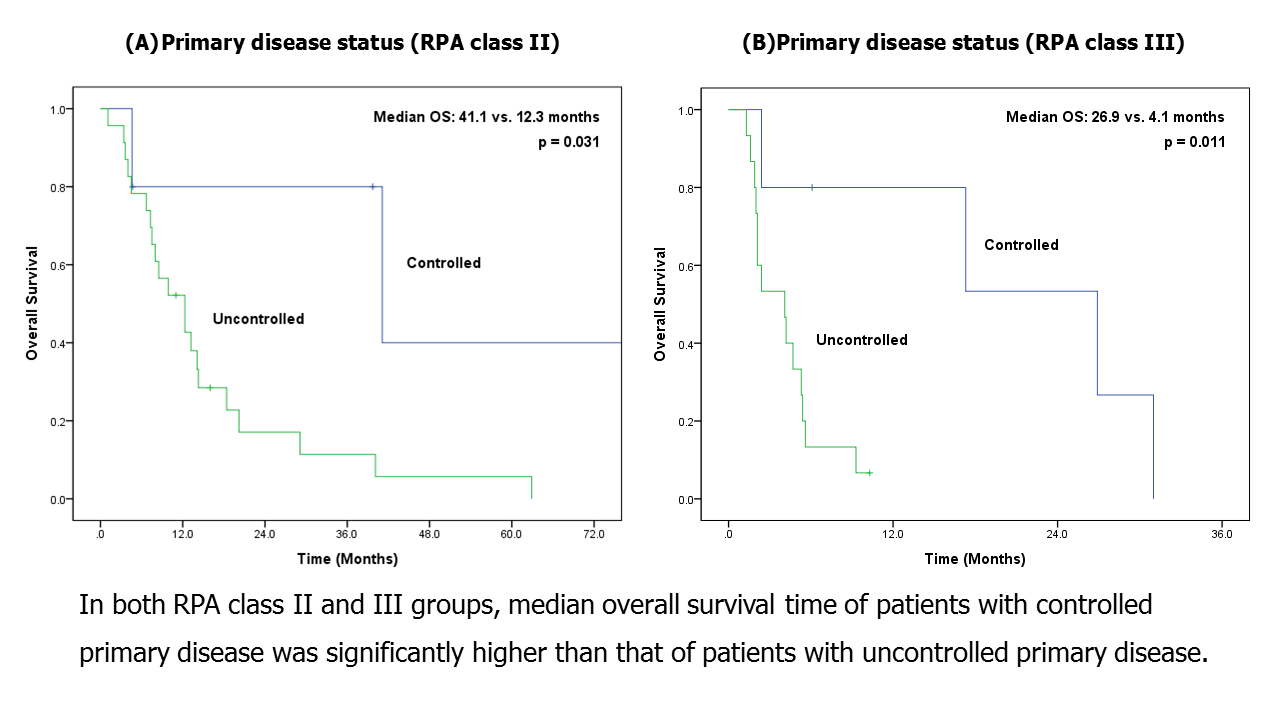
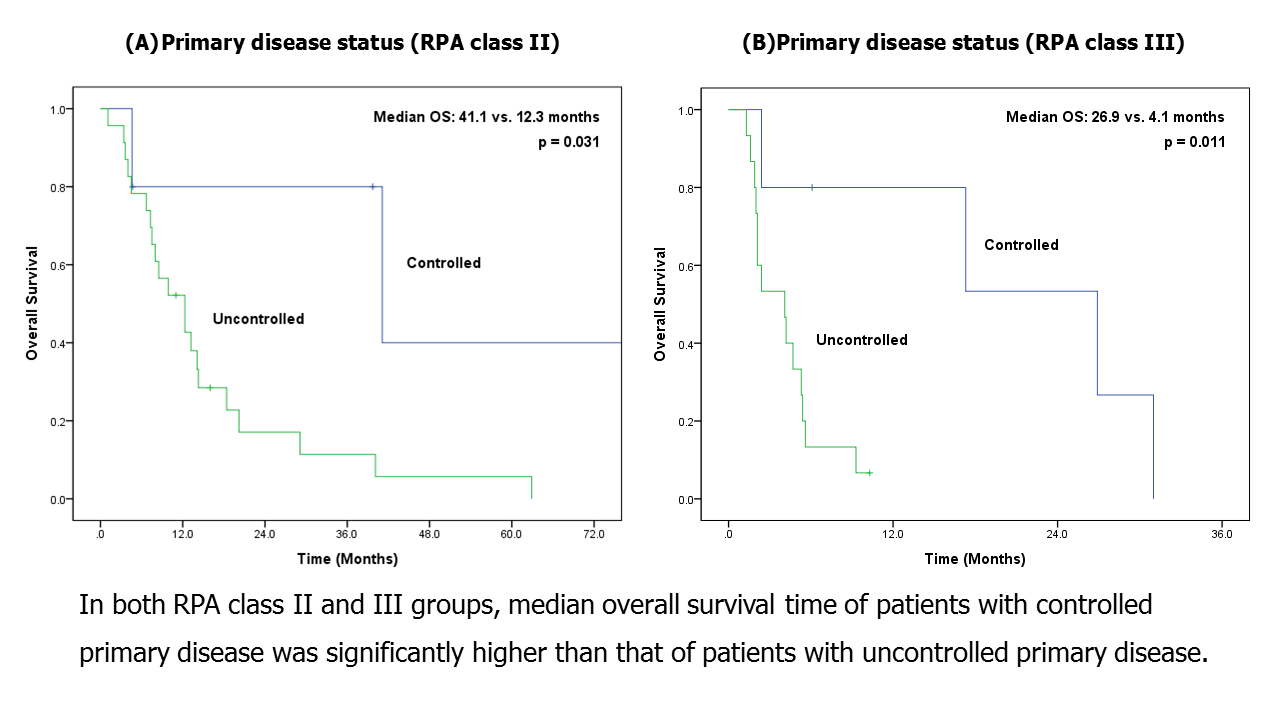
Stereotactic radiosurgery (SRS) is considered the initial treatment for lung cancer patients with small-sized and limited number of brain metastases. The objective of this study was to assess clinical outcomes of SRS treatment using CyberKnife (CK) for recursive partitioning analysis (RPA) class II/III patients with one to three brain metastases from lung cancer and identify which patients in the high RPA class could benefit from SRS. A total of 48 lung cancer patients who received CK-based SRS for their metastatic brain lesions from 2010 to 2017 were retrospectively analyzed. Radiographic response was evaluated during follow-up period. Overall survival (OS) and intracranial progression-free survival (IPFS) were calculated and prognostic variables associated with OS and IPFS were evaluated. Median follow-up time was 6.6 months. Local control rates at 6 months and 1-year following SRS were 98% and 92%, respectively. The median OS of all patients was 8 months. One-year and 2-year OS rates were 40.8% and 20.9%, respectively. In multivariate analysis, uncontrolled primary disease (p = 0.008) and ECOG performance status of 2 or 3 (p = 0.001) were independent prognostic factors for inferior OS. These two factors were also significantly associated with inferior IPFS. In subgroup analysis according to RPA class, primary disease status was the only prognostic factor, showing statistically significant OS differences in both RPA class II and III (controlled vs. uncontrolled: 41.1 vs. 12.3 months in RPA class II, p = 0.031; 26.9 vs. 4.1 months in RPA class III, p = 0.011). Our results indicated that SRS could be an effective treatment option for RPA class II/III patients with brain metastases from lung cancer in the modern treatment era. SRS might be particularly considered for patients with controlled primary disease.