Submitted:
16 May 2023
Posted:
16 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Patients
Manometric Procedure
- Mean resting anal pressure;
- Maximum voluntary contraction during squeeze maneuver (vs. resting pressure);
- Sphincteric asymmetry (difference between resting and squeeze pressure above 20% between four cardinal anal segments, evaluated with 3D analysis);
- RAIR/rectal sensibility (recto-anal inhibitory reflex / first sensation and urge sensation)
- Presence of abdominal-perineal dyssynergia
- General aspects of pressure cylindric image
Statistical Analysis
3. Results
| Type of ARM |
Mean ARP mmHg Mean (SD) |
Ant ARP Mean (SD) |
Post ARP Mean (SD) |
Right ARP Mean (SD) |
Left ARP Mean (SD) |
Mean ASP Mean (SD) |
Ant ASP Mean (SD) |
Post ASP Mean (SD) |
Right ASP Mean (SD) |
Left ASP Mean (SD) |
| Total pts | 35.6 (13.1) | 32.9 (13.6) |
37.2 (13.4) | 33.6 (12.7) | 33.6 (13.7) | 78.9 (31.5) | 74.1 (30.5) | 84.1 (34.3) | 75.8 (32.1) | 53.1 (20.7) |
| High ARM | 26.0 (9.6) | 23.3 (9.7) |
27.4 (10.3) | 24.8 (9.7) | 24.2 (10.5) | 55.4 (19.7) | 51.2 (19.9) | 58.2 (21.2) | 51.4 (21.1) | 53.1 (20.7) |
| Low ARM | 44.3 (9.4) | 41.8 (10.2) |
46.1 (8.9) |
41.6 (9.6) | 42.2 (10.2) |
100.1 (24.1) | 94.9 (22.6) | 107.4 (26.2) | 97.9 (23.1) | 98.9 (24.1) |
| ARM with urological malf | 26.9 (8.9) | 23.9 (8.7) | 28.2 (10.2) | 25.0 (8.7) | 25.1 (9.2) |
59.9 (26.3) | 55.1 (26.2) | 63.3 (27.5) | 56.0 (27.7) | 57.7 (27.8) |
| ARM with spinal malf | 20.1 (5.0) | 17.3 (5.3) | 21.3 (6.1) |
19.1 (5.7) | 18.6 (7.1) |
42.6 (12.1) | 38.4 (12.2) | 44.6 (13.6) | 38.6 (14.7) | 40.0 (14.3) |
| p | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 | < 0.005 |
| Type of ARM |
Lenght HPZ cm Mean (SD) |
Asimmetry > 20% (n/%) |
Duration of contraction < 10 sec (n/%) |
Dyssynergy (n/%) |
RAIR present (n/%) |
| Total pts | 1.9(0.6) | 11/40 | 13/40 | 19/40 | 11/40 |
| High ARM | 1.6(0.5) | 9/19 | 12/19 | 11/19 | 9/19 |
| Low ARM | 2.2(0.5) | 2/21 | 1/21 | 8/21 | 20/21 |
| ARM with urological malf | 1.7(0.48) | 7/16 | 10/16 | 11/16 | 8/16 |
| ARM with spinal malf | 1.4(0.5) | 9/11 | 10/11 | 6/11 | 1/11 |
| p |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- King SK, Krois W, Lacher M, et al. Optimal management of the newborn with an anorectal malformation and evaluation of their continence potential. Semin Pediatr Surg. 2020 Dec;29(6):150996. [CrossRef]
- Masi P, Miele E, Staiano A. Pediatric anorectal disorders. Gastroenterol Clin North Am. 2008 Sep;37(3):709-30, x. [CrossRef]
- Rintala RJ, Pakarinen MP. Imperforate anus: long- and short-term outcome. Semin Pediatr Surg. 2008 May;17(2):79-89. [CrossRef]
- Bischoff A, Levitt MA, Peña A. Update on the management of anorectal malformations. Pediatr Surg Int. 2013 Sep;29(9):899-904. [CrossRef]
- Arnoldi R, Macchini F, Gentilino V, et al. Anorectal malformations with good prognosis: variables affecting the functional outcome. J Pediatr Surg. 2014 Aug;49(8):1232-6. [CrossRef]
