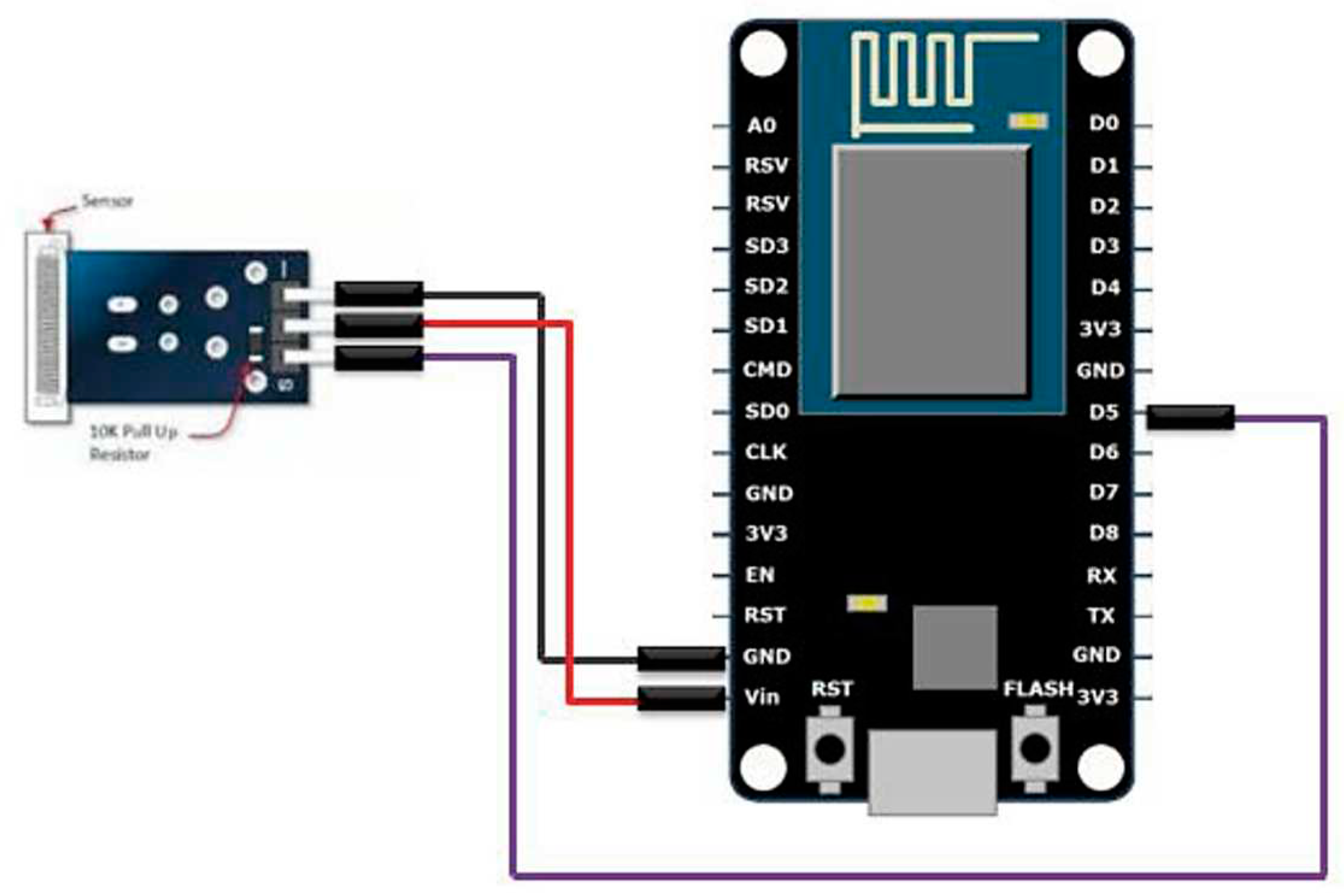
- Connect the GND (Ground) pin of the NodeMCU to the GND pin of the KY-031 sensor. This establishes a common ground reference between the NodeMCU and the sensor.
- Connect the VCC (Power) pin of the NodeMCU to the VCC pin of the KY-031 sensor. This supplies power to the sensor, ensuring proper functionality.
