Submitted:
11 May 2023
Posted:
12 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Background of the Study
2.1. Water Quality of the Network in the Research Area
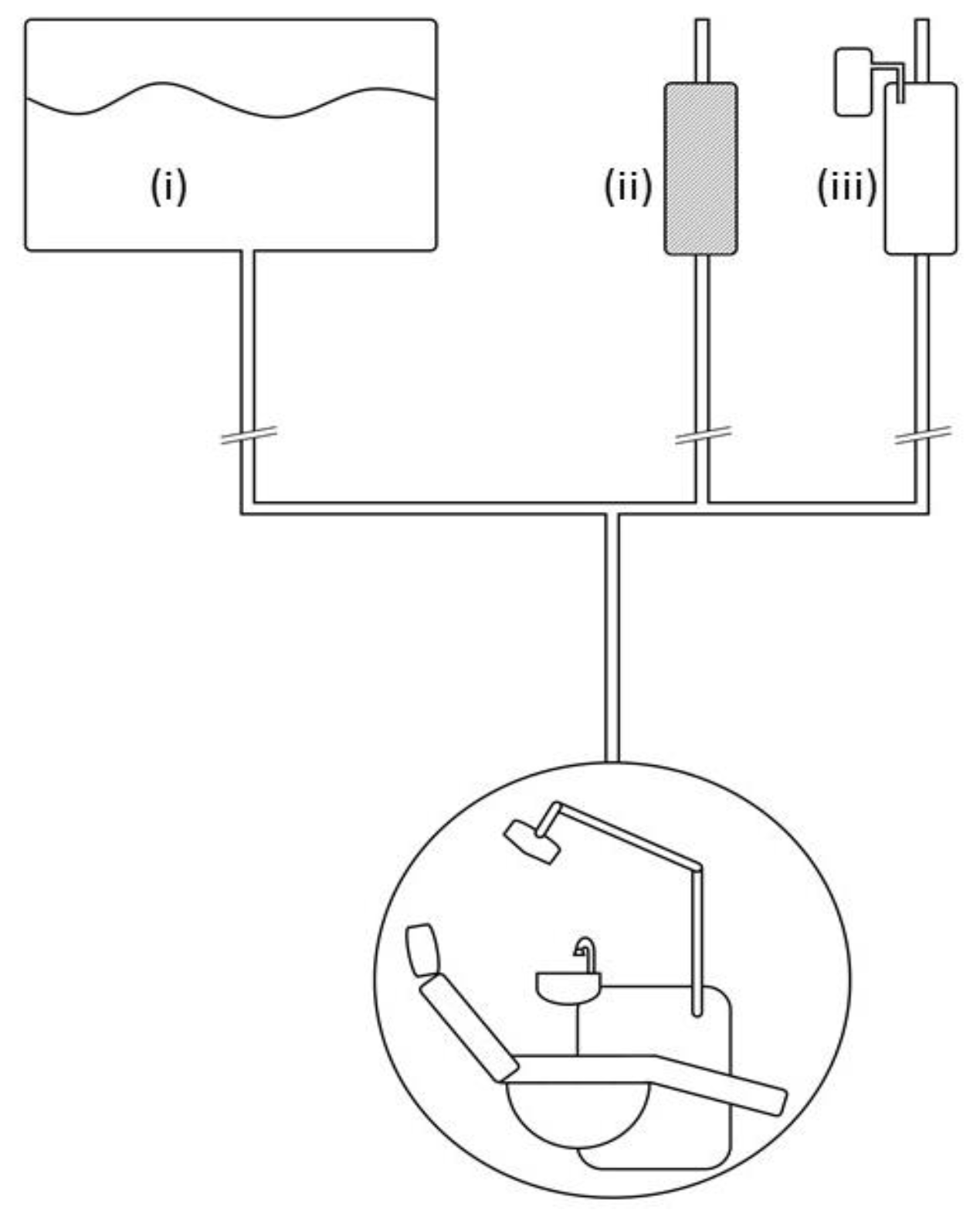
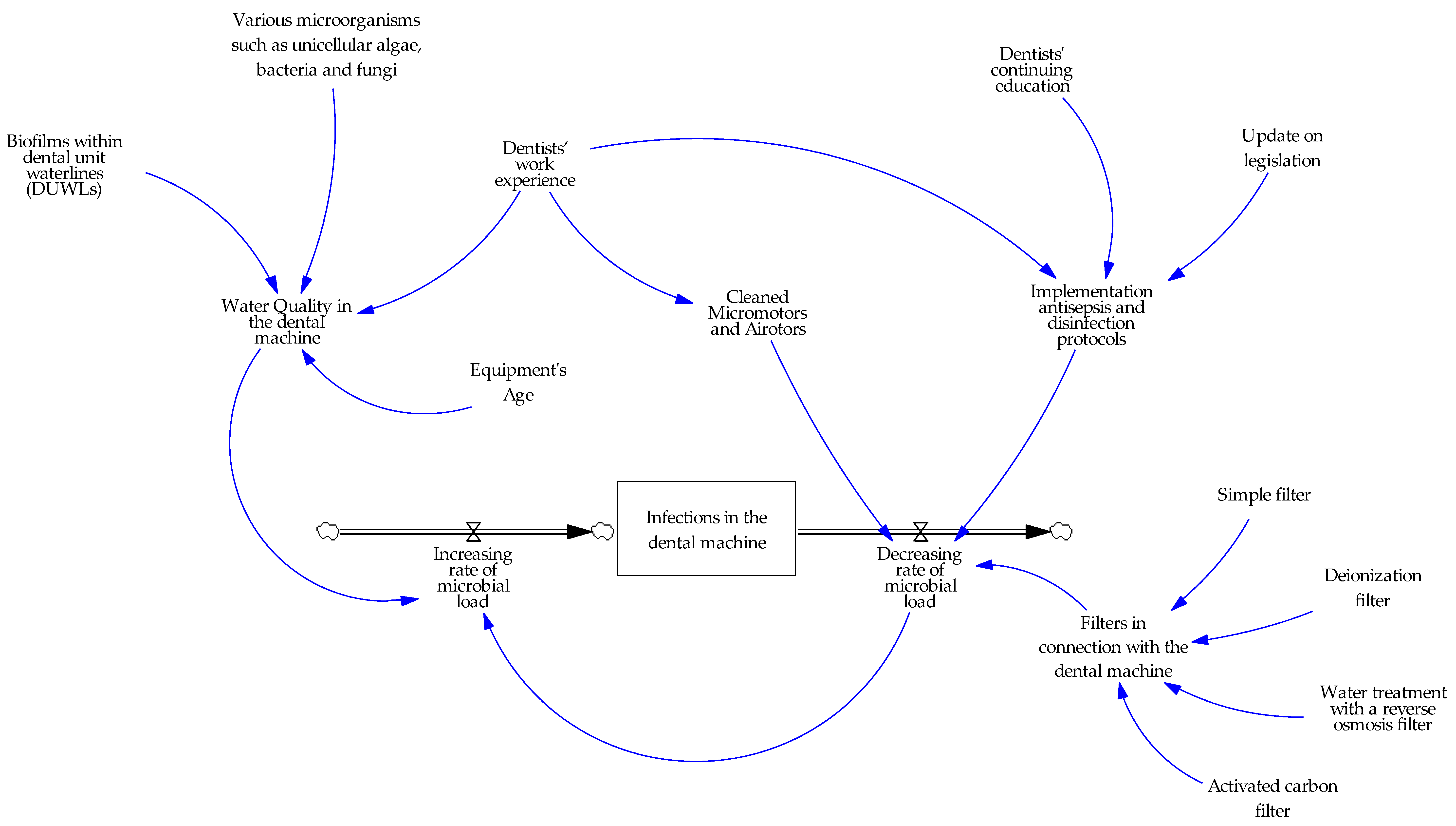
2.2. Water System of the Dental Unit
2.3. Water Quality in the Dental Unit
3. Materials and Methods
6. Statistical analysis
4. Results
The Sample
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Table with Descriptive Statistics of Dentistry Equipment and Water Quality Practices (N=206)
| N | % | ||
| Equipment How Old | 0-5 years | 43 | 20.90% |
| 6-10 years | 41 | 19.90% | |
| 11-20 years | 88 | 42.70% | |
| 21 years and older | 34 | 16.50% | |
| Has assistant | No | 109 | 52.90% |
| Yes | 97 | 47.10% | |
| Was informed when acquiring | No | 80 | 38.80% |
| Yes | 126 | 61.20% | |
| Interested in learning more | No | 44 | 21.40% |
| Yes | 162 | 78.60% | |
| Confident about water quality | No | 92 | 44.70% |
| Yes | 114 | 55.30% | |
| Performs microbiological test | No | 161 | 78.20% |
| Yes | 45 | 21.80% | |
| Continuous water supply system dental unit | No | 144 | 69.90% |
| Yes | 62 | 30.10% | |
| Continuous water supply system cutters | No | 137 | 66.50% |
| Yes | 69 | 33.50% | |
| Water supply to the dental unit | Water from public network | 130 | 65.00% |
| Distilled/Deionized water | 15 | 7.50% | |
| Water from a filter device directly connected to the supply | 55 | 27.50% | |
| Water supply to the cutters | Water from public network | 124 | 62.30% |
| Deionized/Distilled water | 22 | 11.10% | |
| Water from a filter device directly connected to the supply | 53 | 26.60% | |
| Supply to ultrasounds | Water from public network | 114 | 58.50% |
| Distilled/Deionized water | 31 | 15.90% | |
| Water from a filter device directly connected to the supply | 50 | 25.60% | |
| Has water filter | No | 91 | 44.20% |
| Yes | 115 | 55.80% | |
| Water filter replaced/cleaned | No filter/Don’t want to answer | 99 | 52.10% |
| every month | 5 | 2.60% | |
| every 6 months | 36 | 18.90% | |
| every 12 months | 21 | 11.10% | |
| every 2 years | 9 | 4.70% | |
| every 5 years + | 4 | 2.10% | |
| whenever there is a problem with the flow | 16 | 8.40% | |
| Knows the active substance of antisepticAntiseptic to the incisors (auto) | No | 148 | 71.80% |
| Yes | 58 | 28.20% | |
| No | 164 | 90.60% | |
| Antiseptic to the incisors (manually) | Yes | 17 | 9.40% |
| No | 155 | 85.60% | |
| Yes | 26 | 14.40% | |
| Antiseptic reservoir | No | 8 | 3.90% |
| Yes | 198 | 96.10% | |
| Has strong surgical suction | No | 11 | 5.30% |
| Yes | 195 | 94.70% | |
| SmallSalivary | between two patients | 78 | 39.60% |
| every few appointments (3-4) | 37 | 18.80% | |
| per day | 55 | 27.90% | |
| per week | 21 | 10.70% | |
| never before covid | 4 | 2.00% | |
| never again due to covid i let patients flush | 2 | 1.00% | |
| LargeSalivary | between two patients | 18 | 9.00% |
| every few appointments (3-4) | 23 | 11.50% | |
| per day | 89 | 44.50% | |
| per week | 57 | 28.50% | |
| per month | 6 | 3.00% | |
| Never | 7 | 3.50% | |
| SmallSuction | between two patients | 90 | 45.50% |
| every few appointments (3-4) | 30 | 15.20% | |
| per day | 53 | 26.80% | |
| per week | 14 | 7.10% | |
| per month | 5 | 2.50% | |
| Never | 6 | 3.00% | |
| LargeSuction | between two patients | 15 | 7.70% |
| every few appointments (3-4) | 24 | 12.20% | |
| per day | 84 | 42.90% | |
| per week | 58 | 29.60% | |
| per month | 7 | 3.60% | |
| Never | 8 | 4.10% | |
| LargeDentalMach | between two patients | 14 | 7.80% |
| every few appointments (3-4) | 13 | 7.30% | |
| per day | 56 | 31.30% | |
| per week | 54 | 30.20% | |
| per month | 16 | 8.90% | |
| Never | 26 | 14.50% | |
| DisinfSurfaces | between two patients | 189 | 92.20% |
| every few appointments (3-4) | 8 | 3.90% | |
| per day | 7 | 3.40% | |
| per week | 1 | 0.50% | |
| Annual maintenance | No | 76 | 38.40% |
| Yes | 122 | 61.60% | |