- Pelizzo G, Canonica CPM, Destro F, et al. Anorectal Malformations: Ideal Surgery Timing to Reduce Incontinence and Optimize QoL. Children (Basel). 2023 Feb 18;10(2):404. [CrossRef]
- Upadhyaya VD, Bharti LK, Mishra A, et al. Constipation after surgery for anorectal malformations: Unrecognised problem until it is a problem. Afr J Paediatr Surg. 2021 Jan-Mar;18(1):67-71. [CrossRef]
- AbouZeid AA, Bayoumi MM, Abo El-Ela MM. Anorectal anomalies in the female: Highlights on surgical management. J Pediatr Surg. 2021 Sep;56(9):1570-1575. [CrossRef]
- Baxter KJ, Garza JM, Rollins MD, et al. Multi-institutional review of bowel management strategies in children with anorectal malformations. J Pediatr Surg. 2020 Dec;55(12):2752-2757. [CrossRef]
- Style CC, Hsu DM, Verla MA, et al. Development of a multidisciplinary colorectal and pelvic health program: Program implementation and clinical impact. J Pediatr Surg. 2020 Nov;55(11):2397-2402. [CrossRef]
- Nash O, Zobell S, Worst K. Bowel management for the treatment of fecal incontinence and constipation in patients with anorectal malformations. Seminars in Pediatric Surgery. 2020. [CrossRef]
- Tofft L, Klasson S, Salö M, et al. Patient-reported physical and psychosocial significance of abdominal scarring in anorectal malformations. J Pediatr Surg. 2022 Oct;57(10):348-353. [CrossRef]
- Van der Steeg HJJ, Van Rooij IALM, Iacobelli BD, et al. Bowel function and associated risk factors at preschool and early childhood age in children with anorectal malformation type rectovestibular fistula: An ARM-Net consortium study. J Pediatr Surg. 2022 Sep;57(9):89-96. [CrossRef]
- Chang PC, Duh YC, Fu YW, et al. How much do we know about constipation after surgery for anorectal malformation? Pediatr Neonatol. 2020 Feb;61(1):58-62. [CrossRef]
- Bischoff A, Levitt MA, Peña A. Bowel management for the treatment of pediatric fecal incontinence. Pediatr Surg Int. 2009 Dec;25(12):1027-42. [CrossRef]
- Levitt M, Peña A. Update on pediatric faecal incontinence. Eur J Pediatr Surg. 2009 Feb;19(1):1-9. [CrossRef]
- Levitt MA, Kant A, Peña A. The morbidity of constipation in patients with anorectal malformations. J Pediatr Surg. 2010 Jun;45(6):1228-33. [CrossRef]
- Levitt MA, Peña A. Pediatric fecal incontinence: a surgeon's perspective. Pediatr Rev. 2010 Mar;31(3):91-101. [CrossRef]
- Oh C, Youn JK, Han JW, et al. Analysis of Associated Anomalies in Anorectal Malformation: Major and Minor Anomalies. J Korean Med Sci. 2020 Apr 13;35(14):e98. [CrossRef]
- De Beaufort CMC, Van den Akker ACM, Kuijper CF, et al. The importance of screening for additional anomalies in patients with anorectal malformations: A retrospective cohort study. J Pediatr Surg. 2022 Nov 25:S0022-3468(22)00740-0. [CrossRef]
- Kruger P, Teague WJ, Khanal R, et al. Screening for associated anomalies in anorectal malformations: the need for a standardized approach. ANZ J Surg. 2019 Oct;89(10):1250-1252. [CrossRef]
- Skerritt C, DaJusta DG, Fuchs ME, et al. Long-term urologic and gynecologic follow-up and the importance of collaboration for patients with anorectal malformations. Semin Pediatr Surg. 2020 Dec;29(6):150987. [CrossRef]
