Background
Multimorbidity, defined as the coexistence of two or more long-term conditions, is an increasing public health issue. More than 15 million people in England currently live with multimorbidity, and prevalence is projected to rise to 20 million by 2030 [
1,
2,
3]. Multimorbidity is linked with poorer health, reduced mobility, lower quality of life, premature mortality, and higher use of health care [
4,
5,
6,
7]. It has been identified as a priority for global health research [
1]. Primary care delivers much of the routine management for people with multimorbidity in the UK, and descriptive evidence on remission could inform how conditions are recorded, monitored, and understood. Most previous research has concentrated on the development and progression of multimorbidity, including the accumulation of conditions, inequalities in onset, and health-care use. In contrast, remission of single long-term conditions in the context of multimorbidity has received less attention.
Earlier evidence shows that remission of individual conditions is possible. For example, remission of diabetes has been reported after weight loss through lifestyle change or bariatric surgery. A scoping review of 178 studies identified 96 different definitions of remission in diabetes, illustrating both the potential for remission and variation in measurement [
8]. Other studies have described remission of hypertension, depression, chronic kidney disease, and substance use disorders [
9,
10,
11,
12,
13]. These investigations, however, have mainly focused on single-condition populations. In routine UK primary care, resolved or remission codes are also applied to several conditions. For example, “resolved asthma” is coded in some patients and is associated with subsequent variation in respiratory outcomes [
17]. NHS England has recently issued operational guidance on remission coding for severe mental illness [
18]. These coding practices indicate that remission is recognised in clinical data, although criteria and follow-up vary. Only a small number of studies have considered remission in people with multimorbidity. In one London borough, the application of remission and resolution codes in primary care records reduced estimates of multimorbidity prevalence by 2.2% [
19]. A cohort study of more than 800 000 adults in South London found that 1.9% experienced remission of at least one condition during 15 years of follow-up [
