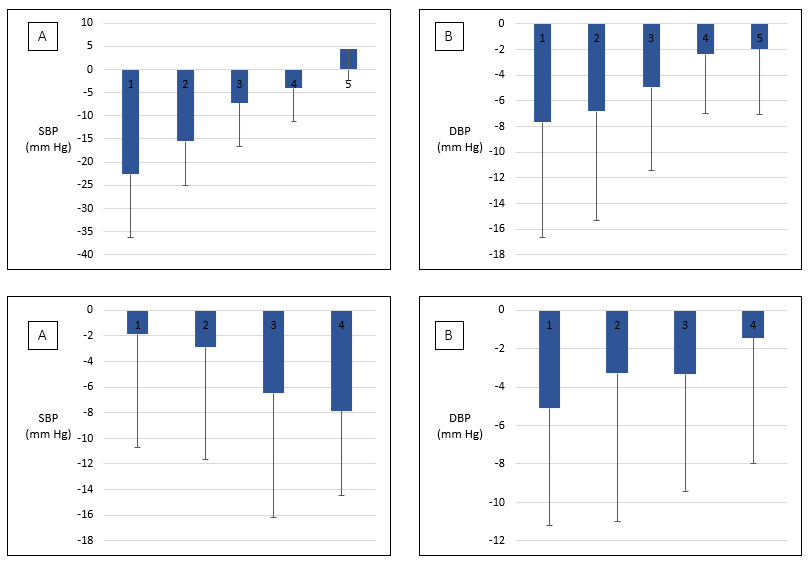
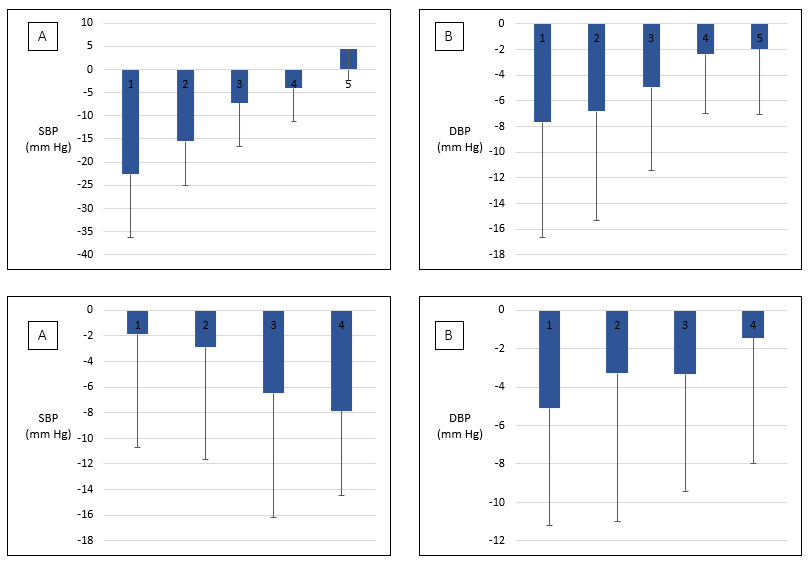
Systemic hypertension has been recognized as a modifiable traditional cardiovascular risk factor and influenced by many factors such as eating habits, physical activity, diabetes and obesity. The objective of this study was to identify cardiometabolic factors that predict changes in blood pressure induced by a one-year lifestyle intervention in primary care settings involving a collaboration between family physicians, dietitians, and exercise specialists. Patients with metabolic syndrome diagnosis were recruited by family physicians participating in primary care lifestyle intervention among several family care clinics across Canada. Participants for whom all cardiometabolic data at the beginning (T0) and the end (T12) of the intervention were available were included in the present analysis (n=101). Patients visited the dietitian and the exercise specialist weekly for the first three months and monthly for the last nine months. Diet quality, exercise capacity, anthropometric indicators, and cardiometabolic variables were evaluated at T0 and at T12. The intervention induced a significant decrease in waist circumference (WC), systolic (SBP) and diastolic (DBP) blood pressure, and plasma triglycerides and an increase in cardiorespiratory fitness (estimated VO2max). Body weight (p<0.001), body mass index (BMI) (p<0.001), and plasma glucose (p=0.006) reduction and VO2max increase (p=0.048) were all related to changes in SBP. WC was the only variable for which changes were significantly correlated with those in both SBP (p<0.0001) and DBP (p=0.0004). Variations in DBP were not associated with changes in other cardiometabolic variables to a statistically significant extent. Twelve participants were identified as adverse responders in both SBP and DBP and displayed less favorable changes in WC. The beneficial effects of a lifestyle intervention on blood pressure were significantly associated with cardiometabolic variables, especially WC. These findings suggest that a structured lifestyle intervention in primary care can help improve cardiometabolic risk factors in patients with metabolic syndrome.