Introduction
Brugada Syndrome (BrS) is a myocardial cells channelopathy, first described in 1992, with characteristic electrocardiographic patterns, and it determines a predisposition to sudden death and lethal ventricular arrhythmias[
1].
Today, the diagnosis of BrS is based on the electrocardiogram (ECG), for which, according to the latest advances, two basic morphological patterns have been described. The diagnosis is made if one of the following criteria is met[
1] (excluding phenocopies):
1. ST segment elevation with type 1 pattern morphology: ≥ 2 mm in one or more of the right precordial leads (V1 or V2), positioned in the second, third, or fourth intercostal space.
2. Type 1 morphology appears either spontaneously or after intravenous pharmacological challenge tests using sodium channel blockers (for example: ajmaline).
The type 1 pattern is diagnostic[
1,
2].
The remaining pattern, called type 2, is characterized by ST segment elevation in right precordial leads ˃ 1 mm, followed by a positive or isobiphasic T wave, which gives the ST-T complex a “saddleback” appearance[
1,
2].
These Brugada patterns exist because of the alteration of the transmural electric potential gradient happening in phase 1 of the action potential, due to the imbalance between the input and output of ions to the cardiomyocyte[
2]. However, the genetic origin of BrS implies the involvement of cardiomyocytes as a whole. Why, then, the specificity of Brugada patterns in right precordial leads? Theoretically, repolarization should also be affected in other leads.
Here we present the case of a patient in whom a type 1 pattern in lead III was found on the same electrocardiographic register, along with a type 2 pattern in lead II, in the context of syncope with refractory vagal symptoms.
Clinical Case
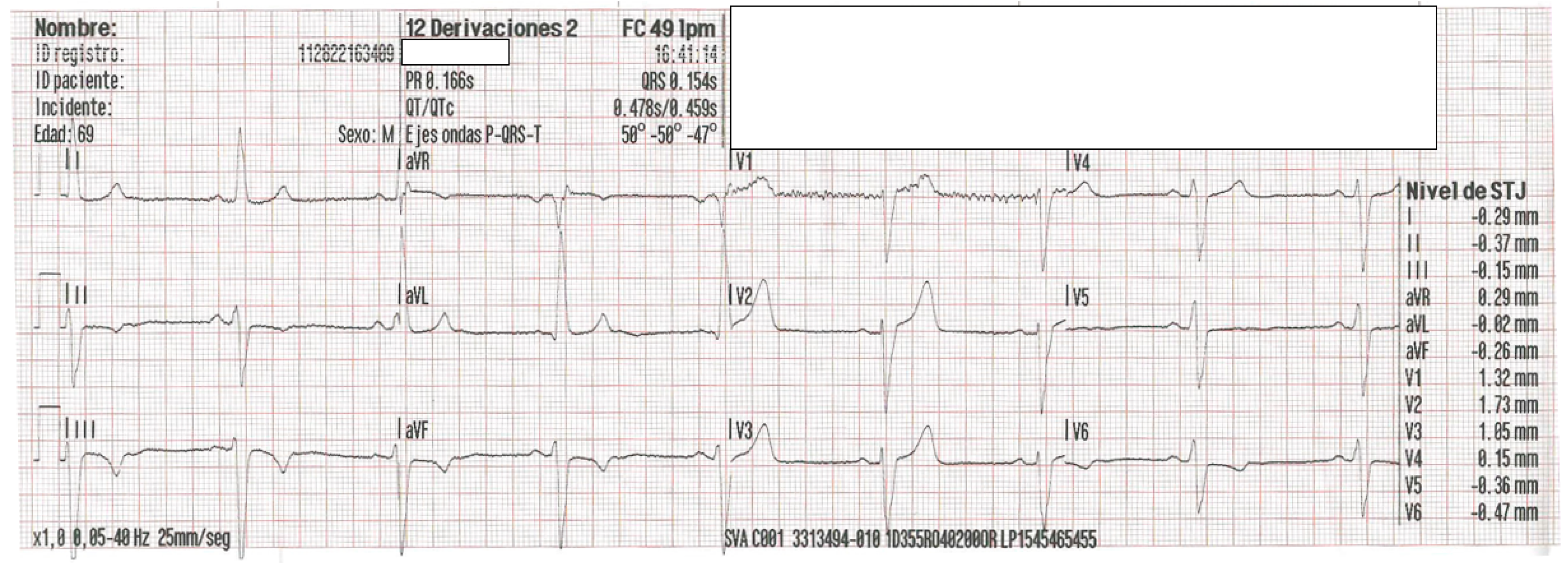