20]. Studies in other contexts, such as after bariatric surgery, have also shown remission across several conditions, but these were not designed to assess multimorbidity specifically [
10,
14]. Reviews in asthma and diabetes similarly highlight the diversity of remission definitions across conditions and settings [
21,
22]. Overall, existing evidence indicates that remission can occur, but there is limited descriptive information on its frequency and patterns among people with multimorbidity. This study aimed to describe the frequency and patterns of remission of individual long-term conditions among adults with multimorbidity in UK primary care, and to quantify remission by age, sex, ethnicity, and socioeconomic status.
Methods
Study Design, Population, and Data Sources
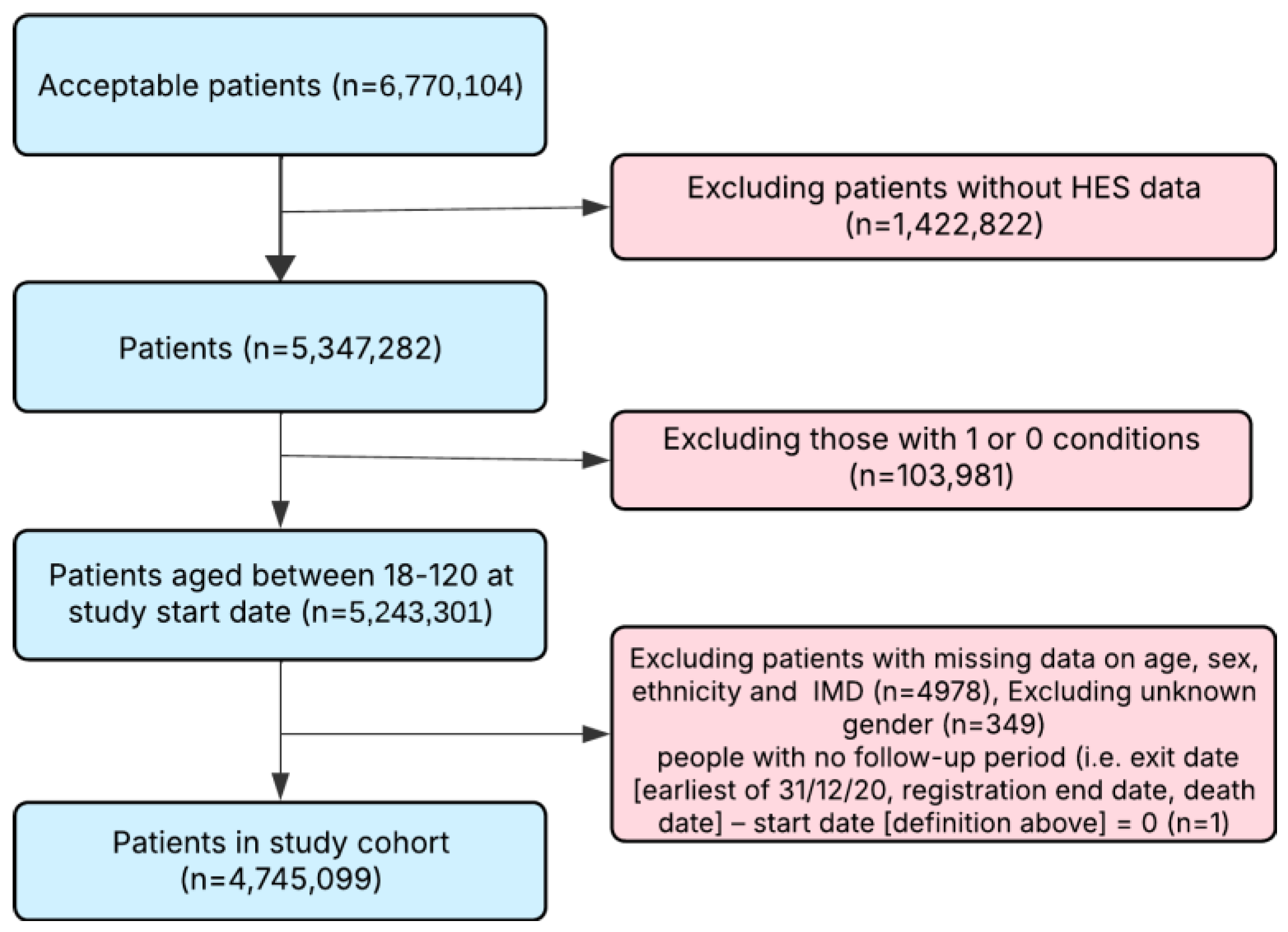
We undertook a descriptive study using data from the Clinical Practice Research Datalink (CPRD) Aurum. CPRD Aurum contains anonymised, routinely collected primary care records from general practices in England, linked to Hospital Episode Statistics (HES), the English Index of Multiple Deprivation (IMD), national disease registries, and death registrations from the Office for National Statistics (ONS) [
17]. The database includes records from about 19 million patients and is broadly representative of the English population by age, sex, and socioeconomic status [
17,
18]. The study population comprised adults (≥18 years) with multimorbidity, registered with a CPRD-contributing practice at any time between 1 January 1987 and 31 December 2020. Entry was defined as the latest of: 1 January 1987, date of practice registration, 18th birthday, or date of diagnosis of a second long-term condition. Follow-up ended at the earliest of 31 December 2020, end of registration, or death. Patients were excluded if they lacked linked HES data, follow-up data, or had missing age, sex, ethnicity, or IMD.
Definition of Multimorbidity
Multimorbidity was defined as the presence of two or more long-term conditions from a list of 59 long-term conditions out of which 56 were identified in CPRD - developed through national consensus methods [
19,
20]. Conditions were identified using diagnostic codes in primary and secondary care records, supported where relevant by biochemical results, clinical assessments, or validated rating scales. For conditions with records in both primary and secondary care, the earliest diagnosis date was used. Absence of codes or test results was considered absence of the condition.
