Submitted:
05 July 2023
Posted:
06 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2-1. BAEPs test in Routine
2-2. BAEPs test in INM
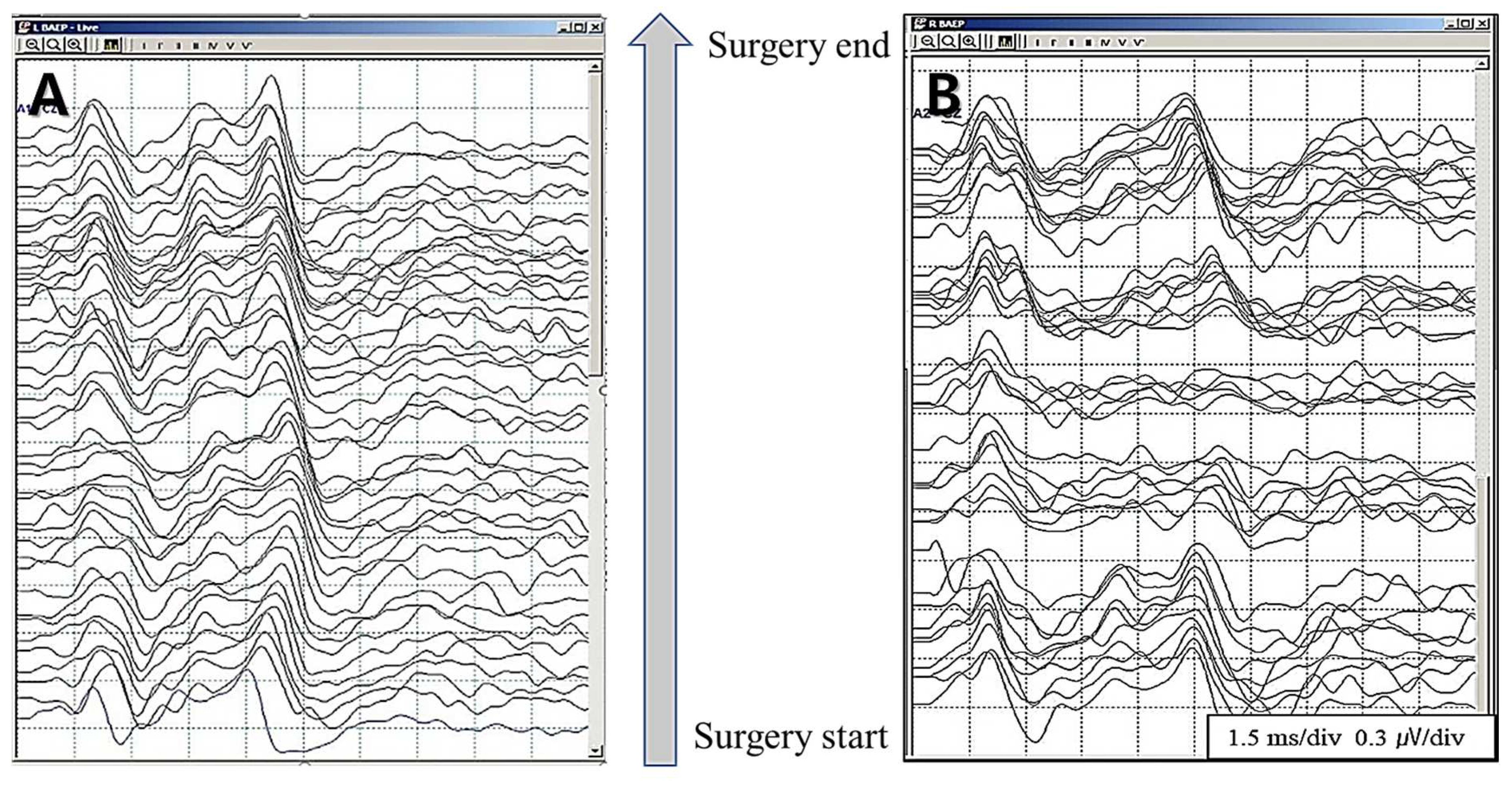
2-2-1. Real-time BAEPs
2-2-1-1. Stimulation rate and averaging time
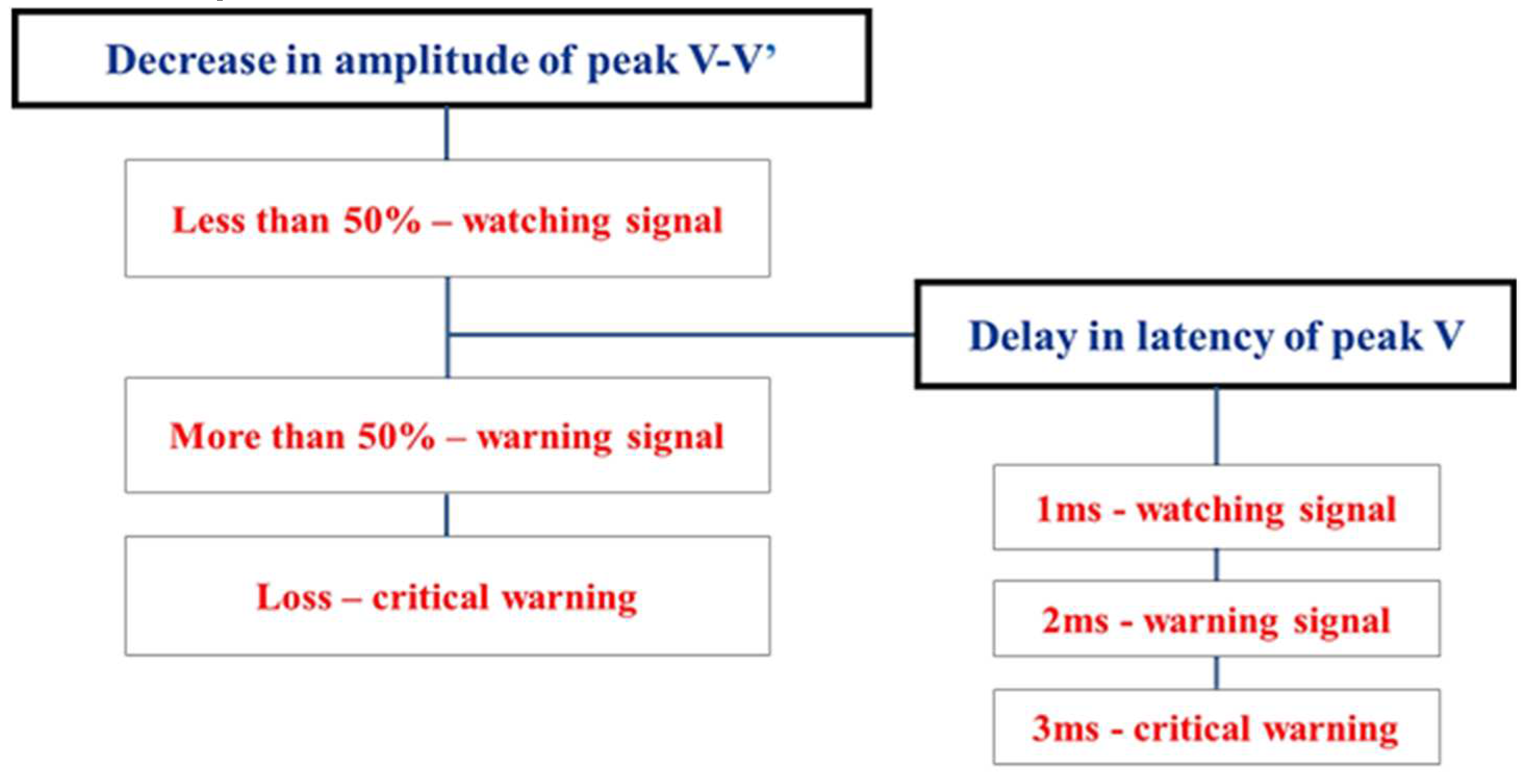
2-2-2. Warning criteria
2-2-2-1. Prewarning sign
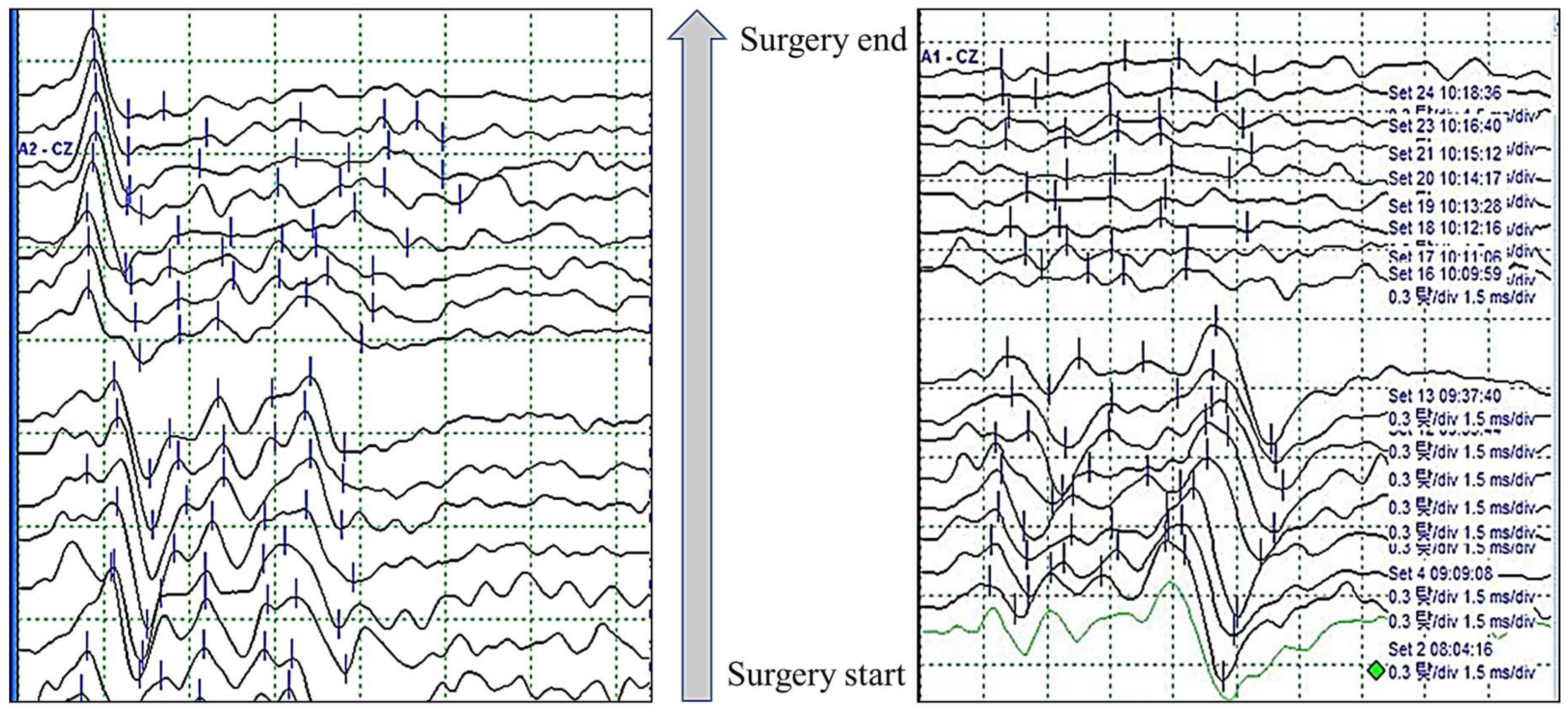
2-2-2-2. Significance of wave I
3. Discussion
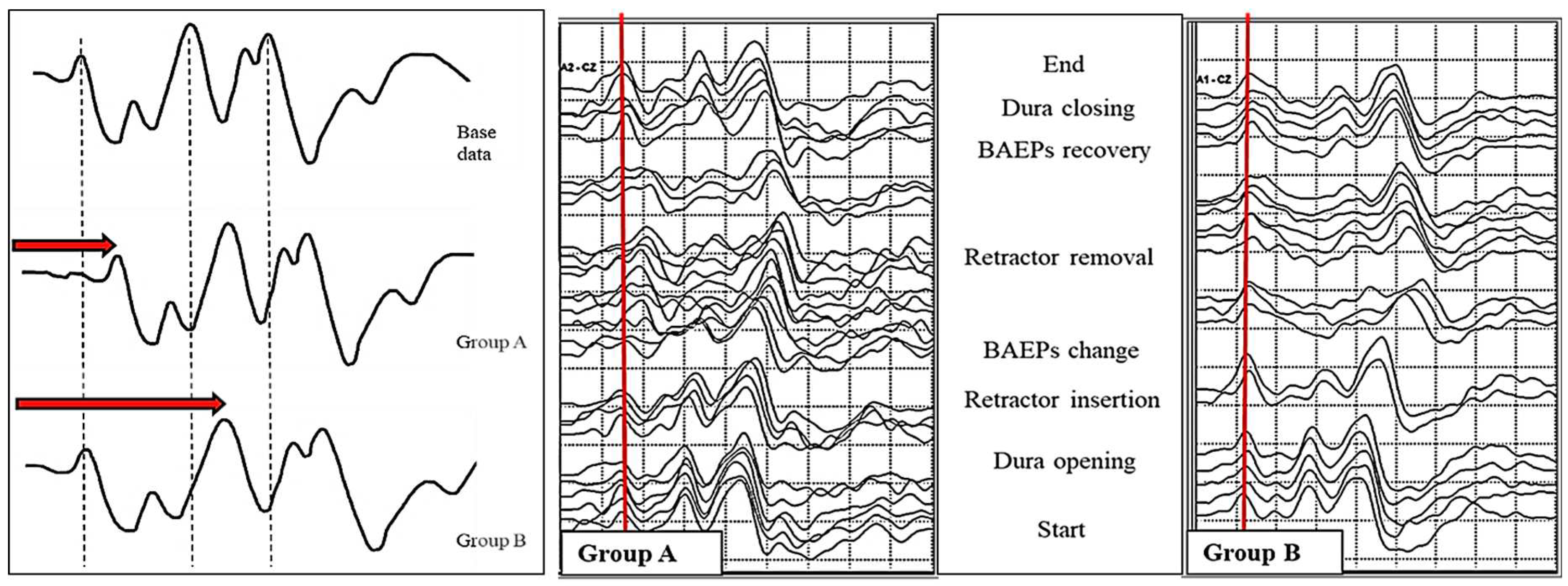
3-1. Patterns of BAEPs wave change during Microvascular Decompression for Hemifacial Spasm
3-1-1. Latency and amplitude of BAEPs wave V
3-1-2. Time-dependent classification of BAEPs wave changes
4. Conclusion
Funding
Author Contributions
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Jewett, D.L.; Williston, J.S. Auditory-evoked far fields averaged from the scalp of humans. Brain 1971, 94, 681–696. [Google Scholar] [CrossRef] [PubMed]
- Doyle, D.J.; Hyde, M.L. Analogue and Digital Filtering of Auditory Brainstem Responses. Scand. Audiol. 1981, 10, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Møller, A.R.; Jannetta, P.J. Comparison Between Intracranially Recorded Potentials from the Human Auditory Nerve and Scalp Recorded Auditory Brainstem Responses (ABR). Scand. Audiol. 1982, 11, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Moller AR, Jannetta PJ. Neural generators of auditory evoked potentials. In: Jacobson JT, editor. The auditory brainstem response. SanDiego: College-Hill Press, 1985, 13-31.