| Micromotors | 1 | 51 | 24.80% |
| 2 | 69 | 33.50% | |
| 3 | 24 | 11.70% | |
| 4 | 25 | 12.10% | |
| 5+ | 37 | 18.00% | |
| Airotors | 1 | 29 | 14.10% |
| 2 | 63 | 30.60% | |
| 3 | 27 | 13.10% | |
| 4 | 25 | 12.10% | |
| 5+ | 62 | 30.10% | |
| HandlesClean | Decontamination | 120 | 58.30% |
| Decontamination/Sterilization | 14 | 6.80% | |
| Sterilization | 36 | 17.50% | |
| Surface cleaning | 36 | 17.50% | |
| Has implantology motor | No | 128 | 62.40% |
| Yes | 77 | 37.60% | |
| Via suction vs central drain | No | 79 | 46.20% |
| Yes | 92 | 53.80% | |
| Has amagalm trap | No | 70 | 35.40% |
| Yes | 128 | 64.60% | |
| Has contract with sewage collection company | No | 82 | 41.80% |
| Yes | 114 | 58.20% | |
| Has contract amagalm removal | No | 141 | 73.40% |
| Yes | 51 | 26.60% | |
| Is informed about water quality legislation | No | 167 | 85.60% |
| Yes | 28 | 14.40% | |
| Time spent | no time | 5 | 2.40% |
| up to 2 hours per month | 57 | 27.70% | |
| up to 4 hours per month | 62 | 30.10% | |
| more than 4 hours | 82 | 39.80% | |
| Money spent | 0 euros per month | 8 | 3.90% |
| less than 25 euros per month | 44 | 21.40% | |
| 25-50 euros per month | 89 | 43.20% | |
| 51-75 euros per month | 38 | 18.40% | |
| more than 75 euros per month | 27 | 13.10% | |
| Environmentally friendly practices | a little bit | 28 | 15.40% |
| Satisfactorily | 85 | 46.70% | |
| Enough | 50 | 27.50% | |
| very much | 19 | 10.40% | |
| Implementation of disinfection protocol is my responsibility | No | 86 | 41.70% |
| Yes | 120 | 58.30% | |
| More strict after Covid-19 | No | 99 | 49.30% |
| Yes | 102 | 50.70% |
References
- Department of health. Environment and sustainability Health Technical Memorandum 07-04: Water management and water efficiency – best practice advice for the healthcare sector. Copyright 2013. Available online: http://www.nationalarchives.gov.uk/doc/open-government-licence/ (accessed on 15 March 2023).
- Facciolà, A.; Laganà, P.; Caruso, G. The COVID-19 pandemic and its implications on the environment. Environ. Res. 2021, 201, 111648–111648. [Google Scholar] [CrossRef] [PubMed]
- Lawler, O.K.; Allan, H.L.; Baxter, P.W.J.; Castagnino, R.; Tor, M.C.; E Dann, L.; Hungerford, J.; Karmacharya, D.; Lloyd, T.J.; López-Jara, M.J.; et al. The COVID-19 pandemic is intricately linked to biodiversity loss and ecosystem health. Lancet Planet. Heal. 2021, 5, e840–e850. [Google Scholar] [CrossRef] [PubMed]
- Marazziti, D.; Cianconi, P.; Mucci, F.; Foresi, L.; Chiarantini, I.; Della Vecchia, A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total. Environ. 2021, 773, 145182–145182. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.; Sarkis, J.; Hervani, A.A.; Helms, M.M. Redesigning Supply Chains using Blockchain-Enabled Circular Economy and COVID-19 Experiences. Sustain. Prod. Consum. 2020, 27, 10–22. [Google Scholar] [CrossRef] [PubMed]
- uropean Commision. Communication from the commission to the European Parliament, the council , the European economic and social committee and the committee of the regions. EU Biodiversity Strategy for 2030. Bringing nature back into our lives. Brussels, 20.5.2020. COM(2020) 380 final.
- Intergovernmental science-policy Plaform for Biodiversity and Ecosystem Services (IPBES) (2019), Summary for policymakers of the global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services, pp. 12-13, A.2.
- European Commission, DG Environment. Available online: http://ec.europa.eu/environment/water/index_en.htm (accessed on 15 March 2023).
- European Environmental Bureau. EEB position for a revised Urban Waste Water Directive. Available online: https://eeb.org/wp-content/uploads/2021/07/EEB-position-for-a-revised-UWWTD.pdf (accessed on 15 April 2023).
- European Parliament. Revision of the Urban Wastewater Treatment Directive. Available online: https://www.europarl.europa.eu/legislative-train/theme-a-european-green-deal/file-revision-of-the-urban-wastewater-treatment-directive-(refit).
