Submitted:
02 March 2023
Posted:
07 March 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
Mycobacterium avium subsp. paratuberculosis (MAP)
MAP Is Difficult to Detect
Sarcoid Epidemiology
Genetic Risk for Sarcoidosis Overlaps with Risk for Mycobacterial Infection
SLC11a1 (NRAMP) and Sarcoidosis
HLA Alleles and Sarcoidosis/Tuberculosis Risk
CARD15 (NOD2)–Early Onset Sarcoidosis (EOS) and Blau Syndrome
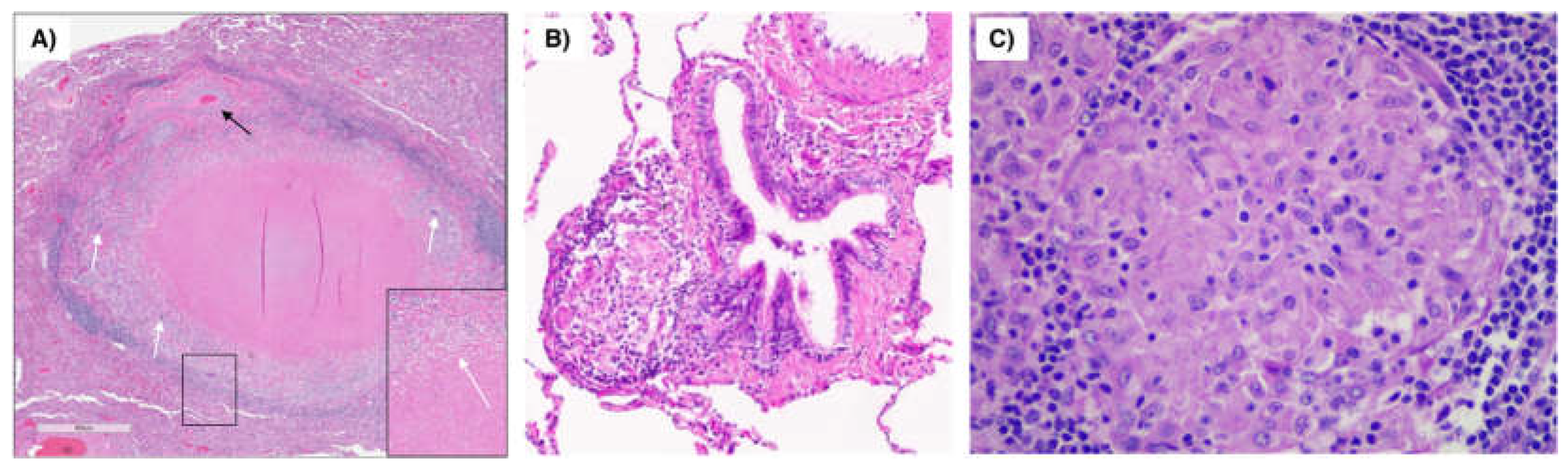
An Illustrative Case of Cardiac Sarcoidosis
2. Discussion
Author Contributions
Abbreviations
References
- Spagnolo, P. Sarcoidosis: a Critical Review of History and Milestones. Clin Rev Allergy Immunol. 2015,49,1-5. [CrossRef]
- Gupta, D. Tuberculosis and sarcoidosis: The continuing enigma. Lung India. 2009,26,1-2. [CrossRef]
- Howell, J.D. Early Clinical Use Of The X-Ray. Trans Am Clin Climatol Assoc. 2016,127,341-49.
- Citron, K.M.;Scadding, J.G. Stenosing non-caseating tuberculosis (sarcoidosis) of the bronchi. Thorax. 1957,12,10-17. [CrossRef]
- Rook, G.A.;Stanford, J.L. Slow bacterial infections or autoimmunity? Immunol Today. 1992,13,160-64.
