1. Introduction
Gastroschisis is a congenital defect of the paraumbilical abdominal wall closure, most often occurring on the right side, without a covering membrane but with an intact umbilical cord. The defect is characterized by the extrusion of the abdominal viscera from beyond the peritoneal cavity [
1].
The prevalence of congenital anomalies typically varies over time and across different regions and countries [
2]. Since the 1960s, gastroschisis has shown a significant global increase. Historically, a “gastroschisis pandemic” was noted in the literature due to increases of up to 300% over two decades [
3]. In contrast, recent data from various health systems suggest trend reversal, with the prevalence of gastroschisis declining over the past 15 years [
2,
4,
5]. These fluctuations in prevalence—both increases and decreases—are difficult to explain, as gastroschisis has a multifactorial etiology [
6].
Patients with gastroschisis experience high morbidity, often requiring multiple operations and prolonged hospital stays [
7]. The costs associated with treating affected children are substantial and represent a significant burden to healthcare systems. The substantial costs associated with the treatment of children with gastroschisis underscore the importance of studying its incidence, associated characteristics, and mortality [
8].
Over the past sixty years, gastroschisis-related mortality has declined in developed and developing countries. This reduction, however, has not been observed in low-income countries. Developed countries currently report mortality rates close to 5% [
9]. Developing nations show intermediate outcomes, while the mortality rate in low-income countries ranges from 75% to 100% [
10,
11,
12].
Despite the relevance of this topic, there is a notable gap in comprehensive longitudinal data from southern Brazil. This study is the first population-based analysis to simultaneously assess incidence, mortality, and maternal-infant factors associated with gastroschisis in the state of Paraná. Paraná is located in southern Brazil, with an estimated population of 11,890,517 in 2025, and ranks fourth in the country according to the Human Development Index (HDI) [
13].
This study aimed to analyze temporal trends in the annual incidence and case fatality rate of gastroschisis in Paraná between 2013 and 2024, and characterize the clinical-epidemiological profile of affected mothers and newborns.
2. Materials and Methods
2.1. Study Design, Setting, and Period
This is a population-based observational study with a temporal trend design, analyzing data on live births diagnosed with gastroschisis in the state of Paraná, Brazil, and its health macroregions (MRs), between 2013 and 2024.
Data on live births, hospitalizations, and mortality associated with gastroschisis were obtained from the official website of the Department of Informatics of the Brazilian Unified Health System (DATASUS) [
14]. The databases accessed were the Live Birth Information System (SINASC) and the Mortality Information System (SIM). Data collection was conducted in 2025 in the city of Maringá, Paraná [
14,
15].
2.2. Population and Inclusion/Exclusion Criteria
This study analyzed hospitalization data for newborns diagnosed with gastroschisis (ICD-10 code Q79.3), classified according to the International Classification of Diseases, 10th Revision (ICD-10).
Variables relating to maternal, pregnancy, and neonatal characteristics were analyzed. Specifically, the following variables were maternal age (10–19 years, 20–24 years, and over 25 years), maternal marital status, maternal education level, number of prenatal visits, type of pregnancy (singleton or multiple), gestational age (< 37 weeks or ≥ 37 weeks), type of delivery (cesarean or vaginal), infant race/ethnicity, Apgar score at one minute, Apgar score at five minutes, birth weight (< 2,500 g or ≥ 2,500 g), sex, annual incidence rate, and mortality rate.
2.3. Study Protocol
For the rate calculations, hospitalizations were selected based on data from the SINASC database for Paraná, in which gastroschisis was recorded as a diagnosis [
14]. Mortality was determined based on data from the SIM database, where Q79.3 (gastroschisis) was listed as the underlying cause of death [
15]. Variables were grouped into three categories:
maternal (age, marital status, and educational level),
gestational (number of prenatal visits, type of pregnancy, and mode of delivery), and
neonatal (sex, race/ethnicity, birth weight, gestational age, and Apgar scores at 1 and 5 minutes). Relative frequencies (percentages) of the variables, the annual incidence, and mortality rate were calculated. Both the annual incidence and mortality rate were calculated as the ratio between the number of events and the total number of live births among residents, multiplied by a constant of 10,000.