- European Green Deal. Available online: https://www.consilium.europa.eu/en/policies/green-deal/#:~:text=The%20European%20Green%20Deal%20is%20a%20package%20of%20policy%20initiatives,a%20modern%20and%20competitive%20economy (accessed on 15 March 2023).
- CDC. Reduce Risk from Water. Available online: https://www.cdc.gov/hai/prevent/environment/water.html.
- World Economic Forum (2020). Nature Risk Rising: Why the Crisis Engulfing Nature Matters for Business and the Economy.
- European Environment Agency. Available online: http://www.eea.europa.eu/publications/european-waters-synthesis-2012.
- Leach, R. Water Management and IP Risk. Infection Control Today, 2023; 27 (3).
- Rezania, S.; Park, J.; Din, M.F.M.; Taib, S.M.; Talaiekhozani, A.; Yadav, K.K.; Kamyab, H. Microplastics pollution in different aquatic environments and biota: A review of recent studies. Mar. Pollut. Bull. 2018, 133, 191–208. [Google Scholar] [CrossRef]
- Dulsat-Masvidal, M.; Ciudad, C.; Infante, O.; Mateo, R.; Lacorte, S. Water pollution threats in important bird and biodiversity areas from Spain. J. Hazard. Mater. 2023, 448, 130938. [Google Scholar] [CrossRef]
- EYDAP Sustainable Development Report. (2021). Sustainable Development EYDAP SA. Athens. Available online: https://www.eydap.gr/userfiles/Presentations/presentations/EYDAP_CSR_2021_21x29-7CM_F13_WEB/index.html#page=1 (accessed on 15 March 2023).
- Preliminary plan for water resources. Available online: http://ec.europa.eu/environment/water/blueprint/index_en.htm (accessed on 20 March 2023).
- Facts and figures of the WFD. Available online: http://ec.europa.eu/environment/water/water-framework/facts_figures/index_en.htm.
- Water Information System for Europe (WISE). Available online: http://water.europa.eu/ (accessed on 20 March 2023).
- European Innovation Partnership on Water. Available online: http://ec.europa.eu/environment/water/innovationpartnership/ (accessed on 20 March 2023).
- Government Gazette. (2017, Σεπτέμβριος 19). Quality of water intended for human consumption in compliance with the provisions of the Directive 98/83/ΕΚ of the Council of the European Union of as amended by Directive (ΕΕ) 2015/1787 (L260, 7.10.2015). No. Sheet 3282, Τεύχος 2. 3 November.
- Joint Research Centre. Available online: http://ec.europa.eu/dgs/jrc/index.cfm?id=10 (accessed on 20 March 2023).
- Horizon 2020. Available online: http://ec.europa.eu/programmes/horizon2020/ (accessed on 20 March 2023).
- Council of the European Union. (2015, Oκτώβριος 27). Directive 98/83/ΕΚ of 3 November 1998 on the quality of water intended for human consumption. 0199. Available online: https://eur-lex.europa.eu/legal-content/EL/TXT/PDF/?uri=CELEX:01998L0083-20151027&from=EN (accessed on 20 March 2023).
- EU. Directorate-General for Environment. Proposal for Ecodesign for Sustainable Products Regulation. Annexes - Proposal for a Regulation establishing a framework for setting Ecodesign requirements for sustainable products and repealing Directive 2009/125/EC. Available online: https://environment.ec.europa.eu/publications/proposal-ecodesign-sustainable-products-regulation_en.
- Szymańska, J.; Sitkowska, J. Bacterial contamination of dental unit waterlines. Environ. Monit. Assess. 2012, 185, 3603–3611. [Google Scholar] [CrossRef]
- Yuan, Q.; Zhang, M.; Zhou, J. To Implement A Clear-Water Supply System for Fine-Sediment Experiment in Laboratories. Water 2019, 11, 2476. [Google Scholar] [CrossRef]
- Cicciu’, M.; Fiorillo, L.; Herford, A.S.; Crimi, S.; Bianchi, A.; D’Amico, C.; Laino, L.; Cervino, G. Bioactive Titanium Surfaces: Interactions of Eukaryotic and Prokaryotic Cells of Nano Devices Applied to Dental Practice. Biomedicines 2019, 7, 12. [Google Scholar] [CrossRef]
- Cicciù, M. Water Contamination Risks at the Dental Clinic. Biology 2020, 9, 43. [Google Scholar] [CrossRef]
- ntoniadou M, Tzoutzas I, Tzermpos F, Panis V, Maltezou H, Tseroni M, Madianos F. Infection control during COVID-19 outbreak in a university dental school. J Oral Hyg Health 2020, 8, 4.
- Cataldi, M.E.; Al Rakayan, S.; Arcuri, C.; Condò, R. DENTAL UNIT WASTEWATER, A CURRENT ENVIRONMENTAL PROBLEM: A SISTEMATIC REVIEW. Oral Implant. 2017, 10, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Innes, N.; Johnson, I.; Al-Yaseen, W.; Harris, R.; Jones, R.; Kc, S.; McGregor, S.; Robertson, M.; Wade, W.; Gallagher, J. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2020, 105, 103556–103556. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, J.-I.; Imazato, S. Autoclave sterilization of dental handpieces: A literature review. J. Prosthodont. Res. 2020, 64, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Tseroni, M.; Vorou, R.; Koutsolioutsou, A.; Antoniadou, M.; Tzoutzas, I.; Panis, V.; Tzermpos, F.; Madianos, P. Preparing dental schools to refunction safely during the COVID-19 pandemic: an infection prevention and control perspective. J. Infect. Dev. Ctries. 2021, 15, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, A.M.; Sartini, M.; Di Cave, D.; Casini, B.; Tuvo, B.; Cristina, M.L. Evaluation of Microbiological and Free-Living Protozoa Contamination in Dental Unit Waterlines. Int. J. Environ. Res. Public Heal. 2019, 16, 2648. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, A.M.; Sartini, M.; Cristina, M.L. Microbial Contamination of Dental Unit Waterlines and Potential Risk of Infection: A Narrative Review. Pathogens 2020, 9, 651. [Google Scholar] [CrossRef]
- Senpuku, H.; Fukumoto, M.; Uchiyama, T.; Taguchi, C.; Suzuki, I.; Arikawa, K. Effects of Extraoral Suction on Droplets and Aerosols for Infection Control Practices. Dent. J. 2021, 9, 80. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Centers for disease control and prevention. Summary of Infection Prevention Practices in Dental Settings. Basic Expectations for Safe Care. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; October 2016. Available online: https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf (accessed on 20 March 2023).