Definition of Remission
This study focused on describing remission in conditions where operational definitions could be applied reliably within UK electronic health records. As remission could not be consistently defined for all long-term conditions, analyses were restricted to a subset of conditions with sufficient coding, test, or treatment data. We examined remission for 11 long-term conditions: anaemia, alcohol dependency, asthma, chronic kidney disease, depression, diabetes, endometriosis, epilepsy, hypertension, heart failure, and inflammatory bowel disease. These conditions were selected because remission could be operationalised using available data sources, including diagnostic and resolution codes, validated test results, clinical assessments, treatment records, and information on condition-specific events. For many other conditions in the multimorbidity list, remission could not be reliably defined due to the absence of validated codes or objective measures.
Remission was defined by evidence of any of the following: a diagnostic code for remission or resolution, test results or scores within accepted thresholds, clinical assessments consistent with remission, absence of condition-specific events (such as hospital admissions), or discontinuation of relevant treatment. Definitions were developed using a structured framework for identifying remission in UK primary care electronic health records, informed by a scoping review of previous studies, consultation with clinicians, and review of published code lists [
21]. Full operational definitions for each condition are provided in the appendix.
Follow-up time was calculated individually for each participant from the earliest date of eligibility to the end of registration, death, or study end. Because conditions varied in their typical age of onset and timing of first recorded diagnosis, available follow-up time differed across conditions.
Handling of Missing Data
Remission was operationalised as a binary outcome based on predefined condition-specific criteria derived from diagnostic codes, clinical measurements, and treatment records. Individuals were classified as having remission only when these criteria were met. Participants without sufficient evidence to meet remission criteria were classified as having no recorded remission, rather than being excluded from analyses. This reflects the nature of routinely collected electronic health records, where absence of qualifying codes or measurements indicates no documented remission rather than missing outcome data.
Missing data in sociodemographic variables (age, sex, ethnicity, and Index of Multiple Deprivation) were assessed at cohort entry; individuals with missing values were excluded prior to analysis.
Statistical Analysis
We used descriptive statistics to summarise the characteristics of the study population, overall and stratified by remission status (defined as remission of one or more long-term conditions at any point during follow-up). Frequencies and proportions were reported for categorical variables and means with standard deviations or medians for continuous variables. For each of the 11 conditions, we calculated the number and proportion of individuals with the condition who experienced remission during follow-up. The denominator was the number of individuals with the condition recorded in their health record, and the numerator was the number of those individuals with evidence of remission. Conditions were then ranked by the proportion of people in remission to identify which conditions most commonly went into remission. For baseline prevalence, we used the number of individuals with each long-term condition recorded at cohort entry, defined as the latest of the 18th birthday, practice registration, or date of diagnosis of the second condition. For remission analyses, we used to “ever-record” denominators, defined as the number of individuals who had a Read/SNOMED code for the condition at any point during follow-up. We also described patterns of remission by examining: (i) whether remission occurred in one condition only or in multiple conditions within the same individual, and (ii) variation in remission across sociodemographic groups (age, sex, ethnicity, and socioeconomic status). Age was summarised using means and standard deviations, sex and ethnicity were presented as proportions, and socioeconomic status was described using the Index of Multiple Deprivation quintiles. Remission was assigned only when diagnostic codes, clinical measures, or treatment records met predefined criteria; individuals without sufficient information were classified as having no recorded remission rather than being excluded from analyses. All analyses were conducted using Stata SE 19.5.
Results
Our study cohort included 4,745,099 adults aged 18 years or older with multimorbidity at baseline.
Figure 1 presents the flow of participants through the study. The median age was 58 years, 2,644,607 (55.73%) were female, and 4,351,881 (91.71%) identified as White ethnicity (
Table 1). The mean number of long-term conditions at baseline was 2.50 (SD 1.44). The most prevalent conditions at baseline were hypertension (1,428,522; 30.11%), depression (1,128,140; 23.77%), and inflammatory bowel disease (838,552; 17.67%). Baseline characteristics are presented in
Table 1.
During follow-up, 900 609 individuals (18.1%) had remission of at least one long-term condition, over a median follow-up of 8.0 years. Those with remission were marginally younger at baseline and more often male than those without remission and were less commonly from Asian or Black ethnic groups. The distribution of deprivation quintiles was broadly similar between groups (
Table 3).