2.4. Data Analysis and Statistical Methods
Trends in mortality and annual incidence rates were analyzed using polynomial regression modeling, with the rates considered as dependent variables (y) and year as the independent variable (x). To avoid autocorrelation, the centered year variable (x–2018) was used. The time series were smoothed using a three-point moving average. Polynomial regression models tested included linear (y=β0+β1x1), quadratic (y=β0+β1x1+β2x2), and cubic (y=β0+β1x1+β2x2+β3x3). A trend was considered statistically significant when the estimated model had a p-value < 0.05. Model selection was further guided by the scatter plot analysis, the coefficient of determination (R2), and residual analysis. When all criteria were significant for more than one model and R2 values were similar, the simpler model was preferred. Trend and polynomial regression analyses were performed for the entire state of Paraná as well as for its health MRs. Paraná is divided into four health MRs: Northern, Northwestern, Eastern, and Western. The southern part of the state is incorporated into the eastern and western regions. To compare the proportions of categorical variables, Pearson’s chi-square test was used. The significance was set at 5%. Analyses were performed using Microsoft Excel (version 2024) and Epi Info (version 7.2.7.0).
2.5. Ethical Aspects
As this study was based on secondary data available in the public domain, it was exempt from review by the Permanent Committee for Ethics in Research Involving Human Beings, in accordance with Resolution No. 510, dated April 7, 2016, of the Brazilian National Health Council [
16].
3. Results
3.1. Annual Incidence and Mortality/Case Fatality