- Connect pin D5 of the NodeMCU to the OUTPUT pin of the KY-031 sensor. This allows the NodeMCU to receive the output signal from the vibration sensor.
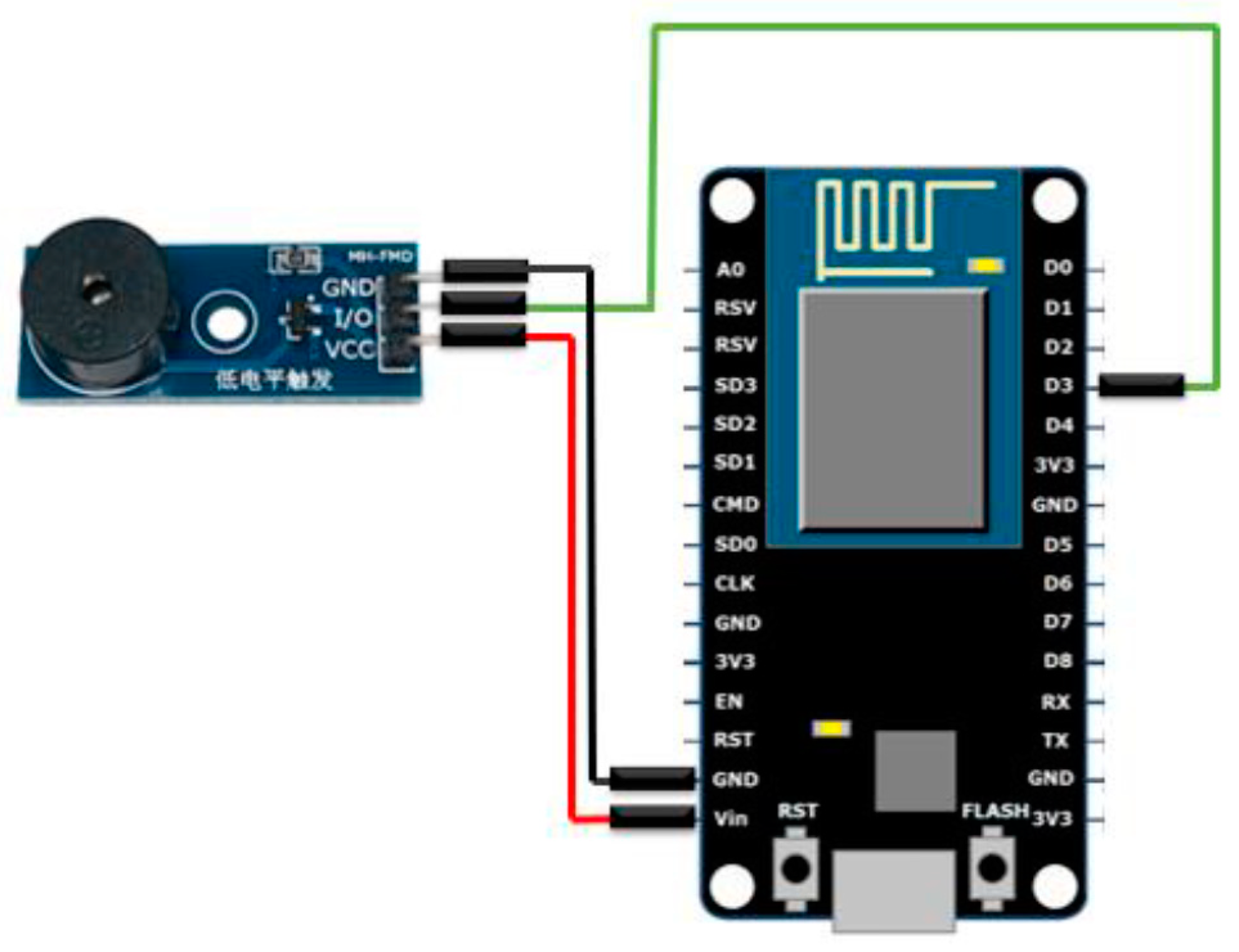
- Connect the GND (Ground) pin of the NodeMCU to the GND pin of the buzzer sensor.