- Gupta, D.; Agarwal, R.; Aggarwal, A.N.;Jindal, S.K. Molecular evidence for the role of mycobacteria in sarcoidosis: a meta-analysis. Eur Respir J. 2007,30,508-16. [CrossRef]
- Brownell, I.; Ramírez-Valle, F.; Sanchez, M.;Prystowsky, S. Evidence for mycobacteria in sarcoidosis. Am J Respir Cell Mol Biol. 2011,45,899-905. [CrossRef]
- Chapman, J.S.;Speight, M. Further studies of mycobacterial antibodies in the sera of sarcoidosis patients. Acta Med Scand. 1964,Suppl 425,61-67. [CrossRef]
- Berger, H.W.; Zaldivar, C.;Chusid, E.L. Anonymous mycobacteria in the etiology of sarcoidosis. Ann Intern Med. 1968,68,872-74. [CrossRef]
- el-Zaatari, F.A.; Naser, S.A.; Markesich, D.C.; Kalter, D.C.; Engstand, L.;Graham, D.Y. Identification of Mycobacterium avium complex in sarcoidosis. J Clin Microbiol. 1996,34,2240-45. [CrossRef] [PubMed]
- Llanos, O.;Hamzeh, N. Sarcoidosis. Med Clin North Am. 2019,103,527-34.
- Mehta, A.C.;Ali, S.R. Mnemonic for the differential diagnosis of non-caseating granulomas. Sarcoidosis Vasc Diffuse Lung Dis. 2017,34,200-07. [CrossRef]
- Jeyanathan, M.; Alexander, D.C.; Turenne, C.Y.; Girard, C.;Behr, M.A. Evaluation of in situ methods used to detect Mycobacterium avium subsp. paratuberculosis in samples from patients with Crohn’s disease. J Clin Microbiol. 2006,44,2942-50. [CrossRef]
- Sechi, L.A.;Dow, C.T. Mycobacterium avium ss. paratuberculosis Zoonosis - The Hundred Year War - Beyond Crohn’s Disease. Front Immunol. 2015,6,96. [CrossRef]
- Naser, S.A.; Ghobrial, G.; Romero, C.;Valentine, J.F. Culture of Mycobacterium avium subspecies paratuberculosis from the blood of patients with Crohn’s disease. . Lancet. 2004,364,1039-44. [CrossRef] [PubMed]
- Naser, S.A.; Schwartz, D.;Shafran, I. Isolation of Mycobacterium avium subsp paratuberculosis from breast milk of Crohn’s disease patients. Am J Gastroenterol. 2000,95,1094-95. [CrossRef]
- Chiodini, R.J. Crohn’s disease and the mycobacterioses: a review and comparison of two disease entities. . Clin Microbiol Rev. 1989,2,90-117. [CrossRef]
- Reid, J.D.;Chiodini, R.J. Serologic reactivity against Mycobacterium paratuberculosis antigens in patients with sarcoidosis. Sarcoidosis. 1993,10,32-35.
- Biet, F.; Boschiroli, M.L.; Thorel, M.F.;Guilloteau, L.A. Zoonotic aspects of Mycobacterium bovis and Mycobacterium avium-intracellulare complex (MAC). Vet Res. 2005,36,411-36. [CrossRef]
- Whittington, R.J.;Sergeant, E.S. Progress towards understanding the spread, detection and control of Mycobacterium avium subsp paratuberculosis in animal populations. Aust Vet J. 2001,79,267-78. [CrossRef]
- Lombard, J.E.; Gardner, I.A.; Jafarzadeh, S.R.; Fossler, C.P.; Harris, B.; Capsel, R.T.; Wagner, B.A.;Johnson, W.O. Herd-level prevalence of Mycobacterium avium subsp. paratuberculosis infection in United States dairy herds in 2007. Prev Vet Med. 2013,108,234-38. [CrossRef]
- Garvey, M. Mycobacterium avium paratuberculosis: A Disease Burden on the Dairy Industry. . Animals (Basel). 2020,10,1773. [CrossRef] [PubMed]
- Beumer, A.; King, D.; Donohue, M.; Mistry, J.; Covert, T.;Pfaller, S. Detection of Mycobacterium avium subsp. paratuberculosis in drinking water and biofilms by quantitative PCR. Appl Environ Microbiol. 2010,76,7367-70. [CrossRef]