- Polo, G.; Fischer, C.; Sindou, M.P.; Marneffe, V. Brainstem Auditory Evoked Potential Monitoring during Microvascular Decompression for Hemifacial Spasm: Intraoperative Brainstem Auditory Evoked Potential Changes and Warning Values to Prevent Hearing Loss—Prospective Study in a Consecutive Series of 84 Patients. Neurosurgery 2004, 54, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Sindou, M.P. Microvascular decompression for primary hemifacial spasm. Importance of intraoperative neurophysiological monitoring. Acta Neurochir. 2005, 147, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Hatayama, T.; Møller, A.R. Intraoperatve recordings in MVD operations. Acta Neurochir (Wien) 1998, 140, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Legatt, A.D. Mechanisms of intra operative brainstem auditory evoked potential changes. J Clin Neurophysiol. 2002, 19, 396–408. [Google Scholar] [CrossRef]
- Martin, W.H.; Stecker, M.M. ASNM position statement: intraoperative monitoring of auditory evoked potentials. J Clin Monit Comput. 2008, 22, 75–85. [Google Scholar] [CrossRef] [PubMed]
- American Clinical Neurophysiology Society. Guideline 9C: Guidelines on short-latency auditory evoked potentials. J Clin Neurophysiol. 2006, 23, 157–167. [Google Scholar] [CrossRef] [PubMed]
- James, M.L.; Husain, A.M. Brainstem auditory evoked potential monitoring: When is change in wave V significant? Neurology 2005, 65, 1551–1555. [Google Scholar] [CrossRef] [PubMed]