- Connect the VCC (Voltage) pin of the NodeMCU to the VCC pin of the buzzer sensor.
- Connect pin D3 of the NodeMCU to the OUTPUT pin of the buzzer sensor.
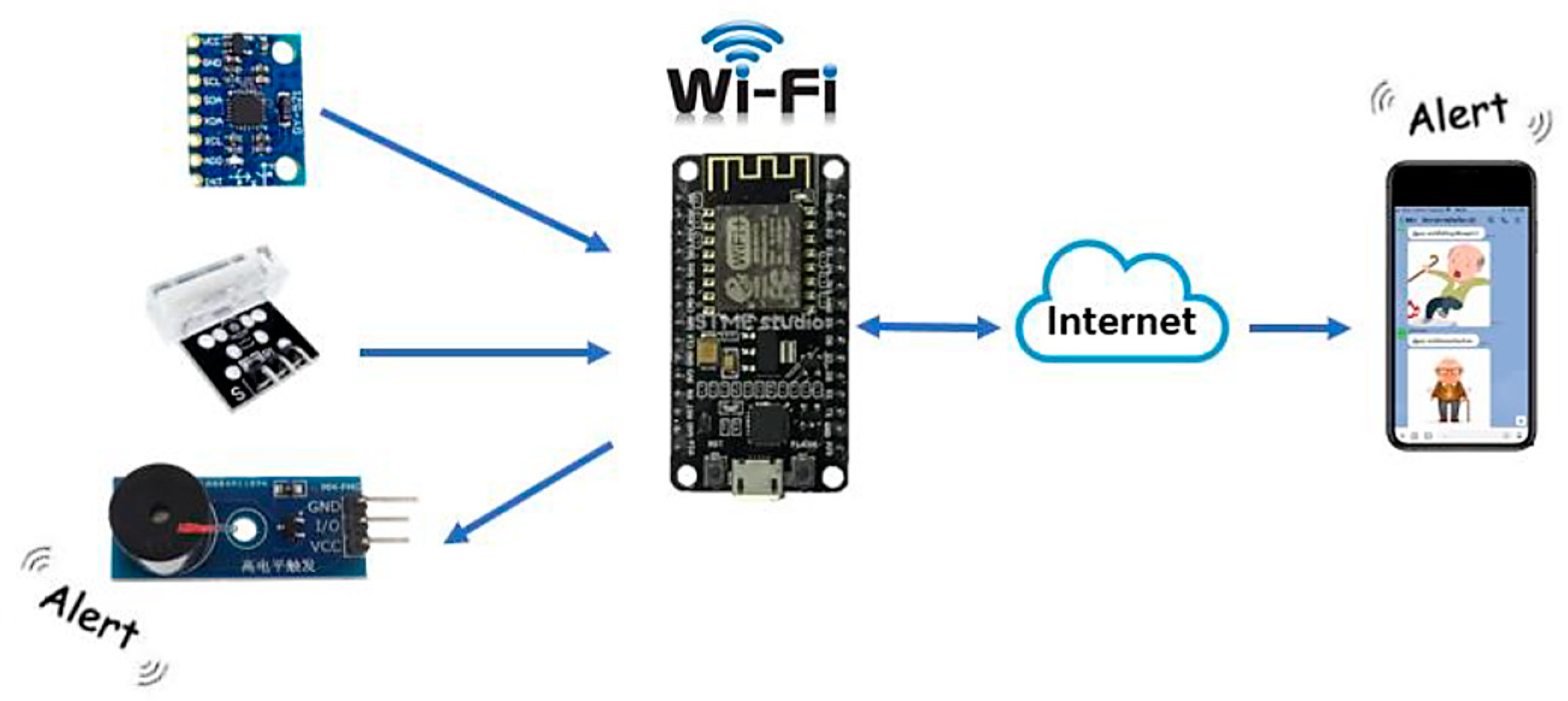
- The integration of a NodeMCU ESP8266 module enables seamless connectivity to a Wi-Fi network, thereby facilitating internet access for the device.
- The system incorporates Line Notify, a robust messaging service, which is configured using a unique LINE TOKEN to establish a reliable communication channel.
