Submitted:
26 April 2023
Posted:
27 April 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
3. Results
4. Discussion
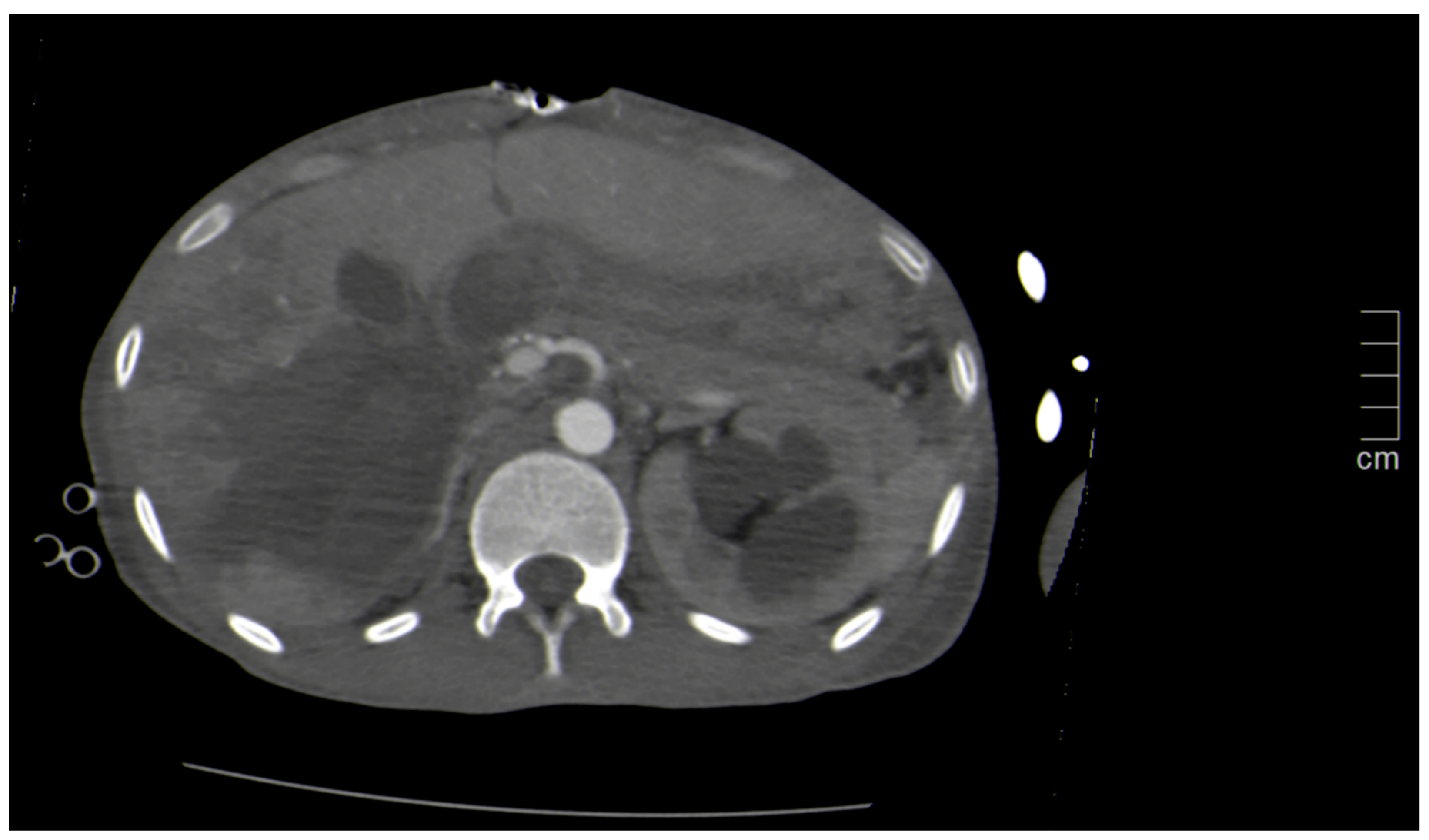