Between 2013 and 2024, 1,798,727 live births were recorded in Paraná. Among these, 491 were diagnosed with gastroschisis. During the same period, 179 gastroschisis-related deaths (36.5%) were reported (
Table 1).
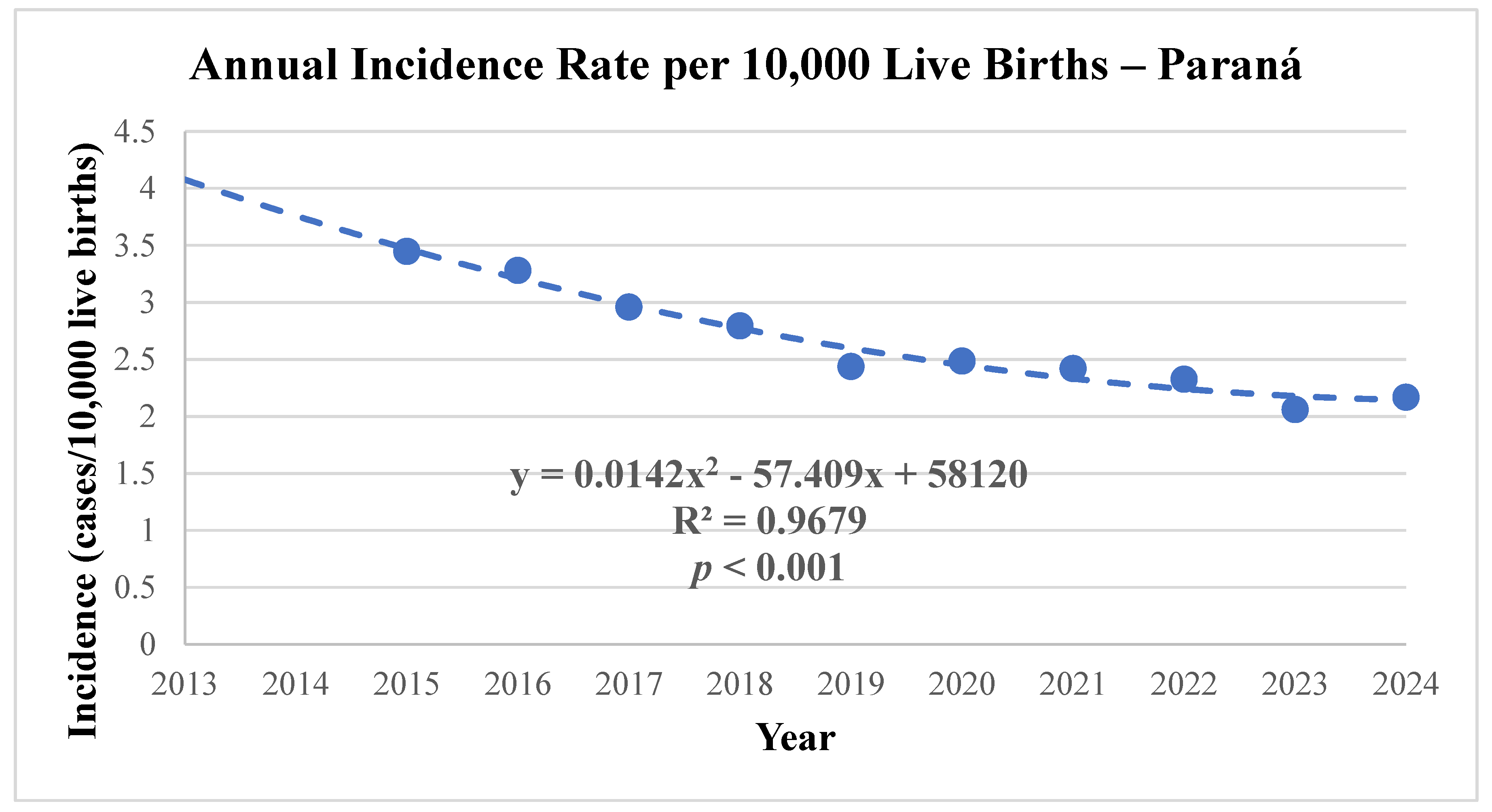
The mean annual incidence of gastroschisis in Paraná during the study period was 2.73 cases per 10,000 live births, ranging from 3.92 (in 2013) to 2.04 (in 2021) (
Table 1;
Figure 1). Polynomial regression analysis confirmed a
significant downward trend in annual incidence (p < 0.001), with a total reduction of 39.5% over the study period. A marked decline in incidence was observed between 2013 and 2021, followed by a stabilization from 2022 to 2024 (
Table 1;
Figure 1;
Table 2).
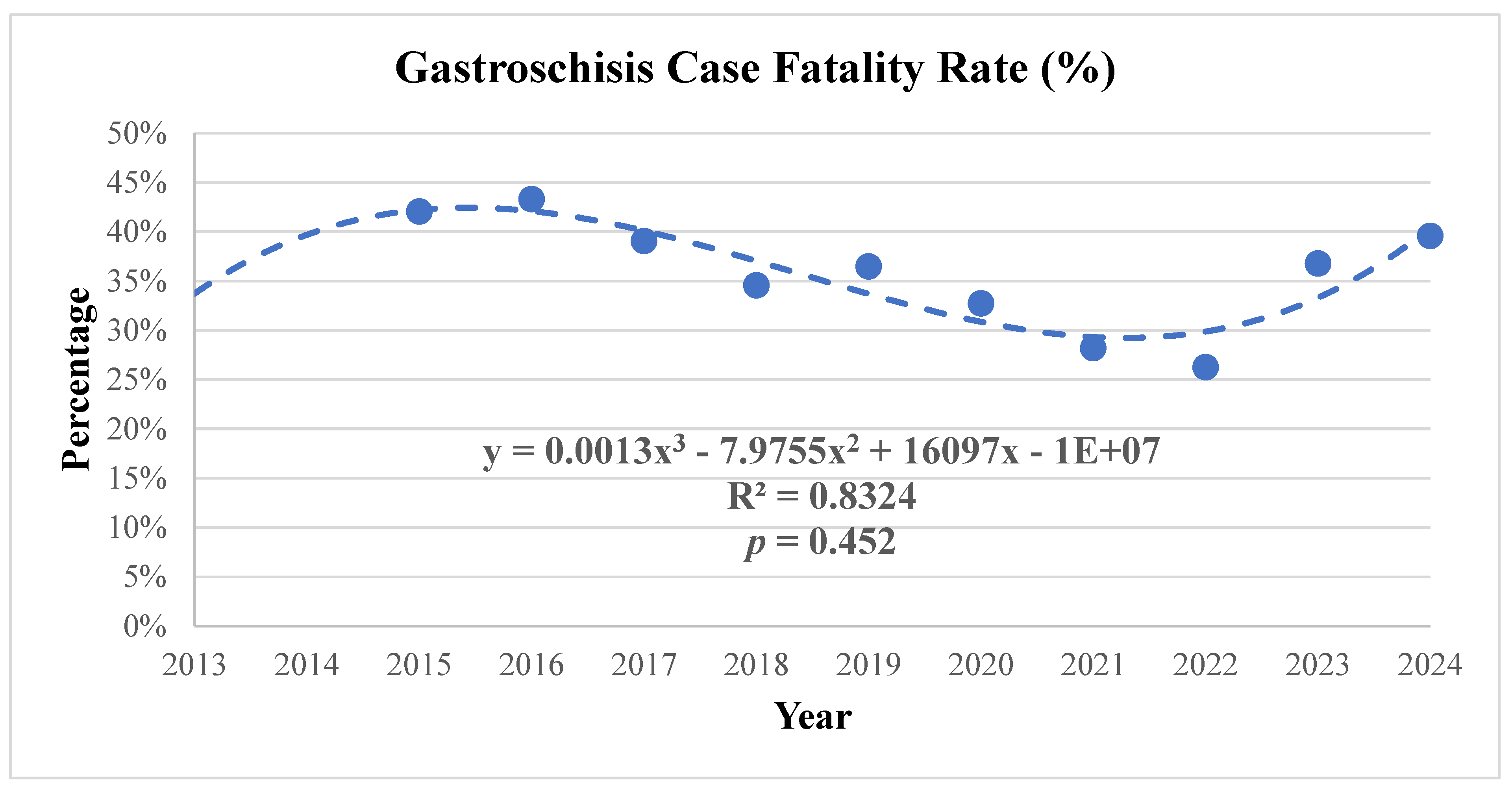
Regarding clinical outcomes, 179 deaths were recorded during the study period, resulting in a
mean case fatality rate of 36.5%. The case fatality rate exhibited a fluctuating pattern, with the lowest rate observed in 2020 (16.7%) and the highest in 2023 (48.3%). Among the deaths, 97.7% occurred within the first year of life. The age of death ranged from the one day old to four years old (
Table 1).
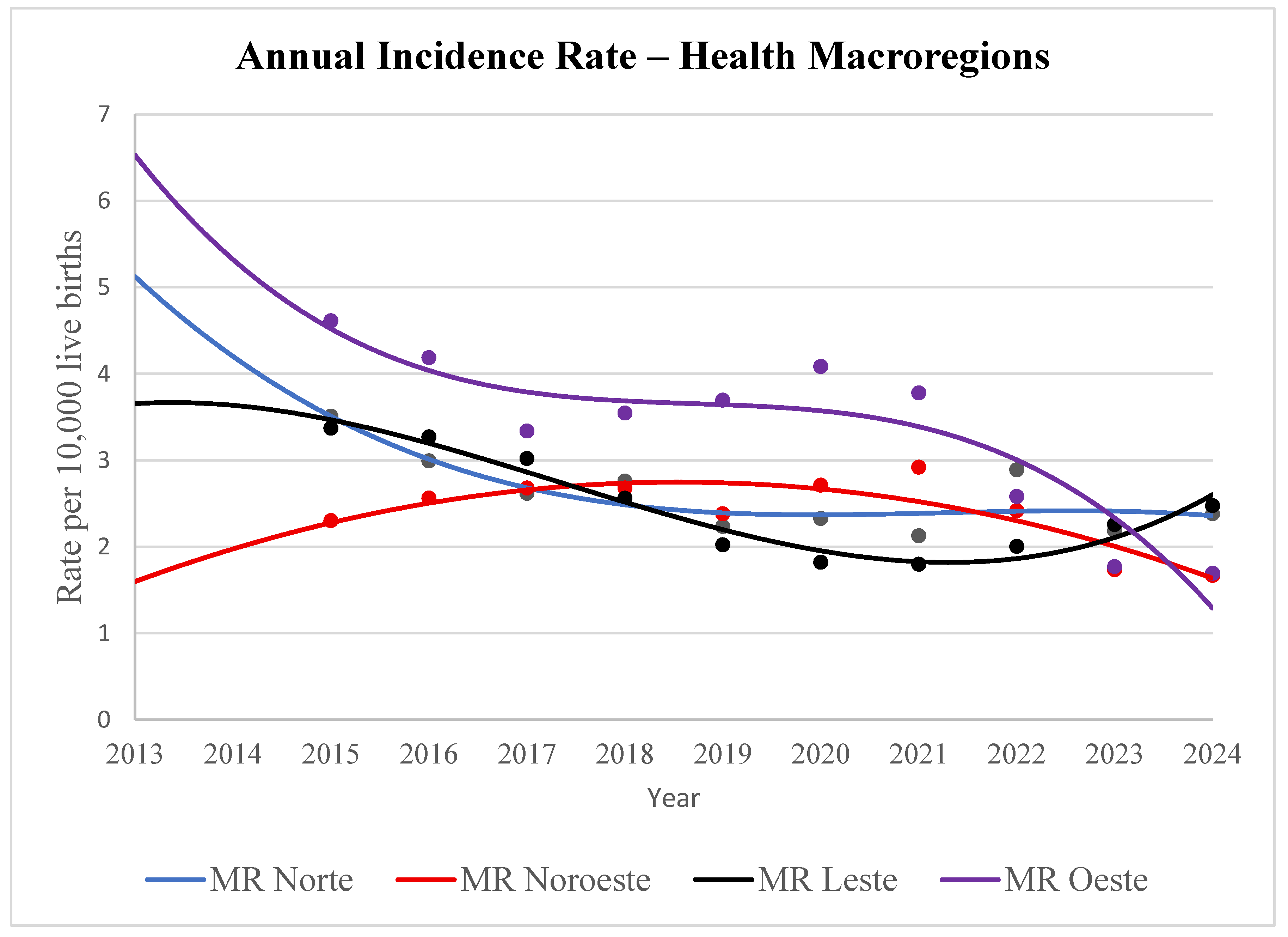
Polynomial regression analysis revealed that the health MRs of Paraná exhibited distinct patterns of annual gastroschisis incidence. Most regions (Northern, Eastern, and Western) showed statistically significant trends. Specifically, the Northern and Western MRs demonstrated a significant decline in incidence, while the Eastern MR displayed a more complex bimodal trend—initially decreasing, then increasing (
p < 0.05 for both). In contrast, the Northwestern MR showed an initial increase followed by a decrease in incidence, though this trend was not statistically significant (