- Data acquisition is facilitated through the utilization of two sensors: the GY-521 MPU6050 sensor, responsible for capturing the inclination angle of the object under observation, and the KY-031 sensor, employed to detect and monitor vibrational patterns.
- In the event of an abrupt impact occurrence, the system promptly captures relevant data from the GY-521 MPU6050 sensor to assess the situational parameters.
- In the absence of any such impact, the system periodically retrieves data from the GY-521 MPU6050 sensor at regular intervals of 2 seconds to maintain a comprehensive monitoring approach.
- A perceptible auditory alert is triggered by the system upon the detection of an object tilt, signifying a potential fall or hazardous event.
- Furthermore, in instances where an object tilt is detected, the system consistently transmits notification messages via Line Notify at 10-second intervals, conveying critical information denoted by the phrase "The patient has encountered an accident."
- Subsequent to the object regaining an upright position, indicative of the individual's ability to self-recover, the system ceases the auditory alert mechanism while simultaneously dispatching a notification message via Line Notify, elaborating on the individual's restored autonomy through the phrase "The patient is capable of self-assistance."
4. Results and Discussion
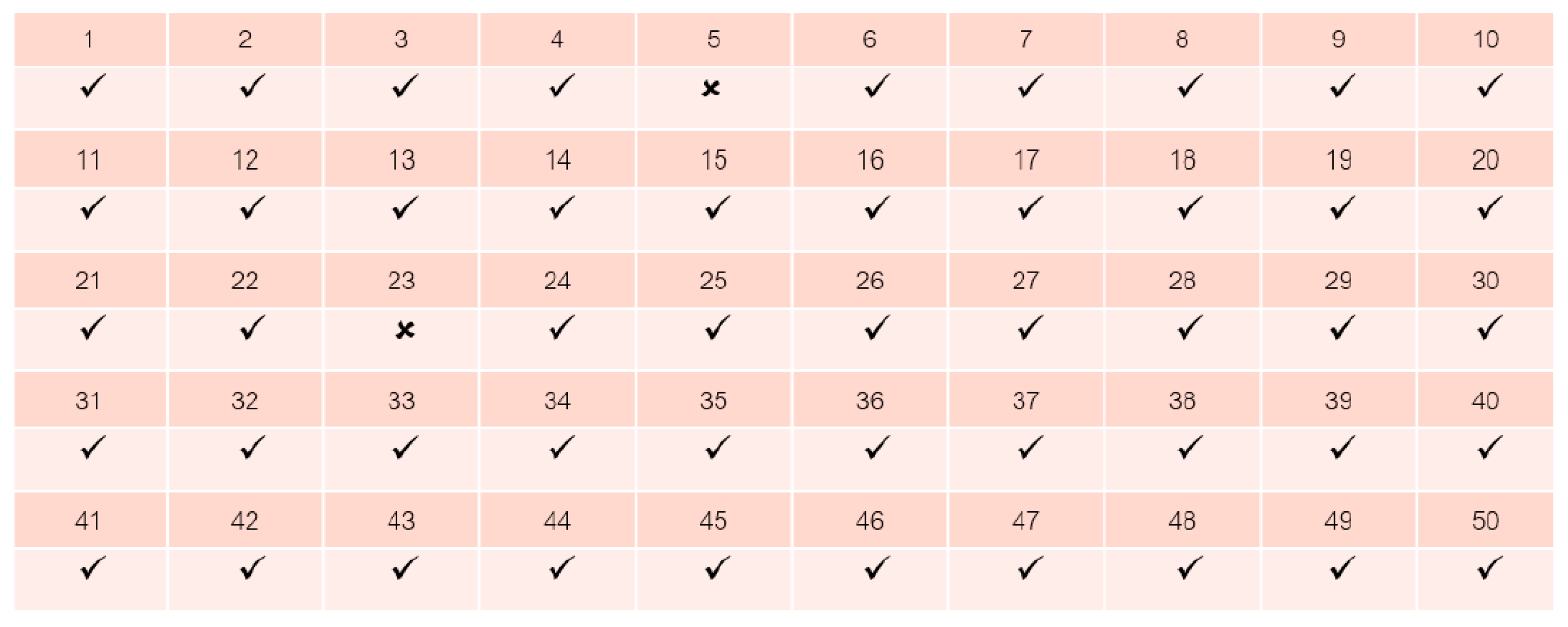
4.2. Evaluation of Intelligent Ankle Device Performance

4.2.2. Alert System Functionality


5. Conclusions
References
- Friedl, K.E.; Looney, D.P. With life there is motion. Activity biomarkers signal important health and performance outcomes. J. Sci. Med. Sport 2023, in press.
