Submitted:
19 April 2023
Posted:
20 April 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Neural Types in the Dorsal Ganglia Root and Their Colocalization with the Vesicular Transporter of Glutamate
Neurons
3. Pain Pathway Alteration
4. Optomodulation of Peripheral Nerve Activity
Optomodulation of Primary Afferent Fibers with Viral Transfections and Constitutive Expression
5. Long-Term Chemogenic Modulation of Pain
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Campbell, J. N., and Meyer, R. A. (2006). Review Mechanisms of Neuropathic Pain. Neuron 52, 77–92. [CrossRef]
- Treede, R.D. , Jensen, T.S., Campbell, J.N., Cruccu, G., Dostrovsky, J.O., Griffin, J.W., Hansson, P., Hughes, R., Nurmikko, T., Serra, J. (2008). Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 70, 1630-1635. [CrossRef]
- Basbaum, A. I., Bautista, D. M., Scherrer, G., and Julius, D. (2009). Cellular and Molecular Mechanisms of Pain. Cell. 139, 267-284. [CrossRef]
- Zhang, J. M. , Song, X. J., and LaMotte, R. H. (1997). An in vitro study of ectopic discharge generation and adrenergic sensitivity in the intact, nerve-injured rat dorsal root ganglion. Pain. 72 51-57. [CrossRef]
- Ruscheweyh, R. , Forsthuber, L., Schoffnegger, D., and Sandkühler, J. (2007). Modification of classical neurochemical markers in identified primary afferent neurons with Aβ-, Aδ-, and C-fibers after chronic constriction injury in mice. J. Comp. Neurol. [CrossRef]
- Chiu, I.M., Barrett, L.B., Williams, E.K., Strochlic, D.E., Lee, S., Weyer, A.D., Lou, S., Bryman, G.S., Roberson, D.P., Ghasemlou, N., Piccoli, C., Ahat, E., Wang, V., Cobos, E.J., Stucky, C.L., Ma. Q., Liberles, S.D., Woolf, C.J. (2014). Transcriptional profiling at whole population and single cell levels reveals somatosensory neuron molecular diversity. Elife. 3, e04660. [CrossRef]
- Medici, T., and Shortland, P. J. (2015). Effects of peripheral nerve injury on parvalbumin expression in adult rat dorsal root ganglion neurons. BMC Neurosci. 16, 1–10. [CrossRef]
- Taylor-Clark, T. E. , Wu, K. Y., Thompson, J. A., Yang, K., Bahia, P. K., and Ajmo, J. M. (2015). Thy1.2 YFP-16 transgenic mouse labels a subset of large-diameter sensory neurons that lack TRPV1 expression. PLoS One. 10, 1–16. [CrossRef]
- Crawford, L. T. K. , and Caterina, M. J. (2020). Functional Anatomy of the Sensory Nervous System: Updates From the Neuroscience Bench. Toxicol. Pathol. 48, 174–189. [CrossRef]
- Amaya, F. , Decosterd, I., Samad, T. A., Plumpton, C., Tate, S., Mannion, R. J., et al. (2000). Diversity of expression of the sensory neuron-specific TTX-resistant voltage-gated sodium ion channels SNS and SNS2. Mol. Cell. Neurosci. 15, 331–342. [CrossRef]
- Smith, T. , Al Otaibi, M., Sathish, J., and Djouhri, L. (2015). Increased expression of HCN2 channel protein in L4 dorsal root ganglion neurons following axotomy of L5- and inflammation of L4-spinal nerves in rats. Neuroscience 295, 90–102. [CrossRef]
- Usoskin, D. , Furlan, A., Islam, S., Abdo, H., Lönnerberg, P., Lou, D., Hjerling-Leffler, J., Haeggström, J., Kharchenko, O., Kharchenko, P.V., Linnarsson, S., Ernfors, P. (2015). Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat. Neurosci. 18, 145–153. [CrossRef]
- Acosta, C. , McMullan, S., Djouhri, L., Gao, L., Watkins, R., Berry, C., Dempsey, K., Lawson, S.N. (2012). HCN1 and HCN2 in Rat DRG neurons: levels in nociceptors and non-nociceptors, NT3-dependence and influence of CFA-induced skin inflammation on HCN2 and NT3 expression. PLoS One. 7, e50442. [CrossRef]
- Levanon, D. , Bettoun, D., Harris-Cerruti, C., Woolf, E., Negreanu, V., Eilam, R., Bernstein, Y., Goldenberg, D., Xiao, C., Fliegauf, M., Kremer, E., Otto, F., Brenner, O., Lev-Tov, A., Groner, Y. (2002). The Runx3 transcription factor regulates development and survival of TrkC dorsal root ganglia neurons. EMBO J. 21, 3454-3463. [CrossRef]
- Nakamura, S. , Senzaki, K., Yoshikawa, M., Nishimura, M., Inoue, K. I., Ito, Y., Ozaki, S., Shiga, T. (2008). Dynamic regulation of the expression of neurotrophin receptors by Runx3. 135, 1703-1711. Development. [CrossRef]
- de Nooij, J. C., Doobar, S., and Jessell, T. M. (2013). Etv1 Inactivation Reveals Proprioceptor Subclasses that Reflect the Level of NT3 Expression in Muscle Targets. Neuron 77, 1055–1068. [CrossRef]
- Yoshikawa, M., Senzaki, K., Yokomizo, T., Takahashi, S., Ozaki, S., and Shiga, T. (2007). Runx1 selectively regulates cell fate specification and axonal projections of dorsal root ganglion neurons. Dev. Biol. 303, 663–674. [CrossRef]
- Hu, J. , Huang, T., Li, T., Guo, Z., and Cheng, L. (2012). C-Maf is required for the development of dorsal horn laminae III/IV neurons and mechanoreceptive DRG axon projections. J. Neurosci. 32, 5362–5373. [CrossRef]
- Li, B., Yang, X., Qian, F., Tang, M., and Ma, C. (2015). A novel analgesic approach to optogenetically and speci fi cally inhibit pain transmission using TRPV1 promoter. Brain Res. 1609, 12–20. [CrossRef]