- Duci M, Midrio P, Castagnetti M, et al. Urinary Tract Anomalies in Patients With Anorectal Malformations: The Role of Screening and Clinical Follow-Up. Urology. 2020 Sep;143:216-220. [CrossRef]
- Levitt MA, Patel M, Rodriguez G,et al. The tethered spinal cord in patients with anorectal malformations. J Pediatr Surg. 1997 Mar;32(3):462-8. [CrossRef]
- Kim SM, Chang HK, Lee MJ, Shim KW, Oh JT, Kim DS, et al. Spinal dysraphism with anorectal malformation: lumbosacral magnetic resonance imaging evaluation of 120 patients. J Pediatr Surg 2010;45:769e76. [CrossRef]
- Kyrklund K, Pakarinen MP, Taskinen S, et al. Spinal cord anomalies in patients with anorectal malformations without severe sacral abnormalities or meningomyelocele: outcomes after expectant, conservative management. J Neurosurg Spine. 2016 Dec;25(6):782-789. [CrossRef]
- Marı´a Fanjul, I. Samuk, P. Bagolan et al. Tethered cord in patients affected by anorectal malformations: a survey from the ARM-Net Consortium. Pediatr Surg Int (2017) 33:849–854. [CrossRef]
- Fernandez-Portilla E, Moreno-Acosta L, Dominguez-Muñoz A, et al. Functional outcome after cord detethering in fecally incontinent patients with anorectal malformations. Pediatr Surg Int. 2021 Apr;37(4):419-424. [CrossRef]
- Esposito G, Totonelli G, Morini F, et al. Predictive value of spinal bone anomalies for spinal cord abnormalities in patients with anorectal malformations. J Pediatr Surg. 2021 Oct;56(10):1803-1810. [CrossRef]
- Ahmad H, Halleran DR, Vardanyan J,et al. Functional fecal and urinary outcomes after sacrococcygeal mass resection in pediatric patients. J Pediatr Surg. 2021 Jun;56(6):1142-1147. [CrossRef]
- Chen Z, Zheng L, Zhang M, Zhang J, Kong R, Chen Y, Liang Z, Levitt MA, Wei CH, Wang Y. Sacral Curvature in Addition to Sacral Ratio to Assess Sacral Development and the Association With the Type of Anorectal Malformations. Front Pediatr. 2021 Oct 1;9:732524. https://doi.org/10.3389/fped.2021.732524. Erratum in: Front Pediatr. 2022 May 06;10:922448. PMID: 34660489; PMCID: PMC8519007.
- Bjoersum-Meyer T, Kaalby L, Lund L, et al. Long-term Functional Urinary and Sexual Outcomes in Patients with Anorectal Malformations-A Systematic Review. Eur Urol Open Sci. 2021 Feb 3;25:29-38. [CrossRef]
- Senel E, Demirbag S, Tiryaki T, et al. Postoperative anorectal manometric evaluation of patients with anorectal malformation. Pediatr Int. 2007 Apr;49(2):210-4. [CrossRef]
- Banasiuk M, Banaszkiewicz A, Dziekiewicz M, et al. Values From Three-dimensional High-resolution Anorectal Manometry Analysis of Children Without Lower Gastrointestinal Symptoms. Clin Gastroenterol Hepatol. 2016 Jul;14(7):993-1000.e3. [CrossRef]
- Bjørsum-Meyer T, Christensen P, Jakobsen MS, et al. Correlation of anorectal manometry measures to severity of fecal incontinence in patients with anorectal malformations - a cross-sectional study. Sci Rep. 2020 Apr 7;10(1):6016. [CrossRef]