- Fritz, S.; Lusardi, M. White paper: “Walking speed: The sixth vital sign”. J. Geriatr. Phys. Ther. 2009, 32, 2–5. [Google Scholar] [CrossRef]
- Atrsaei, A.; Corrà, M.F.; Dadashi, F.; Vila-Chã, N.; Maia, L.; Mariani, B.; Maetzler, W.; Aminian, K. Gait speed in clinical and daily living assessments in Parkinson’s disease patients: Performance versus capacity. NPJ Park. Dis. 2021, 7, 24. [Google Scholar] [CrossRef]
- Merchant, R.A.; Goh, J.; Chan, Y.; Lim, J.; Vellas, B. Slow gait, subjective cognitive decline and motoric cognitive RISK syndrome: Prevalence and associated factors in community dwelling older adults. J. Nutr. Health Aging 2021, 25, 48–56. [Google Scholar] [CrossRef]
- Ozsoy, I.; Kodak, M.I.; Zerman, N.; Karartı, C.; Ozsoy, G.; Erturk, A. Gait speed predictors and gait-speed cut-off score to discriminate asthma control status and physical activity in patients with asthma. Adv. Respir. Med. 2022, 90, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; Pieruccini-Faria, F.; Bartha, R.; Black, S.E.; Finger, E.; Freedman, M.; Greenberg, B.; Grimes, D.A.; Hegele, R.A.; Hudson, C. Motor phenotype in neurodegenerative disorders: Gait and balance platform study design protocol for the Ontario neurodegenerative research initiative (ONDRI). J. Alzheimer’s Dis. 2017, 59, 707–721. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, A.; Katz, M.J.; Lipton, M.L.; Lipton, R.B.; Verghese, J. The association of brain structure with gait velocity in older adults: A quantitative volumetric analysis of brain MRI. Neuroradiology 2015, 57, 851–861. [Google Scholar] [CrossRef]
- Braak, H.; Braak, E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol. Aging 1995, 16, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Jia Luen Chua, Yoong Choon Chang, and Wee Keong Lim, “Intelligent Visual Based Fall Detection Technique for Home Surveillance”, Computer, Consumer and Control (IS3C) 2012, pp. 183 – 187.
- Miao Yu, Adel Rhuma, Syed Mohsen Naqvi, Liang Wang and Jonathon Chambers, “Posture Recognition Based Fall Detection System For Monitoring An Elderly Person In A Smart Home Environment”, Information Technology in Biomedicine, IEEE Transactions on Issue: 99, 2012, pp. 1– 11.
- Damien Brulin, Yannick Benezeth, and Estelle Courtial, “Posture Recognition Based on Fuzzy Logic for Home Monitoring of the Elderly”, Information Technology in Biomedicine, IEEE Transactions Volume: 16, Issue: 5, 2012, pp. 974 – 982.
- Caroline Rougier, Edouard Auvinet, Jacqueline Rousseau, Max Mignotte and Jean Meunier, “Fall Detection from Depth Map Video Sequences”, 9th International Conference on Smart Homes and Health Telematics (ICOST), 2011, pp. 121 – 128.
- Shaou-Gang Miaou, Pei-Hsu Sung, and Chia-Yuan Huang, “A Customized Human Fall Detection System Using Omni-Camera Images and Personal Information”,IEEE International Conference on Distributed Diagnosis and Home Healthcare (D2H2) Conference, 2006, pp.103-107.
- Peng Shen Ong, et al, “An FPGA-Based Hardware Implementation of Visual based Fall Detection,” IEEE International Conference on Region 10 Symposium, 2014, pp. 397-402.