- Costigan, M. , and Woolf, C. J. (2000). Pain: molecular mechanisms. J Pain 1, 35–44. [CrossRef]
- Brumovsky, P. , Watanabe, M., and Hökfelt, T. (2007). Expression of the vesicular glutamate transporters-1 and -2 in adult mouse dorsal root ganglia and spinal cord and their regulation by nerve injury. Neuroscience 147, 469–490. [CrossRef]
- Lagerström, M. C. , Rogoz, K., Abrahamsen, B., Persson, E., Reinius, B., Nordenankar, K., Olund, C., Smith, C., Mendez, J.A., Chen, Z.F., Wood, J.N., Wallén-Mackenzie, A., Kullander, K. (2010). VGLUT2-Dependent Sensory Neurons in the TRPV1 Population Regulate Pain and Itch. Neuron. [CrossRef]
- Beaudry, H. , Daou, I., Ase, A. R., Ribeiro-Da-Silva, A., and Séguela, P. (2017). Distinct behavioral responses evoked by selective optogenetic stimulation of the major TRPV1+ and MrgD+ subsets of C-fibers. Pain 158, 2329–2339. [CrossRef]
- Duan, B. , Cheng, L., Bourane, S., Britz, O., Padilla, C., Garcia-Campmany, L., Krashes, M., Knowlton, W., Velasquez, T., Ren, X., Ross, S., Lowell, B.B., Wang, Y., Goulding, M., Ma. Q. (2014). Identification of spinal circuits transmitting and gating mechanical pain. Cell. 59(6):1417-1432. [CrossRef]
- Häring, M. , Zeisel, A., Hochgerner, H., Rinwa, P., Jakobsson, J.E.T., Lönnerberg, P., La Manno, G., Sharma, N., Borgius, L., Kiehn, O., Lagerström, M.C., Linnarsson, S., Ernfors, P. (2018). Neuronal atlas of the dorsal horn defines its architecture and links sensory input to transcriptional cell types. Nat Neuroscience, 21(6):869-880. [CrossRef]
- Jiang, Y.Q., Sun, Q., Tu, H.Y., Wan, Y. (2008) Characteristics of HCN channels and their participation in neuropathic pain. Neurochem Research. 33, 1979-1989. [CrossRef]
- Kobayashi, K. , Fukuoka, T., Obata, K., Yamanaka, H., Dai, Y., Tokunaga, A., Noguchi, K. (2005) Distinct expression of TRPM8, TRPA1, and TRPV1 mRNAs in rat primary afferent neurons with adelta/c-fibers and colocalization with trk receptors. J Comp Neurol. 26;493(4):596-606. [CrossRef]
- Patil, M.J. , Hovhannisyan, A.H., Akopian, A.N. (2018) Characteristics of sensory neuronal groups in CGRP-cre-ER reporter mice: Comparison to Nav1.8-cre, TRPV1-cre and TRPV1-GFP mouse lines. PLoS One. 13(6):e0198601. [CrossRef]
- Peirs, C. , Williams, S.P., Zhao, X., Walsh, C.E., Gedeon, J.Y., Cagle, N.E., Goldring, A.C., Hioki, H., Liu, Z., Marell, P.S., Seal, R.P. (2015). Dorsal Horn Circuits for Persistent Mechanical Pain. Neuron. 87(4):797-812. [CrossRef]
- Scherrer, G., Imamachi, N., Cao, Y. Q., Contet, C., Mennicken, F., O’Donnell, D., Kieffer, B.L., Basbaum, A.I. (2009). Dissociation of the opioid receptor mechanisms that control mechanical and heat pain. Cell 137, 1148–1159. [CrossRef]
- Scherrer, G. , Low, S.A., Wang, X., Zhang, J., Yamanaka, H., Urban, R., Solorzano, C., Harper, B., Hnasko, T.S., Edwards, R.H., Basbaum. A.I. (2010). VGLUT2 expression in primary afferent neurons is essential for normal acute pain and injury-induced heat hypersensitivity. Proc Natl Acad Sci U S A. 107, 22296-22301. [CrossRef]
- Wright, D.E. , Snider, W.D. (1995). Neurotrophin receptor mRNA expression defines distinct populations of neurons in rat dorsal root ganglia. J Comp Neurol. 351(3):329-38. [CrossRef]
- Bardoni, R., Tawfik, V.L., Wang, D., François, A., Solorzano, C., Shuster, S.A., Choudhury, P., Betelli, C., Cassidy, C., Smith, K., de Nooij, J.C., Mennicken, F., O'Donnell, D., Kieffer, B.L., Woodbury, C.J., Basbaum, A.I., MacDermott, A.B., Scherrer, G. (1014). Delta opioid receptors presynaptically regulate cutaneous mechanosensory neuron input to the spinal cord dorsal horn. Neuron. 81, 1312-1327. [CrossRef]
- Heinke, B. , Gingl, E., Sandkühler, J. (2011). Multiple targets of μ-opioid receptor-mediated presynaptic inhibition at primary afferent Aδ- and C-fibers. J Neurosci. 31, 1313-1322. [CrossRef]
- Li, L. , Rutlin, M., Abraira, V. E., Cassidy, C., Kus, L., Gong, S., Jankowski, M.P., Luo, W., Heintz, N., Koerber, H.R., Woodbury, C.J., Ginty, D.D. (2011). The functional organization of cutaneous low-threshold mechanosensory neurons. Cell. 1615. [Google Scholar] [CrossRef]
- Abrahamsen, B. , Zhao, J., Asante, C.O., Cendan, C.M., Marsh, S., Martinez-Barbera, J.P., Nassar, M.A., Dickenson, A.H., Wood, J.N. (2008). The cell and molecular basis of mechanical, cold, and inflammatory pain. Science. 321, 702-705. [CrossRef]
- Acton, D. , Ren, X., Di, Costanzo, S., Dalet, A., Bourane, S., Bertocchi, I., Eva, C., Goulding, M. (2019). Spinal neuropeptide Y1 receptor-expressing neurons form an essential excitatory pathway for mechanical itch. Cell Rep. 28, 625–639. [CrossRef]
- Brumovsky, P., Stanic, D., Shuster, S., Herzog, H., Villar, M., Hökfelt, T. (2005). Neuropeptide Y2 receptor protein is present in peptidergic and nonpeptidergic primary sensory neurons of the mouse. J Comp Neurol. 489, 328-48.