- Thirumala, P.D.; Carnovale, G.; Habeych, M.E.; Crammond, D.J.; Balzer, J.R. Diagnostic accuracy of brainstem auditory evoked potentials during microvascular decompression. Neurology 2014, 83, 1747–1752. [Google Scholar] [CrossRef] [PubMed]
- Polo, G.; Fischer, C.; Sindou, M.P.; Marneffe, V. Brain auditory evoked potentialmonitoring during microvascular decompression for hemifacial spasm: intra-operative brainstem auditory evoked potential changes and warning values to prevent hearing loss—prospective study in a consecutive series of 84 patients. Neurosurgery 2004, 54, 97–106. [Google Scholar] [PubMed]
- Sprenghers, L.; Lemmens, R.; van Loon, J. Usefulness of intraoperative monitoring in microvascular decompression for hemifacial spasm: a systematic review and meta-analysis. Br. J. Neurosurg. 2022, 36, 346–357. [Google Scholar] [CrossRef] [PubMed]
- American Clinical Neurophysiology Society. Guideline 9C: Guidelines on short-latency auditory evoked potentials. J Clin Neurophysiol. 2006. [Google Scholar]
- Chiappa, K.; Gladstone, K.J.; Young, R.R. Brainstem auditory evoked responses. Studies of waveform variation in 50 normal human subjects. Arch Neurol 1979, 36, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Joo, B.-E.; Park, S.-K.; Cho, K.-R.; Kong, D.-S.; Seo, D.-W.; Park, K. Real-time intraoperative monitoring of brainstem auditory evoked potentials during microvascular decompression for hemifacial spasm. J. Neurosurg. 2016, 125, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-K.; Joo, B.