- Behçet Uğur Töreyin, Yiğithan Dedeoğlu and A. Enis Çetin, “HMM based falling person detection using both audio and video”, IEEE International Workshop on Human–Computer Interaction,Vol. 3766, 2005, pp. 211–220.
- Alex Edgcomb and Frank Vahid, “Automated Fall Detection on PrivacyEnhanced Video”, IEEE International Conference on Engineering in Medicine and Biology Society (EMBC), 2012, pp. 252-255.
- Ji Tao, et al, “Fall Incidents Detection for Intelligent Video Surveillance,” IEEE International Conference on Information, Communications and Signal Processing, 2005, pp. 1590 - 1594.
- Georgios Mastorakis and Dimitrios Makris, “Fall detection system using Kinect’s infrared sensor”, Journal of Real-Time Image Processing, Vol. 9, Issue 4, 2012, pp. 635-646.
- Vitoantonio Bevilacqua, et al, “Fall Detection in indoor environment with Kinect sensor,” IEEE International Symposium on Innovations in Intelligent Systems and Applications (INISTA), 2014, pp. 319-324.
- Y.S. Delahoz and M.A. Labrador, “Survey on fall detection and fall prevention using wearable and external sensors,” Sensors, vol. 14, no. 10, pp. 19806–19842, 2014.
- S. Eamsamai, R. Mhuansit and C. Thongmag, “An elderly care model among caregiving volunteers at Phukrang municipality, Amphur Praputthabat, Saraburi province,” (In Thai). Nursing Journal of the Ministry of Public Health, vol. 22, no. 3, pp. 77-87, 2012.
- T. Yu, A. Stamm and R. Hartanto, “Design and implementation of a Bluetooth low energy-based local area network for fall detection,” in Proc. 12th Conference of the International Sports Engineering Association, Queensland, Australia, March 26-29, 2018.
- Y. Lee, H. Yeh, K. Kim and O. Choi, “A real-time fall detection system based on the acceleration sensor of smartphone,” International Journal of Engineering Business Management, vol. 10, pp. 1–8, 2018.
- C. Ko, F. Leu and I. Lin, “A wandering path tracking and fall detection system for people with dementia,” in Proc. 9th International Conference on Broadband and Wireless Computing, Communication and Applications, Guangdong, China, November 8-10, 2014.
- Y. Xiang, Y. Tang, B. Ma, H. Yan, J. Jiang and X. Tia, “Remote safety monitoring for elderly persons based on omni-vision analysis,” PLoS ONE, vol. 10, no. 5, e0124068, 2015.
- L.H. Juang and M.N. Wu, “Fall down detection under smart home system,” Journal of Medical Systems, vol. 39, no. 10, pp. 1–12, 2015.
- W. Zhuang, X. Sun, Y Zhi, Y. Han and H. Mao. “A novel wearable smart button system for fall detection,” in Proc. the 1st International Conference on Materials Science, Energy Technology, Power Engineering (MEP 2017), Hangzhou, China, April 15-16, 2017, pp. 020075-1 - 020075-6.
- V. Muenruekam, V. Sudkratok, S. Surarochprajak and T. Thongkrau, “Automatic accident alert system using multi-layer perceptron,” (In Thai). TNI Journal of Engineering and Technology, vol. 5, no. 2, pp. 49 – 53, 2017.
