Submitted:
31 May 2023
Posted:
01 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Mechanism of radiation in combination with immune checkpoint inhibitors
3. Gastroesophageal Cancer
- Phase I/II Studies
- Retrospective Studies
- Phase III Study
- Ongoing Studies
4. Hepatocellular carcinoma (HCC)
- ICI alone studies in HCC
- RT with TKI in HCC
- RT with ICI in HCC: Phase I study
- RT with ICI in HCC: Retrospective Data
- RT with ICI in HCC: Ongoing studies
- TARE with ICI in HCC
5. Cholangiocarcinoma (CCA)
- ICI in advanced CCA
- RT with ICI in CCA: Phase II Studies
6. Pancreas cancer
- RT with ICI in RPC and BRPC
- RT with ICI in LAPC
| NCT Number | Disease status | Interventions | Outcome Measures | Phase |
|---|---|---|---|---|
| NCT04098432 | Locally Advanced Unresectable Pancreatic Adenocarcinoma | SBRT + Nivolumab | Safety | 1/2 |
| NCT04247165 | Pancreatic Cancer. | SBRT + Ipilimumab + Nivolumab | PFS | 1/2 |
| NCT04390399 | Locally Advanced or Metastatic Pancreatic Cancer | SBRT + Chemo +/- IT | PFS/ ORR | 2 |
| NCT04361162 | MSS Pancreatic Cancer | RT + Nivolumab + Ipilimumab | ORR | 2 |
| NCT03563248 | Localized Pancreatic Cancer | FOLFIRINOX + SBRT + Surgery +/- Nivolumab +/- Losartan | R0 Resection | 2 |
| NCT05116917 | Pancreatic Cancer. | SBRT + Nivolumab + Influenza Vaccine | ORR | 2 |
| NCT03161379 | Borderline Resectable Pancreatic Cancer | SBRT + Nivolumab + GVAX Pancreas Vaccine | ORR | 2 |
7. Colorectal Cancer
- ICI alone in CRC: Phase II Studies
- RT with ICI in CRC: Phase I/II Studies
- RT with ICI in CRC: Ongoing Studies
8. Anal Cancer
9. Limitations
10. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Lu, L.; Mullins, C.S.; Schafmayer, C.; Zeißig, S.; Linnebacher, M. A Global Assessment of Recent Trends in Gastrointestinal Cancer and Lifestyle-Associated Risk Factors. Cancer Commun (Lond) 2021, 41, 1137–1151. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA Cancer J Clin 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Kraehenbuehl, L.; Weng, C.-H.; Eghbali, S.; Wolchok, J.D.; Merghoub, T. Enhancing Immunotherapy in Cancer by Targeting Emerging Immunomodulatory Pathways. Nat Rev Clin Oncol 2022, 19, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Wolchok, J.D. Cancer Immunotherapy Using Checkpoint Blockade. Science 2018, 359, 1350–1355. [Google Scholar] [CrossRef] [PubMed]
- Seidel, J.A.; Otsuka, A.; Kabashima, K. Anti-PD-1 and Anti-CTLA-4 Therapies in Cancer: Mechanisms of Action, Efficacy, and Limitations. Front Oncol 2018, 8, 86. [Google Scholar] [CrossRef] [PubMed]
- Burnette, B.; Weichselbaum, R.R. Radiation as an Immune Modulator. Semin Radiat Oncol 2013, 23, 273–280. [Google Scholar] [CrossRef]
- Park, B.; Yee, C.; Lee, K.-M. The Effect of Radiation on the Immune Response to Cancers. Int J Mol Sci 2014, 15, 927–943. [Google Scholar] [CrossRef]
- Van Limbergen, E.J.; De Ruysscher, D.K.; Olivo Pimentel, V.; Marcus, D.; Berbee, M.; Hoeben, A.; Rekers, N.; Theys, J.; Yaromina, A.; Dubois, L.J.; et al. Combining Radiotherapy with Immunotherapy: The Past, the Present and the Future. Br J Radiol 2017, 90, 20170157. [Google Scholar] [CrossRef]