Male, 69 years old, with no known toxic habits, who consumes bisoprolol 2.5 mg every 12 hours, with a personal history of non-compaction cardiomyopathy, and mild-moderate aortic and mitral regurgitation. No family history. He suffers from syncope without prodromes at home with a refractory vagal episode immediately after regaining consciousness. The ECG performed by the Advanced Life Support team (
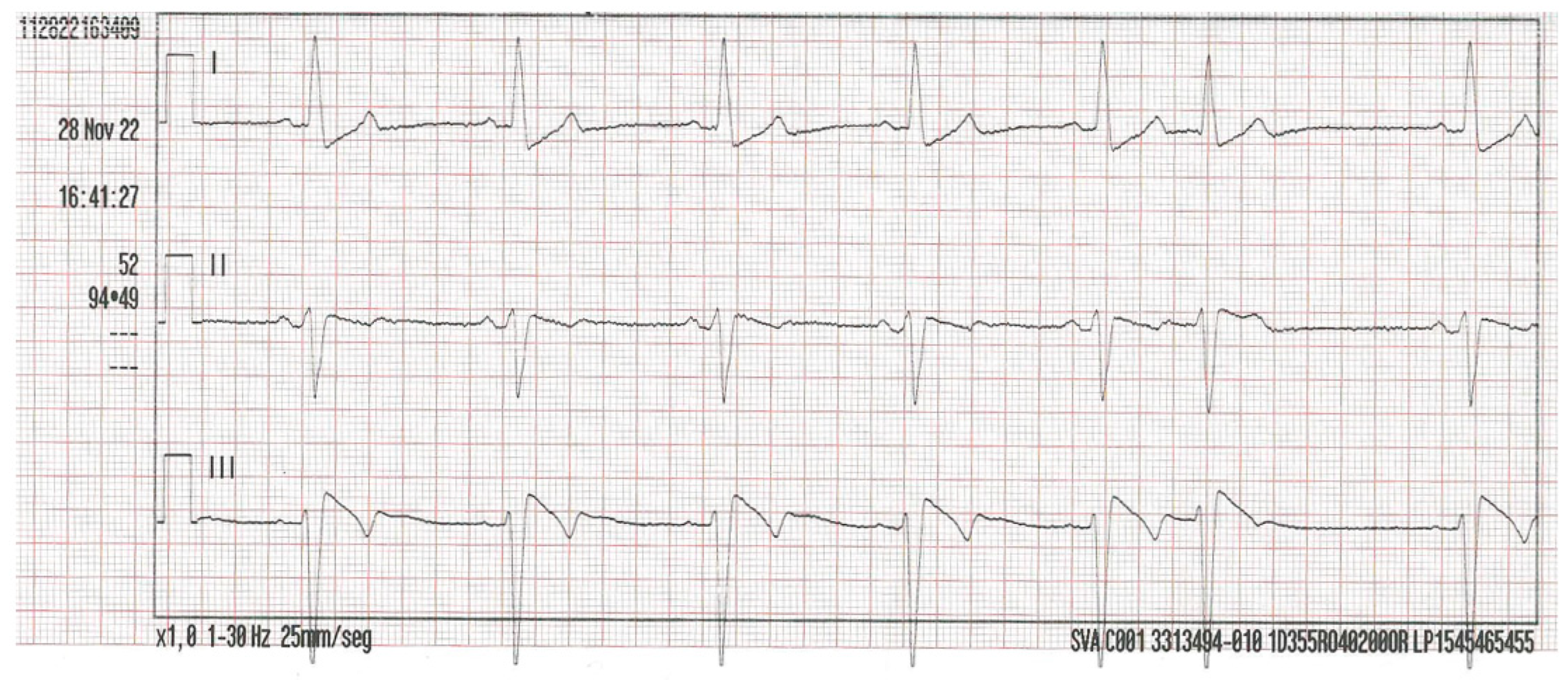
Figure 1) showed sinus bradycardia and a posterior three-lead bipolar rhythm strip (
Figure 2) revealed a Brugada type 1 pattern morphology in III, along with a type 2 pattern in II.
Upon his arrival at the hospital, he had a blood pressure of 80/40 mmHg; the rest of physical examination was normal. The analysis was anodyne, with negative troponin seriation. After the initial assessment in the ER, consultation with Cardiology was made.
Discussion
In the electrocardiographic analysis of
Figure 2 we have:
Lead I: we shall interpret it as a mirror image of III.
Lead II: Brugada pattern type 2.
Lead III: Brugada pattern type 1.
Variability of Brugada patterns in the same patient has been described in the literature, even on the same day[
1], as well as the existence of BrS patterns in lower limb leads[
3]. However, we did not find reported cases that presented different patterns at the same time, in the same tracing.
Regarding the presentation of Brugada patterns in lower leads, Sarkozy et al.[
3] concluded that there are indeed Brugada patterns only in lower leads. Even in one of these cases with a single presentation with a type 2 pattern, the test with ajmaline produced a transformation towards a type 1 pattern, also inferior[
3].
In a molecular biology study, Potet et al.[
4] detected that mutations of the SCN5A gene, which encodes structures for the sodium channel of myocardial cells, can produce a Brugada phenotype in inferior leads.