- Daou, I. , Beaudry, H., Ase, A. R., Wieskopf, J. S., Ribeiro-da-Silva, A., Mogil, J. S., Séguela, P. (2016). Optogenetic silencing of Nav1.8-positive afferents alleviates inflammatory and neuropathic pain. eNeuro 3, 702–705. [CrossRef]
- Szabo NE, da Silva RV, Sotocinal SG, Zeilhofer HU, Mogil JS, Kania A. Hoxb8 intersection defines a role for Lmx1b in excitatory dorsal horn neuron development, spinofugal connectivity, and nociception. J Neurosci. 2015 Apr 1;35(13):5233-46.
- Takasaki, I. , Watanabe, A., Yokai, M., Watanabe, Y., Hayakawa, D., Nagashima, R., Fukuchi, M., Okada, T., Toyooka, N., Miyata, A., Gouda, H., Kurihara, T. (2018). In silico screening identified novel small-molecule antagonists of PAC1 receptors. J. Pharmacol. Exp. Ther. 365, 1–8. [CrossRef]
- Wende, H. , Lechner, S.G., Cheret, C., Bourane, S., Kolanczyk, M.E., Pattyn, A., Reuter, K., Munier, F.L., Carroll, P., Lewin, G.R., Birchmeier, C. (2012). The transcription factor c-Maf controls touch receptor development and function. Science. 335, 1373-1376. [CrossRef]
- Xiang, C.X., Zhang, K.H., Johnson, R.L., Jacquin, M.F., Chen, Z.F. (2012). The transcription factor, Lmx1b, promotes a neuronal glutamate phenotype and suppresses a GABA one in the embryonic trigeminal brainstem complex. Somatosens Mot Res. 29, 1-12. [CrossRef]
- Xu, Y., Lopes, C., Wende, H., Guo, Z., Cheng, L., Birchmeier, C., Ma, Q. (2013). Ontogeny of excitatory spinal neurons processing distinct somatic sensory modalities. J Neurosci. 33, 14738-14748. [CrossRef]
- Draxler, P. , Honsek, S.D., Forsthuber, L., Hadschieff, V., Sandkühler, J. (2014). VGluT3⁺ primary afferents play distinct roles in mechanical and cold hypersensitivity depending on pain etiology. J Neurosci. 34, 12015-12028. [CrossRef]
- Duitama, M. , Vargas-López, V., Casas, Z., Albarracin, S.L., Sutachan, J.J., Torres, Y.P. TRP Channels Role in Pain Associated With Neurodegenerative Diseases. Frontiers in Neuroscience. 2020 Aug 4;14:782. [CrossRef]
- Collo, G. , North, R.A., Kawashima, E., Merlo-Pich, E., Neidhart, S., Surprenant, A., Buell, G. (1996). Cloning of P2X5 and P2X6 receptors and the distribution and properties of an extended family of ATP-gated ion channels. J Neurosci. 16, 2495–2507. [CrossRef]
- Teixeira, J.M. , Bobinski, F., Parada, C.A., Sluka, K.A., Tambeli, C,H. (2017) P2X3 and P2X2/3 receptors play a crucial role in articular hyperalgesia development through infammatory mechanisms in the knee joint experimental synovitis. Mol Neurobiol. 54, 6174-6186. [CrossRef]
- Rau, K. K., Caudle, R. M., Cooper, B. Y., and Johnson, R. D. (2005). Diverse immunocytochemical expression of opioid receptors in electrophysiologically defined cells of rat dorsal root ganglia. J. Chem. Neuroanat. 29, 255–264. [CrossRef]
- Wang, D. , Tawfik, V. L., Corder, G., Low, S. A., François, A., Basbaum, A. I., Scherrer, G. (2018). Functional Divergence of Delta and Mu Opioid Receptor Organization in CNS Pain Circuits. Neuron 98, 90-108.e5. [CrossRef]