- Gupta, A.; Probst, H.C.; Vuong, V.; Landshammer, A.; Muth, S.; Yagita, H.; Schwendener, R.; Pruschy, M.; Knuth, A.; van den Broek, M. Radiotherapy Promotes Tumor-Specific Effector CD8+ T Cells via Dendritic Cell Activation. J Immunol 2012, 189, 558–566. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, W.; Li, N.; Neri, S.; Sharma, A.; Jiang, W.; Lin, S.H. Combining Immunotherapy and Radiotherapy for Cancer Treatment: Current Challenges and Future Directions. Front Pharmacol 2018, 9, 185. [Google Scholar] [CrossRef]
- Sharabi, A.B.; Lim, M.; DeWeese, T.L.; Drake, C.G. Radiation and Checkpoint Blockade Immunotherapy: Radiosensitisation and Potential Mechanisms of Synergy. Lancet Oncol 2015, 16, e498–509. [Google Scholar] [CrossRef] [PubMed]
- Sharabi, A.B.; Nirschl, C.J.; Kochel, C.M.; Nirschl, T.R.; Francica, B.J.; Velarde, E.; Deweese, T.L.; Drake, C.G. Stereotactic Radiation Therapy Augments Antigen-Specific PD-1-Mediated Antitumor Immune Responses via Cross-Presentation of Tumor Antigen. Cancer Immunol Res 2015, 3, 345–355. [Google Scholar] [CrossRef]
- Germino, E.A.; Govindarajan, A.; Sedrak, M.S.; Li, D.; Amini, A. Multimodality Treatment with Radiotherapy and Immunotherapy in Older Adults: Rationale, Evolving Data, and Current Recommendations. Semin Radiat Oncol 2022, 32, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Pointer, K.B.; Pitroda, S.P.; Weichselbaum, R.R. Radiotherapy and Immunotherapy: Open Questions and Future Strategies. Trends Cancer 2022, 8, 9–20. [Google Scholar] [CrossRef]
- Badiyan, S.; Kaiser, A.; Eastman, B.; Forsthoefel, M.; Zeng, J.; Unger, K.; Chuong, M. Immunotherapy and Radiation Therapy for Gastrointestinal Malignancies: Hope or Hype? Transl Gastroenterol Hepatol 2020, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Oh, P.; Du, K.L.; Leichman, L.; Aifantis, I. PD-1 Blockade Enhances the Efficacy of Chemoradiation in a Mouse Model of Esophageal Cancer. International Journal of Radiation Oncology*Biology*Physics 2016, 96, S127–S128. [Google Scholar] [CrossRef]
- Hong, S.; Bi, M.; Yu, H.; Yan, Z.; Wang, H. Radiation Therapy Enhanced Therapeutic Efficacy of Anti-PD1 against Gastric Cancer. J Radiat Res 2020, 61, 851–859. [Google Scholar] [CrossRef]
- Zhang, W.; Yan, C.; Gao, X.; Li, X.; Cao, F.; Zhao, G.; Zhao, J.; Er, P.; Zhang, T.; Chen, X.; et al. Safety and Feasibility of Radiotherapy Plus Camrelizumab for Locally Advanced Esophageal Squamous Cell Carcinoma. Oncologist 2021, 26, e1110–e1124. [Google Scholar] [CrossRef]
- Uboha, N.V.; Eickhoff, J.C.; Maloney, J.D.; McCarthy, D.; DeCamp, M.; Deming, D.A.; LoConte, N.K.; Matkowskyj, K.A.; Patel, M.A.; Hurst, N.; et al. Phase I/II Trial of Perioperative Avelumab in Combination with Chemoradiation (CRT) in the Treatment of Stage II/III Resectable Esophageal and Gastroesophageal Junction (E/GEJ) Cancer. JCO 2022, 40, 4034–4034. [Google Scholar] [CrossRef]
- Zhu, M.; Chen, C.; Foster, N.R.; Hartley, C.; Mounajjed, T.; Salomao, M.A.; Fruth, B.F.; Beamer, S.E.; Kim, Y.; Harrington, S.M.; et al. Pembrolizumab in Combination with Neoadjuvant Chemoradiotherapy for Patients with Resectable Adenocarcinoma of the Gastroesophageal Junction. Clin Cancer Res 2022, 28, 3021–3031. [Google Scholar] [CrossRef]