- Leoni, E.; Dallolio, L.; Stagni, F.; Sanna, T.; D’Alessandro, G.; Piana, G. Impact of a Risk Management Plan on Legionella Contamination of Dental Unit Water. Int. J. Environ. Res. Public Heal. 2015, 12, 2344–2358. [Google Scholar] [CrossRef]
- Dallolio, L.; Scuderi, A.; Rini, M.S.; Valente, S.; Farruggia, P.; Sabattini, M.A.B.; Pasquinelli, G.; Acacci, A.; Roncarati, G.; Leoni, E. Effect of Different Disinfection Protocols on Microbial and Biofilm Contamination of Dental Unit Waterlines in Community Dental Practices. Int. J. Environ. Res. Public Heal. 2014, 11, 2064–2076. [Google Scholar] [CrossRef] [PubMed]
- Shajahan, I.F.; Kandaswamy, D.; Srikanth, P.; Narayana, L.L.; Selvarajan, R. Dental unit waterlines disinfection using hypochlorous acid-based disinfectant. J. Conserv. Dent. 2016, 19, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Ditommaso, S.; Giacomuzzi, M.; Ricciardi, E.; Zotti, C.M. Efficacy of a Low Dose of Hydrogen Peroxide (Peroxy Ag+) for Continuous Treatment of Dental Unit Water Lines: Challenge Test with Legionella pneumophila Serogroup 1 in a Simulated Dental Unit Waterline. Int. J. Environ. Res. Public Heal. 2016, 13, 745. [Google Scholar] [CrossRef] [PubMed]
- Lizzadro, J.; Mazzotta, M.; Girolamini, L.; Dormi, A.; Pellati, T.; Cristino, S. Comparison between Two Types of Dental Unit Waterlines: How Evaluation of Microbiological Contamination Can Support Risk Containment. Int. J. Environ. Res. Public Heal. 2019, 16, 328. [Google Scholar] [CrossRef] [PubMed]
- Noopan, S.; Unchui, P.; Techotinnakorn, S.; Ampornaramveth, R.S. Plasma Sterilization Effectively Reduces Bacterial Contamination in Dental Unit Waterlines. Int. J. Dent. 2019, 2019, 1–6. [Google Scholar] [CrossRef]
- Han, P.; Li, H.; Walsh, L.J.; Ivanovski, S. Splatters and Aerosols Contamination in Dental Aerosol Generating Procedures. Appl. Sci. 2021, 11, 1914. [Google Scholar] [CrossRef]
- Fiorillo, L. Conscious Sedation in Dentistry. Medicina 2019, 55, 778. [Google Scholar] [CrossRef]
- Walker, J.T.; Bradshaw, D.J.; Bennett, A.M.; Fulford, M.R.; Martin, M.V.; Marsh, P.D. Microbial Biofilm Formation and Contamination of Dental-Unit Water Systems in General Dental Practice. Appl. Environ. Microbiol. 2000, 66, 3363–3367. [Google Scholar] [CrossRef]
- Walker, J.T.; Bradshaw, D.J.; Fulford, M.R.; Marsh, P.D. Microbiological Evaluation of a Range of Disinfectant Products To Control Mixed-Species Biofilm Contamination in a Laboratory Model of a Dental Unit Water System. Appl. Environ. Microbiol. 2003, 69, 3327–3332. [Google Scholar] [CrossRef]
- Yabune, T.; Imazato, S.; Ebisu, S. Assessment of Inhibitory Effects of Fluoride-Coated Tubes on Biofilm Formation by Using the In Vitro Dental Unit Waterline Biofilm Model. Appl. Environ. Microbiol. 2008, 74, 5958–5964. [Google Scholar] [CrossRef]
- Costa, D.; Girardot, M.; Bertaux, J.; Verdon, J.; Imbert, C. Efficacy of dental unit waterlines disinfectants on a polymicrobial biofilm. Water Res. 2016, 91, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Tuvo, B.; Totaro, M.; Cristina, M.L.; Spagnolo, A.M.; Di Cave, D.; Profeti, S.; Baggiani, A.; Privitera, G.; Casini, B. Prevention and Control of Legionella and Pseudomonas spp. Colonization in Dental Units. Pathogens 2020, 9, 305. [Google Scholar] [CrossRef] [PubMed]
- Hoogenkamp, M.A.; Brandt, B.W.; Laheij, A.M.; de Soet, J.J.; Crielaard, W. The microbiological load and microbiome of the Dutch dental unit; ‘please, hold your breath’. Water Res. 2021, 200, 117205. [Google Scholar] [CrossRef] [PubMed]
- Gawlik, BM, Easton P, Koop S, Van Leeuwen K, Elelman R. (eds.), 2017, Urban Water Atlas for Europe. European Commission, Publications Office of the European Union, Luxembourg. 160 pp. [CrossRef]
- EYDAP SA. (n.d.). Available online: https://www.eydap.gr/ (accessed on 20 March 2023).
- Engsomboon, N.; Pachimsawat, P.; Thanathornwong, B. Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study. Dent. J. 2022, 10, 142. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, Z.; Ma, H.; Hursthouse, A.S. Removal of Manganese(II) from Acid Mine Wastewater: A Review of the Challenges and Opportunities with Special Emphasis on Mn-Oxidizing Bacteria and Microalgae. Water 2019, 11, 2493. [Google Scholar] [CrossRef]
- Engelmann, C.; Schmidt, L.; Werth, C.J.; Walther, M. Quantification of Uncertainties from Image Processing and Analysis in Laboratory-Scale DNAPL Release Studies Evaluated by Reflective Optical Imaging. Water 2019, 11, 2274. [Google Scholar] [CrossRef]
- Yoon, H.Y.; Lee, S.Y. Susceptibility of bacteria isolated from dental unit waterlines to disinfecting chemical agents. J. Gen. Appl. Microbiol. 2018, 64, 269–275. [Google Scholar] [CrossRef]
- Ajami, B.; Ghazvini, K.; Movahhed, T.; Ariaee, N.; Shakeri, M.; Makarem, S. Contamination of a Dental Unit Water Line System by Legionella Pneumophila in the Mashhad School of Dentistry in 2009. 2012, 14, 376–378.
- Cervino, G.; Fiorillo, L.; Monte, I.P.; De Stefano, R.; Laino, L.; Crimi, S.; Bianchi, A.; Herford, A.S.; Biondi, A.; Cicciù, M. Advances in Antiplatelet Therapy for Dentofacial Surgery Patients: Focus on Past and Present Strategies. Materials 2019, 12, 1524. [Google Scholar] [CrossRef]
- Mills, S.E. THE DENTAL UNIT WATERLINE CONTROVERSY: DEFUSING THE MYTHS, DEFINING THE SOLUTIONS. J. Am. Dent. Assoc. 2000, 131, 1427–1441. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Laino, L.; Herford, A.S.; Lauritano, F.; Giudice, G.L.; Famà, F.; Santoro, R.; Troiano, G.; Iannello, G.; et al. Oral Health Impact Profile in Celiac Patients: Analysis of Recent Findings in a Literature Review. Gastroenterol. Res. Pr. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Gawish, S.; Abbass, A.; Abaza, A. Occurrence and biofilm forming ability of Pseudomonas aeruginosa in the water output of dental unit waterlines in a dental center in Alexandria, Egypt. GERMS 2019, 9, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Pouralibaba, F.; Balaei, E.; Kashefimehr, A. Evaluation of Gram Negative Bacterial Contamination in Dental Unit Water Supplies in a University Clinic in Tabriz, Iran. J Dent Res Dent Clin Dent Prospect 2011, 5, 94–97. [Google Scholar] [CrossRef]
- Giacomuzzi, M.; Zotti, C.M.; Ditommaso, S. Colonization of Dental Unit Waterlines by Helicobacter pylori: Risk of Exposure in Dental Practices. Int. J. Environ. Res. Public Heal. 2019, 16, 2981. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, A.M.; Campos-Bijit, V.; Di Francesco, F.; Schwarz, F.; Cafferata, E.A.; Vernal, R. Electrolyzed water for the microbiologic control in the pandemic dental setting: a systematic review. BMC Oral Heal. 2022, 22, 1–43. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Smith, G.; Smith, A. Biofouling of surgical power tools during routine use. J. Hosp. Infect. 2015, 90, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Kauppinen, A.; Pitkänen, T.; Al-Hello, H.; Maunula, L.; Hokajärvi, A.-M.; Rimhanen-Finne, R.; Miettinen, I.T. Two Drinking Water Outbreaks Caused by Wastewater Intrusion Including Sapovirus in Finland. Int. J. Environ. Res. Public Heal. 2019, 16, 4376. [Google Scholar] [CrossRef] [PubMed]
- Pasquarella, C.; Veronesi, L.; Napoli, C.; Castiglia, P.; Liguori, G.; Rizzetto, R.; Torre, I.; Righi, E.; Farruggia, P.; Tesauro, M.; et al. Microbial environmental contamination in Italian dental clinics: A multicenter study yielding recommendations for standardized sampling methods and threshold values. Sci. Total. Environ. 2012, 420, 289–299. [Google Scholar] [CrossRef]
- Zhang, Y.; Ping, Y.; Zhou, R.; Wang, J.; Zhang, G. High throughput sequencing-based analysis of microbial diversity in dental unit waterlines supports the importance of providing safe water for clinical use. J. Infect. Public Heal. 2018, 11, 357–363. [Google Scholar] [CrossRef]