- Fridriksdottir, V.; Gunnarsson, E.; Sigurdarson, S.;Gudmundsdottir, K.B. Paratuberculosis in Iceland: epidemiology and control measures, past and present. Vet Microbiol. 2000,77,263-67. [CrossRef] [PubMed]
- Whittington, R.J.; Taragel, C.A.; Ottaway, S.; Marsh, I.; Seaman, J.;Fridriksdottir, V. Molecular epidemiological confirmation and circumstances of occurrence of sheep (S) strains of Mycobacterium avium subsp. paratuberculosis in cases of paratuberculosis in cattle in Australia and sheep and cattle in Iceland. Vet Microbiol. 2001,79,311-22. [CrossRef]
- Dow, C.T.;Alvarez, B.L. Mycobacterium paratuberculosis zoonosis is a One Health emergency. . Ecohealth. 2022,19,164-74. [CrossRef] [PubMed]
- Chamberlin, W.; Borody, T.;Naser, S. MAP-associated Crohn’s disease MAP, Koch’s postulates, causality and Crohn’s disease. Dig Liver Dis. 2007,39,792-94. [CrossRef]
- Hansen, R.; Thomson, J.M.; El-Omar, E.M.;Hold, G.L. The role of infection in the aetiology of inflammatory bowel disease. J Gastroenterol. 2010,45,266-76. [CrossRef] [PubMed]
- Harris, N.B.;Barletta, R.G. Mycobacterium avium subsp. paratuberculosis in Veterinary Medicine. . Clin Microbiol Rev. 2001,14,489-512. [CrossRef]
- Hines, M.E., 2nd.;Styer, E.L. Preliminary characterization of chemically generated Mycobacterium avium subsp. paratuberculosis cell wall deficient forms (spheroplasts). Vet Microbiol. 2003,95,247-58. [CrossRef]
- Lamont, E.A.; Bannantine, J.P.; Armién, A.; Ariyakumar, D.S.;Sreevatsan, S. Identification and characterization of a spore-like morphotype in chronically starved Mycobacterium avium subsp. paratuberculosis cultures. PLoS One. 2012,7,e30648. [CrossRef]
- Waddell, L.; Rajić, A.; Stärk, K.;McEwen, S.A. Mycobacterium avium ssp. paratuberculosis detection in animals, food, water and other sources or vehicles of human exposure: A scoping review of the existing evidence. . Prev Vet Med. 2016,132,32-48. [CrossRef]
- Mullan, W. Are we closer to understanding why viable cells of Mycobacterium avium subsp. paratuberculosis are still being reported in pasteurised milk? Int J Dairy Technol. 2019,72,332–44. [CrossRef]
- Gill, C.O.; Saucier, L.;Meadus, W.J. Mycobacterium avium subsp. paratuberculosis in dairy products, meat, and drinking water. J Food Prot. 2011,74,480-99. [CrossRef]
- Eltholth, M.M.; Marsh, V.R.; Van Winden, S.;Guitian, F.J. Contamination of food products with Mycobacterium avium paratuberculosis: a systematic review. J Appl Microbiol. 2009,107,1061-71. [CrossRef] [PubMed]
- Van Brandt, L.; Coudijzer, K.; Herman, L.; Michiels, C.; Hendrickx, M.;Vlaemynck, G. Survival of Mycobacterium avium ssp. paratuberculosis in yoghurt and in commercial fermented milk products containing probiotic cultures. . J Appl Microbiol. 2011,110,1252-61. [CrossRef]
- Alonso-Hearn, M.; Molina, E.; Geijo, M.; Vazquez, P.; Sevilla, I.; Garrido, J.M.;Juste, R.A. Isolation of Mycobacterium avium subsp. paratuberculosis from muscle tissue of naturally infected cattle. Foodborne Pathog Dis. 2009,6,513-18. [CrossRef]
- Hammer, P.; Walte, H.G.; Matzen, S.; Hensel, J.;Kiesner, C. Inactivation of Mycobacterium avium subsp. paratuberculosis during cooking of hamburger patties. J Food Prot. 2013,76,1194-201. [CrossRef] [PubMed]
- Hruska, K.; Bartos, M.; Kralik, P.;Pavlik, I. Mycobacterium avium subsp. paratuberculosis in powdered infant milk: Paratuberculosis in cattle—The public health problem to be solved. Vet Med. 2005,50,327–35.