Table 2;
Figure 2).
Polynomial regression analysis applied to the
case fatality rate (percentage of deaths relative to the number of cases per year) demonstrated a stable trend with fluctuations and
no statistical significance (
Table 1;
Table 2;
Figure 3).
3.2. Maternal Characteristics: Maternal Age, Marital Status, Educational Level, and Prenatal Care Visits
The annual incidence of gastroschisis increased significantly among mothers under 25 years of age (5.61 cases per 10,000 live births). The incidence was even higher among those under 20 years of age (8.09 cases per 10,000) (
Table 3). Relative risk (RR) analysis and Pearson’s chi-square test comparing mothers under 25 versus those aged 25 or older revealed a
relative risk of 2.05 (p < 0.001; 95% confidence interval [95% CI]: 1.95–2.15).
This result indicated that mothers under 25 years of age was 2.05 times more likely to have a child with gastroschisis than those 25 years and over. The
risk difference corresponded to a
105% higher likelihood (more than double the probability) (
Table 3).
A significant association was observed between maternal marital status and the occurrence of gastroschisis. Mothers without a partner had a relative risk (RR) of 1.38 (95% CI: 1.29–1.49; p < 0.001) compared to those with a partner. This indicated that women without a partner had a 38% higher risk of giving birth to a child with this malformation. Additionally, the absolute risk difference was 16.5%, highlighting greater vulnerability in this group (
Table 3).