-E.; Lee, S.; Lee, J.-A.; Hwang, J.-H.; Kong, D.-S.; Seo, D.-W.; Park, K.; Lee, H.-T. The critical warning sign of real-time brainstem auditory evoked potentials during microvascular decompression for hemifacial spasm. Clin. Neurophysiol. 2018, 129, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-K.; Joo, B.-E.; Park, K. Intraoperative Neurophysiological Monitoring in Hemifacial Spasm. A Practical Guide. 2021. ISBN 978-981-16-1326-5 ISBN 978-981-16-1327-2 (eBook). [CrossRef]
- Park, S.-K.; Joo, B.-E.; Kwon, J.; Kim, M.; Lee, S.; Lee, J.-A.; Park, K. A prewarning sign for hearing loss by brainstem auditory evoked potentials during microvascular decompression surgery for hemifacial spasm. Clin. Neurophysiol. 2020, 132, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Thirumala, P.D.; Krishnaiah, B.; Crammond, D.J.; Habeych, M.E.; Balzer, J.R. Analysis of Wave III of Brain stem Auditory Evoked Potential Waveforms during Microvascular Decompression of Cranial Nerve VII for Hemifacial Spasm. J. Clin. Neurophysiol. 2014, 31, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Joo, B.-E.; Park, S.-K.; Lee, M.H.; Lee, S.; Lee, J.-A.; Park, K. Significance of wave I loss of brainstem auditory evoked potentials during microvascular decompression surgery for hemifacial spasm. Clin. Neurophysiol. 2020, 131, 809–815. [Google Scholar] [CrossRef] [PubMed]
| Group | Latency | Amplitude | N = 463 | Post OP HL |
|---|---|---|---|---|