- Ambartsumyan L, Rodriguez L, Morera C, et al. Longitudinal and radial characteristics of intra-anal pressures in children using 3D high-definition anorectal manometry: new observations. Am J Gastroenterol. 2013 Dec;108(12):1918-28. [CrossRef]
- Holschneider, A.; Hutson, J.; Peña, A.; Beket, E.; Chatterjee, S.; Coran, A.; Davies, M.; Georgeson, K.; Grosfeld, J.; Gupta, D.; et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J. Pediatr. Surg. 2005, 40, 1521–1526. [Google Scholar] [CrossRef] [PubMed]
- Levitt, M.A.; Pena, A. Imperforate Anus and Cloacal Malformations. In Aschcraft’s Pediatric Surgery, 6th ed.; Holcomb, G.W., III, Murphy, J.P., St Peter, S.D., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Di Pace MR, Catalano P, Caruso AM et al. Is rectal disimpact always necessary in children with chronic constipation? Evaluation with pelvic ultrasound. Pediatr Surg Int 2010; 26:601–606. [CrossRef]
- Rintala R., J. , Lindahl H et al. Is normal bowel function possible after repair of intermediate and high anorectal malformations ?. Journal of Pediatric Surgery 1995; vol. 30 (3): 491–49. [CrossRef]
- Caruso AM, Milazzo MPM, Bommarito D et al. Advanced management protocol of Transanal Irrigation in order to improve the outcome of pediatric patients with fecal incontinence Children 2021; dec11: 8(12):1174. [CrossRef]
- Roupakias S, Sinopidis X. Pelvic Floor Muscles Contribution in Surgical Outcome of Children with High-type Anorectal Malformations. Prague Med Rep. 2021;122(3):191-200. [CrossRef]
- Feil P, Krois W, Weber M, et al. Low muscle volume of the anal sphincter complex: A novel prognostic factor in children with anorectal malformations? J Pediatr Surg. 2022 Aug;57(8):1467-1472. [CrossRef]
- Lim IIP, Cushing CC, Jenkins T, et al. Prospective quality of life outcomes in pediatric fecal incontinence following bowel management. J Pediatr Surg. 2021 Aug;56(8):1459-1464. https://doi.org/10.1016/j.jpedsurg.2021.04.025. [CrossRef]
- Deng C. Re: role of urodynamics in male patients of high-anorectal malformations: a prospective study. Pediatr Surg Int. 2021 Aug;37(8):1149-1150. [CrossRef]
- Mert M, Sayan A, Köylüoğlu G. Comparing the fecal continence scores of patients with anorectal malformation with anorectal manometric findings. Pediatr Surg Int. 2021 Aug;37(8):1013-1019. [CrossRef]
- Kumar S, Al Ramadan S, Gupta V, et al. Use of anorectal manometry for evaluation of postoperative results of patients with anorectal malformation: a study from Kuwait. J Pediatr Surg. 2010 Sep;45(9):1843-8. [CrossRef]
- Kyrklund K, Pakarinen MP, Rintala RJ. Manometric findings in relation to functional outcomes in different types of anorectal malformations. J Pediatr Surg. 2017 Apr;52(4):563-568. [CrossRef]
- Keshtgar AS, Athanasakos E, Clayden GS, et al. Evaluation of outcome of anorectal anomaly in childhood: the role of anorectal manometry and endosonography. Pediatr Surg Int. 2008 Aug;24(8):885-92. [CrossRef]
- Bhat NA, Grover VP, Bhatnagar V. Manometric evaluation of postoperative patients with anorectal anomalies. Indian J Gastroenterol. 2004 Nov-Dec;23(6):206-8.