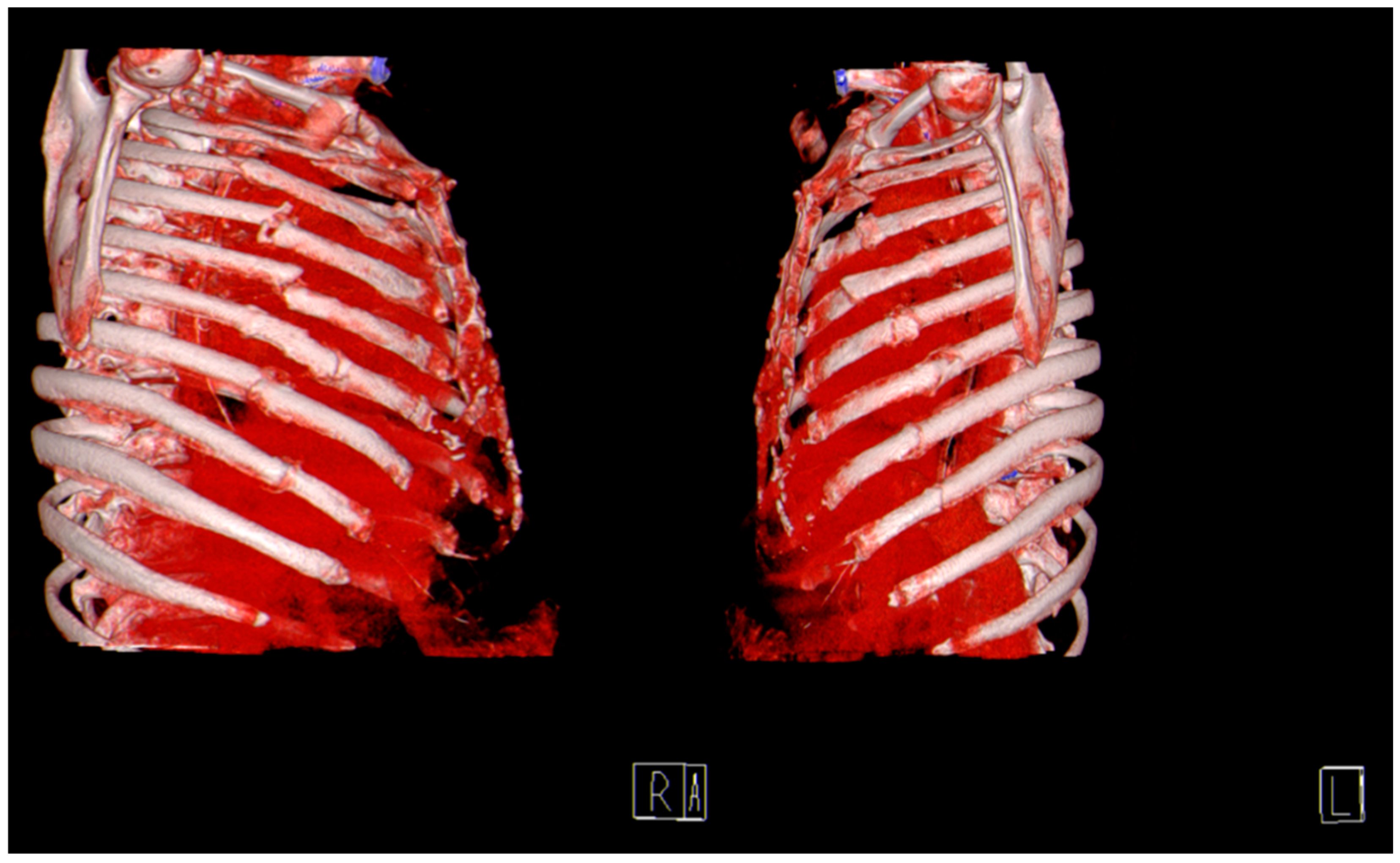
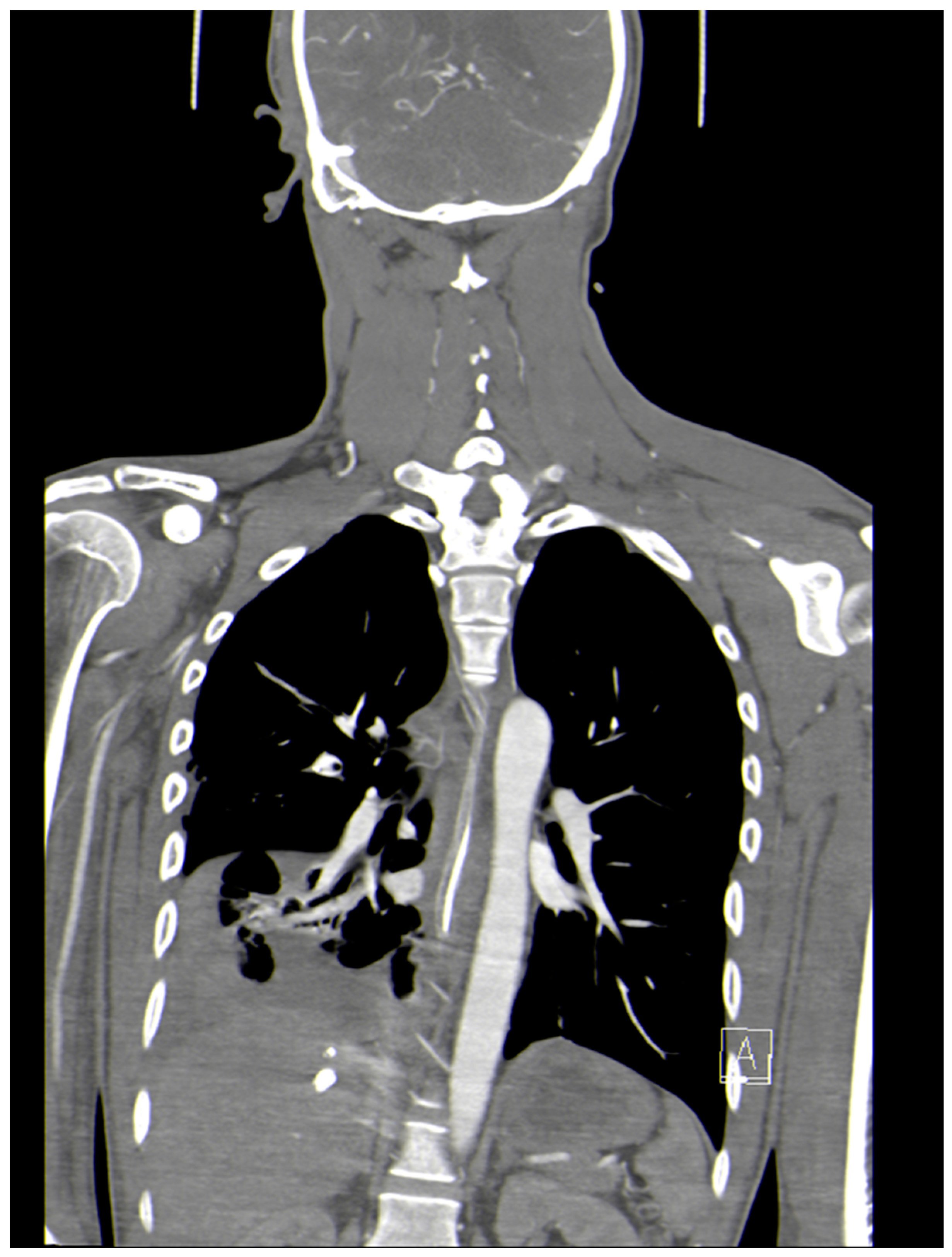