- Hruska, K.; Slana, I.; Kralik, P.;Pavlik, I. Mycobacterium avium subsp. paratuberculosis in powdered infant milk: F57 competitive real time PCR. Vet Med. 2011,56,226–30. [CrossRef]
- Botsaris, G.; Swift, B.M.; Slana, I.; Liapi, M.; Christodoulou, M.; Hatzitofi, M.; Christodoulou, V.;Rees, C.E. Detection of viable Mycobacterium avium subspecies paratuberculosis in powdered infant formula by phage-PCR and confirmed by culture. Int J Food Microbiol. 2016,216,91-94. [CrossRef] [PubMed]
- Sung, N.;Collins, M.T. Effect of three factors in cheese production (pH, salt, and heat) on Mycobacterium avium subsp. paratuberculosis viability. Appl Environ Microbiol. 2000,66,1334-39. [CrossRef] [PubMed]
- Spahr, U.;Schafroth, K. Fate of Mycobacterium avium subsp. paratuberculosis in Swiss hard and semihard cheese manufactured from raw milk. . Appl Environ Microbiol. 2001,67,4199-205. [CrossRef]
- Donaghy, J.A.; Totton, N.L.;Rowe, M.T. Persistence of Mycobacterium paratuberculosis during manufacture and ripening of cheddar cheese. Appl Environ Microbiol. 2004,70,4899-905. [CrossRef]
- Galiero, A.; Fratini, F.; Mataragka, A.; Turchi, B.; Nuvoloni, R.; Ikonomopoulos, J.;Cerri, D. Detection of Mycobacterium avium subsp. paratuberculosis in cheeses from small ruminants in Tuscany. Int J Food Microbiol. 2016,217,195-99. [CrossRef]
- Barsi, F.; Dalzini, E.; Russo, S.; Cosciani-Cunico, E.; Monastero, P.; Arrigoni, N.; Garbarino, C.A.; Cortimiglia, C.; Losio, M.N.;Ricchi, M. Isothermal inactivation of Mycobacterium avium subsp. paratuberculosis in curd simulating the stretching phase in pasta-filata cheese process. Front Microbiol. 2022,13,1052222. [CrossRef]
- Dow, C.T.;Sechi, L.A. Cows Get Crohn’s Disease and They’re Giving Us Diabetes. Microorganisms. 2019,7,466. [CrossRef]
- Ekundayo, T.C.;Okoh, A.I. Systematic Assessment of Mycobacterium avium Subspecies Paratuberculosis Infections from 1911-2019: A Growth Analysis of Association with Human Autoimmune Diseases. Microorganisms. 2020,8,1212. [CrossRef]
- Dow, C.T. M. paratuberculosis Heat Shock Protein 65 and Human Diseases: Bridging Infection and Autoimmunity. Autoimmune Dis. 2012,2012,150824. [CrossRef] [PubMed]
- Arkema, E.V.;Cozier, Y.C. Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Curr Opin Pulm Med. 2020,26,527-34. [CrossRef]
- Hena, K.M. Sarcoidosis Epidemiology: Race Matters. Front Immunol. 2020,11,537382. [CrossRef]
- Erdal, B.S.; Clymer, B.D.; Yildiz, V.O.; Julian, M.W.;Crouser, E.D. Unexpectedly high prevalence of sarcoidosis in a representative U.S. Metropolitan population. Respir Med. 2012,106,893-99. [CrossRef] [PubMed]
- Yoon, H.Y.; Kim, H.M.; Kim, Y.J.;Song, J.W. Prevalence and incidence of sarcoidosis in Korea: a nationwide population-based study. Respir Res. 2018,19,158. [CrossRef] [PubMed]
- Fidler, L.M.; Balter, M.; Fisher, J.H.; To, T.; Stanbrook, M.B.;Gershon, A. Epidemiology and health outcomes of sarcoidosis in a universal healthcare population: a cohort study. Eur Respir J. 2019,54,1900444. [CrossRef]
- Seedahmed, M.I.; Baugh, A.D.; Albirair, M.T.; Luo, Y.; Chen, J.; McCulloch, C.E.; Whooley, M.A.; Koth, L.L.;Arjomandi, M. Epidemiology of Sarcoidosis in U.S. Veterans from 2003 to 2019. Ann Am Thorac Soc. 2023,E-pub. [CrossRef]