- Emblem R, Mørkrid L, Bjørnland K. Anal endosonography is useful for postoperative assessment of anorectal malformations. J Pediatr Surg. 2007 Sep;42(9):1549-54. [CrossRef]
- Wang Z, Hu L, Jin X, et al. Evaluation of postoperative anal functions using endoanal ultrasonography and anorectal manometry in children with congenital anorectal malformations. J Pediatr Surg. 2016 Mar;51(3):416-20. [CrossRef]
- Caldaro T, Romeo E, De Angelis P, et al. Three-dimensional endoanal ultrasound and anorectal manometry in children with anorectal malformations: new discoveries. J Pediatr Surg. 2012 May;47(5):956-63. [CrossRef]
- Desai SN, Choudhury H, Joshi P, et al. Magnetic resonance imaging evaluation after anorectal pull-through surgery for anorectal malformations: a comprehensive review. Pol J Radiol. 2018 Jul 11;83:e348-e352. [CrossRef]
- Bjørsum-Meyer T, Christensen P, Baatrup G, et al. Magnetic resonance imaging of the anal sphincter and spine in patients with anorectal malformations after posterior sagittal anorectoplasty: a late follow-up cross-sectional study. Pediatr Surg Int. 2021 Jan;37(1):85-91. [CrossRef]
- Husberg B, Rosenborg M, Frenckner B. Magnetic resonance imaging of anal sphincters after reconstruction of high or intermediate anorectal anomalies with posterior sagittal anorectoplasty and fistula-preserving technique. J Pediatr Surg. 1997 Oct;32(10):1436-42. [CrossRef]
- Fukuya T, Honda H, Kubota M, et al. Postoperative MRI evaluation of anorectal malformations with clinical correlation. Pediatr Radiol. 1993;23(8):583-6. [CrossRef]
- Morandi A, Borzani I, Macchini F, et al. Correlation between magnetic resonance imaging findings after posterior sagittal anorectoplasty for anorectal malformations and the clinical outcome: Preliminary report. J Pediatr Surg. 2016 Nov;51(11):1859-1863. [CrossRef]
- Caruso AM, Catalano P, Li Voti G, et al. Prognostic evaluation of biofeedback response in patients treated for anorectal malformation. J Pediatr Surg. 2015 Oct;50(10):1648-52. [CrossRef]
- Cheeney G, Remes-Troche JM, Attaluri A, Rao SS. Investigation of anal motor characteristics of the sensorimotor response (SMR) using 3-D anorectal pressure topography. Am J Physiol Gastrointest Liver Physiol. 2011;300(2):G236-G240.
- Liu, J. et al. Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am. J. Gastroenterol. 101, 1092–7 (2006).
- Li, Y. , Yang, X., Xu, C., Zhang, Y. & Zhang, X. Normal values and pressure morphology for three-dimensional high-resolution anorectal manometry of asymptomatic adults: a study in 110 subjects. Int. J. Colorectal Dis. 28, 1161–68 (2013).
- Padda BS, Jung SA, Pretorius D, Nager CW, Den-Boer D, Mittal RK. Effects of pelvic floor muscle contraction on anal canal pressure. Am J Physiol Gastrointest Liver Physiol. 2007;292(2):G565-G571.
- Raizada V, Mittal RK. Pelvic floor anatomy and applied physiology. Gastroenterol Clin North Am. 2008;37(3):493-509, vii.
- Liu J, Guaderrama N, Nager CW, Pretorius DH, Master S, Mittal RK. Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am J Gastroenterol. 2006;101(5):1092-1097.
- Ambartsumyan L, Shaffer M, Carlin K, et al. Comparison of longitudinal and radial characteristics of intra-anal pressures using 3D high-definition anorectal manometry between children with anoretal malformations and functional constipation. Neurogastroenterol Motil. 2021 Feb;33(2):e13971. [CrossRef]
- Makosiej R, Makosiej A, Bossowski A, et al. Dyssynergic Defecation and Anal Sphincter Disorders in Children in High-Resolution Anorectal Manometry Investigation. J Pediatr Gastroenterol Nutr. 2020 Oct;71(4):484-490. [CrossRef]
- Bjørsum-Meyer T, Christensen P, Baatrup G, et al. Dyssynergic patterns of defecation in constipated adolescents and young adults with anorectal malformations. Sci Rep. 2020 Nov 12;10(1):19673. [CrossRef]
- Gupta CR, Bhoy T, Mohta A, et al. Comparison of clinical outcome and anal manometry following laparoscopic-assisted anorectoplasty and posterior sagittal anorectoplasty in patients with high and intermediate anorectal malformation: A randomised controlled trial. Afr J Paediatr Surg. 2022 Jul-Sep;19(3):160-163. [CrossRef]
- Pathak M, Saxena AK. Postoperative "complications" following laparoscopic-assisted anorectoplasty: A systematic review. Pediatr Surg Int. 2020 Nov;36(11):1299-1307. [CrossRef]
- K.J. Baxter, J.M. K.J. Baxter, J.M. Garza, M.D. Rollins, et al., Multi-institutional review of bowel management strategies in children with anorectal malformations, Journal of Pediatric Surgery (2020), doi.org/10.1016/j.jpedsurg.2020.04.023on Day Month Year).