The analysis also revealed that low educational attainment (less than 12 years of schooling) is associated with a higher risk of gastroschisis. The relative risk was 1.18 (95% CI: 1.14–1.22; p < 0.001), indicating that mothers of children with this malformation are 18% more likely to have lower education levels compared to the reference group. The absolute risk difference of 13.5% reinforced the higher likelihood of low education among mothers of infants with gastroschisis (
Table 3).
Babies of mothers who had fewer than seven prenatal care visits had a significantly greater rate of gastroschisis. The relative risk was 1.61 (95% CI: 1.38–1.87; p < 0.001), suggesting that mothers of affected children were 61% more likely to have had inadequate prenatal care compared to mothers of unaffected children. The absolute risk difference was 9.6%, confirming the greater probability of insufficient prenatal visits in the case group (
Table 3).
3.3. Pregnancy Characteristics: Type of Pregnancy, Gestational Age, and Mode of Delivery
The type of pregnancy did not reveal a significant association with the occurrence of gastroschisis. The relative risk was 0.97 (95% CI: 0.53–1.77;
p = 0.94), indicating that twin pregnancies do not carry a higher risk for the malformation compared to singleton pregnancies (
Table 4).
A strong association was observed between gastroschisis and prematurity. While only 10.7% of the general live birth population was born before 37 weeks of gestation, this percentage rose to 57.3% among gastroschisis cases. The calculated relative risk was
5.33 (95% CI: 4.93–5.76; p < 0.001), indicating that infants with gastroschisis are five times more likely to be born preterm. The absolute risk difference of 46.5% further highlighted the high probability of early delivery in these cases (
Table 4).