Marked variation in remission was observed across conditions (
Table 2). The highest proportions of remission for at least 6 months were recorded for endometriosis (114 678; 90.36%), anaemia (560 445; 63.0%), and asthma (676 291; 44.71%), followed by diabetes (301 313; 15.51%). Remission was uncommon in hypertension (30 124; 1.20%) and alcohol dependency (1 328; 0.25%) and was rare in chronic kidney disease (1 460; 0.14%), heart failure (1 273; 0.11%), and inflammatory bowel disease, where remission was recorded only in isolated cases. No remission events were observed for epilepsy, consistent with clinical expectations and the limitations of available coding.
Sustained remission was infrequent across all conditions. The highest counts occurred in endometriosis (16 individuals; 0.01%), asthma (64; <0.01%), diabetes (3; <0.01%), and hypertension (12; <0.01%), although absolute numbers remained very small. Sustained remission was virtually absent in anaemia, chronic kidney disease, alcohol dependency, and heart failure. Across the cohort, remission typically occurred in a single condition, with only a minority experiencing remission in more than one condition during follow-up.
Table 2.
Remission of Multimorbidity During Follow-up in the CPRD Multimorbidity Cohort: Condition-Specific Counts of Affected Individuals, Proportions Achieving Remission for ≥6 Months, Rates of Permanent or Sustained Remission, and Median Follow-up Time Across 4,745,099 Adults Aged 18 Years and Over in the UK.
Table 2.
Remission of Multimorbidity During Follow-up in the CPRD Multimorbidity Cohort: Condition-Specific Counts of Affected Individuals, Proportions Achieving Remission for ≥6 Months, Rates of Permanent or Sustained Remission, and Median Follow-up Time Across 4,745,099 Adults Aged 18 Years and Over in the UK.
| Condition |
Number of people with condition |
Number of people achieving remission (for ≥6 months) (%) |
Number of people achieving permanent/sustained remission (%) |
Median follow-up (years) |
| Anaemia |
889562 |
560445 (63%) |
0 (0%) |
10.4 |
| Alcohol dependency |
523509 |
1328 (0.25%) |
1 (0%) |
7.97 |
| Asthma |
1512649 |
676291 (44.71%) |
64 (0%) |
9.54 |
| Chronic kidney disease |
1030034 |
1460 (0.14%) |
1 (0%) |
12.36 |
| Depression |
1878060 |
44105 (2.35%) |
18 (0%) |
8.44 |
| Diabetes |
1942207 |
301313 (15.51%) |
3 (0%) |
11.46 |
| Endometriosis |
126912 |
114678 (90.36%) |
16 (0.01%) |
8.37 |
| Epilepsy |
689874 |
0 (0%) |
0 (0%) |
10.66 |
| Hypertension |
2508411 |
30124 (1.20%) |
12 (0%) |
10.59 |
| Heart failure |
1125689 |
1273 (0.11%) |
0 (0%) |
9.35 |
| Inflammatory bowel disease |
992264 |
2 (<0.01%) |
0 |
11 |
Number of people with condition for remission analyses differed from baseline prevalence because remission was evaluated among all individuals who had ever recorded the condition in their clinical history, not solely those with the condition at cohort entry. Consequently, counts for some conditions were lower or higher than their baseline prevalence, depending on whether diagnoses occurred before or after entry into the multimorbidity cohort.
Baseline prevalence was defined using condition status at cohort entry. Remission analyses used ever-diagnosed denominators to capture conditions diagnosed both before and during follow-up.
Sociodemographic characteristics of individuals who achieved remission are presented in
Table 3. Across conditions, the age at remission varied widely: remission tended to occur earlier in conditions with onset in young or mid-adulthood, and later in conditions more closely associated with ageing. Sex distributions also differed markedly by condition. Women represented the majority of remission cases in several conditions, including anaemia, asthma, and endometriosis, the latter being almost exclusively observed in women. By contrast, remission was more common among men with alcohol dependency and heart failure.