- van den Ende, T.; de Clercq, N.C.; van Berge Henegouwen, M.I.; Gisbertz, S.S.; Geijsen, E.D.; Verhoeven, R.H.A.; Meijer, S.L.; Schokker, S.; Dings, M.P.G.; Bergman, J.J.G.H.M.; et al. Neoadjuvant Chemoradiotherapy Combined with Atezolizumab for Resectable Esophageal Adenocarcinoma: A Single-Arm Phase II Feasibility Trial (PERFECT). Clin Cancer Res 2021, 27, 3351–3359. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cheng, Y.; Wu, Y.; Cao, F.; Liu, Q.; Gao, G. Efficacy and Safety of Consolidative Camrelizumab Following Definitive Concurrent Chemoradiotherapy in Patients with Locally Advanced Esophageal Squamous Cell Cancer. Annals of Oncology 2022, 33, S1124. [Google Scholar] [CrossRef]
- Wei, T.; Ti, W.; Song, Q.; Cheng, Y. Study of PD-1 Inhibitors in Combination with Chemoradiotherapy/Chemotherapy in Patients with Esophageal Squamous Carcinoma. Curr Oncol 2022, 29, 2920–2927. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Yao, G.; Li, L.; Feng, A.; Zhang, W.; Xu, X.; Li, Q.; Yang, Z. Effects of Radiotherapy on Survival of Esophageal Cancer Patients Receiving Immunotherapy: Propensity Score Analysis and Nomogram Construction. Cancer Manag Res 2022, 14, 2357–2371. [Google Scholar] [CrossRef]
- Peng, F.; Lian, H.M.; Niu, S.Q.; Liufu, W.J.; Yu, T.T.; Bao, Y. Induction Anti-PD-1 Immunotherapy plus Chemotherapy Followed by Definitive Chemoradiation Therapy in Locally Advanced Esophageal Squamous Cell Carcinoma: A Real-World Retrospective Study. International Journal of Radiation Oncology*Biology*Physics 2022, 114, e165. [Google Scholar] [CrossRef]
- Kelly, R.J.; Ajani, J.A.; Kuzdzal, J.; Zander, T.; Van Cutsem, E.; Piessen, G.; Mendez, G.; Feliciano, J.; Motoyama, S.; Lièvre, A.; et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N Engl J Med 2021, 384, 1191–1203. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Benson, A.B.; D’Angelica, M.I.; Abbott, D.E.; Anaya, D.A.; Anders, R.; Are, C.; Bachini, M.; Borad, M.; Brown, D.; Burgoyne, A.; et al. Hepatobiliary Cancers, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2021, 19, 541–565. [Google Scholar] [CrossRef] [PubMed]
- Sayan, M.; Yegya-Raman, N.; Greco, S.H.; Gui, B.; Zhang, A.; Chundury, A.; Grandhi, M.S.; Hochster, H.S.; Kennedy, T.J.; Langan, R.C.; et al. Rethinking the Role of Radiation Therapy in the Treatment of Unresectable Hepatocellular Carcinoma: A Data Driven Treatment Algorithm for Optimizing Outcomes. Front Oncol 2019, 9, 345. [Google Scholar] [CrossRef]
- Falette Puisieux, M.; Pellat, A.; Assaf, A.; Ginestet, C.; Brezault, C.; Dhooge, M.; Soyer, P.; Coriat, R. Therapeutic Management of Advanced Hepatocellular Carcinoma: An Updated Review. Cancers (Basel) 2022, 14, 2357. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Lau, G.; Kudo, M.; Chan, S.L.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Van Dao, T.; De Toni, E.N.; et al. Tremelimumab plus Durvalumab in Unresectable Hepatocellular Carcinoma. NEJM Evidence 2022, 1. [Google Scholar] [CrossRef]
- Dawson, L.A.; Winter, K.; Knox, J.; Zhu, A.X.; Krishnan, S.; Guha, C.; Kachnic, L.A.; Gillin, M.T.; Hong, T.S.; Craig, T.; et al. NRG/RTOG 1112: Randomized Phase III Study of Sorafenib vs. Stereotactic Body Radiation Therapy (SBRT) Followed by Sorafenib in Hepatocellular Carcinoma (HCC) (NCT01730937). International Journal of Radiation Oncology*Biology*Physics 2022, 114, 1057. [Google Scholar] [CrossRef]