- Rossides, M.; Grunewald, J.; Eklund, A.; Kullberg, S.; Di Giuseppe, D.; Askling, J.;Arkema, E.V. Familial aggregation and heritability of sarcoidosis: a Swedish nested case-control study. Eur Respir J.52,1800385. [CrossRef]
- Swigris, J.J.; Olson, A.L.; Huie, T.J.; Fernandez-Perez, E.R.; Solomon, J.; Sprunger, D.;Brown, K.K. Sarcoidosis-related mortality in the United States from 1988 to 2007. Am J Respir Crit Care Med. 2011,183,1524-30. [CrossRef]
- Dubaniewicz, A.; Jamieson, S.E.; Dubaniewicz-Wybieralska, M.; Fakiola, M.; Miller, E.N.;Blackwell, J.M. Association between SLC11A1 (formerly NRAMP1) and the risk of sarcoidosis in Poland. Eur J Hum Genet. 2005,13,829-34. [CrossRef]
- Canonne-Hergaux, F.; Gruenheid, S.; Govoni, G.;Gros, P. The Nramp1 protein and its role in resistance to infection and macrophage function. Proc Assoc Am Physicians. 1999,111,283-89. [CrossRef]
- Lapham, A.S.; Phillips, E.S.;Barton, C.H. Transcriptional control of Nramp1: a paradigm for the repressive action of c-Myc. Biochem Soc Trans. 2004,32(Pt 6),1084-86. [CrossRef] [PubMed]
- Wyllie, S.; Seu, P.;Goss, J.A. The natural resistance-associated macrophage protein 1 Slc11a1 (formerly Nramp1) and iron metabolism in macrophages. Microbes Infect. 2002,4,351-59. [CrossRef] [PubMed]
- Hackam, D.J.; Rotstein, O.D.; Zhang, W.; Gruenheid, S.; Gros, P.;Grinstein, S. Host resistance to intracellular infection: mutation of natural resistance-associated macrophage protein 1 (Nramp1) impairs phagosomal acidification. J Exp Med. 1998,188,351-64. [CrossRef] [PubMed]
- Stienstra, Y.; van der Werf, T.S.; Oosterom, E.; Nolte, I.M.; van der Graaf, W.T.; Etuaful, S.; Raghunathan, P.L.; Whitney, E.A.; Ampadu, E.O.; Asamoa, K.; et al. Susceptibility to Buruli ulcer is associated with the SLC11A1 (NRAMP1) D543N polymorphism. Genes Immun. 2006,7,185-89. [CrossRef]
- Brochado, M.J.; Gatti, M.F.; Zago, M.A.;Roselino, A.M. Association of the solute carrier family 11 member 1 gene polymorphisms with susceptibility to leprosy in a Brazilian sample. Mem Inst Oswaldo Cruz. 2016,111,101-05. [CrossRef] [PubMed]
- Hu, B.; Wang, Y.; Wang, Z.; He, X.; Wang, L.; Yuan, D.; He, Y.; Jin, T.;He, S. Association of SLC11A1 Polymorphisms With Tuberculosis Susceptibility in the Chinese Han Population. Front Genet. 2022,13,899124. [CrossRef]
- Shahzad, F.; Bashir, N.; Ali, A.; Nadeem, A.; Ammar, A.; Kashif, M.; Javaid, K.; Jahan, S.; Tahir, R.; Rizwan, M.; et al. SLC11A1 genetic variation and low expression may cause immune response impairment in TB patients. Genes Immun. 2022,23,85-92. [CrossRef] [PubMed]
- Ruiz-Larrañaga, O.; Garrido, J.M.; Manzano, C.; Iriondo, M.; Molina, E.; Gil, A.; Koets, A.P.; Rutten, V.P.; Juste, R.A.;Estonba, A. Identification of single nucleotide polymorphisms in the bovine solute carrier family 11 member 1 (SLC11A1) gene and their association with infection by Mycobacterium avium subspecies paratuberculosis. J Dairy Sci. 2010,93,1713-21. [CrossRef]