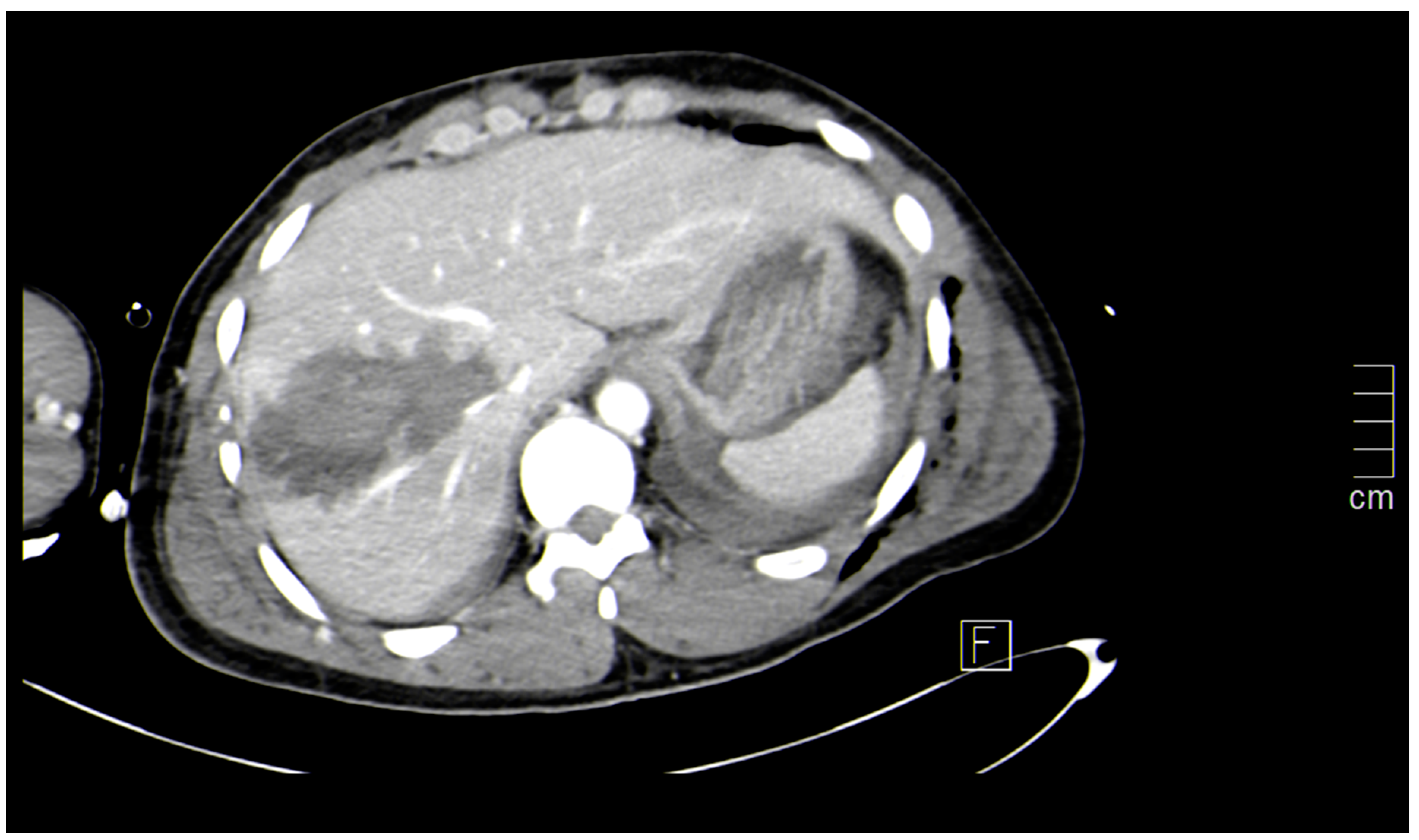
- 1. PAN CT (Whole Body CT)
- 2.
- CT Neck
- 3.
- CT Chest
- 4.