- Juloori, A.; Katipally, R.R.; Lemons, J.M.; Singh, A.K.; Iyer, R.; Robbins, J.R.; George, B.; Hall, W.A.; Pitroda, S.P.; Arif, F.; et al. Phase 1 Randomized Trial of Stereotactic Body Radiation Therapy Followed by Nivolumab plus Ipilimumab or Nivolumab Alone in Advanced/Unresectable Hepatocellular Carcinoma. Int J Radiat Oncol Biol Phys 2023, 115, 202–213. [Google Scholar] [CrossRef] [PubMed]
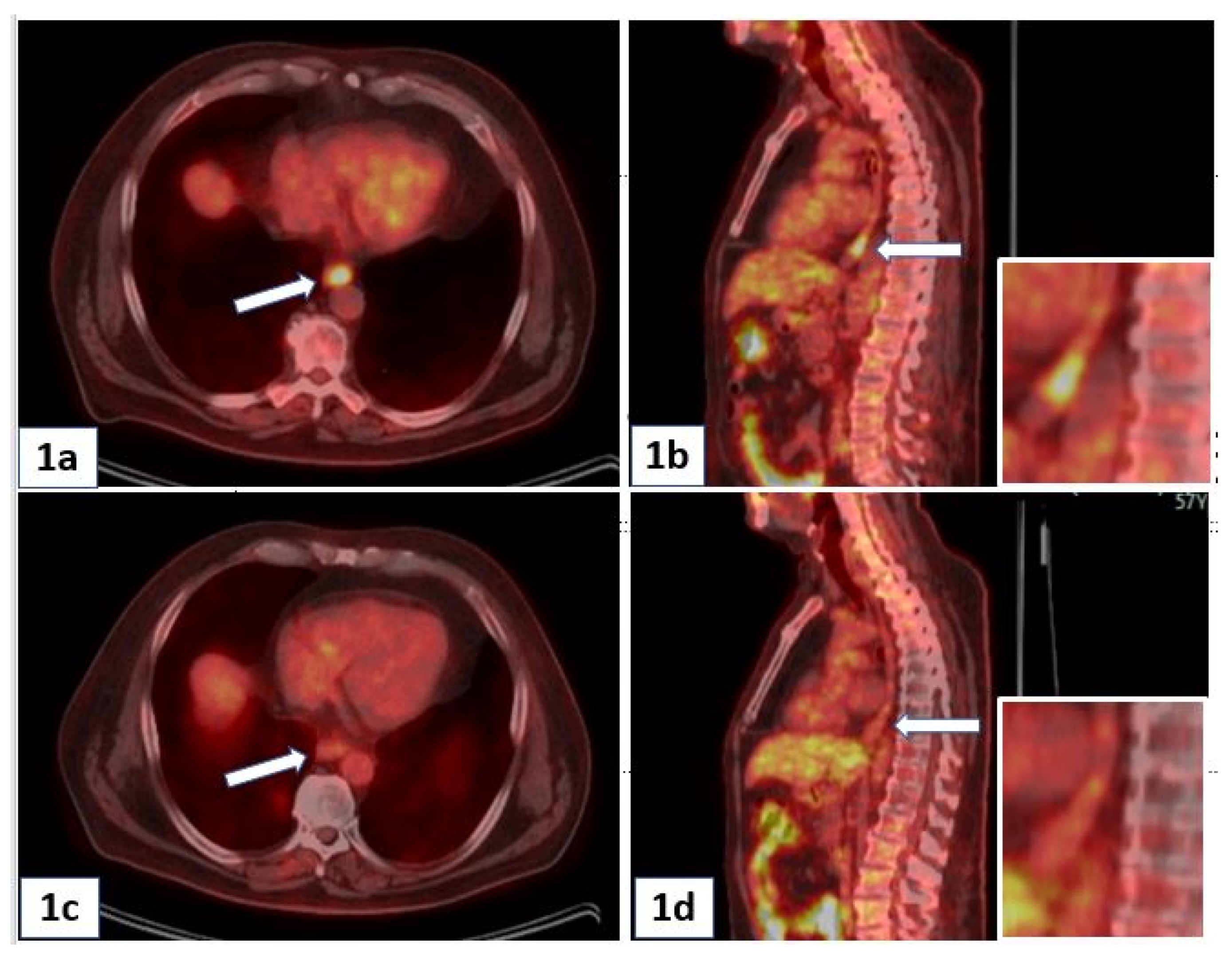
- Chiang, C.-L.; Chan, A.C.Y.; Chiu, K.W.H.; Kong, F.-M.S. Combined Stereotactic Body Radiotherapy and Checkpoint Inhibition in Unresectable Hepatocellular Carcinoma: A Potential Synergistic Treatment Strategy. Front Oncol 2019, 9, 1157. [Google Scholar] [CrossRef]
- Chiang, C.L.; Chan, A.C.Y.; Chiu, W.H.K.; Kong, F.M. Combined Stereotactic Body Radiotherapy and Immunotherapy (SBRT-IO) vs. TACE in Locally Advanced Hepatocellular Carcinoma (HCC): Propensity Score Matching Analysis. International Journal of Radiation Oncology*Biology*Physics 2021, 111, e35–e36. [Google Scholar] [CrossRef]
- Chew, V.; Lee, Y.H.; Pan, L.; Nasir, N.J.M.; Lim, C.J.; Chua, C.; Lai, L.; Hazirah, S.N.; Lim, T.K.H.; Goh, B.K.P.; et al. Immune Activation Underlies a Sustained Clinical Response to Yttrium-90 Radioembolisation in Hepatocellular Carcinoma. Gut 2019, 68, 335–346. [Google Scholar] [CrossRef]
- Rivoltini, L.; Bhoori, S.; Camisaschi, C.; Bergamaschi, L.; Lalli, L.; Frati, P.; Citterio, D.; Castelli, C.; Mazzaferro, V. Y90-Radioembolisation in Hepatocellular Carcinoma Induces Immune Responses Calling for Early Treatment with Multiple Checkpoint Blockers. Gut 2023, 72, 406–407. [Google Scholar] [CrossRef]
- de la Torre-Aláez, M.; Matilla, A.; Varela, M.; Iñarrairaegui, M.; Reig, M.; Lledó, J.L.; Arenas, J.I.; Lorente, S.; Testillano, M.; Márquez, L.; et al. Nivolumab after Selective Internal Radiation Therapy for the Treatment of Hepatocellular Carcinoma: A Phase 2, Single-Arm Study. J Immunother Cancer 2022, 10, e005457. [Google Scholar] [CrossRef]
- Tai, D.; Loke, K.; Gogna, A.; Kaya, N.A.; Tan, S.H.; Hennedige, T.; Ng, D.; Irani, F.; Lee, J.; Lim, J.Q.; et al. Radioembolisation with Y90-Resin Microspheres Followed by Nivolumab for Advanced Hepatocellular Carcinoma (CA 209-678): A Single Arm, Single Centre, Phase 2 Trial. Lancet Gastroenterol Hepatol 2021, 6, 1025–1035. [Google Scholar] [CrossRef]
- Gkika, E.; Hawkins, M.A.; Grosu, A.-L.; Brunner, T.B. The Evolving Role of Radiation Therapy in the Treatment of Biliary Tract Cancer. Front Oncol 2020, 10, 604387. [Google Scholar] [CrossRef] [PubMed]
- Ben-Josef, E.; Guthrie, K.A.; El-Khoueiry, A.B.; Corless, C.L.; Zalupski, M.M.; Lowy, A.M.; Thomas, C.R.; Alberts, S.R.; Dawson, L.A.; Micetich, K.C.; et al. SWOG S0809: A Phase II Intergroup Trial of Adjuvant Capecitabine and Gemcitabine Followed by Radiotherapy and Concurrent Capecitabine in Extrahepatic Cholangiocarcinoma and Gallbladder Carcinoma. J Clin Oncol 2015, 33, 2617–2622. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.-Y.; Ruth He, A.; Qin, S.; Chen, L.-T.; Okusaka, T.; Vogel, A.; Kim, J.W.; Suksombooncharoen, T.; Ah Lee, M.; Kitano, M.; et al. Durvalumab plus Gemcitabine and Cisplatin in Advanced Biliary Tract Cancer. NEJM Evidence 2022, 1. [Google Scholar] [CrossRef]