- Mazari, W.; Boucherit-Otmani, Z.; El Haci, I.A.; Ilahi, A.; Boucherit, K. Risk assessment for the spread of Candida sp. in dental chair unit waterlines using molecular techniques. Int. Dent. J. 2020, 68, 386–392. [Google Scholar] [CrossRef]
- Fiorillo, L. We Do Not Eat Alone: Formation and Maturation of the Oral Microbiota. Biology 2020, 9, 17. [Google Scholar] [CrossRef]
- Adedoja, O.S.; Hamam, Y.; Khalaf, B.; Sadiku, R. Development of a Contaminant Distribution Model for Water Supply Systems. Water 2019, 11, 1510. [Google Scholar] [CrossRef]
- Watanabe, A.; Tamaki, N.; Yokota, K.; Matsuyama, M.; Kokeguchi, S. Monitoring of bacterial contamination of dental unit water lines using adenosine triphosphate bioluminescence. J. Hosp. Infect. 2016, 94, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Baudet, A.; Lizon, J.; Martrette, J.-M.; Camelot, F.; Florentin, A.; Clément, C. Efficacy of BRS® and Alpron®/Bilpron® Disinfectants for Dental Unit Waterlines: A Six-Year Study. Int. J. Environ. Res. Public Heal. 2020, 17, 2634. [Google Scholar] [CrossRef] [PubMed]
- Putnins, E.E.; Di Giovanni, D.; Bhullar, A.S. Dental Unit Waterline Contamination and Its Possible Implications During Periodontal Surgery. J. Periodontol. 2001, 72, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Toomarian, L.; Rikhtegaran, S.; Sadighi, M.; Oskoee, S.S.; Oskoee, P.A. Contamination of Dental Unit Water and Air Outlets Following Use of Clean Head System and Conventional Handpieces. J Dent Res Dent Clin Dent Prospect 2007, 1, 43–47. [Google Scholar] [CrossRef]
- Laino, L.; Cicciù, M.; Fiorillo, L.; Crimi, S.; Bianchi, A.; Amoroso, G.; Monte, I.P.; Herford, A.S.; Cervino, G. Surgical Risk on Patients with Coagulopathies: Guidelines on Hemophiliac Patients for Oro-Maxillofacial Surgery. Int. J. Environ. Res. Public Health 2019, 16, 1386. [Google Scholar] [CrossRef]
- Takenaka, S.; Sotozono, M.; Yashiro, A.; Saito, R.; Kornsombut, N.; Naksagoon, T.; Nagata, R.; Ida, T.; Edanami, N.; Noiri, Y. Efficacy of Combining an Extraoral High-Volume Evacuator with Preprocedural Mouth Rinsing in Reducing Aerosol Contamination Produced by Ultrasonic Scaling. Int. J. Environ. Res. Public Heal. 2022, 19, 6048. [Google Scholar] [CrossRef]
- Acosta-Gio, E.; Bednarsh, H.; Cuny, E.; Eklund, K.; Mills, S.; Risk, D. Sterilization of dental handpieces. Am. J. Infect. Control. 2017, 45, 937–938. [Google Scholar] [CrossRef]
- Walker, J.; Marsh, P. Microbial biofilm formation in DUWS and their control using disinfectants. J. Dent. 2007, 35, 721–730. [Google Scholar] [CrossRef]
- Offner, D.; Fioretti, F.; Musset, A.-M. Contamination of dental unit waterlines: assessment of three continuous water disinfection systems. BDJ Open 2016, 2, 16007. [Google Scholar] [CrossRef]
- Pawar, A.; Garg, S.; Mehta, S.; Dang, R. Breaking the Chain of Infection: Dental Unit Water Quality Control. J. Clin. Diagn. Res. 2016, 10, ZC80–4. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Mittal, S.; Kaur, P. Dental unit waterline management: historical perspectives and current trends. J. Investig. Clin. Dent. 2012, 3, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Jaywant, S.A.; Arif, K.M. A Comprehensive Review of Microfluidic Water Quality Monitoring Sensors. Sensors 2019, 19, 4781. [Google Scholar] [CrossRef] [PubMed]
- Kwietniewski, M.; Miszta-Kruk, K.; Niewitecka, K.; Sudoł, M.; Gaska, K. Certainty Level of Water Delivery of the Required Quality by Water Supply Networks. Int. J. Environ. Res. Public Heal. 2019, 16, 1860. [Google Scholar] [CrossRef] [PubMed]
- Fujita, M.; Mashima, I.; Nakazawa, F. Monitoring the decontamination efficacy of the novel Poseidon-S disinfectant system in dental unit water lines. J. Microbiol. Immunol. Infect. 2017, 50, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Noopan, S.; Unchui, P.; Techotinnakorn, S.; Ampornaramveth, R.S. Plasma Sterilization Effectively Reduces Bacterial Contamination in Dental Unit Waterlines. Int. J. Dent. 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pantanella, F.; Schippa, S.; Solimini, A.; Rosa, L.; Bettucci, A.; Berlutti, F. Efficacy of acoustic waves in preventing Streptococcus mutans adhesion on dental unit water line. . 2019, 31, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Laino, L.; Cicciù, M.; Cervino, G.; Fiorillo, L.; D’amico, C.; Zhurakivska, K.; Muzio, L.L. Comparison of Two Routes of Administration of Dexamethasone to Reduce the Postoperative Sequelae After Third Molar Surgery: A Systematic Review and Meta-Analysis. Open Dent. J. 2018, 12, 181–188. [Google Scholar] [CrossRef]
- Kohn, W.G.; Collins, A.S.; Cleveland, J.L.; Harte, J.A.; Eklund, K.J.; Malvitz, D.M.; Centers for Disease Control and Prevention (CDC). Guidelines for infection control in dental health-care settings—2003. MMWR. Recomm. Rep. 2003, 52, 1–61. [Google Scholar]
- ADA STATEMENT ON DENTAL UNIT WATERLINES. J. Am. Dent. Assoc. 1996, 127, 185–186. [CrossRef]
- Rosa, V.; Agarwalla, S.V.; Tan, B.L.; Choo, S.Y.; Sim, Y.F.; Boey, F.Y.C.; Anantharaman, S.; Duggal, M.S.; Tan, K.S. Pandemic Preparedness and Response: A Foldable Tent to Safely Remove Contaminated Dental Aerosols—Clinical Study and Patient Experience. Appl. Sci. 2022, 12, 7409. [Google Scholar] [CrossRef]
- Alkhulaifi, M.M.; Alotaibi, D.H.; Alajlan, H.; Binshoail, T. Assessment of nosocomial bacterial contamination in dental unit waterlines: Impact of flushing. Saudi Dent. J. 2020, 32, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Tims, M.; Bakker, A.B.; Derks, D. Development and validation of the job crafting scale. J. Vocat. Behav. 2012, 80, 173–186. [Google Scholar] [CrossRef]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Green, H.; Weller, D.; Johnson, S.; Michalenko, E. Microbial Source-Tracking Reveals Origins of Fecal Contamination in a Recovering Watershed. Water 2019, 11, 2162. [Google Scholar] [CrossRef] [PubMed]
- Ayers, K.M.; Thomson, W.M.; Rich, A.M.; Newton, J.T. Gender differences in dentists’ working practices and job satisfaction. J. Dent. 2008, 36, 343–350. [Google Scholar] [CrossRef] [PubMed]
- McKay, J.C.; Ahmad, A.; Shaw, J.L.; Rashid, F.; Clancy, A.; David, C.; Figueiredo, R.; Quiñonez, C. Gender Differences and Predictors of Work Hours in a Sample of Ontario Dentists. J Can Dent Assoc 2016, 82, g26. [Google Scholar]
- Walker, S.; Flores-Mir, C.; Heo, G.; Amin, M.S.; Keenan, L. Work pattern differences between male and female orthodontists in Canada. J Can Dent Assoc 2016, 82, g6. [Google Scholar]
- Emrani, R.; Sargeran, K.; Shamshiri, A.R.; Hessari, H. Job Satisfaction Among Dentists According to Workplace in Tehran. Front. Dent. 2021, 18, 11. [Google Scholar] [CrossRef]
- Surdu, S.; Mertz, E.; Langelier, M.; Moore, J. Dental Workforce Trends: A National Study of Gender Diversity and Practice Patterns. Med Care Res. Rev. 2020, 78, 30S–39S. [Google Scholar] [CrossRef]
- Archer, J. The reality and evolutionary significance of human psychological sex differences. Biol. Rev. 2019, 94, 1381–1415. [Google Scholar] [CrossRef] [PubMed]
- Baptiste, D.; Fecher, A.M.; Dolejs, S.C.; Yoder, J.; Schmidt, C.M.; Couch, M.E.; Ceppa, D.P. Gender differences in academic surgery, work-life balance, and satisfaction. J. Surg. Res. 2017, 218, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Rich-Edwards, J.W.; Kaiser, U.B.; Chen, G.L.; Manson, J.E.; Goldstein, J.M. Sex and Gender Differences Research Design for Basic, Clinical, and Population Studies: Essentials for Investigators. Endocr. Rev. 2018, 39, 424–439. [Google Scholar] [CrossRef] [PubMed]
- Shannon G, Jansen M, Williams K, Cáceres C, Motta A, Odhiambo A et al. Gender equality in science, medicine, and global health: where are we at and why does it matter? Lancet 2019, 393, 560–569. [CrossRef] [PubMed]
- Nirupama YS, Boppana NK, Vinnakota NR, Thetakala RK, Kallakuri P, Karthik BK. Indian women dentists’ perspectives towards balancing professional, personal and social responsibilities. J Dent Res 2020, 31, 358–362.