| Anatomic parameter | Score 0 | Score 1 |
| Perineal and buttock trophism | poor | good |
| Anal folds | ipoplasic | normal |
| Scrotum/fornix- anus distance | normal | short or long |
| Lateral deviation of neoanus | present | absent |
| Mucosal anal prolaps | present | absent |
| Perineal scar | good | ugly |
| Perianal lesions | present | absent |
| Sacral anomalies | present | absent |
| Intergluteal line | dysmorphic | normal |
| Dyscromic or fluff presacral | Present | absent |
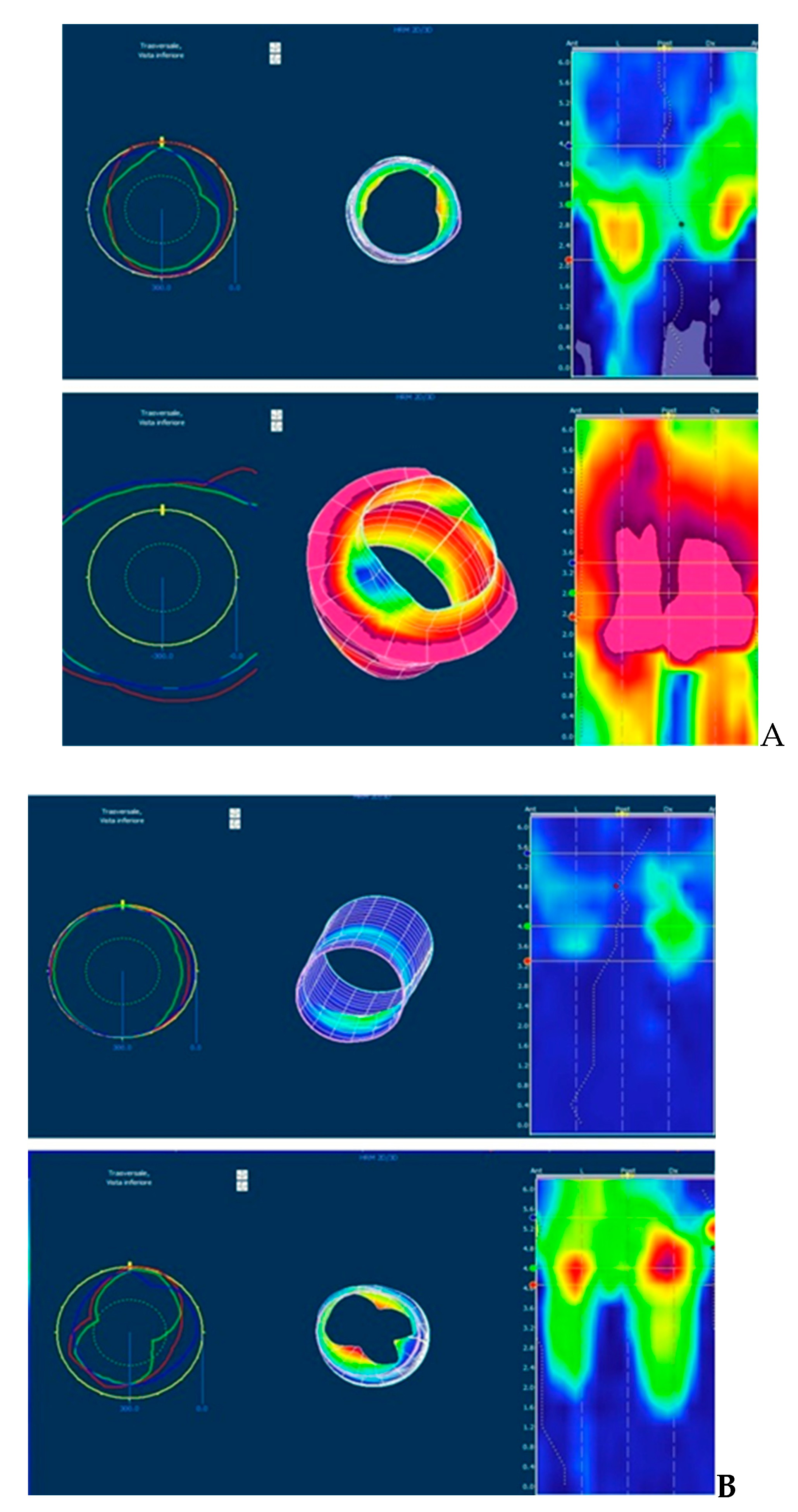
| HRM parameter | Score 0 | Score 1 |
| Lenght of HPZ (cm) | < 1.5 |
|
| ARP (mmHg) | < 50 | >50 |
| Sphincter asimmetry (%) |
|
< 20% |
| ASP ( mmHg) | < 40 |
|
| Duration of MVC (sec) | < 10 |
|
| Dyssinergic evacuation | yes | absent |
| Rectal sensitivity/RAIR | Altered/absent | Normal/present |