- Liu, X.; Yao, J.; Song, L.; Zhang, S.; Huang, T.; Li, Y. Local and Abscopal Responses in Advanced Intrahepatic Cholangiocarcinoma with Low TMB, MSS, PMMR and Negative PD-L1 Expression Following Combined Therapy of SBRT with PD-1 Blockade. J Immunother Cancer 2019, 7, 204. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Chen, Y.; Du, S.; Yang, X.; Chen, Y.; Ji, Y.; Zeng, Z. Integration of Radiotherapy with Anti-PD-1 Antibody for the Treatment of Intrahepatic or Hilar Cholangiocarcinoma: Reflection from Four Cases. Cancer Biol Ther 2021, 22, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.A.; Duong, M.; Sohal, D.P.S.; Gandhi, N.S.; Beg, M.S.; Wang-Gillam, A.; Wade, J.L.; Chiorean, E.G.; Guthrie, K.A.; Lowy, A.M.; et al. Surgical Outcome Results From SWOG S1505: A Randomized Clinical Trial of MFOLFIRINOX Versus Gemcitabine/Nab-Paclitaxel for Perioperative Treatment of Resectable Pancreatic Ductal Adenocarcinoma. Ann Surg 2020, 272, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Versteijne, E.; Suker, M.; Groothuis, K.; Akkermans-Vogelaar, J.M.; Besselink, M.G.; Bonsing, B.A.; Buijsen, J.; Busch, O.R.; Creemers, G.-J.M.; van Dam, R.M.; et al. Preoperative Chemoradiotherapy Versus Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J Clin Oncol 2020, 38, 1763–1773. [Google Scholar] [CrossRef]
- Rahma, O.; Katz, M.; Bauer, T.; Wolpin, B.; Stucky, C.-C.; Bekaii-Saab, T.; Elias, R.; Dias-Costa, A.; Nowak, J.; Patrick, L.; et al. Randomized Multicenter Study of Neoadjuvant Chemoradiation Therapy (CRT) Alone or in Combination with Pembrolizumab in Patients with Resectable or Borderline Resectable Pancreatic Cancer. J Immunother Cancer 2021, 9, A1010–A1010. [Google Scholar] [CrossRef]
- Zhu, X.; Cao, Y.; Liu, W.; Ju, X.; Zhao, X.; Jiang, L.; Ye, Y.; Jin, G.; Zhang, H. Stereotactic Body Radiotherapy plus Pembrolizumab and Trametinib versus Stereotactic Body Radiotherapy plus Gemcitabine for Locally Recurrent Pancreatic Cancer after Surgical Resection: An Open-Label, Randomised, Controlled, Phase 2 Trial. Lancet Oncol 2022, 23, e105–e115. [Google Scholar] [CrossRef]
- Koopman, M.; Kortman, G. a. M.; Mekenkamp, L.; Ligtenberg, M.J.L.; Hoogerbrugge, N.; Antonini, N.F.; Punt, C.J.A.; van Krieken, J.H.J.M. Deficient Mismatch Repair System in Patients with Sporadic Advanced Colorectal Cancer. Br J Cancer 2009, 100, 266–273. [Google Scholar] [CrossRef]
- Lumish, M.A.; Cercek, A. Immunotherapy for the Treatment of Colorectal Cancer. J Surg Oncol 2021, 123, 760–774. [Google Scholar] [CrossRef] [PubMed]
- Lenz, H.-J.; Van Cutsem, E.; Luisa Limon, M.; Wong, K.Y.M.; Hendlisz, A.; Aglietta, M.; García-Alfonso, P.; Neyns, B.; Luppi, G.; Cardin, D.B.; et al. First-Line Nivolumab Plus Low-Dose Ipilimumab for Microsatellite Instability-High/Mismatch Repair-Deficient Metastatic Colorectal Cancer: The Phase II CheckMate 142 Study. J Clin Oncol 2022, 40, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Diaz, L.A.; Shiu, K.-K.; Kim, T.-W.; Jensen, B.V.; Jensen, L.H.; Punt, C.; Smith, D.; Garcia-Carbonero, R.; Benavides, M.; Gibbs, P.; et al. Pembrolizumab versus Chemotherapy for Microsatellite Instability-High or Mismatch Repair-Deficient Metastatic Colorectal Cancer (KEYNOTE-177): Final Analysis of a Randomised, Open-Label, Phase 3 Study. Lancet Oncol 2022, 23, 659–670. [Google Scholar] [CrossRef]
