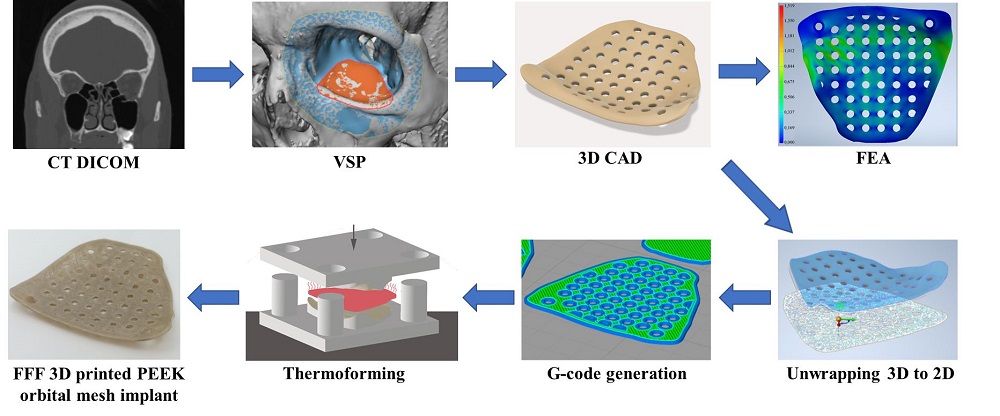
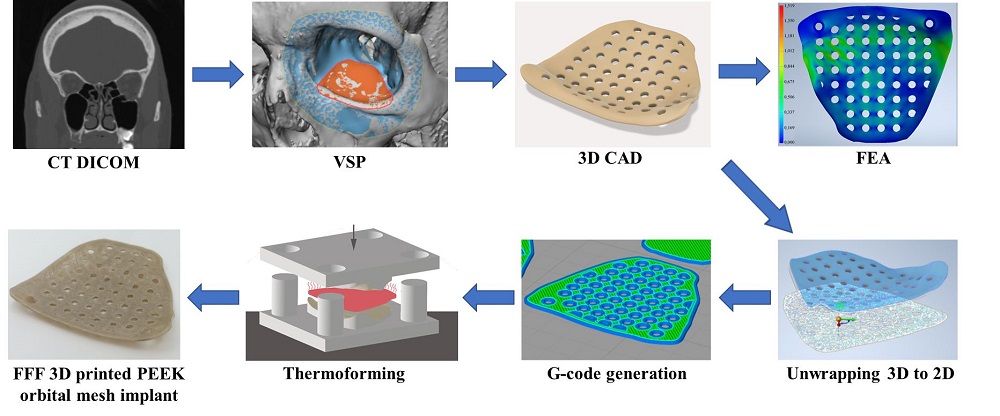
Pure orbital blowout fractures occur within the confines of the internal orbital wall. Restoration of orbital form and volume is paramount to prevent functional and esthetic impairment. The anatomical peculiarity of the orbit has encouraged surgeons to develop implants with customized features to restore its architecture. This has resulted in worldwide clinical demand for patient-specific implants (PSIs) designed to fit precisely in the patient's unique anatomy. Fused filament fabrication (FFF) three-dimensional (3D) printing technology has enabled the fabrication of implant-grade polymers such as Polyetheretherketone (PEEK), paving the way for a more sophisticated generation of biomaterials. This study evaluates the FFF 3D printed PEEK orbital mesh customized implants with a metric considering the relevant design, biomechanical, and morphological parameters. The performance of the implants is studied as a function of varying thicknesses and porous design constructs through a finite element (FE) based computational model and a decision matrix based statistical approach. The maximum stress values achieved in our results predict the high durability of the implants, and the maximum deformation values were under one-tenth of a millimeter (mm) domain in all the implant profile configurations. The circular patterned implant (0.9 mm) had the best performance score. The study demonstrates that compounding multi-design computational analysis with 3D printing can be beneficial for the optimal restoration of the orbital floor.