- Zhang, X.Y. , Dou, Y.N., Yuan, L., Li, Q., Zhu, Y.J., Wang, M., Sun, Y.G. (2020). Different neuronal populations mediate inflammatory pain analgesia by exogenous and endogenous opioids. Elife. 9:e55289. [CrossRef]
- Tamae, A. , Nakatsuka, T., Koga, K., Kato, G., Furue, H., Katafuchi, T., Yoshimura, M. (2005). Direct inhibition of substantia gelatinosa neurones in the rat spinal cord by activation of dopamine D2-like receptors. J. Physiol. 568, 243–253. [CrossRef]
- Taniguchi, W. , Nakatsuka, T., Miyazaki, N., Yamada, H., Takeda, D., Fujita, T., Kumamoto, E., Yoshida, M. (2011). In vivo patch-clamp analysis of dopaminergic antinociceptive actions on substantia gelatinosa neurons in the spinal cord. Pain 152, 95–105. [CrossRef]
- Lu, Y., Doroshenko, M., Lauzadis, J., Kanjiya, M. P., Rebecchi, M. J., Kaczocha, M., Puopolo, M. (2018). Presynaptic inhibition of primary nociceptive signals to dorsal horn lamina I neurons by dopamine. J. Neurosci. 38, 8809–8821. [CrossRef]
- Almanza, A. , Simón-Arceo, K., Coffeen, U., Fuentes-García, R., Contreras, B., Pellicer, F., et al. (2015). A D2-like receptor family agonist produces analgesia in mechanonociception but not in thermonociception at the spinal cord level in rats. Pharmacol. Biochem. Behav. 137, 119–125. [CrossRef]
- Mercado-Reyes, J., Almanza, A., Segura-Chama, P., Pellicer, F., and Mercado, F. (2019). D2-like receptor agonist synergizes the μ-opioid agonist spinal antinociception in nociceptive, inflammatory and neuropathic models of pain ni ht e art. Eur. .J Pharmacol. 853, 56–64. [CrossRef]
- Ohnou T, Yokai M, Kurihara T, Hasegawa-Moriyama M, Shimizu T, Inoue K, Kambe Y, Kanmura Y, Miyata A (2016). Pituitary adenylate cyclase-activating polypeptide type 1 receptor signaling evokes long-lasting nociceptive behaviors through the activation of spinal astrocytes in mice. J Pharmacol Sci. 130,194-203. [CrossRef]
- Yokai, M., Kurihara, T., and Miyata, A. (2016). Spinal astrocytic activation contributes to both induction and maintenance of pituitary adenylate cyclase-activating polypeptide type 1 receptor-induced longlasting mechanical allodynia in mice. Mol. Pain 12:1744806916646383. [CrossRef]
- Brumovsky, P. , Hygge-Blakeman, K., Villar, M. J., Watanabe, M., Wiesenfeld-Hallin, Z., and Hökfelt, T. (2006). Phenotyping of sensory and sympathetic ganglion neurons of a galanin-overexpressing mouse-Possible implications for pain processing. J. Chem. Neuroanat. 31, 243–262. [CrossRef]
- François, A. , Schüetter, N., Laffray, S., Sanguesa, J., Pizzoccaro, A., Dubel, S., Mantilleri, A., Nargeot, J., Noël, J., Wood, J.N., Moqrich, A., Pongs, O., Bourinet, E. (2015). The Low-Threshold Calcium Channel Cav3.2 Determines Low-Threshold Mechanoreceptor Function. Cell Rep. 10 370-382. [CrossRef]
- Seal, R. P. (2016). Do the distinct synaptic properties of VGLUTs shape pain?. Neurochem. Int. 98, 82–88. [CrossRef]
- Liu, X.J. , Salter, M.W. (2010) Glutamate receptor phosphorylation and trafficking in pain plasticity in spinal cord dorsal horn. Eur J Neurosci. 2010 Jul;32(2):278-89. [CrossRef]