- Chalabi, M.; Fanchi, L.F.; Dijkstra, K.K.; Van den Berg, J.G.; Aalbers, A.G.; Sikorska, K.; Lopez-Yurda, M.; Grootscholten, C.; Beets, G.L.; Snaebjornsson, P.; et al. Neoadjuvant Immunotherapy Leads to Pathological Responses in MMR-Proficient and MMR-Deficient Early-Stage Colon Cancers. Nat Med 2020, 26, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Chalabi, M.; Verschoor, Y.L.; van den Berg, J.; Sikorska, K.; Beets, G.; Lent, A.V.; Grootscholten, M.C.; Aalbers, A.; Buller, N.; Marsman, H.; et al. LBA7 Neoadjuvant Immune Checkpoint Inhibition in Locally Advanced MMR-Deficient Colon Cancer: The NICHE-2 Study. Annals of Oncology 2022, 33, S1389. [Google Scholar] [CrossRef]
- Cercek, A.; Lumish, M.; Sinopoli, J.; Weiss, J.; Shia, J.; Lamendola-Essel, M.; El Dika, I.H.; Segal, N.; Shcherba, M.; Sugarman, R.; et al. PD-1 Blockade in Mismatch Repair-Deficient, Locally Advanced Rectal Cancer. N Engl J Med 2022, 386, 2363–2376. [Google Scholar] [CrossRef]
- Deng, L.; Liang, H.; Burnette, B.; Beckett, M.; Darga, T.; Weichselbaum, R.R.; Fu, Y.-X. Irradiation and Anti-PD-L1 Treatment Synergistically Promote Antitumor Immunity in Mice. J Clin Invest 2014, 124, 687–695. [Google Scholar] [CrossRef]
- Dovedi, S.J.; Adlard, A.L.; Lipowska-Bhalla, G.; McKenna, C.; Jones, S.; Cheadle, E.J.; Stratford, I.J.; Poon, E.; Morrow, M.; Stewart, R.; et al. Acquired Resistance to Fractionated Radiotherapy Can Be Overcome by Concurrent PD-L1 Blockade. Cancer Res 2014, 74, 5458–5468. [Google Scholar] [CrossRef]
- Yoshino, T.; Bando, H.; Tsukada, Y.; Inamori, K.; Yuki, S.; Komatsu, Y.; Homma, S.; Uemura, M.; Kato, T.; Kotani, D.; et al. Voltage: Investigator-Initiated Clinical Trial of Nivolumab Monotherapy and Subsequent Radical Surgery Following Preoperative Chemoradiotherapy in Patients with Microsatellite Stable Locally Advanced Rectal Cancer. JCO 2019, 37, 3606–3606. [Google Scholar] [CrossRef]
- George, T.J.; Yothers, G.; Rahma, O.E.; Hong, T.S.; Russell, M.M.; You, Y.N.; Parker, W.; Jacobs, S.A.; Lucas, P.C.; Colangelo, L.H.; et al. Long-Term Results from NRG-GI002: A Phase II Clinical Trial Platform Using Total Neoadjuvant Therapy (TNT) in Locally Advanced Rectal Cancer (LARC). JCO 2023, 41, 7–7. [Google Scholar] [CrossRef]
- Eng, C.; Ciombor, K.K.; Cho, M.; Dorth, J.A.; Rajdev, L.N.; Horowitz, D.P.; Gollub, M.J.; Jácome, A.A.; Lockney, N.A.; Muldoon, R.L.; et al. Anal Cancer: Emerging Standards in a Rare Disease. J Clin Oncol 2022, 40, 2774–2788. [Google Scholar] [CrossRef] [PubMed]
- Morris, V.K.; Salem, M.E.; Nimeiri, H.; Iqbal, S.; Singh, P.; Ciombor, K.; Polite, B.; Deming, D.; Chan, E.; Wade, J.L.; et al. Nivolumab for Previously Treated Unresectable Metastatic Anal Cancer (NCI9673): A Multicentre, Single-Arm, Phase 2 Study. Lancet Oncol 2017, 18, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Marabelle, A.; Cassier, P.A.; Fakih, M.; Kao, S.; Nielsen, D.; Italiano, A.; Guren, T.K.; van Dongen, M.G.J.; Spencer, K.; Bariani, G.M.; et al. Pembrolizumab for Previously Treated Advanced Anal Squamous Cell Carcinoma: Results from the Non-Randomised, Multicohort, Multicentre, Phase 2 KEYNOTE-158 Study. Lancet Gastroenterol Hepatol 2022, 7, 446–454. [Google Scholar] [CrossRef] [PubMed]