- Korou, L.M.; Liandris, E.; Gazouli, M.;Ikonomopoulos, J. Investigation of the association of the SLC11A1 gene with resistance/sensitivity of goats (Capra hircus) to paratuberculosis. . Vet Microbiol. 2010,144,353-58. [CrossRef]
- Purdie, A.C.; Plain, K.M.; Begg, D.J.; de Silva, K.;Whittington, R.J. Candidate gene and genome-wide association studies of Mycobacterium avium subsp. paratuberculosis infection in cattle and sheep: a review. Comp Immunol Microbiol Infect Dis. 2011,34,197-208. [CrossRef]
- Roupie, V.; Rosseels, V.; Piersoel, V.; Zinniel, D.K.; Barletta, R.G.;Huygen, K. Genetic resistance of mice to Mycobacterium paratuberculosis is influenced by Slc11a1 at the early but not at the late stage of infection. Infect Immun. 2008,76,2099-105. [CrossRef]
- Ates, O.; Dalyan, L.; Müsellim, B.; Hatemi, G.; Türker, H.; Ongen, G.; Hamuryudan, V.;Topal-Sarikaya, A. NRAMP1 (SLC11A1) gene polymorphisms that correlate with autoimmune versus infectious disease susceptibility in tuberculosis and rheumatoid arthritis. Int J Immunogenet. 2009,36,15-19. [CrossRef] [PubMed]
- Sechi, L.A.; Gazouli, M.; Sieswerda, L.E.; Molicotti, P.; Ahmed, N.; Ikonomopoulos, J.; Scanu, A.M.; Paccagnini, D.;Zanetti, S. Relationship between Crohn’s disease, infection with Mycobacterium avium subspecies paratuberculosis and SLC11A1 gene polymorphisms in Sardinian patients. World J Gastroenterol. 2006,12,7161-64. [CrossRef]
- Kotlowski, R.; Bernstein, C.N.; Silverberg, M.S.;Krause, D.O. Population-based case-control study of alpha 1-antitrypsin and SLC11A1 in Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2008,14,1112-17. [CrossRef]
- Kotze, M.J.; de Villiers, J.N.; Rooney, R.N.; Grobbelaar, J.J.; Mansvelt, E.P.; Bouwens, C.S.; Carr, J.; Stander, I.;du Plessis, L. Analysis of the NRAMP1 gene implicated in iron transport: association with multiple sclerosis and age effects. Blood Cells Mol Dis. 2001,27,44-53. [CrossRef]
- Takahashi, K.; Satoh, J.; Kojima, Y.; Negoro, K.; Hirai, M.; Hinokio, Y.; Kinouchi, Y.; Suzuki, S.; Matsuura, N.; Shimosegawa, T.; et al. Promoter polymorphism of SLC11A1 (formerly NRAMP1) confers susceptibility to autoimmune type 1 diabetes mellitus in Japanese. Tissue Antigens. 2004,63,231-36. [CrossRef]
- Malkova, A.; Starshinova, A.; Zinchenko, Y.; Basantsova, N.; Mayevskaya, V.; Yablonskiy, P.;Shoenfeld, Y. The opposite effect of human leukocyte antigen genotypes in sarcoidosis and tuberculosis: a narrative review of the literature. ERJ Open Res. 2020,6,00155-2020. [CrossRef]
- Grunewald, J.; Spagnolo, P.; Wahlström, J.;Eklund, A. Immunogenetics of Disease-Causing Inflammation in Sarcoidosis. Clin Rev Allergy Immunol. 2015,49,19-35. [CrossRef]
- Saltini, C.; Pallante, M.; Puxeddu, E.; Contini, S.; Voorter, C.E.; Drent, M.;Amicosante, M. M. avium binding to HLA-DR expressed alleles in silico: a model of phenotypic susceptibility to sarcoidosis. . Sarcoidosis Vasc Diffuse Lung Dis. 2008,25,100-16.
- Rossman, M.D.; Thompson, B.; Frederick, M.; Iannuzzi, M.C.; Rybicki, B.A.; Pander, J.P.; Newman, L.S.; Rose, C.; Magira, E.;Monos, D. ACCESS Group. HLA and environmental interactions in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2008,25,125-32.