| 3D spatial image | Uneven cylinder | Uniform cylinder |
| Variable | High ARM | Low ARM | Tot | P | |
| sex | M | 12 | 15 | 27 | 0.738 |
| F | 7 | 6 | 13 | ||
| tot | 19 | 21 | 40 | ||
| Age (years) | 8.8 ± 2.8 | 8.1± 3.1 | 0.47 | ||
| Spinal malformation | 9 | 2 | 11 | 0.012 | |
| Urological malformation | 13 | 3 | 16 | < 0.05 | |
| Other associated anomalies | 3 | 2 | 5 | 0.65 | |
| Colostomy | 13 | 0 | 13 | < 0.05 | |
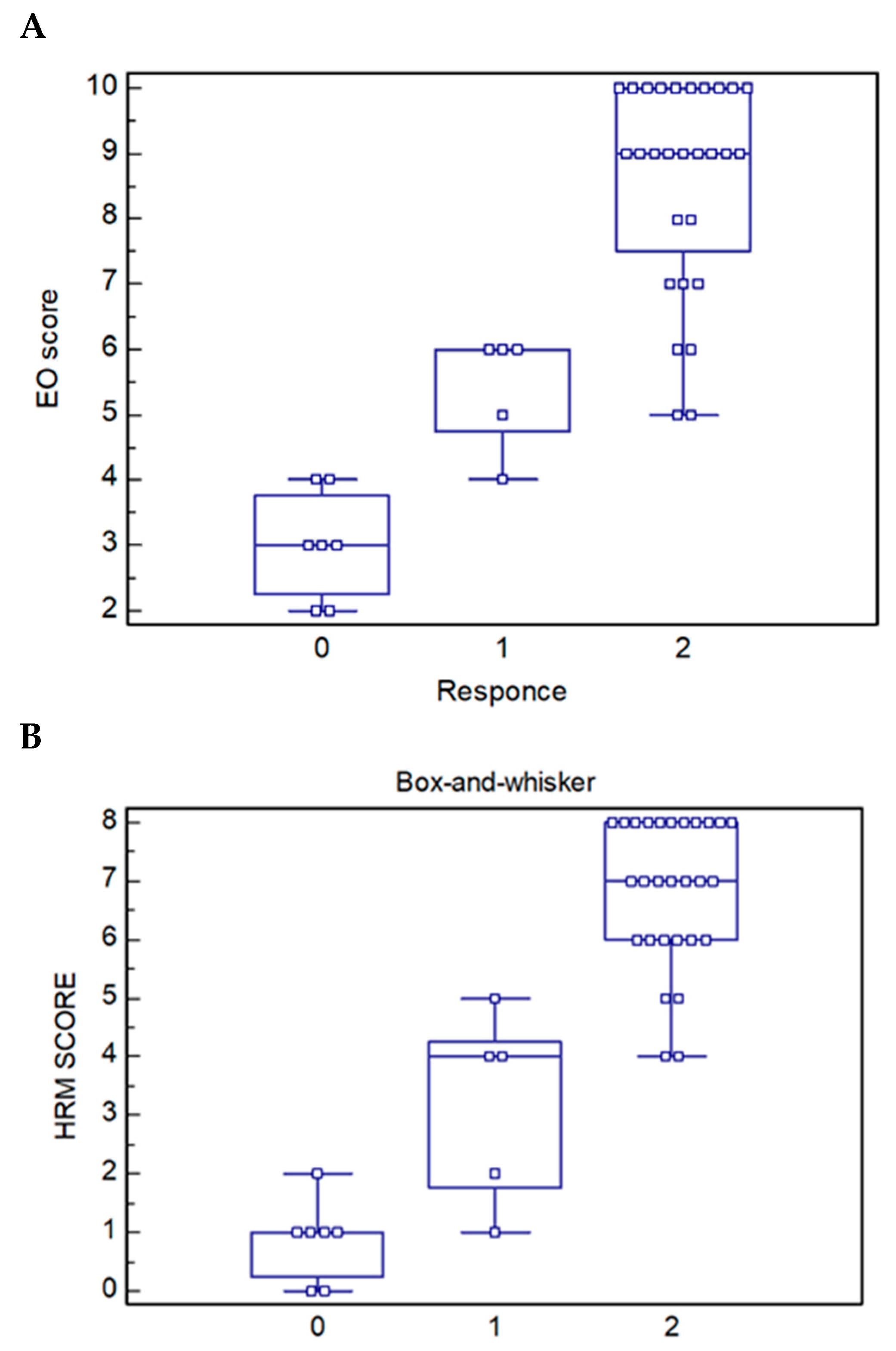
| High ARM | Low ARM |
ARM with Uro Vs ARM without Uro |
ARM with spinal Vs ARM without spinal |
p | |
| Parameter | |||||
| Anatomical score (mean) | 5.05±2.0 | 9.1± 1.1 | 5.5 ± 2.4 8.3 ± 2.1 p .00 |
3.8 ± 1.4 8.4 ± 1.6 p .00 |
<0.05 |
| Pre BM Rintala score | 5.7 ± 4.8 | 15.9± 2.6 | 14. 4 ± 5.3 6.6 ± 5.2 p .00 |
3.1 ± 3.2 14.0 ± 4.3 p .00 |
<0.05 |