| Author/Study | Type of study | Number (n) | Disease status | ICI | Intervention | Results |
|---|---|---|---|---|---|---|
| Zhang[18] | Phase 1 | 19 | Locally advanced | Camrelizumab | RT-ICI f/b ICI | PFS 11.7 months OS 16.7 months |
| Zhu[20] | Phase 1/2 | 31 | Resectable (Stage II/III) |
Pembrolizumab | CRT-ICI f/b Surgery f/b adjuvant ICI | pCR in 22.6% |
| PERFECT[21] | Phase 2 | 40 | Resectable | Atezolizumab | CRT-ICI f/b Surgery | pCR in 25% |
| Wang[22] | Phase 2 | 12 | Locally advanced | Camrelizumab | Definitive CRT f/b consolidative ICI (n=12) | 11/12 patients had SD |
| Wie[23] | Retrospective | 55 | Inoperable | Camrelizumab Tislelizumab Sintilimab |
CRT-ICI (n=26) CRT alone (n= 29) |
Improved OS with CRT-ICI |
| Nie[24] | Retrospective | 134 | Locally advanced | Carmelizumab Pembrolizumab |
CHT- ICI f/b RT(n=55) CHT- ICI (n= 79) |
PFS (15.7 vs. 5.7 m) OS (15.7 vs. 12 m) |
| Peng[25] | Retrospective | 62 | Locally advanced | ---- | CHT-ICI f/b definitive CRT | PFS 28.8 months |
| CheckMate 577[26] | Phase 3 | 794 | Resectable | Nivolumab | NA-CRT f/b Surgery +/-adjuvant ICI (n= 532 vs 262) | DFS 24.4 vs 11 months |
| NCT Number | Interventions | Primary outcome | Phase |
|---|---|---|---|
| NCT05650216 | Camrelizumab + CRT | Safety, pCR | 2 |
| NCT05043688 | Camrelizumab + CRT | pCR | 2 |
| NCT04229459 | Nivolumab + CRT | pCR | 2 |
| NCT03777813 | Durvalumab +CRT vs. CRT | PFS | 2 |
| NCT05520619 | Tislelizumab + CRT | PFS | 2 |
| NCT05387681 | Envafolimab + CRT | pCR | 2 |
| NCT04929392 | Pembrolizumab + CRT | pCR | 2 |
| NCT04888403 | Toripalimab + CRT | pCR | 2 |
| NCT03257163 | Pembrolizumab → Surgery → adj CHT and CRT with Pembrolizumab | DFS | 2 |
| NCT04973306 | Tislelizumab + CRT vs. CRT | pCR, OS | 2,3 |
| NCT03604991 | Pre-op Nivolumab + CRT vs Pre-op CRT with post-surgery adjuvant (Nivo vs Nivo/Ipi) | pCR, DFS, OS | 3 |
| NCT04404491 | Camrelizumab + RT vs. RT + CHT | AE, PFS | 3 |
| NCT04821843 | Nimotuzumab + CRT vs. Nimotuzumab + CHT | OS | 3 |
| NCT04821778 | Nimotuzumab + CRT vs CRT | OS | 3 |
| NCT05244798 | Sintilimab + CHT vs. Sintilimab + CRT vs. CRT | pCR | 3 |
| NCT04807673 | Pembrolizumab + CRT | Event Free Survival (EFS) | 3 |
| Author | Type of study | Patient characteristics | Intervention | Results |
|---|---|---|---|---|
| Chiang | Case series | N = 5 Unresectable HCC |
SBRT + Nivolumab | CR: 2/5 PR: 3/5 |
| Chiang | Retrospective | N = 16 | SBRT + Nivolumab | CR: 50% PR: 37.5% |
| Juloori | Prospective Phase 1 RCT | N = 14 | SBRT + Nivolumab (n = 6) | PR—12.5% SD—37.5% PD—50% |
| SBRT + Ipilimumab + nivolumab (n = 8) | PR—50% SD—37.5% PD—12.5% |
| NCT Number | Interventions | Outcome Measures | Phase |
|---|---|---|---|
| NCT05488522 | SBRT + atezolizumab and bevacizumab | PFS | 1 |
| NCT03817736 | TACE followed by SBRT followed by Avelumab | Response Rate/ Amenable to surgery | 2 |
| NCT04913480 | SBRT + Durvalumab (1 yr) | PFS | 2 |