- CT Abdomen
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhattacharyya KB. Godfrey Newbold Hounsfield (1919-2004): The man who revolutionized neuroimaging, Ann Indian Acad Neurol. 2016 Oct-Dec; 19(4):448-450. [CrossRef]
- Harntaweesup S, Krutsri C, Sumritpradit P, Singhatas P, Thampongsa T, Jenjitranant P, Wongwaisayawan S, Saksobhavivat N, Kaewlai R. Usefulness and outcome of whole-body computed tomography (pan-scan) in trauma patients: A prospective study. Ann Med Surg (Lond). 2022 Mar 28;76:103506. [CrossRef]
- Yoong S, Kothari R, Brooks A. Assessment of sensitivity of whole body CT for major trauma. Eur J Trauma Emerg Surg. 2019; 45(3): 489-492. [CrossRef]
- Singh N, Hardcastle TC. Selective non-operative management of gunshot wounds to the abdomen: A Collective Review. Int Emerg Nurs 2015, 23(1): 22-31. [CrossRef]
- Keijzers GB, Giannakopoulos GF, Del Mar C, Bakker FC, Geeraedts LM Jr. The effect of tertiary surveys on missed injuries in trauma: a systematic review. Scand J Trauma Resusc Emerg Med. 2012; 20: 77. 3. Jones J, Murphy A, Kusel K. Whole-body CT (protocol). Radiopeadia.org. 15 May 2010. [CrossRef]
- Hardcastle TC. Missed Injury: Decreasing Morbidity and Mortality. A literature review. S Afr J Surg. 2011; 49: 199 – 201.
- Mayet M, Hardcastle TC, Muckart DJJ. Intra-abdominal injury identified by Computed Tomographic Angiography in haemodynamically stable polytrauma patients with injury both above the thoracic and below the pelvic diaphragm. S Afr J Surg, 2019; 57(1): 49-53. http://doi.org/10.17159/2078-5151/2019/v57n1a2715.
- Sierink JC, Treskes K, Edwards MJ, Beuker BJ, den Hartog D, Hohmann J, Dijkgraaf MG, Luitse JS, Beenen LF, Hollmann MW, Goslings JC; REACT-2 study group. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016; 388(10045): 673-683. [CrossRef]
- Murphy SP, Hawthorne N, Haase D, Chiku C, Wen J, Rodriguez RM. Low Yield of Clinically Significant Injury With Head-To-Pelvis Computed Tomography in Blunt Trauma Evaluation. J Emerg Med. 2017; 53(6): 865-870. [CrossRef]
- Gordic S, Alkadhi H, Hodel S, Whole-body CT-based imaging algorithm for multiple trauma patients: radiation dose and time to diagnosis. Br J Radiol. 2015 Mar;88(1047). [CrossRef]
- Cao, CF., Ma, KL., Shan, H. et al. CT Scans and Cancer Risks: A Systematic Review and Dose-response Meta-analysis. BMC Cancer 22, 1238 (2022). [CrossRef]
- Ordoñez CA, Parra MW, Holguín A, Whole-body computed tomography is safe, effective and efficient in the severely injured hemodynamically unstable trauma patient. Colomb Med (Cali). 2020; 51(4): e4054362. [CrossRef]
- Aycock RD, Westafer LM, Boxen JL, Majlesi N, Schoenfeld EM, Bannuru RR. Acute Kidney Injury After Computed Tomography: A Meta-analysis. Ann Emerg Med. 2018; 71(1): 44-53.e4. [CrossRef]
- Hinson JS, Ehmann MR, Fine DM, Fishman EK, Toerper MF, Rothman RE, Klein EY. Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Ann Emerg Med. 2017; 69(5): 577-586.e4. [CrossRef]
- Ehmann MR, Mitchell J, Levin S, Smith A, Menez S, Hinson JS, Klein EY. Renal outcomes following intravenous contrast administration in patients with acute kidney injury: a multi-site retrospective propensity-adjusted analysis. Intensive Care Med. 2023 Feb;49(2):205-215. [CrossRef]
- Goto Y, Koyama K, Katayama S, Tonai K, Shima J, Koinuma T, Nunomiya S. Influence of contrast media on renal function and outcomes in patients with sepsis-associated acute kidney injury: a propensity-matched cohort study. Crit Care. 2019; 23(1): 249. [CrossRef]
- Parag P, Hardcastle TC. Interpretation of emergency CT scans in polytrauma: trauma surgeon vs radiologist. Afr J Emerg Med 2020, 10: 90-94. [CrossRef]
- Parag P, Hardcastle TC. Shortage of Radiologists in Low to Middle Income Countries in the Interpretation of CT scans in Trauma. Bangl J Med Sci 2022; 21(03 July): 489-491. [CrossRef]
- Adams A, Shah N, Stephenson R. An approach to accurate computed tomography imaging interpretation in penetrating neck trauma. Acta Radiol Open. 2020 ; 9(6): 2058460120938742. [CrossRef]
- Ryan B. Fransman, Faris K. Azar, William Mallon, The “No zone” Approach to penetrating Neck Trauma. American college of Surgeon, 24 Feb 2021.