- Todd, A.J., Hughes, D.I., Polgár, E., Nagy, G.G., Mackie, M., Ottersen, O.P., Maxwell, D.J (2003). The expression of vesicular glutamate transporters VGLUT1 and VGLUT2 in neurochemically defined axonal populations in the rat spinal cord with emphasis on the dorsal horn. The European Journal of Neuroscies. 17, 13-27. [CrossRef]
- Alvarez, F.J. , Villalba, R.M., Zerda, R., Schneider, S.P. (2004). Vesicular glutamate transporters in the spinal cord, with special reference to sensory primary afferent synapses. J Comp Neurol. 472(3):257-80. [CrossRef] [PubMed]
- Larsson, M. , and Broman, J. (2019). Synaptic Organization of VGLUT3 Expressing Low-Threshold Mechanosensitive C Fiber Terminals in the Rodent Spinal Cord. eNeuro 6. [CrossRef]
- Deuchars SA, Milligan CJ, Stornetta RL, Deuchars J. (2005). GABAergic neurons in the central region of the spinal cord: a novel substrate for sympathetic inhibition. J Neurosci. 25:1063-70. [CrossRef]
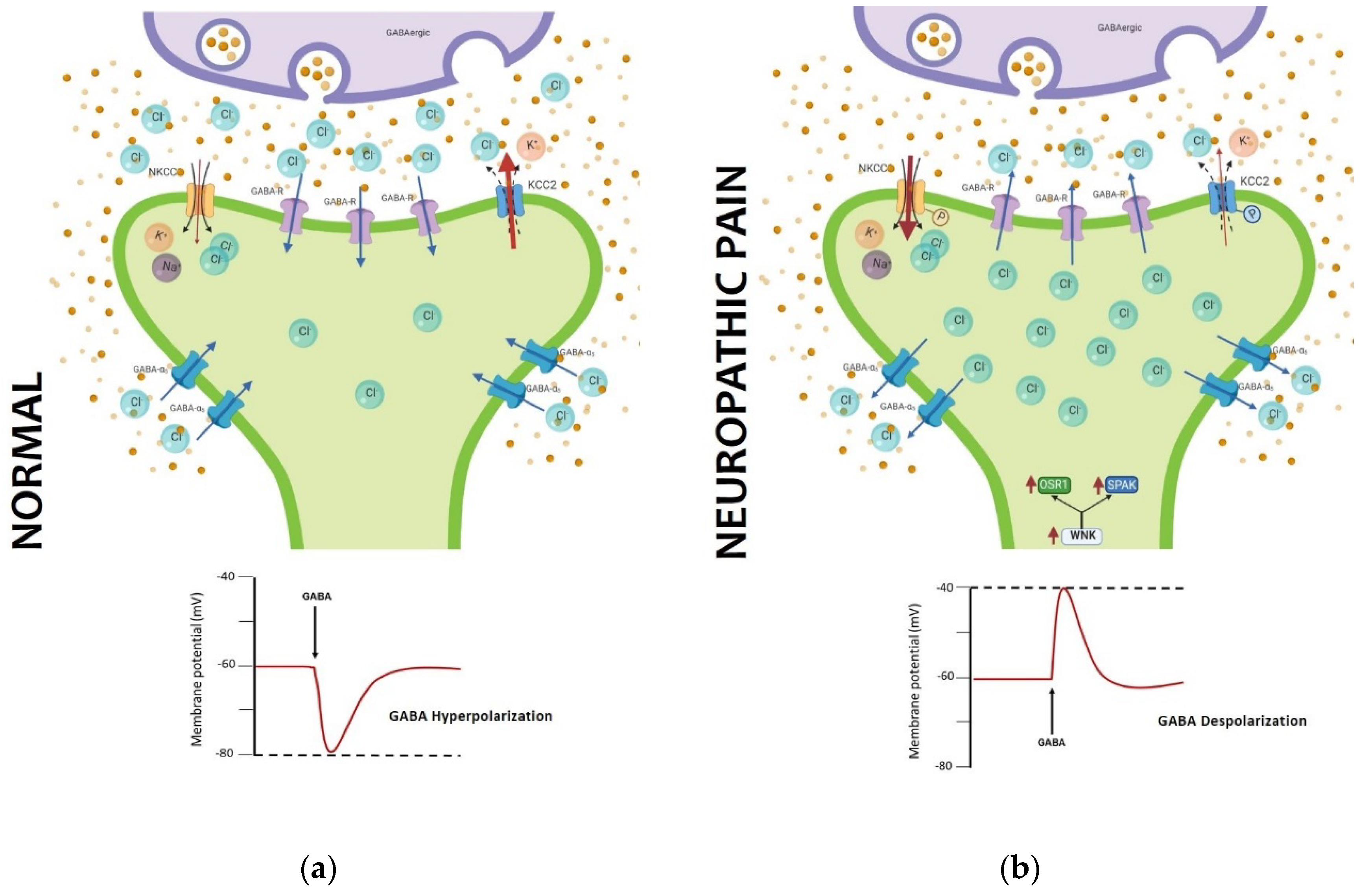
- Coull, J. A. , Boudreau, D., Bachand, K., Prescott, S. A., Nault, F., Sik, A., De Koninck, P., & De Koninck, Y. (2003). Trans-synaptic shift in anion gradient in spinal lamina I neurons as a mechanism of neurophatic pain Nature, 424, 938–942.
- Paul, J., Zeilhofer, H. U., & Fritschy, J. M. (2012). Selective distribution of GABAA receptor subtypes in mouse spinal dorsal horn neurons and primary afferents. Journal of Comparative Neurology, 520, 3895–3911. [CrossRef]
- Kahle, K. T. , Schmouth, J. F., Lavastre, V., Latremoliere, A., Zhang, J., Andrews, N., Omura, T., Laganière, J., Rochefort, D., Hince, P., Castonguay, G., Gaudet, R., Mapplebeck, J.C., Sotocinal, S.G., Duan, J., Ward, C., Khanna, A.R., Mogil, J.S., Dion, P.A., Woolf, C.J., Inquimbert, P., Rouleau, G.A. (2016). Inhibition of the kinase WNK1/HSN2 ameliorates neuropathic pain by restoring GABA inhibition. Sci. Signal. 9, ra32. [CrossRef]
- Lee, H. K., Ahmed, M. M., King, K. C., Miranpuri, G. S., Kahle, K. T., Resnick, D. K., Sun, D. (2014). Persistent phosphorylation of NKCC1 and WNK1 in the epicenter of the spinal cord following contusion injury. Spine J. 14, 777–781. [CrossRef]
- Tillman, L. , Zhang, J. Crossing the Chloride Channel: The Current and Potential Therapeutic Value of the Neuronal K+-Cl- Cotransporter KCC2. Biomed Res Int. 2019 ;2019:8941046. 21 May. [CrossRef]
- Deisseroth, K. , Feng, G., Majewska, A. K., Miesenböck, G., Ting, A., and Schnitzer, M. J. (2006). Next-Generation Optical Technologies for Illuminating Genetically Targeted Brain Circuits. J Neurosci. 26, 10380-10386. [CrossRef]
- Deisseroth, K. , and Hegemann, P. (2017). The form and function of channelrhodopsin. Science 15,357:6356. [CrossRef]
- Boyden, E. S. , Zhang, F., Bamberg, E., Nagel, G., and Deisseroth, K. (2005). Millisecond-timescale, genetically targeted optical control of neural activity. Nat. Neurosci. 8, 1263–1268. [CrossRef]
- Chow, B. Y., Han, X., Dobry, A. S., Qian, X., Chuong, A. S., Li, M., Henninger, M.A., Belfort, G.M., Lin, Y., Monahan, P.E., Boyden, E.S. (2010). High-performance genetically targetable optical neural silencing by light-driven proton pumps. Nat. 2010 4637277 463, 98–102. [CrossRef]