| NCT04988945 | TACE followed by SBRT followed by Durvalumab + Tremelimumab | Response Rate/ Amenable to surgery | 2 |
| NCT04611165 | Hypofractionated radiation (10 fractions) + Nivolumab | PFS | 2 |
| NCT04430452 | Hypofractionated radiation + Durvalumab +/- Tremelimumab | Response Rate | 2 |
| NCT03316872 | SBRT + Pembrolizumab | Response Rate | 2 |
| NCT05366829 | RT + Tislelizumab | PFS | 2 |
| NCT04167293 | SBRT + Sintilimab | PFS | 2/3 |
| NCT Number | Interventions | Outcome Measures | Phase |
|---|---|---|---|
| NCT04708067 | RT + Bintrafusp Alfa | Response | 1 |
| NCT04866836 | RT + Tislelizumab | Response | 2 |
| NCT03898895 (CORRECT) |
RT + Camrelizumab | PFS | 2 |
| NCT Number | Phase | Stage | ARM | Interventions | Outcome Measures |
|---|---|---|---|---|---|
| NCT03127007 (R-IMMUNE) |
Phase 1/2 | LARC | A | LC CRT + Atezolizumab → TME | AE, pCR |
| B | LC CRT → TME | ||||
| NCT02948348 | Phase 1/2 | LARC | -- | LC CRT + Nivo → TME | pCR |
| NCT05245474 | Phase 2 | LARC | A | LC CRT + Concurrent Tislelizumab → TME | pCR |
| B | LC CRT + Sequential Tislelizumab → TME | ||||
| C | LC CRT → TME | ||||
| NCT05576480 | Phase 2 | LARC | -- | SCRT → Penpulimab + CAPEOX → TME | pCR |
| NCT05086627 | Phase 2 | LARC | A | SCRT → Tislelizumab + CAPEOX → TME → CAPEOX | pCR |
| B | SCRT → CAPEOX → TME → CAPEOX | ||||
| NCT04621370 (PRIME-RT) |
Phase 2 | LARC | A | SCRT + Durvalumab → FOLFOX | pCR, cCR |
| B | LCRT + Durvalumab → FOLFOX | ||||
| NCT05507112 | Phase 2 | LARC | A | LC CRT + Concurrent Tislelizumab → TME | pCR |
| B | LC CRT → TME | ||||
| NCT04503694 | Phase 2 | LARC | -- | Regorafenib + Nivolumab → SCRT → Regorafenib + Nivolumab → TME → +/- adjuvant Chemo | pCR |
| NCT04751370 | Phase 2 | LARC | -- | Nivo/Ipi → SCRT → Nivo/Ipi → TME | pCR |
| NCT03921684 | Phase 2 | LARC | -- | LC CRT → FOLFOX + Nivolumab → TME | pCR |
| NCT04124601 | Phase 2 | LARC | A | LC CRT | AE, Response |
| B | LC CRT → Nivo/Ipi | ||||
| NCT03299660 | Phase 2 | LARC | -- | LC CRT → Avelumab → TME | pCR |
| NCT03854799 | Phase 2 | LARC | -- | LC CRT → Avelumab → TME | pCR |
| NCT03503630 | Phase 2 | LARC | -- | SCRT → Avelumab + FOLFOX → TME | pCR |
| NCT04293419 (DUREC) |
Phase 2 | LARC | -- | FOLFOX + Durvalumab → LCCRT → TME | pCR |
| NCT05009069 | Phase 2 | LARC | A | LC CRT + Atezolizumab + Tiragolumab → TME | pCR |
| NCT05484024 | Phase 2/3 | LARC | A | SCRT → NACT + Sintilimab → W/W or TME | pCR, DFS |
| B | SCRT → NACT → W/W or TME |
| NCT Number | Phases | Stage | Interventions | Outcome Measures |
|---|---|---|---|---|
| NCT04046133 (CORINTH) |
Phase 1 | LA III A/B |
CRT + Pembrolizumab | AE, Response |
| NCT04230759 (RADIANCE) |
Phase 2 | LA IIB-IIIC |
CRT (with 5FU/ MMC) | DFS |
| CRT (with 5FU/ MMC/ Durvalumab) | ||||
| NCT04929028 | Phase 2 | Low Risk HIV | CRT (with 5FU/ MMC) | AE, DFS |
| High Risk HIV | CRT (with 5FU/ MMC/ Nivolumab) | |||
| NCT05661188 (TIRANUS) |
Phase 2 | I - IIIB | CRT (with 5FU/ MMC/ Tiraglolumab/ Atezolizumab) | cCR |
| NCT03233711 | Phase 3 | LA II-IIIB |
CRT | DFS |
| CRT → Nivolumab | ||||
| NCT05374252 | Phase 3 | LA III |
CRT (with 5FU/ MMC) | PFS, OS, cCR |
| CRT (with 5FU/ MMC/ Sintilimab) → Adjuvant Sintilimab |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