Based on the work of Chevallier et al.[
5], we have been able to verify that the type 2 pattern morphology of the record in
Figure 2 is equivalent to the type 2 pattern described for right precordial leads. We measured the angle β (> 58º) and length of the base of the triangle of the r' wave, 5 mm below the point of maximum ascent[
1] (4 mm,
Figure 3). These are variables with high predictive values, sensitivity and specificity that allow discerning between type 2 patterns and other causes such as, for example, branch blocks[
1].
Based on this, we can anticipate that in this case, a mixed electrocardiographic pattern was observed, at the same moment, in two lower leads.
To support the diagnosis of BrS in this case, the presence of BrS phenocopies -as cited by Baranchuk et al.[
6]- was discarded (ECG tracings with morphology that mimics BrS but with demonstrable environmental etiology, such as metabolic causes, extracardiac mechanical compression, ischemia, coronary artery disease, pericardial disease, tricuspid valve defects, and electrocution).
It is also interesting to make a reference to the relationship between vagal symptoms and BrS. Mizumaki et al.[
7] conclude that in BrS there is a spontaneous increase in ST elevation related to an increase in vagal tone that may occur at some point throughout daily life.
Lastly, regarding the previous diagnosis of non-compaction cardiomyopathy in the patient we present, there are precedents in the literature of its possible correlation with BrS. Park et al.[
8] described a man with non-compaction cardiomyopathy whose baseline ECG showed a Brugada type 2 pattern in right precordial leads. Chevallier et al.[
5] reported a case of non-compaction cardiomyopathy in a sample of patients with Brugada patterns. This generated the need for us to investigate if any data was reported that related these two pathologies from a more scientifically sustainable profile, for example, from a genetic profile. Shan et al.[
9] described in 2007 a mutation of the SCN5A gene in patients with non-compaction cardiomyopathy who presented arrhythmias. Here we would have a molecular origin, a gene, common to two phenotypically different pathologies, BrS and non-compaction cardiomyopathy.
Conclusions
Brugada patterns should no longer be considered as circumscribed to right precordial leads; it is possible to distinguish them also on the inferior side. There is even the possibility of finding mixed patterns (type 1 together with type 2) in lower leads, on the same electrocardiographic tracing.
In patients with non-compaction cardiomyopathy, with or without vagal symptoms, the coexistence of a BrS is possible due to a possible common genetic origin in the SCN5A gene. For this reason, when faced with a refractory vagal clinical picture, an ECG is recommended. The association of these clinical entities should be studied more deeply, in order to incorporate them into the differential diagnosis of these patients if necessary and thus achieve, with the correct diagnosis of the syndrome, the prevention of malignant arrhythmias and improve the morbidity and survival of these patients.
References
- Brugada J, Campuzano O, Arbelo E, Sarquella-Brugada G, Brugada R. Present Status of Brugada Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018 Aug 28;72(9):1046-1059. [CrossRef]
- Brugada R, Campuzano O, Sarquella-Brugada G, Brugada J, Brugada P. Brugada syndrome. Methodist Debakey Cardiovasc J. 2014 Jan-Mar;10(1):25-8. [CrossRef]
- Sarkozy A, Chierchia GB, Paparella G, Boussy T, De Asmundis C, Roos M, Henkens S, Kaufman L, Buyl R, Brugada R, Brugada J, Brugada P. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009 Apr;2(2):154-61. [CrossRef]
- Potet F, Mabo P, Le Coq G, Probst V, Schott JJ, Airaud F, Guihard G, Daubert JC, Escande D, Le Marec H. Novel brugada SCN5A mutation leading to ST segment elevation in the inferior or the right precordial leads. J Cardiovasc Electrophysiol. 2003 Feb;14(2):200-3. [CrossRef]
- Chevallier S, Forclaz A, Tenkorang J, et al. New Electrocardiographic Criteria for Discriminating Between Brugada Types 2 and 3 Patterns and Incomplete Right Bundle Branch Block. J Am Coll Cardiol. 2011 Nov, 58 (22) 2290–2298. [CrossRef]
- Baranchuk A, Nguyen T, Ryu MH, Femenía F, Zareba W, Wilde AA, Shimizu W, Brugada P, Pérez-Riera AR. Brugada phenocopy: new terminology and proposed classification. Ann Noninvasive Electrocardiol. 2012 Oct;17(4):299-314. [CrossRef]
- Mizumaki K, Fujiki A, Tsuneda T, Sakabe M, Nishida K, Sugao M, Inoue H. Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2004 Jun;15(6):667-73. [CrossRef]
- Park BE, Yang DH. A Case of Ventricular Noncompaction with Brugada-Like Electrocardiography Pattern. Chonnam Med J. 2020 Sep;56(3):208-209. [CrossRef]
- Shan L, Makita N, Xing Y, Watanabe S, Futatani T, Ye F, Saito K, Ibuki K, Watanabe K, Hirono K, Uese K, Ichida F, Miyawaki T, Origasa H, Bowles NE, Towbin JA. SCN5A variants in Japanese patients with left ventricular noncompaction and arrhythmia. Mol Genet Metab. 2008 Apr;93(4):468-74. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).