Most remission events occurred among individuals of White ethnicity, reflecting the underlying population structure. The representation of Asian and Black ethnic groups varied by condition, with the highest proportions of remission in these groups observed for diabetes. Remission was observed across all deprivation quintiles, with broadly similar distributions for most conditions. Alcohol dependency demonstrated a strong social gradient, with remission most frequently recorded in the most deprived quintile, whereas remission in hypertension and diabetes showed relatively even distribution across levels of deprivation.
Table 3.
Sociodemographic Characteristics of Individuals Achieving Remission in the CPRD Multimorbidity Cohort among 4,745,099 Adults Aged 18 Years and Over With Recorded Remission of Long-Term Conditions During Longitudinal Follow-up From UK Primary Care Data (1987–2020).
Table 3.
Sociodemographic Characteristics of Individuals Achieving Remission in the CPRD Multimorbidity Cohort among 4,745,099 Adults Aged 18 Years and Over With Recorded Remission of Long-Term Conditions During Longitudinal Follow-up From UK Primary Care Data (1987–2020).
| Condition (n=) |
n with remission |
Age (mean, SD) |
Sex (%) |
Ethnicity (%) |
Index of Multiple Deprivation |
| |
|
|
Male |
Female |
White |
Asian |
Black |
Mixed |
Other |
1 (Least deprived |
2 |
3 |
4 |
5 (Most deprived) |
| Anaemia |
560445 |
61.89 (17.19) |
40.3 |
59.68 |
89.1 |
6.21 |
3.3 |
0.47 |
0.93 |
18.3 |
20 |
19.7 |
20.2 |
21.8 |
| Alcohol dependency |
1328 |
48.48 (12.39) |
66 |
34.03 |
95 |
2.35 |
1.59 |
0.19 |
0.89 |
8.78 |
12.9 |
18.5 |
22.5 |
37.3 |
| Asthma |
676291 |
53.68 (17.20) |
39.7 |
60.29 |
91.9 |
4.23 |
2.26 |
0.58 |
1 |
17.9 |
19.1 |
18.8 |
20.7 |
23.5 |
| Chronic kidney disease |
1460 |
62.40 (11.95) |
38.6 |
61.37 |
94.7 |
2.67 |
1.99 |
0.34 |
0.27 |
18 |
19.5 |
25.2 |
19.3 |
18 |
| Depression |
44105 |
48.70 (17.08) |
36.6 |
63.36 |
90.9 |
5.37 |
2.15 |
0.64 |
0.98 |
15.2 |
17.9 |
18.9 |
22.7 |
25.3 |
| Diabetes |
301313 |
60.05 (13.41) |
46.6 |
53.45 |
89.4 |
5.31 |
3.49 |
0.49 |
1.33 |
19.3 |
20.7 |
19.9 |
20.1 |
20.1 |
| Endometriosis |
114678 |
42.61 (13.88) |
0.11 |
99.89 |
89.5 |
5.03 |
3.18 |
0.95 |
1.36 |
19.2 |
20.3 |
19.5 |
20.4 |
20.5 |
| Epilepsy |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
| Hypertension |
30124 |
60.68 (14.93) |
40.3 |
59.66 |
92.8 |
3.53 |
2.42 |
0.37 |
0.85 |
21.4 |
20.7 |
19.5 |
19.1 |
19.3 |
| Heart failure |
1273 |
58.66 (14.53) |
51.9 |
48.14 |
92.9 |
3.26 |
2.89 |
0.15 |
0.76 |
17.8 |
21.4 |
18.1 |
17.5 |
25.2 |
| Inflammatory bowel disease |
2 |
36.77 (15.34) |
50 |
50 |
100 |
0 |
0 |
0 |
0 |
50 |
0 |
0 |
50 |
0 |
Discussion
In this large, population-based cohort of adults with multimorbidity in UK primary care, 18.1% experienced remission of at least one long-term condition during a median follow-up of 8 years. Remission was most frequently recorded for endometriosis, anaemia, asthma, and diabetes, whereas remission of chronic kidney disease, heart failure, inflammatory bowel disease, alcohol dependency, and depression was uncommon, and no remission was documented for epilepsy. Sustained remission was rare across all conditions, and remission most often occurred in a single condition rather than across multiple conditions within the same individual. Patterns of remission varied by age, sex, and ethnicity, but showed relatively little variation across deprivation quintiles.