Regarding the mode of delivery, statistical analysis demonstrated a significant association between gastroschisis and cesarean section. The relative risk for cesarean delivery was
1.32 (95% CI: 1.27–1.38; p < 0.001), indicating that infants with gastroschisis have a 32% higher risk of being born via this surgical procedure compared to the general population. The absolute risk difference was 20.8%, reinforcing the increased likelihood of surgical intervention in such cases (
Table 4).
3.4. Neonatal Characteristics: Race/Ethnicity, 1-Minute Apgar Score, 5-Minute Apgar Score, Birth Weight, and Sex
Considering
race/ethnicity, a predominance of White newborns was observed (74.5%), a proportion similar to that of the general live birth population (73.9%). Statistical analysis confirmed that there were no significant differences among racial/ethnic categories (p > 0.05), indicating that race/ethnicity was not a risk factor for gastroschisis in this sample (
Table 5).
Neonatal vitality at the first minute of life showed severe compromise among gastroschisis cases. While only 12.1% of newborns in the general population presented an Apgar score below 8, this proportion rose to 49.8% among those with the malformation. Statistical analysis confirmed a
relative risk of 4.10 (95% CI: 3.75–4.49; p < 0.001), indicating that infants with gastroschisis are four times more likely to exhibit low vitality at one minute of life. The absolute risk difference of 37.6% underscores the need for specialized care and immediate neonatal resuscitation for these patients (
Table 5).
Evaluation at five minutes of life revealed an even stronger association with gastroschisis. The calculated relative risk was
9.28 (95% CI: 7.77 – 11.10; p < 0.001), indicating that infants with the malformation have a nine-fold increased risk of maintaining Apgar scores below 8 at the fifth minute than that of the control group. Although the absolute risk difference was 17.7%, the high relative risk highlights the persistence of immediate clinical compromise in these newborns (
Table 5).
Moreover, gastroschisis was strongly associated with low birth weight (< 2,500 g). While only 8.7% of the general live birth population presented with low birth weight, this proportion rose sharply to 63.7% among affected cases. Statistical analysis revealed a
relative risk of 7.29 (95% CI: 6.82–7.80; p < 0.001), indicating that infants with the malformation were seven times more likely to be born with insufficient weight. The absolute risk difference of 55.0% confirmed the high prevalence of low birth weight associated with this condition (
Table 5).
Furthermore, the sex distribution of gastroschisis was similar (50.7% male and 49.3% female) to that observed in the general live birth population. Statistical analysis revealed no significant association between sex and the presence of the malformation, with a
relative risk of 0.99 (95% CI: 0.90–1.08; p = 0.82) (
Table 5).
4. Discussion
This is the first population-based study in the state of Paraná, Brazil, to investigate the annual incidence and mortality of gastroschisis. Paraná is located in the southern region of Brazil, one of the most developed areas in the country. The state has a Human Development Index (HDI) of 0.769, which is classified as high human development. This study advances the field by integrating temporal trend analysis with maternal, gestational, and neonatal characteristics, in addition to examining mortality outcomes associated with the malformation [
13].
The findings revealed a statistically significant 48% reduction in the trend of annual gastroschisis incidence in Paraná from 2013 to 2024. Globally, the incidence and prevalence of this malformation have shown divergent patterns since the year 2000 [
17,
18,
19]. While the first decade of the 21st century was marked by an upward trend in several regions worldwide [
3,
12,
19,
20], more recent data have demonstrated a general decline. Among the available studies, a pioneering study conducted in Liaoning Province, China, in 2016 was the first to report this decline [
21]. This result was later corroborated by other investigations [
17,
22]. The results from this present study are consistent with these previous findings. Notably, evidence from the United States suggests that the reduction in gastroschisis prevalence may be strongly linked to a decline in pregnancy rates among women under 20 years of age [
22]. In Brazil, the Ministry of Health reported, through a technical note, a decrease in adolescent births from 18.9% to 11.9% over the past decade. This reduction in adolescent pregnancies may be positively associated with the decline in gastroschisis cases, although further scientific studies are needed to confirm this hypothesis [
23].