- Antoniadou, M. Estimation of Factors Affecting Burnout in Greek Dentists before and during the COVID-19 Pandemic. Dent. J. 2022, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Dousin, O.; Collins, N.; Kler, B.K. The experience of work-life balance for women doctors and nurses in Malaysia. Asia Pac. J. Hum. Resour. 2021, 60, 362–380. [Google Scholar] [CrossRef]
- McCarthy, G.M.; Macdonald, J.K. Gender differences in characteristics, infection control practices, knowledge and attitudes related to HIV among Ontario dentists. Community Dent. Oral Epidemiol. 1996, 24, 412–415. [Google Scholar] [CrossRef]
- Reza E, Sargeran K, Hessari H, Masoumeh E. Differences in the work pattern of male and female dentists in Tehran in 2021. Ital J Gender-Specific Med 2022, 8, 143–146.
- Li J, de Souza R, Esfandiari S, Feine J. Have women broken the glass ceiling in North American dental leadership? J Adv Dent Res 2019, 30, 78–84. [CrossRef]
- Shahin, S.Y.; Bugshan, A.S.; Almulhim, K.S.; AlSharief, M.S.; Al-Dulaijan, Y.A.; Siddiqui, I.; Al-Qarni, F.D. Knowledge of dentists, dental auxiliaries, and students regarding the COVID-19 pandemic in Saudi Arabia: a cross-sectional survey. BMC Oral Heal. 2020, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Qabool, H.; Sukhia, R.; Fida, M. Knowledge and awareness of dental specialists, general dentists and dental assistants regarding SARS-CoV-2. Dent. Med Probl. 2021, 58, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Schalli, M.; Kogler, B.; Miorini, T.; Gehrer, M.; Reinthaler, F.F. High-Speed Dental Instruments: An Investigation of Protein-Contaminated Dental Handpieces with the Bicinchoninic Acid Assay in Dental Offices in Styria, Austria. Int. J. Environ. Res. Public Heal. 2023, 20, 1670. [Google Scholar] [CrossRef] [PubMed]
- Pinto, F.M.G.; Bruna, C.Q.d.M.; Camargo, T.C.; Marques, M.; Silva, C.B.; Sasagawa, S.M.; Mimica, L.M.J.; Graziano, K.U. The practice of disinfection of high-speed handpieces with 70% w/v alcohol: An evaluation. Am. J. Infect. Control. 2016, 45, e19–e22. [Google Scholar] [CrossRef] [PubMed]
- Osegueda-Espinosa, A.A.D.; Sánchez-Pérez, L.D.; Perea-Pérez, B.M.; Labajo-González, E.D.; Acosta-Gio, A.E.D. Dentists Survey on Adverse Events During Their Clinical Training. J. Patient Saf. 2017, 16, e240–e244. [Google Scholar] [CrossRef]
- Hbibi, A.; Kasouati, J.; Charof, R.; Chaouir, S.; El Harti, K. Evaluation of the knowledge and attitudes of dental students toward occupational blood exposure accidents at the end of the dental training program. J. Int. Soc. Prev. Community Dent. 2018, 8, 77–86. [Google Scholar] [CrossRef]
- Agahi, R.H.; Hashemipour, M.A.; Kalantari, M.; Ayatollah-Mosavi, A.; Aghassi, H.; Nassab, A.H.G. Effect of 0.2% chlorhexidine on microbial and fungal contamination of dental unit waterlines. Dent Res 2014, 11, 351–356. [Google Scholar]
- Dupont, D.; Adamowicz, W.L.; Krupnick, A. Differences in water consumption choices in Canada: the role of socio-demographics, experiences, and perceptions of health risks. J. Water Heal. 2010, 8, 671–686. [Google Scholar] [CrossRef]
- Banakar, M.; Lankarani, K.B.; Jafarpour, D.; Moayedi, S.; Banakar, M.H.; MohammadSadeghi, A. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Heal. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Chate, R.A.C. An audit improves the quality of water within the dental unit water lines of general dental practices across the East of England. Br. Dent. J. 2010, 209, E11–E11. [Google Scholar] [CrossRef]
- Italian Health Ministry. Guidelines for Prevention and Control of Legionellosis. Rome, Italy: 2015. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2362_allegato.pdf (accessed on 17 June 2020).
- Mcmanus, K.R.; Fan, P. Purchasing, installing and operating dental amalgam separators. J. Am. Dent. Assoc. 2003, 134, 1054–1065. [Google Scholar] [CrossRef] [PubMed]
- Spaveras, A.; Antoniadou, M. Awareness of Students and Dentists on Sustainability Issues, Safety of Use and Disposal of Dental Amalgam. Dent. J. 2023, 11, 21. [Google Scholar] [CrossRef] [PubMed]
- Oosthuysen, J.; Potgieter, E.; Fossey, A. Compliance with infection prevention and control in oral health-care facilities: a global perspective. Int. Dent. J. 2014, 64, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Carraro E, Bonetta S, Bonetta S. Hospital Wastewater: Existing Regulations and Current Trends in Management. In: Verlicchi, P. (eds) Hospital Wastewaters. The Handbook of Environmental Chemistry, vol 60. Springer, Cham. 2017. [CrossRef]
- Antoniadou, M.; Chrysochoou, G.; Tzanetopoulos, R.; Riza, E. Green Dental Environmentalism among Students and Dentists in Greece. Sustainability 2023, 15, 9508. [Google Scholar] [CrossRef]
| Female | Male | |||||
| N | % | N | % | χ2(p) | ||
| Interested in learning more | 77 | 87.50% | 84 | 71.80% | 7.35(.006) | |
| Continuous water supply system cutters | 22 | 25.00% | 47 | 40.20% | 5.17(.023) | |
| Water supply to the dental unit | Water from public network | 62 | 73.80% | 67 | 58.30% | 8.90(.012) |
| Distilled/Deionized water | 8 | 9.50% | 7 | 6.10% | ||
| Water from a filter device directly connected to the supply | 14 | 16.70% | 41 | 35.70% | ||
| Water supply to the handpieces | Water from public network | 58 | 70.70% | 66 | 56.90% | 6.72(.035) |
| Deionized/Distilled water | 10 | 12.20% | 11 | 9.50% | ||
| Water from a filter device directly connected to the supply | 14 | 17.10% | 39 | 33.60% | ||
| Supply to ultrasonic scaler | Water from public network | 55 | 68.80% | 59 | 51.80% | 10.31(.006) |
| Distilled/Deionized water | 14 | 17.50% | 16 | 14.00% | ||
| Water from a filter device directly connected to the supply | 11 | 13.80% | 39 | 34.20% | ||