- Madsen AS, Bruce JL, Oosthuizen GV. Correlation between the level of the external wound and the internal injury in penetrating neck injury does not favour an initial zonal management approach. BJS Open. 2020 Aug;4(4):704-713. [CrossRef]
- Maritz, JPB; Bagadia, A; Lubbe, JA. Can computed tomographic angiography accurately exclude digestive tract injury after penetrating cervical trauma? S Afr J surg. 2020, 58(4): 92-198. http://doi.org/10.17159/2078-5151/2020/v58n4a3159.
- Conradie WJ, Gebremariam FA. Can computed tomography esophagography reliably diagnose traumatic penetrating upper digestive tract injuries? Clin Imaging 2015; 39(6): 1039-1045. [CrossRef]
- Parida PK, Kalaiarasi R, Alexander A. Management of Laryngotracheal Trauma: A Five-Year Single Institution Experience. Iran J Otorhinolaryngol. 2018; 30(100): 283-290.
- Eissa L., Mehanna AM. Biphasic CT imaging of deep neck infections (DNIs): how does dual injection mode help in differentiation between types of collections? Egypt J Otolaryngol 2020; 36: 40. [CrossRef]
- Yonetsu K, Izumi M, Nakamura T. Deep facial infections of odontogenic origin: CT assessment of pathways of space involvement. AJNR Am J Neuroradiol 1998; 19: 123–128.
- Cutaia, G., Messina, M., Rubino, S. et al. Caustic ingestion: CT findings of esophageal injuries and thoracic complications. Emerg Radiol 2021; 28: 845–856. [CrossRef]
- Muckart DJJ, Hardcastle TC, Skinner DL. Pneumomediastinum and Pneumopericardium Following Blunt Thoracic Trauma: Much Ado About Nothing? Eur J Trauma and Emerg Surg, 2019, 45: 927-931. [CrossRef]
- Mason AC, Mirvis SE, Templeton PA. Imaging of acute tracheobronchial injury: Review of literature. Emergency Radiology, 1994; 1: 250-260. [CrossRef]
- Awais M, Qamar S, Shafqat G. Accuracy of CT chest without oral contrast for ruling out esophageal perforation using fluoroscopic esophagography as reference standard: retrospective study. Eur J Trauma Emerg Surg, 2019; 45: 517-525. [CrossRef]
- Strumwasser A, Chong V, Chu E, Victorino GP. Thoracic computed tomography is an effective screening modality in patients with penetrating injuries to the chest. Injury. 2016; 47(9): 2000-2005. [CrossRef]
- Chou YP, Kuo LC, Soo KM, Tarng YW, Chiang HI, Huang FD, Lin HL. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardiothorac Surg. 2014; 46(1): 107-111. [CrossRef]
- Velmahos GC, Demetriades D, Chan L, Tatevossian R, Cornwell EE, Yassa N, Murray JA, Asensio JA, Berne TV. Predicting the need for thoracoscopic evacuation of residual traumatic hemothorax: chest radiograph is insufficient. J Trauma. 1999; 46(1): 65-70. [CrossRef]
- Scaglione M, Pinto A, Romano L. CT features of descending necrotizing mediastinitis – a pictorial essay. Emerg Radiol, 2007; 14: 77-81. [CrossRef]
- Guan X, Laing X, Wang F, Qian W, Zhang W. A new classification of descending necrotizing mediastinitis and surgical strategies. Ann Transl Med 2021; 9(4): 356. [CrossRef]
- Exarhos DN, Malagari K, Tsatalou EG, Acute mediastinitis: spectrum of computed tomography findings. Eur Radiol. 2005 Aug;15(8): 1569-1574. [CrossRef]