- Han, X. , Chow, B. Y., Zhou, H., Klapoetke, N. C., Chuong, A., Rajimehr, R., Yang, A,. Baratta, M.V., Winkle, J., Desimone, R., Boyden, E.S. (2011). A high-light sensitivity optical neural silencer: Development and application to optogenetic control of non-human primate cortex. Front. Syst. Neurosci. 5, 18. [CrossRef]
- Watakabe, A., Sadakane, O., Hata, K., Ohtsuka, M., Takaji, M., Yamamori, T. (2017). Application of viral vectors to the study of neural connectivities and neural circuits in the marmoset brain. Dev Neurobiol. 77, 354-372. (. [CrossRef]
- Anastassiadis, K. , Fu, J., Patsch, C., Hu, S., Weidlich, S., Duerschke, K., Buchholz, F., Edenhofer, F., Stewart, A.F. (2009). Dre recombinase, like Cre, is a highly efficient site-specific recombinase in E. coli, mammalian cells and mice. Disease models & mechanisms. 9,508-515. [CrossRef]
- Daou, I., Tuttle, A. H., Longo, G., Wieskopf, J. S., Bonin, R. P., Ase, A. R., et al. (2013). Remote Optogenetic Activation and Sensitization of Pain Pathways in Freely Moving Mice. 33, 18631–18640. [CrossRef]
- Michoud, F., Seehus, C., Schönle, P., Brun, N., Taub, D., Zhang, Z., Jain, A., Furfaro, I., Akouissi, O., Moon, R., Meier, P., Galan, K., Doyle, B., Tetreault, M., Talbot, S., Browne, L.E., Huang, Q., Woolf, C.J., Lacour, S.P. (2021). Epineural optogenetic activation of nociceptors initiates and amplifies inflammation. Nat. Biotechnol. 39, 179–185. [CrossRef]
- Wang, L. , Chen, S. R., Ma, H., Chen, H., Hittelman, W. N., and Pan, H. L. (2018). Regulating nociceptive transmission by VGluT2-expressing spinal dorsal horn neurons. J. Neurochem. 147, 526–540. [CrossRef]
- Iyer, S. M. , Montgomery, K. L., Towne, C., Lee, S. Y., Ramakrishnan, C., Deisseroth, K., Delp, S.L. (2014). Virally mediated optogenetic excitation and inhibition of pain in freely moving nontransgenic mice. Nat. Biotechnol. 32, 274–278. [CrossRef]
- Iyer, S. M. , Vesuna, S., Ramakrishnan, C., Huynh, K., Young, S., Berndt, A., Lee, S.Y., Gorini, C.J., Deisseroth, K., Delp, S.L. (2016). Optogenetic and chemogenetic strategies for sustained inhibition of pain. Sci. Rep. 6, 1–10. [CrossRef]
- Tashima, R. , Koga, K., Sekine, M., Kanehisa, K., Kohro, Y., Tominaga, K., Matsushita, K., Tozaki-Saitoh, H., Fukazawa, Y., Inoue, K., Yawo, H., Furue, H., Tsuda, M. (2018). Optogenetic Activation of Non-Nociceptive Aβ Fibers Induces Neuropathic Pain-Like Sensory and Emotional Behaviors after Nerve Injury in Rats. eNeuro. 5, ENEURO.0450-17.2018.
- Boada, M. D. , Martin, T. J., Peters, C. M., Hayashida, K., Harris, M. H., Houle, T. T., et al. (2014). Fast-conducting mechanoreceptors contribute to withdrawal behavior in normal and nerve injured rats. Pain 155, 2646–2655. [CrossRef]
- Cavanaugh, D. J., Lee, H., Lo, L., Shields, S. D., Zylka, M. J., Basbaum, A. I., Anderson, D.J. (2009). Distinct subsets of unmyelinated primary sensory fibers mediate behavioral responses to noxious thermal and mechanical stimuli. Proc. Natl. Acad. Sci. U. S. A. 106, 9075–9080. [CrossRef]