- Rossman, M.D.; Thompson, B.; Frederick, M.; Maliarik, M.; Iannuzzi, M.C.; Rybicki, B.A.; Pandey, J.P.; Newman, L.S.; Magira, E.; Beznik-Cizman, B.; et al. ACCESS Group. HLA-DRB1*1101: a significant risk factor for sarcoidosis in blacks and whites. Am J Hum Genet. 2003,73,720-35. [CrossRef]
- Grunewald, J.;Eklund, A. Löfgren’s syndrome: human leukocyte antigen strongly influences the disease course. . Am J Respir Crit Care Med. 2009,179,307-12. [CrossRef]
- Garman, L.; Pezant, N.; Pastori, A.; Savoy, K.A.; Li, C.; Levin, A.M.; Iannuzzi, M.C.; Rybicki, B.A.; Adrianto, I.;Montgomery, C.G. Genome-Wide Association Study of Ocular Sarcoidosis Confirms HLA Associations and Implicates Barrier Function and Autoimmunity in African Americans. Ocul Immunol Inflamm. 2021,29,244-49. [CrossRef]
- Oswald-Richter, K.; Sato, H.; Hajizadeh, R.; Shepherd, B.E.; Sidney, J.; Sette, A.; Newman, L.S.;Drake, W.P. Mycobacterial ESAT-6 and katG are recognized by sarcoidosis CD4+ T cells when presented by the American sarcoidosis susceptibility allele, DRB1*1101. J Clin Immunol. 2010,30,157-66. [CrossRef]
- Dawkins, B.A.; Garman, L.; Cejda, N.; Pezant, N.; Rasmussen, A.; Rybicki, B.A.; Levin, A.M.; Benchek, P.; Seshadri, C.; Mayanja-Kizza, H.; et al. Novel HLA associations with outcomes of Mycobacterium tuberculosis exposure and sarcoidosis in individuals of African ancestry using nearest-neighbor feature selection. Genet Epidemiol. 2022,46,463-74. [CrossRef]
- Grosser, M.; Luther, T.; Fuessel, M.; Bickhardt, J.; Magdolen, V.;Baretton, G. Clinical course of sarcoidosis in dependence on HLA-DRB1 allele frequencies, inflammatory markers, and the presence of M. tuberculosis DNA fragments. Sarcoidosis Vasc Diffuse Lung Dis. 2005,22,66-74.
- Inohara, N.; Ogura, Y.; Fontalba, A.; Gutierrez, O.; Pons, F.; Crespo, J.; Fukase, K.; Inamura, S.; Kusumoto, S.; Hashimoto, M.; et al. Host recognition of bacterial muramyl dipeptide mediated through NOD2. Implications for Crohn’s disease. J Biol Chem. 2003,278,5509-12. [CrossRef]
- Hugot, J.P.; Chamaillard, M.; Zouali, H.; Lesage, S.; Cézard, J.P.; Belaiche, J.; Almer, S.; Tysk, C.; O’Morain, C.A.; Gassull, M.; et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. . Nature. 2001,411,599-603. [CrossRef]
- Miceli-Richard, C.; Lesage, S.; Rybojad, M.; Prieur, A.M.; Manouvrier-Hanu, S.; Häfner, R.; Chamaillard, M.; Zouali, H.; Thomas, G.;Hugot, J.P. CARD15 mutations in Blau syndrome. Nat Genet. 2001,29,19-20. [CrossRef]
- Hampe, J.; Grebe, J.; Nikolaus, S.; Solberg, C.; Croucher, P.J.; Mascheretti, S.; Jahnsen, J.; Moum, B.; Klump, B.; Krawczak, M.; et al. Association of NOD2 (CARD 15) genotype with clinical course of Crohn’s disease: a cohort study. Lancet. 2002,359,1661-65. [CrossRef]
- Wang, X.; Kuivaniemi, H.; Bonavita, G.; Mutkus, L.; Mau, U.; Blau, E.; Inohara, N.; Nunez, G.; Tromp, G.;Williams, C.J. CARD15 mutations in familial granulomatosis syndromes: a study of the original Blau syndrome kindred and other families with large-vessel arteritis and cranial neuropathy. Arthritis Rheum. 2002,46,3041-45. [CrossRef]
- Lesage, S.; Zouali, H.; Cézard, J.P.; Colombel, J.F.; Belaiche, J.; Almer, S.; Tysk, C.; O’Morain, C.; Gassull, M.; Binder, V.; et al. EPWG-IBD Group; EPIMAD Group; GETAID Group. CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002,70,845-57. [CrossRef]
- Dow, C.T.;Ellingson, J.L. Detection of Mycobacterium avium ss. Paratuberculosis in Blau Syndrome Tissues. . Autoimmune Dis. 2010,2011,127692.