| Disinf. Surfaces | between two patients | 85 | 97.70% | 103 | 88.00% | 12.54(.028) |
| every few appointments | 0 | 0.00% | 8 | 6.80% | ||
| per day | 1 | 1.10% | 6 | 5.10% | ||
| per week | 1 | 1.10% | 0 | 0.00% | ||
| Annual maintenance | 55 | 66.30% | 66 | 57.90% | 10.10(.018) | |
| Has implantology motor | 24 | 27.60% | 52 | 44.40% | 6.07(.014) | |
| Experience | ||||||||||
| 0-10 έτη | 11-20 έτη | 21-30 έτη | 31 και άνω έτη | |||||||
| N | % | N | % | N | % | N | % | χ2(p) | ||
| Water supply to the dental unit | Water from public network | 25 | 89.30% | 36 | 63.20% | 37 | 64.90% | 32 | 55.20% | 13.70(.033) |
| Distilled/Deionized water | 1 | 3.60% | 7 | 12.30% | 4 | 7.00% | 3 | 5.20% | ||
| Water from filter | 2 | 7.10% | 14 | 24.60% | 16 | 28.10% | 23 | 39.70% | ||
| Water supply to the handpieces | Water from public network | 24 | 92.30% | 37 | 62.70% | 34 | 60.70% | 29 | 50.00% | 16.69(.010) |
| Deionized/Distilled water | 1 | 3.80% | 9 | 15.30% | 6 | 10.70% | 6 | 10.30% | ||
| Water from filter | 1 | 3.80% | 13 | 22.00% | 16 | 28.60% | 23 | 39.70% | ||
| Supply to ultrasonic scaler | Water from public network | 21 | 80.80% | 38 | 64.40% | 32 | 58.20% | 23 | 41.80% | 13.63(.034) |
| Distilled/Deionized water | 3 | 11.50% | 8 | 13.60% | 7 | 12.70% | 13 | 23.60% | ||
| Water from filter | 2 | 7.70% | 13 | 22.00% | 16 | 29.10% | 19 | 34.50% | ||
| Large amount of water through surgical suction to the dental unit | between two patients | 5 | 17.20% | 0 | 0.00% | 2 | 3.60% | 8 | 15.10% | 31.12(.008) |
| every few appointments (3-4) | 2 | 6.90% | 5 | 8.60% | 10 | 17.90% | 7 | 13.20% | ||
| per day | 9 | 31.00% | 28 | 48.30% | 22 | 39.30% | 25 | 47.20% | ||
| per week or more | 13 | 44.80% | 25 | 43.10% | 22 | 39.40% | 13 | 24.60% | ||
| Large amount of water to the dental unit | between two patients | 4 | 16.00% | 2 | 3.80% | 4 | 8.30% | 4 | 7.40% | 27.69(.024) |
| every few appointments (3-4) | 1 | 4.00% | 3 | 5.80% | 2 | 4.20% | 7 | 13.00% | ||
| per day | 10 | 40.00% | 11 | 21.20% | 13 | 27.10% | 22 | 40.70% | ||
| per week or more | 10 | 40.00% | 36 | 69.30% | 29 | 60.40% | 21 | 39.00% | ||
| Micromotors | 1 | 15 | 46.90% | 18 | 30.50% | 12 | 21.10% | 6 | 10.30% | 25.92(.011) |
| 2 | 5 | 15.60% | 22 | 37.30% | 19 | 33.30% | 23 | 39.70% | ||
| 3 | 3 | 9.40% | 5 | 8.50% | 9 | 15.80% | 7 | 12.10% | ||
| 4 | 3 | 9.40% | 8 | 13.60% | 3 | 5.30% | 11 | 19.00% | ||
| 5+ | 6 | 18.80% | 6 | 10.20% | 14 | 24.60% | 11 | 19.00% | ||
| Airotors | 1 | 11 | 34.40% | 8 | 13.60% | 5 | 8.80% | 5 | 8.60% | 29.17(.004) |
| 2 | 10 | 31.30% | 20 | 33.90% | 17 | 29.80% | 16 | 27.60% | ||
| 3 | 1 | 3.10% | 14 | 23.70% | 5 | 8.80% | 7 | 12.10% | ||
| 4 | 3 | 9.40% | 5 | 8.50% | 11 | 19.30% | 6 | 10.30% | ||
| 5+ | 7 | 21.90% | 12 | 20.30% | 19 | 33.30% | 24 | 41.40% | ||
| Is informed about water quality legislation | 8 | 27.60% | 3 | 5.40% | 7 | 13.20% | 10 | 17.50% | 8.34(.039) | |
| Time Spent | no time | 4 | 12.50% | 0 | 0.00% | 1 | 1.80% | 0 | 0.00% | 26.21(.002) |
| up to 2 hours per month | 13 | 40.60% | 13 | 22.00% | 15 | 26.30% | 16 | 27.60% | ||
| up to 4 hours per month | 10 | 31.30% | 22 | 37.30% | 14 | 24.60% | 16 | 27.60% | ||
| more than 4 hours | 5 | 15.60% | 24 | 40.70% | 27 | 47.40% | 26 | 44.80% | ||
| Education abroad | Postgraduate education | Recognized specialty | ||||||||||||||
| No | Yes | No | Yes | No | Yes | |||||||||||
| N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | ||
| Has assistant | 83 | 49.40% | 14 | 36.80% | ns | 41 | 35.70% | 56 | 61.50% | 13.66(<.001) | 82 | 44.30% | 15 | 71.40% | 5.56(.018) | |
| Knows the active substance of antiseptic | 45 | 31.70% | 13 | 39.40% | ns | 25 | 25.50% | 33 | 42.90% | 5.86(.016) | 55 | 35.00% | 3 | 16.70% | ns | |
| Antiseptic to the handpieces (auto) | 15 | 9.90% | 2 | 6.70% | ns | 5 | 4.90% | 12 | 15.20% | 5.54(.019) | 15 | 9.20% | 2 | 11.10% | ns | |
| Antiseptic to the handpieces (manually) | 17 | 11.30% | 9 | 30.00% | 7.15(.008) | 18 | 17.60% | 8 | 10.10% | ns | 25 | 15.30% | 1 | 5.60% | ns | |
| SmallSuction | between two patients | 80 | 50.00% | 10 | 26.30% | 13.26(.021) | 44 | 40.70% | 46 | 51.10% | 13.04(.023) | 85 | 47.80% | 5 | 25.00% | ns |
| every few appointments | 25 | 15.60% | 5 | 13.20% | 13 | 12.00% | 17 | 18.90% | 28 | 15.70% | 2 | 10.00% | ||||
| per day | 36 | 22.50% | 17 | 44.70% | 38 | 35.20% | 15 | 16.70% | 45 | 25.30% | 8 | 40.00% | ||||
| per week or more | 19 | 11.80% | 6 | 15.8% | 13 | 12.00% | 12 | 13.40% | 20 | 11.20% | 5 | 25.00% | ||||
| Annual maintenance | 103 | 64.00% | 19 | 51.40% | ns | 58 | 53.20% | 64 | 71.90% | 7.24(.007) | 114 | 64.00% | 8 | 40.00% | 4.40(.036) | |
| Micromotors | 1 | 38 | 22.60% | 13 | 34.20% | ns | 34 | 29.60% | 17 | 18.70% | 12.72(.013) | 43 | 23.20% | 8 | 38.10% | ns |
| 2 | 55 | 32.70% | 14 | 36.80% | 41 | 35.70% | 28 | 30.80% | 63 | 34.10% | 6 | 28.60% | ||||
| 3 | 20 | 11.90% | 4 | 10.50% | 8 | 7.00% | 16 | 17.60% | 22 | 11.90% | 2 | 9.50% | ||||
| 4 | 22 | 13.10% | 3 | 7.90% | 17 | 14.80% | 8 | 8.80% | 24 | 13.00% | 1 | 4.80% | ||||
| 5+ | 33 | 19.60% | 4 | 10.50% | 15 | 13.00% | 22 | 24.20% | 33 | 17.80% | 4 | 19.00% | ||||
| Airotors | 1 | 21 | 12.50% | 8 | 21.10% | ns | 21 | 18.30% | 8 | 8.80% | 8.94(.063) | 20 | 10.80% | 9 | 42.90% | 22.76(<.001) |
| 2 | 49 | 29.20% | 14 | 36.80% | 36 | 31.30% | 27 | 29.70% | 54 | 29.20% | 9 | 42.90% | ||||
| 3 | 21 | 12.50% | 6 | 15.80% | 16 | 13.90% | 11 | 12.10% | 27 | 14.60% | 0 | 0.00% | ||||
| 4 | 21 | 12.50% | 4 | 10.50% | 16 | 13.90% | 9 | 9.90% | 25 | 13.50% | 0 | 0.00% | ||||
| 5+ | 56 | 33.30% | 6 | 15.80% | 26 | 22.60% | 36 | 39.60% | 59 | 31.90% | 3 | 14.30% | ||||
| Has amalgam trap | 106 | 65.80% | 22 | 59.50% | ns | 70 | 63.60% | 58 | 65.90% | ns | 121 | 68.00% | 7 | 35.00% | 8.56(.003) | |