- Caya, M. V. C., Magwili, G. V., Agulto, D. L., Laranang, R. J., & Palomo, L. K. G. (2019). Supervised machine learning-based fall detection. 2018 IEEE 10th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment and Management, HNICEM 2018, 1–6. [CrossRef]
- He, J., Zhou, M., Wang, X., & Han, Y. (2016). A wearable method for autonomous fall detection based on Kalman filter and k-NN algorithm. Proceedings - 2016 IEEE Biomedical Circuits and Systems Conference, BioCAS2016, 420–423. [CrossRef]
- Hsu, Y. W., Chen, K. H., Yang, J. J., & Jaw, F. S. (2017). Smartphone-based fall detection algorithm using feature extraction. Proceedings - 2016 9th International Congress on Image and Signal Processing, BioMedical Engineering and Informatics, CISP-BMEI 2016, 1535–1540. [CrossRef]
- Ning, Y., Hu, S., Nie, X., Liang, S., Li, H., & Zhao, G. (2018). Real-time Action Recognition and Fall Detection Based on Smartphone. Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, 2018, 4418–4422. [CrossRef]
- ShahzadShahzad, A., & Kim, K. (2019). FallDroid: An Automated Smart-Phone-Based Fall Detection System Using Multiple Kernel Learning. IEEE Transactions on Industrial Informatics, 15(1), 35–44. [CrossRef]
- Sucerquia, A., López, J. D., & Vargas-Bonilla, J. F. (2017). SisFall: A fall and movement dataset. Sensors (Switzerland), 17(1). [CrossRef]
- Tsinganos, P. & Skodras, A. (2018). On the comparison of wearable sensor data fusion to a single sensor machine learning technique in fall detection. Sensors, 18(2), 59-67. [CrossRef]
- Ricardo Goncalves1,2,Joao Reis1, Emanuel Santana1, Nuno B. Carvalho1,2,Pedro Pinho1,3 and Luca Roselli4, “Smart Floor: Indoor navigation based on RFID”, In Proc. IEEE JOURNAL 2013,103- 106.
- Lih-Jen Kau, et al., “A Smart Phone-Based Pocket Fall Accident Detection, Positioning, and Rescue System”, In Proc. IEEE JOURNAL OF BIOMEDICAL AND HEALTH INFORMATICS, JANUARY 2015.
- Ludovic Minvielle, et al., “Fall Detection Using Smart Floor Sensor and Supervised Learning*”, In Proc. International Conference of the IEEE 2017, 3445-3448.
- Ben Heller, Terry Senior and Jon Wheat. “Smart Floor with Integrated Triboelectric Nanogenerator As Energy Harvester and Motion Sensor”, In Proc. American Chemical Society United Kingdom, 2017, 26126-26133. [CrossRef]
- Amman, Jordan Leicester, “Indoor Human Detection and Tracking Using Advanced Smart floor”, In Proc. International Conference on Information and Communication Systems (ICICS),2017,34- 39.
- Angel Ramos และ Antonio Lazaro, “Time-domain UWB RFID tags for smart floor applications” In Proc. IEEE journal of RFID Technology and applications Conference, 2014,165-169.
- Apkan, V., Agbogun J., Omotehinwa, O., & Omotehinwa, O. T. (2019). Development of an Automatic Body Mass Index Machines. P. 42-51. In: Proceedings of the 1st Ibadan Conference on Biomedical Engineering ICBME 1, 5-8 February, Ibadan, Nigeria.
- Godfrey, A. Wearables for independent living in older adults: Gait and falls. Maturitas 2017, 100, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Strozzi, N.; Parisi, F.; Ferrari, G. Impact of on-body IMU placement on inertial navigation. IET Wirel. Sens. Syst. 2017, 8, 3–9. [Google Scholar] [CrossRef]
- Garai, Á.; Péntek, I.; Adamkó, A. Revolutionizing healthcare with IoT and cognitive, cloud-based telemedicine. Acta Polytech. Hung 2019, 16, 163–181. [Google Scholar]
- Abdellatif, M.M.; Mohamed, W. Telemedicine: An IoT Based Remote Healthcare System. Int. J. Online Biomed. Eng. 2020, 16.
- Nguyen, H.H.; Mirza, F.; Naeem, M.A.; Nguyen, M. A review on IoT healthcare monitoring applications and a vision for transforming sensor data into real-time clinical feedback. In Proceedings of the 2017 IEEE 21st International Conference on Computer Supported Cooperative Work in Design (CSCWD), Wellington, New Zealand, 26–28 April 2017; pp. 257–262. [Google Scholar]
- Barata, J.J.R.; Munoz, R.; Silva, R.D.D.C.; Rodrigues, J.J.; De Albuquerque, V.H.C. Internet of Things based on electronic and mobile health systems for blood glucose continuous monitoring and management. IEEE Access 2019, 7, 175116–175125. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