These findings demonstrate substantial heterogeneity in remission across long-term conditions, reflecting both underlying clinical trajectories and how remission is recorded in routine care. High remission proportions in asthma and endometriosis likely reflect established coding practices, including the use of “resolved asthma” codes, which are commonly applied following symptom resolution, and remission or historical codes in endometriosis after surgery or stabilisation of symptoms. For conditions subject to sustained monitoring and performance incentives in UK primary care, such as those included in the Quality and Outcomes Framework, remission or resolution codes may be applied less frequently, contributing to lower observed remission rates despite clinical improvement. By contrast, sustained remission was exceptionally rare across all conditions, consistent with the strict operational definition applied in this study, whereby any subsequent prescribing, monitoring, or administrative activity precluded classification as sustained remission. Differences between baseline prevalence and remission denominators further reflect the use of ever-recorded diagnoses for remission analyses, capturing conditions diagnosed both before and during follow-up. Together, these findings indicate that observed remission patterns in multimorbidity are influenced not only by clinical change but also by coding behaviours within electronic health records.
Most remission events occurred in a single condition, consistent with existing literature that predominantly examines remission in single-condition cohorts, such as diabetes and asthma, where definitions and minimum durations vary widely. Evidence addressing remission in the context of multimorbidity remains limited. Population-based studies have largely focused on whether remission signals are recorded in routine data, and scoping work highlights substantial variation in operational definitions. Reports of remission across multiple conditions within the same individual are uncommon and typically confined to specific settings, such as after metabolic or bariatric surgery, and selected populations. These observations align with our findings that multi-condition remission is infrequently documented in routine primary care.
This study has several strengths. We used CPRD Aurum, a large and nationally representative primary care dataset linked to hospital records, death registrations, and area-level deprivation indices, enabling comprehensive assessment of remission in routine care. Multimorbidity was defined using a nationally agreed list of long-term conditions, and remission was operationalised using a transparent, condition-specific framework incorporating diagnostic codes, laboratory results, clinical assessments, and treatment patterns. We provide detailed, condition-level estimates and sociodemographic patterns relevant to primary care.
Several limitations should be considered. Remission ascertainment depended on clinical coding, available measurements, and treatment data, and misclassification or under-recording is possible. Remission definitions could not be applied to all long-term conditions, and differences in follow-up time may have influenced observed remission proportions. Remission events recorded exclusively in secondary care might not always be reflected in primary care records. The study was descriptive and was not designed to assess causal pathways or trajectories of remission across multiple conditions. Because remission was identified only when explicitly recorded or inferable from predefined criteria, estimates should be interpreted as documented remission in primary care records, and may underestimate true clinical remission.
Overall, remission of selected long-term conditions is recorded in UK primary care but varies substantially by condition and coding practice. More standardised remission definitions, consistent use of SNOMED codes, and clearer recording of remission onset and duration could improve data quality and support future research examining the role of remission within multimorbidity care.
Clinical and Policy Implications
Our findings indicate that remission is recorded for selected long-term conditions in UK primary care and can be incorporated into routine management. Consistent, condition-specific recording of remission would support accurate registers, recall scheduling, and safety-netting. Incorporating remission status into MLTC and medication reviews could inform treatment de-intensification or continued monitoring where sustained remission is uncommon. Practice and system templates could include remission fields and prompts, with stratified summaries by age, sex, ethnicity, and deprivation to support data quality and equity monitoring.
At commissioning and national levels, standard definitions, shared code lists, and guidance on reconciliation between primary and secondary care would facilitate comparable reporting and enable validation across settings.
Author Contributions
AJ analysed data, interpreted findings, and drafted manuscript. HDM and HH conceptualised the study. BB contributed to the analysis. All authors reviewed and edited the manuscript.
Funding
National Institute for Health and Care Research (NIHR).
Conflicts of Interest
None.