| 1 | < 1ms | < 50% | 346 | 0 |
| 2 | > 2ms | < 50% | 38 | 0 |
| 3 | < 1ms | > 50% | 15 | 0 |
| 4 | > 2ms | > 50% | 36 | 1 |
| 5 | Permanent loss | 5 | 5 | |
| 6 | Transient loss | 23 | 0 | |
| The final change of wave V | Group A | Group B | p-value |
|---|---|---|---|
| Latency prolongation (<1 ms) with amplitude decrement (<50%) |
72 (88.9%) | 105 (65.6%) | <0.001 |
| Only latency prolongation (1 ms) | 8 (9.9%) | 45 (28.1%) | 0.001 |
| Only amplitude decrement (50%) | 0 | 0 | ns |
| Latency prolongation (1 ms) with amplitude decrement (50%) |
0 | 0 | ns |
| Wave V loss | 1 (1.2%) | 10 (6.3%) | 0.078 |
| Total | 81 | 160 |
| w/i persistence of wave I |
w/o persistence of wave I |
P value | |
|---|---|---|---|
| Patients, n | 24 | 12 | |
| Hearing loss, n (%) | 2 (8.33%) | 6 (50.00%) | 0.009 |
|
Subtype of Hearing loss, n (Low : High : Total) |
2 : 0 : 0 | 0 : 0 : 6 | |
| Dizziness, n (%) | 0 | 5 (41.67%) | 0.002 |
| Tinnitus, n (%) | 0 | 3 (25.00%) | 0.031 |
| Diplopia, n (%) | 0 | 1 (8.34%) | 0.333 |
| Hoarseness, n (%) | 0 | 1 (8.34%) | 0.333 |
| Damage degree | Latency change | Amplitude change | ||
|---|---|---|---|---|
| Phase I | Mild | < 1ms | < 50% | |
|
Phase II |
Moderate | > 1ms | > 50% | |
|
Severe |
1 | > 2ms | > 80% | |
| 2 | No change | > 50% (abrupt change) | ||
| 3 | No reproducibility | |||
|
Phase III |
Critical |
1 2 |
Loss - traumatic mechanical damage Loss – vascular circulation damage |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