- Armbruster, B. N. , Li, X., Pausch, M. H., Herlitze, S., and Roth, B. L. (2007). Evolving the lock to fit the key to create a family of G protein-coupled receptors potently activated by an inert ligand. Proc. Natl. Acad. Sci. 104, 5163–5168. [CrossRef]
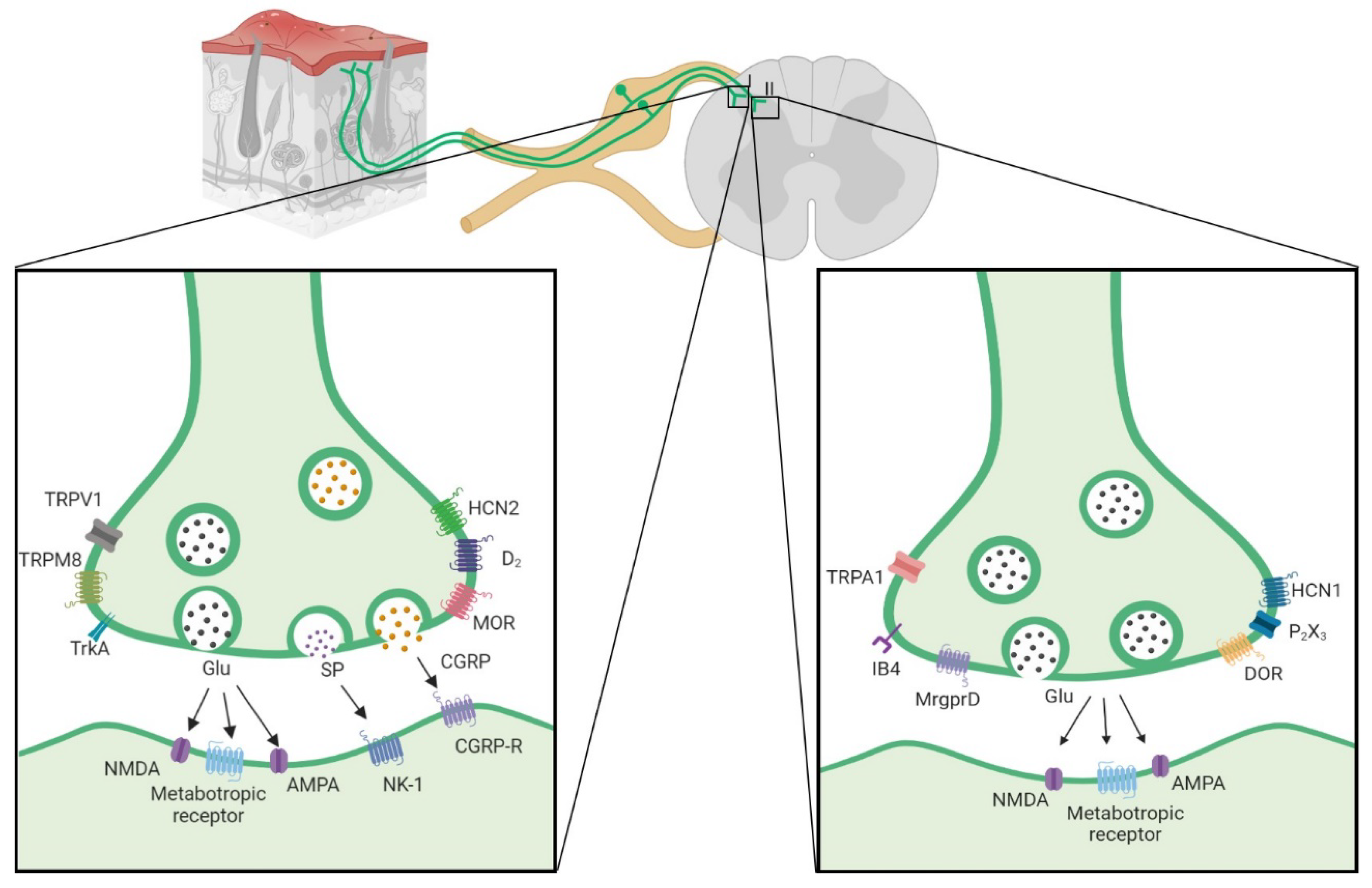
| Fiber Type | Conduction velocity | Vesiculator type | Protein Markers | Channels | Membrane receptors | Dorsal Laminar distribution | Transcription factor | References | |
|---|---|---|---|---|---|---|---|---|---|
| Aβ | 30-80 m/s | Vglut 1 | NF200 Thy-1 parvalbumin Caderina SPP1 NEFH |
Nav1.1 Nav1.6 HCN3 ASIC1 Nav1.8 |
DOR TrkC |
III, IV, V | RunX3 ETV1 Etv4 Cdh12 |
[4-8,11,12,24-32] | |
| Aδ | 5-25 m/s | Vglut 2 | NF200 NEFH CGRP Substance P |
TRPM8 Nav 1.8 HCN1 HCN3 Cav 3.2 |
TrkA TRKB MOR DOR |
I, II | CNTNAP2 FAM19A RET |
[5,11,12,24- 29,31-35] |
|
| C | Peptidergic | 0.5-2 m/s | Vglut 2 | Substance P CGRP Cdk 5mTOR |
TRPV1 TRPA1 TRPM8 Nav1.7 Nav1.8 HCN2 HCN3 |
D2 MOR MrgprA3 mGlu2 Ntrk1 PAC1 TrkA Y1R Y2R |
I | cMAF GDNF HOB8 LMBX1 RET TAC1 |
[5,6,21-26,29,30,36-44] |
| Non-peptidergiC | 0.5-2 m/s | Vglut 2 | IB4 Cdk 5mTOR |
TRPA1 TRPM3 TRPC3 Nav1.7 Nav1.8 Nav1.9 HCN1 HCN3 P2X3 |
DOR MrgprA3 MrgprB4 MrgprD Y1R Y2R |
II | GfrA1 LMBX1 NGF PLXNC1 RET RunX |
[5,6,11,21,23,24,25, 28- 30,35,36-38,43-45] |
|
| LTMR | <0.5 m/s | Vglut 3 | TH | TRPM8 Nav 1.8 Nav 1.9 |
TrkB | I, II, III | GfrA2 PIEZO2 RET |
[12,25,28,29,35,45] | |
| Specificity strategy | Construct | Fiber and Cell type | Injection site | Place of stimulation | Behavioral phenotype | Painful condition | Reference | |
| Cre dependent |
Nav1.8 ::Cre / Ai32 ( carry the ChR2(H134R)–EYFP in Gt(ROSA)26Sor locus ) Product: Nav1.8–ChR2+ |
Aβ Fiber Aδ Fiber C- fibers: -Peptidergic and -nonpeptidergic |
NA | The plantar surface of the hindpaw blue light (473 nm) |
paw withdrawal and paw licking | Not sensitized |
[79] | |
|
TRPV1::Cre / AAV5-TRPV1-ArchT-eGFP Product: TRPV1-Arch+ |
C-fiber Peptidergic |
DRG injection | The plantar surface of the hindpaw Green light (532 nm) |
Increases in mechanical withdrawal threshold and thermal latency | [19] | |||
|
TRPV1::Cre / AAV2/8-CAG-floxed stop-ChR2[H134R]-tdTomato-WPRE Product: TRPV1-ChR2 |
C-fiber Peptidergic |
Intrathecal | The plantar surface of the hindpaw Blue light (473 nm) |
Increases in paw withdrawal, paw lifting and paw licking | [23] | |||
|
TRPV1::Cre/Ai27D (carry Rosa-CAG-LSL-hChR2(H134R)-tdTomato-WPRE) Product: TRPV1-ChR2 |
C-fiber Peptidergic |
NA | Epineural in sciatic nerve Blue light (470 nm) |
Thermal and mechanical sensitivity | [80] | |||
|
MrgD::CreERT2 / Ai32 (carry in the ROSA26 locus the floxed stop-ChR2(H134R)-EYFP) Product: MrgD-ChR2 (Opsin induced by tamoxiofen) |
C-fiber Nonpeptidergic |
NA | The plantar surface of the hindpaw Blue light (473 nm) |
Paw withdrawal and lifting. | [23] | |||
|
VGluT2::Cre / AAV8-hSyn-DIO-hM3Dq-mCherry Product: VGluT2- hM3D-Gq |