Funding Statement
HDM has received funding from the National Institute for Health and Care Research - the Artificial Intelligence for Multiple Long-Term Conditions, or "AIM". 'The development and validation of population clusters for integrating health and social care: A mixed-methods study on multiple long-term conditions' (NIHR202637); receives funding from the National Institute for Health and Care Research ‘Multiple Long-Term Conditions (MLTC) Cross NIHR Collaboration (CNC)’ (NIHR207000); and receives funding from the National Institute for Health and Care Research ‘Developing and optimising an intervention prototype for addressing health and social care need in multimorbidity’ (NIHR206431). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care. This study was funded by the National Institute for Health and Care Research (NIHR) under its Research for Patient Benefit (Grant Reference number: NIHR206873). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. .
Ethics
The study is approved by the Independent Scientific Advisory Committee (ISAC) for CPRD research (ISAC protocol number 21_001667).
Data sharing
Data may be obtained from a third party and are not publicly available. This study is based on Clinical Practice Research Datalink (CPRD) and is subject to a full license agreement that does not permit data sharing outside of the research team. However, data can be obtained by applying to CPRD (enquiries@cprd.com) for any replication of the study.
List of Abbreviations
| CPRD – Clinical Practice Research Datalink |
| EHR – Electronic Health Records |
| HES – Hospital Episode Statistics |
| IMD – Index of Multiple Deprivation |
| ISAC – Independent Scientific Advisory Committee |
| LTC – Long-Term Condition |
| MLTC – Multiple Long-Term Conditions |
| NIHR – National Institute for Health and Care Research |
| NHS – National Health Service |
| ONS – Office for National Statistics |
| QOF – Quality and Outcomes Framework |
| SD – Standard Deviation |
| SNOMED – Systematized Nomenclature of Medicine |
| UK – United Kingdom |
References
- The Academy of Medical Sciences. Multimorbidity: A priority for global health research. 2018. Available online: https://acmedsci.ac.uk/file-download/82222577 (accessed on 15 Jan 2024).
- Head, A; Fleming, K; Kypridemos, C; Schofield, P; Pearson-Stuttard, J; O’Flaherty, M. Inequalities in incident and prevalent multimorbidity in England, 2004–19: a population-based, descriptive study. Lancet Healthy Longev. 2021, 2(8), e489–e497. [Google Scholar] [CrossRef] [PubMed]
- Kingston, A; Robinson, L; Booth, H; Knapp, M; Jagger, C; MODEM project. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018, 47(3), 374–380. [Google Scholar] [CrossRef]
- Makovski, TT; Schmitz, S; Zeegers, MP; Stranges, S; van den Akker, M. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. 2019, 53, 100903. [Google Scholar] [CrossRef]
- Cassell, A; Edwards, D; Harshfield, A; Rhodes, K; Brimicombe, J; Payne, R; Griffin, S. The epidemiology of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2018, 68(669), e245–e251. [Google Scholar] [CrossRef]
- National Health Service. Breaking down barriers to better health and care. 2019 [cited 30 Aug 2023]. Available from.