| Has contract for amalgam removal | 42 | 27.30% | 9 | 23.70% | ns | 22 | 20.60% | 29 | 34.10% | 4.46(.035) | 48 | 28.10% | 3 | 14.30% | ns | |
| Environment friendly practices | A little | 26 | 17.20% | 2 | 6.50% | 10.93(.012) | 18 | 17.10% | 10 | 13.00% | ns | 28 | 17.10% | 0 | 0.00% | ns |
| Satisfactory | 73 | 48.30% | 12 | 38.70% | 48 | 45.70% | 37 | 48.10% | 76 | 46.30% | 9 | 50.00% | ||||
| Enough | 41 | 27.20% | 9 | 29.00% | 30 | 28.60% | 20 | 26.00% | 43 | 26.20% | 7 | 38.90% | ||||
| Very much | 11 | 7.30% | 8 | 25.80% | 9 | 8.60% | 10 | 13.00% | 17 | 10.40% | 2 | 11.10% | ||||
| Implementation of disinfection protocol is my responsibility | 99 | 58.90% | 21 | 55.30% | ns | 76 | 66.10% | 44 | 48.40% | 6.57(.010) | 111 | 60.00% | 9 | 42.90% | ns | |
| General dentistry | Clinic vs private practice | Family Income | ||||||||||||||||
| No | Yes | No | Yes | <25.000 euros | 25.001-50.000 euros | >50.000 euros | ||||||||||||
| N | % | N | % | χ2(p) | N | % | N | % | χ2(p) | N | % | N | % | N | % | χ2(p) | ||
| Equipment’s age | 0-5 years | 12 | 24.00% | 31 | 19.90% | ns | 30 | 19.90% | 13 | 23.60% | 16.12(.001) | 19 | 27.50% | 11 | 12.20% | 10 | 57.50% | ns |
| 6-10 years | 13 | 26.00% | 28 | 17.90% | 21 | 13.90% | 20 | 36.40% | 12 | 17.40% | 17 | 18.90% | 11 | 30.30% | ||||
| 11-20 years | 17 | 34.00% | 71 | 45.50% | 70 | 46.40% | 18 | 32.70% | 30 | 43.50% | 44 | 48.90% | 11 | 30.30% | ||||
| 21 and above | 8 | 16.00% | 26 | 16.70% | 30 | 19.90% | 4 | 7.30% | 8 | 11.60% | 18 | 20.00% | 7 | 15.20% | ||||
| Has assistant | 39 | 78.00% | 58 | 37.20% | 25.32(<.001) | 50 | 33.10% | 47 | 85.50% | 44.26(<.001) | 22 | 31.90% | 45 | 50.00% | 27 | 66.70% | 14.36(<.001) | |
| Performs microbiological test | 13 | 26.00% | 32 | 20.50% | ns | 33 | 21.90% | 12 | 21.80% | ns | 17 | 24.60% | 13 | 14.40% | 14 | 56.10% | 7.60(.022) | |
| Continuous water supply system to dental unit | 15 | 30.00% | 47 | 30.10% | ns | 41 | 27.20% | 21 | 38.20% | ns | 16 | 23.20% | 26 | 28.90% | 18 | 48.50% | 6.38(.041) | |
| Antiseptic to the handpieces (auto) | 6 | 13.60% | 11 | 8.00% | ns | 8 | 6.10% | 9 | 18.40% | 6.36(.012) | 8 | 14.00% | 3 | 3.80% | 6 | 16.10% | 6.21(.045) | |
| Antiseptic to the handpieces (manually) | 2 | 4.50% | 24 | 17.50% | 4.56(.033) | 19 | 14.40% | 7 | 14.30% | ns | 9 | 15.80% | 10 | 12.50% | 6 | 16.10% | ns | |
| Clean suction Large Small | between two patients | 21 | 45.70% | 69 | 45.40% | ns | 63 | 44.10% | 27 | 49.10% | ns | 27 | 40.30% | 39 | 46.40% | 0 | 45.50% | 23.24(.010) |
| every few appointments | 3 | 6.50% | 27 | 17.80% | 24 | 16.80% | 6 | 10.90% | 13 | 19.40% | 9 | 10.70% | 1 | 18.20% | ||||
| per day | 13 | 28.30% | 40 | 26.30% | 38 | 26.60% | 15 | 27.30% | 13 | 19.40% | 30 | 35.70% | 5 | 15.20% | ||||
| per week or more | 9 | 19.5% | 16 | 10.6% | 18 | 12.6% | 7 | 12.7% | 14 | 20.9% | 6 | 7.2% | 6 | 12.1% | ||||
| between two patients | 4 | 8.50% | 11 | 7.40% | 11.64(.040) | 8 | 5.60% | 7 | 13.00% | ns | 6 | 9.10% | 3 | 3.60% | 8 | 6.10% | ns | |
| every few appointments | 3 | 6.40% | 21 | 14.10% | 14 | 9.90% | 10 | 18.50% | 9 | 13.60% | 12 | 14.30% | 1 | 9.10% | ||||
| per day | 24 | 51.10% | 60 | 40.30% | 61 | 43.00% | 23 | 42.60% | 20 | 30.30% | 38 | 45.20% | 0 | 63.60% | ||||
| per week or more | 16 | 34.00% | 57 | 38.30% | 59 | 41.50% | 14 | 25.90% | 31 | 47.00% | 31 | 37.00% | 8 | 38.00% | ||||
| Micromotors | 1 | 9 | 18.00% | 42 | 26.90% | ns | 46 | 30.50% | 5 | 9.10% | 31.40(<.001) | 23 | 33.30% | 20 | 22.20% | 15 | 18.20% | 24.39(.002) |
| 2 | 19 | 38.00% | 50 | 32.10% | 58 | 38.40% | 11 | 20.00% | 20 | 29.00% | 39 | 43.30% | 3 | 24.20% | ||||
| 3 | 5 | 10.00% | 19 | 12.20% | 16 | 10.60% | 8 | 14.50% | 9 | 13.00% | 12 | 13.30% | 11 | 9.10% | ||||
| 4 | 4 | 8.00% | 21 | 13.50% | 15 | 9.90% | 10 | 18.20% | 8 | 11.60% | 8 | 8.90% | 4 | 15.20% | ||||
| 5+ | 13 | 26.00% | 24 | 15.40% | 16 | 10.60% | 21 | 38.20% | 9 | 13.00% | 11 | 12.20% | 0 | 33.30% | ||||
| Airotors | 1 | 10 | 20.00% | 19 | 12.20% | ns | 24 | 15.90% | 5 | 9.10% | 22.04(<.001) | 13 | 18.80% | 13 | 14.40% | 2 | 6.10% | Ns |
| 2 | 16 | 32.00% | 47 | 30.10% | 53 | 35.10% | 10 | 18.20% | 23 | 33.30% | 28 | 31.10% | 1 | 30.30% | ||||
| 3 | 6 | 12.00% | 21 | 13.50% | 23 | 15.20% | 4 | 7.30% | 9 | 13.00% | 15 | 16.70% | 14 | 3.00% | ||||
| 4 | 5 | 10.00% | 20 | 12.80% | 19 | 12.60% | 6 | 10.90% | 9 | 13.00% | 10 | 11.10% | 6 | 15.20% | ||||
| 5+ | 13 | 26.00% | 49 | 31.40% | 32 | 21.20% | 30 | 54.50% | 15 | 21.70% | 24 | 26.70% | 6 | 45.50% | ||||
| Has implantology motor | 17 | 34.70% | 60 | 38.50% | ns | 48 | 32.00% | 29 | 52.70% | 7.37(.007) | 28 | 41.20% | 28 | 31.10% | 0 | 45.50% | Ns | |
| Has amalgam trap | 25 | 52.10% | 103 | 68.70% | 4.38(.038) | 90 | 62.50% | 38 | 70.40% | ns | 46 | 71.90% | 54 | 61.40% | 38 | 62.50% | Ns | |
| Has contract for amalgam removal | 10 | 21.70% | 41 | 28.10% | ns | 32 | 22.70% | 19 | 37.30% | 4.07(.044) | 16 | 27.10% | 21 | 23.90% | 20 | 34.40% | Ns | |
| MoneySpent | <25€/month | 11 | 22.00% | 33 | 21.20% | 37 | 24.50% | 7 | 12.70% | 21 | 30.40% | 18 | 20.00% | 5 | 12.10% | |||
| 25-50€/month | 18 | 36.00% | 71 | 45.50% | 73 | 48.30% | 16 | 29.10% | 30 | 43.50% | 42 | 46.70% | 8 | 30.30% | ||||
| 50-75€/month | 9 | 18.00% | 29 | 18.60% | 24 | 15.90% | 14 | 25.50% | 10 | 14.50% | 14 | 15.60% | 3 | 36.40% | ||||
| >75€/month | 9 | 18.00% | 18 | 11.50% | 12 | 7.90% | 15 | 27.30% | 6 | 8.70% | 12 | 13.30% | 1 | 18.20% | ||||
| Implementation of disinfection protocol is my responsibility | 19 | 38.00% | 101 | 64.70% | 11.14(<.001) | 104 | 68.90% | 16 | 29.10% | 26.24(<.001) | 49 | 71.00% | 47 | 52.20% | 0 | 54.50% | 6.26(.044) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





