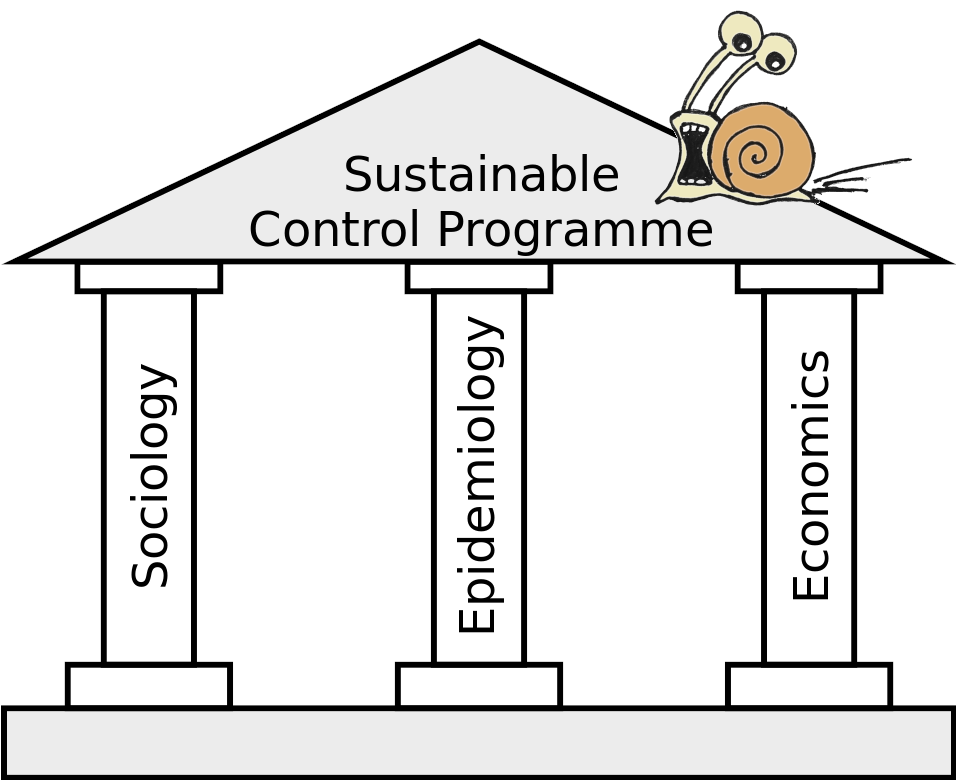
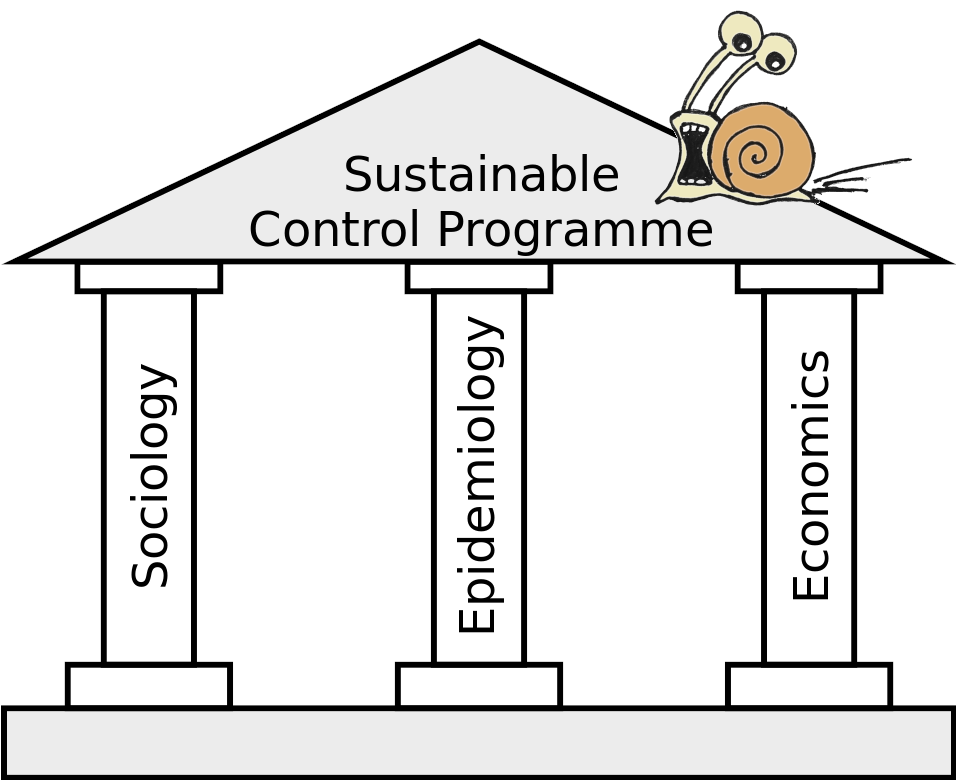
Schistosomiasis is a parasitic disease acquired through contact with contaminated freshwater. The definitive hosts are terrestrial mammals, including humans, with some Schistosoma species crossing the animal-human boundary through zoonotic transmission. An estimated 12 million people live at risk of zoonotic schistosomiasis caused by Schistosoma japonicum and Schistosoma mekongi, largely in the World Health Organization’s Western Pacific Region and in Indonesia. Mathematical models have played a vital role in our understanding of the biology, transmission, and impact of intervention strategies, however, these have mostly focused on non-zoonotic Schistosoma species. Whilst these non-zoonotic-based models capture some aspects of zoonotic schistosomiasis transmission dynamics, the commonly-used frameworks are yet to adequately capture the complex epi-ecology of multi-host zoonotic transmission. However, overcoming these knowledge gaps goes beyond transmission dynamics modelling. To improve model utility and enhance zoonotic schistosomiasis control programmes, we highlight three pillars that we believe are vital to sustainable interventions at the implementation (community) and policy-level, and discuss the pillars in the context of a One-Health approach, recognising the interconnection between humans, animals and their shared environment. These pillars are: (1) human and animal epi-ecological understanding; (2) economic considerations (such as treatment costs and animal losses); and (3) sociological understanding, including inter- and intra-human and animal interactions.