- Meyer DM, Thal ER, Weigelt JA, Redman HC. The role of abdominal CT in the evaluation of stab wounds to the back. J Trauma1989; 29(9): 1226-1228; discussion 1228-1230. [CrossRef]
- Mayet M, Hardcastle TC, Muckart DJ. Benign portal venous gas after blunt abdominal trauma. Injury Extra 2011; 42: 189-191. [CrossRef]
- Navsaria P, Nicol A, Krige J, Edu S, Chowdhury S. Selective nonoperative management of liver gunshot injuries. Eur J Trauma Emerg Surg. 2019; 45(2): 323-328. [CrossRef]
- Chmielewski GW, Nicholas JM, Dulchavsky SA, Diebel LN. Nonoperative management of gunshot wounds of the abdomen. Am. Surg.1995 Aug;61(8). PMID:7618803.
- Morell-Hofert D, Florian Primavesi F, Fodor M. Validation of the revised 2018 AAST-OIS classification and the CT severity index for prediction of operative management and survival in patients with blunt spleen and liver injuries. Eur Radiol. 2020; 30(12) :6570-6581. [CrossRef]
- Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Scalea TM. Triple-contrast helical CT in penetrating torso trauma: a prospective study to determine peritoneal violation and the need for laparotomy. AJR Am J Roentgenol. 2001 Dec;177(6):1247-56. [CrossRef]
- Mahummad Q, Sarah A, Mahmoud HA. Use of Multi-detector computed tomography by the emergency physicians in patients presenting with acute abdomen. A Retrospective Observational study in a large tertiary center. Trauma Emerg Care 6. [CrossRef]
- Sartelli M, Chichom-Mefire A, Labricciosa FM, Hardcastle T, Abu-Zidan FM, Adesunkanmi AK, Ansaloni L, Bala M, Balogh ZJ, Beltrán MA, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017; 12: 29. [CrossRef]
- Sartelli M; Coccolini F; Kluger Y; Agastra E; Abu-Zidan FM; Abbas AES; Ansaloni L; Adesunkanmi AK; Atanasov B; Augustin G; et al. WSES/GAIS/SIS-E/WSIS/AAST Global Clinical Pathways for Patients with Intra-Abdominal Infections. World J Emerg Surg, 2021; 16(1):49. [CrossRef]
- Aschoff AJ, Stuber G, Becker BW, Hoffmann MH, Schmitz BL, Schelzig H, Jaeckle T. Evaluation of acute mesenteric ischemia: accuracy of biphasic mesenteric multi-detector CT angiography. Abdom Imaging. 2009 May-Jun; 34(3): 345-357. [CrossRef]

Indications will vary from institution-to-institution but indications by mechanism include:
|
| Surgical causes acute abdomen | Medical causes of Acute Abdomen |
|---|---|
| 1. Acute Gastritis | 1. Acute myocardial infarction |
| 2. Acute Cholecystitis | 2. Diffuse gastritis |
| 3. Acute Appendicitis | 3. Uremic gastritis |
| 4. Acute Pancreatitis | 4. Pneumonia |
| 5. Perforated Peptic ulcer | 5. Pulmonary embolus |
| 6. Pelvic Inflammatory disease | 6. Oesophagitis |
| 7. Urinary tract stones | 7. Pyeloniphritis |
| 8. Testicular torsion | 8. Nephrolithiasis |
| 9. Abdominal aortic aneurysm | 9. Cystitis |
| 10. Acute gynecology pathology such as infections, ovarian torsion, fibroid uterus & ectopic pregnancy. | 10. Acute urinary retention. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