- Soley-Bori, M; Ashworth, M; Bisquera, A; et al. Impact of multimorbidity on healthcare costs and utilisation: a systematic review of the UK literature. Br J Gen Pract. 2020, 71(702), e39–e46. [Google Scholar] [CrossRef]
- Riddle, MC; Cefalu, WT; Evans, PH; Gerstein, HC; Nauck, MA; Oh, WK; Rothberg, AE; le Roux, CW; Rubino, F; Schauer, P; Taylor, R; Twenefour, D. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care 2021, 44(10), 2438–44. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dambha-Miller, H; Hounkpatin, H; Stuart, B; Farmer, A. Type 2 diabetes remission trajectories and variation in risk of diabetes complications: a population-based cohort study. PLOS One. 2023, 18(8), e0290791. [Google Scholar] [CrossRef]
- Stenberg, E; Marsk, R; Sundbom, M; et al. Remission, relapse, and risk of major cardiovascular events after metabolic surgery in persons with hypertension: a Swedish nationwide registry-based cohort study. PLOS Med. 2021, 18(11), e1003817. [Google Scholar] [CrossRef]
- Dennehy, EB; Robinson, RL; Stephenson, JJ; et al. Impact of non-remission of depression on costs and resource utilisation: from the COmorbidities and symptoms of DEpression (CODE) study. Curr Med Res Opin. 2015, 31(6), 1165–1177. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, LA; Jensen, H; Virgilsen, LF; Falborg, AZ; Møller, H; Vedsted, P. Healthcare utilisation in general practice and hospitals in the year preceding a diagnosis of cancer recurrence or second primary cancer: a population-based register study. BMC Health Serv Res. 2019, 19(1), 941. [Google Scholar] [CrossRef] [PubMed]
- Shardlow, A; McIntyre, NJ; Fluck, RJ; McIntyre, CW; Taal, MW. Chronic kidney disease in primary care: outcomes after five years in a prospective cohort study. PLOS Med. 2016, 13(9), e1002128. [Google Scholar] [CrossRef]
- Cooiman, MI; Aarts, EO; Janssen, IMC; Hazebroek, EJ; Berends, FJ. Weight loss, remission of comorbidities, and quality of life after bariatric surgery in young adult patients. Obes Surg. 2019, 29(6), 1851–1857. [Google Scholar] [CrossRef]
- Ledwaba-Chapman, L; Bisquera, A; Gulliford, M; et al. Applying resolved and remission codes reduced prevalence of multimorbidity in an urban multi-ethnic population. J Clin Epidemiol. 2021, 140, 135–148. [Google Scholar] [CrossRef]
- Bisquera, A; Turner, EB; Ledwaba-Chapman, L; et al. Inequalities in developing multimorbidity over time: a population-based cohort study from an urban, multi-ethnic borough in the United Kingdom. Lancet Reg Health Eur. 2021, 12, 100247. [Google Scholar] [CrossRef]
- Hounkpatin, H; Barton, B; Ogden, M; Mathur, R; Stuart, B; Dambha-Miller, H. Understanding remission of long-term conditions through electronic health records: A scoping review JMIR Preprints. 16/07/2025, 80796. Available online: https://preprints.jmir.org/preprint/80796. [CrossRef]
- Mahadevan, P; Harley, M; Fordyce, S; Hodgson, S; Ghosh, R; Myles, P; Booth, H; Axson, E. Completeness and representativeness of small area socioeconomic data linked with the UK Clinical Practice Research Datalink (CPRD). J Epidemiol Community Health. 2022, 76(10), 880–886. [Google Scholar] [CrossRef]
- Ho, ISS; Azcoaga-Lorenzo, A; Akbari, A; Davies, J; Khunti, K; Kadam, UT; Lyons, RA; McCowan, C; Mercer, SW; Nirantharakumar, K; Staniszewska, S; Guthrie, B. Measuring multimorbidity in research: Delphi consensus study. BMJ Med. 2022, 1(1), e000247. [Google Scholar] [CrossRef] [PubMed]
- Dambha-Miller, H; Farmer, A; Nirantharakumar, K; et al. Artificial intelligence for multiple long-term conditions (AIM): a consensus statement from the NIHR AIM consortia. NIHR Open Res. 2023. [Google Scholar] [CrossRef]
- Hounkpatin, H; Barton, B; Ogden, M; et al. Understanding remission of long-term conditions through electronic health records: a scoping review. JMIR Preprints. [CrossRef]
- Le-Rademacher, JG; Therneau, TM; Ou, FS. The utility of multistate models: a flexible framework for time-to-event data. Curr Epidemiol Rep. 2022, 9(3), 183–189. [Google Scholar] [CrossRef]
- Meira-Machado, L; de Uña-Alvarez, J; Cadarso-Suárez, C; Andersen, PK. Multi-state models for the analysis of time-to-event data. Stat Methods Med Res. 2009, 18(2), 195–223. [Google Scholar] [CrossRef] [PubMed]
- Crowther, MJ. STAFT: Stata module to fit flexible parametric accelerated failure time models. Statistical Software Components S458361. Boston College Department of Economics; 2017 (revised 31 Jul 2017).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).