- Caso, F.; Galozzi, P.; Costa, L.; Sfriso, P.; Cantarini, L.;Punzi, L. Autoinflammatory granulomatous diseases: from Blau syndrome and early-onset sarcoidosis to NOD2-mediated disease and Crohn’s disease. RMD Open. 2015,1,e000097. [CrossRef]
- Takeuchi, Y.; Shigemura, T.; Kobayashi, N.; Kaneko, N.; Iwasaki, T.; Minami, K.; Kobayashi, K.; Masumoto, J.;Agematsu, K. Early diagnosis of early-onset sarcoidosis: a case report with functional analysis and review of the literature. Clin Rheumatol. 2017,36,1189-96. [CrossRef]
- Matsui, Y.; Iwai, K.; Tachibana, T.; Fruie, T.; Shigematsu, N.; Izumi, T.; Homma, A.H.; Mikami, R.; Hongo, O.; Hiraga, Y.; et al. Clinicopathological study of fatal myocardial sarcoidosis. Ann N Y Acad Sci. 1976,278,455-69. [CrossRef]
- Roberts, W.C.; McAllister, H.A., Jr.;Ferrans, V.J. Sarcoidosis of the heart. A clinicopathologic study of 35 necropsy patients (group 1) and review of 78 previously described necropsy patients (group 11). Am J Med. 1977,63,86-108. [CrossRef]
- Silverman, K.J.; Hutchins, G.M.;Bulkley, B.H. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978,58,1204-11. [CrossRef]
- Dubrey, S.W.;Falk, R.H. Diagnosis and management of cardiac sarcoidosis. Prog Cardiovasc Dis. 2010,52,336-46. [CrossRef]
- Kandolin, R.; Lehtonen, J.; Graner, M.; Schildt, J.; Salmenkivi, K.; Kivistö, S.M.;Kupari, M. Diagnosing isolated cardiac sarcoidosis. . J Intern Med. 2011,270,461-68. [CrossRef]
- Dow, C.T.;Collins, M.T. Detection of M. paratuberculosis in Sarcoisosis Cardiac Tissue. 3rd International WASOG Conference on Diffuse Lung Diseases. Catania, ItalyJune 21, 2006.
- Celler, B.G. Case Study: Cardiac sarcoidosis resolved with Mycobacterium avium paratuberculosis antibiotics (MAP). Sarcoidosis Vasc Diffuse Lung Dis. 2018,35,171-77. [CrossRef]
- Borody, T.J.; Leis, S.; Warren, E.F.; Surace, R. Treatment of severe Crohn’s disease using antimycobacterial triple therapy--approaching a cure? Dig Liver Dis. 2002,34,29-38. [CrossRef]
- Borody, T.J.; Bilkey, S.; Wettstein, A.R.; Leis, S.; Pang, G.; Tye, S. Anti-mycobacterial therapy in Crohn’s disease heals mucosa with longitudinal scars. Dig Liver Dis. 2007,39,438-44. [CrossRef]
- Alcedo, K.P.; Thanigachalam, S.; Naser, S.A. RHB-104 triple antibiotics combination in culture is bactericidal and should be effective for treatment of Crohn’s disease associated with Mycobacterium paratuberculosis. Gut Pathog. 2016, 8, 32. [Google Scholar] [CrossRef]
- Agrawal, G.; Clancy, A.; Huynh, R.; Borody, T. Profound remission in Crohn’s disease requiring no further treatment for 3-23 years: a case series. Gut Pathog. 2020, 12, 16. [Google Scholar] [CrossRef]
- Kuenstner, J.T.; Naser, S.; Chamberlin, W.; Borody, T.; Graham, D.Y.; McNees, A.; Hermon-Taylor, J.; Hermon-Taylor, A.; Dow, C.T.; Thayer, W.; et al. The Consensus from the Mycobacterium avium ssp. paratuberculosis (MAP) Conference 2017. Front Public Health, 2017,5,208. [CrossRef]
- Johnson, S. Who Moved My Cheese? Putnam Adult; 1998.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




