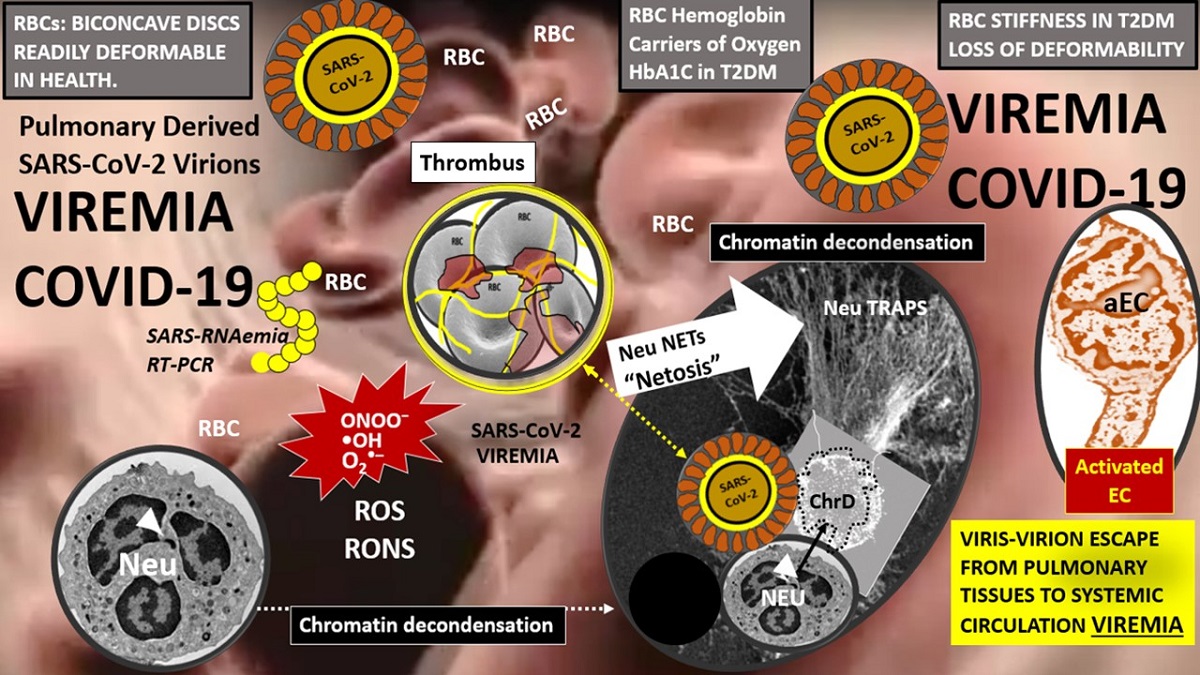
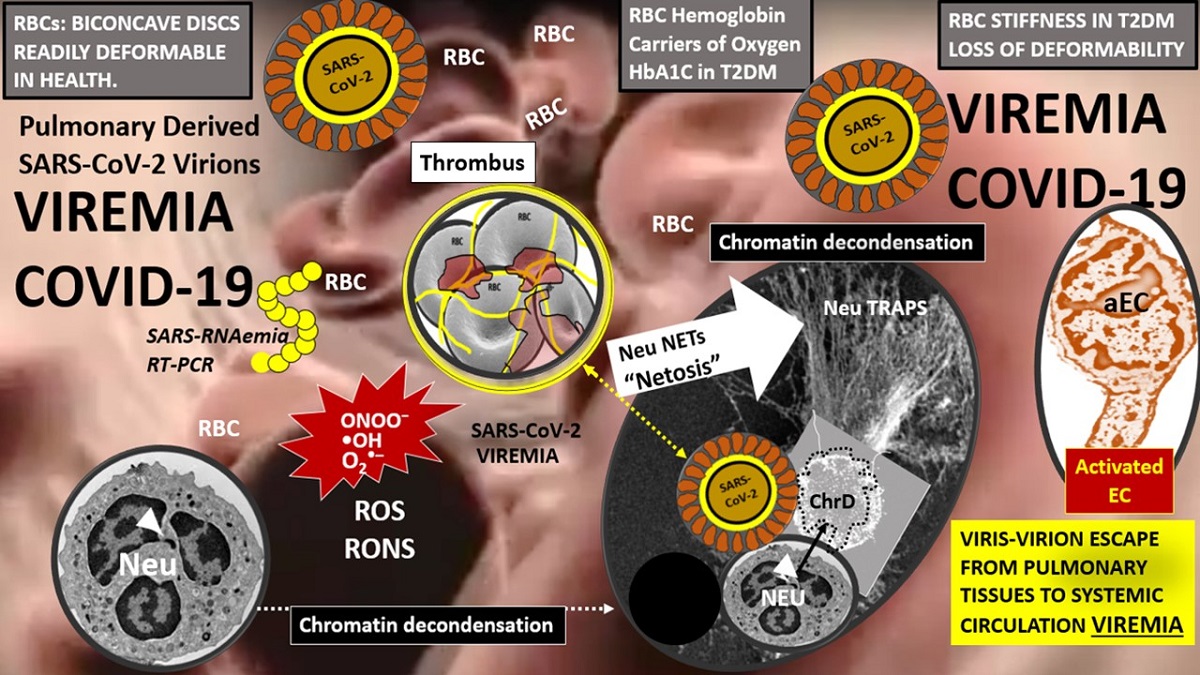
Abstract: Viremia in coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is often only discussed in passing and there are very few references detailing its structural mechanisms. In addition to viremia in the classic closed cardiovascular system, the lymphatic system is discussed in relation to a possible “lympho-viremia”. The cells that comprise each of these separate but interacting systems will be examined and include endothelial cells, erythrocytes, leukocytes (monocytes/monocyte-derived macrophages and resident tissue macrophages) (lymphocytes) (neutrophils) and thrombocytes -platelets. The SARS-CoV-2 virus has been identified in multiple extrapulmonary target organs at autopsy in those with severe COVID-19 requiring intensive care. Vulnerable COVID-19 patients may suffer from multiple storms including viral/virion storm, redox storm, cytokine storm and thrombo-embolic storm. Therefore, it is important that the possible mechanisms of viremia be explored in greater detail and how these mechanisms might affect intravascular blood components, extracellular tissue interstitium and organ structural remodeling and function. While the co-morbidity of T2DM does not increase the risk of acquiring COVID-19, it is commonly accepted that T2DM increases the risk for COVID-19 admissions to hospitals, assisted ventilation, morbidity and mortality. Importantly, the co-existence of T2DM and COVID-19 may have synergistic detrimental outcomes.