C-fiber: -Peptidergic and –nonpeptidergic (Vglut2-dorsal horn) |
Dorsal horn of the spinal cord | clozapine N-oxide intraperitoneally | Increases in mechanical and thermal sensitivities | [81] | |||
| No Cre dependent | AAV6-hSyn-ChR2-eYFP Product: Chr2-eYFP |
C- fiber: -Unmyelinated primary afferent |
intrasciatic | The plantar Surface Blue light (473 nm) |
Decreases in paw withdrawal Place aversion |
[82] |
||
| AAV6-hSyn-SwiChR-eYFP Product: SwiChR-eYFP |
C- fiber: -Unmyelinated primary afferent |
intraneural | The plantar surface of the hindpaw Blue light (473 nm) |
Increases in mechanical withdrawal threshold and thermal withdrawal latency | [83] | |||
| AAV6-hSyn-biC1C2-TS-eYFP Product: iC1C2-eYFP |
C- fiber: -Unmyelinated primary afferent |
intraneural | The plantar surface of the hindpaw Blue light (473 nm) |
Increases in mechanical withdrawal threshold and thermal withdrawal latency | [83] |
|||
| AAV6-hSyn-eNpHR3.0-eYFP |
C- fiber: -Unmyelinated primary afferent |
Intrasciatic | The plantar Surface Yellow light (590 nm) |
Increases in mechanical withdrawal threshold and thermal withdrawal latency | [82] |
|||
| AAV6-hSyn-HA-HM4D(Gi)-IRES-mCitrine Product:hM4D-Gi |
C- fiber: -Unmyelinated primary afferent |
Intraneural | Clozapine-N-oxide intraperitoneally |
Increases in mechanical withdrawal threshold and thermal withdrawal latency | [83] |
|||
| Cre-dependetn |
VGluT3::Cre/Ai32 carry ChR2 Product: VGluT3-ChR2 |
LTMR Fiber: VGluT3+ |
NA | The plantar surface of the hindpaw Blue light (470 nm) |
Elicit nociceptive behaviour |
sensitized |
Oxaliplatin-induced neuropathy | [45] |
|
Nav1.8::Cre / Ai35 (carry the floxed stop-Arch-EGFP gene in the ROSA26 locus) Product: Nav1.8-Arch+ |
C-fiber Peptidergic |
NA | The plantar surface of the hindpaw yellow light |
Decrease in mechanical allodynia |
Spared nerve injury | [39] | ||
|
VGluT2::Cre / AAV8-hSyn-DIO-HA-KORD-IRES-mCitrine Product: VGluT2-KORD-Gi |
Peptidergic and nonpeptidergic (Vglut2-dorsal horn) |
Dorsal horn of the spinal cord | Salvinorin B intraperitoneal | Decrease in tactile allodynia / Decrease in pain hipersensibility |
SNI / CFA | [81] | ||
| Thy1-COP4/YFP / W-TChR2V4 | Aβ fibers | NA | The plantar surface of the hindpaw Yellow light |
Lifting and flinching behaviors. | PNI | [84] | ||
| No Cre-dependetn |
AAV6-hSyn-SwiChR-eYFP Product: SwiChR-eYFP |
C-fiber: Unmyelinated primary afferent |
intrasciatic | The plantar surface of the hindpaw Blue light (473 nm) |
Reduced pain behavior in phase I | Formalin test | [83] | |
| AAV6-hSyn-eNpHR3.0-eYFP Product: eNpHR-eYFP |
C-fiber unmyelinated primary afferent |
intraneural | The plantar surface of the hindpaw Yellow light (490 nm) |
Reduction of mechanical allodynia and thermal hyperalgesia | CCI | [82] | ||
| AAV8/CAG-ArchT-GFP In myelinated neurons. Product: ArchT-GFP |
AHTMR-fiber myelinated primary afferent |
intrathecal | The plantar surface of the hindpaw Green light |
Increase in paw withdrawal threshold | SNL | [85] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