| HRM score | 3.3 ± 2.4 | 7.1 ± 1.2 | 3.7 ± 2.5 6.3 ± 2.2 p .001 |
1.8 ± 1.5 6.6± 1.5 p .00 |
<0.05 |
| Post BM Rintala score | 12.3 ± 5.1 | 19.1± 1.8 | 13 .1 ± 5.1 17.7 ± 4.1 p .003 |
8.9 ± 3.1 18.5 ± 2.3 p .00 |
<0.05 |
| p | <0.05 | <0.05 | <0.05 | <0.05 |
| Type of ARM |
HRM score Mean (SD) |
Response to BM | p | ||
| poor | sufficient | excellent | |||
| High ARM | 19 PTS 3.32 (2.4) |
7 PTS 0.86(0.69) |
3 PTS 2.67(2.08) |
9 PTS 5.44(1.01) |
<0.0005 |
| Low ARM | 21 PTS 7.14(1.23) |
0 PTS | 2 4.0(0.0) |
19 PTS 7.47(0.70) |
<0.0005 |
| ARM with urological malformation | 16 PTS 3.75(2.59) |
5 PTS 0.60(0.55) |
3 PTS 3.67(1.52) |
8 PTS 5.75(1.39) |
<0.0005 |
| ARM with spinal malformation | 11 PTS 1.82(1.53) |
7 PTS 0.86(0.69) |
3 PTS 3.33(1.15) |
1 PTS 4.0(0.0) |
0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