Stratified analysis by the four health MRs of Paraná revealed decreasing trends in gastroschisis rates (per 10,000 live births), with statistical significance in the Northern, Eastern, and Western regions. Although current scientific knowledge does not fully explain the determinants of these spatial disparities, similar regional variations have been documented in previous studies, such as those by Calderon et al., and in a prior investigation by our group in the state of Rio Grande do Sul [
12,
24].
The etiology of gastroschisis is widely recognized as multifactorial, with environmental variables playing a crucial role in the fluctuations of its incidence and prevalence. The hypothesis that external exposures and exogenous factors may influence the epidemiological behavior of this malformation has been widely discussed in specialized literature. Environmental factors, such as exposure to herbicides and electromagnetic fields have already been described. These factors, in theory, could explain the variations observed among the different health MRs analyzed in this study [
18,
25].
The mortality rate was 36%. Moreover, nearly all deaths (98%) occurred within the first year of life. These findings corroborate previous investigations conducted in other states of southern Brazil [
12]. This mortality rate reflects the typical scenario in developing countries. In Brazil, studies by authors such as Alves and Bilibio have reported variations, ranging from 14.9% to values exceeding 50% [
12,
26,
27,
28]. Globally, gastroschisis case fatality shows marked disparities. Rates as high as 98% have been recorded in Uganda [
10], while in the United States, Allman and Georgeades, the reported case fatality is below 10% [
7,
9]. In this study, mortality rates remained stable at approximately 36%, a figure expected for the region, yet significantly distant from those in developed countries, such as the United States, where mortality rates have remained below 10% since the 1990s [
9,
29].
4.1. Maternal Characteristics: Maternal Age, Marital Status, Educational Level, and Prenatal Care Visits
In this study, the annual incidence of gastroschisis was significantly higher among younger mothers (p < 0.001; 95% CI: 1.95 – 2.15). Women under 25 years of age accounted for 77% of the cases (rate of 5.61 per 10,000 live births), a proportion markedly higher than the 37% observed in the general live birth population. These findings are consistent with data reported by Calderon [
24], and a previous investigation conducted in Rio Grande do Sul [
12]. Statistically, mothers in this age group had a 40% higher probability (absolute risk difference) of having a child with the malformation compared to those 25 years old and over. Although the pathophysiological mechanisms linking young maternal age to gastroschisis have not yet been fully elucidated, this association remains an epidemiological constant across nearly all contemporary studies [
4,
22,
30].
Regarding family structure, it was observed that mothers of children with gastroschisis were 16.5% more likely to lack a stable partner, with statistical significance. Approximately 60% of these women were without a partner at the time of birth, reflecting the predominance of young mothers in the study sample. Young mothers are often associated with less stable relationships and a higher incidence of unplanned pregnancies. Notably, the literature on the specific impact of paternal absence in cases of gastroschisis remains limited. A study by Kidane, et al. [
31] in Rwanda highlighted the additional challenges in managing this condition when social support is lacking. These findings underscore the need for a multidisciplinary approach that considers not only clinical factors but also the psychosocial context of these mothers [
31].
Mothers of children with gastroschisis had significantly lower levels of education compared to the general population (p < 0.001; 95% CI: 1.14 – 1.22). A higher prevalence of women who had not completed 12 years of education was observed. In the Brazilian system, this corresponded to the completion of high school. This educational deficit is closely linked to the identified age profile, as early motherhood often disrupts the academic trajectory. Low maternal education, combined with young maternal age, constitutes a vulnerability scenario that may affect both early access to prenatal care and the understanding of the complex care required for the malformation. Low maternal education has also been reported in Brazil in a previous study by Regadas [
32]
Regarding obstetric care, it was found that mothers of children with gastroschisis attended significantly fewer prenatal consultations compared to the control group (
p < 0.001; 95% CI: 1.38 – 1.87). This finding revealed a significant gap in healthcare delivery. Given that gastroschisis is routinely diagnosed through prenatal ultrasonography, closer and more frequent follow-ups are warranted. However, the lower number of consultations observed may be largely explained by the high rate of prematurity identified in this sample, which reduces the total duration of gestational care. This deficit in prenatal care among gastroschisis cases corroborates findings reported by Regadas in other Brazilian contexts, highlighting a persistent challenge within the country’s public health system [
32].
4.2. Pregnancy Characteristics: Type of Pregnancy, Gestational Age, and Mode of Delivery
This study had a predominance of singleton pregnancies, accounting for 97.7% in both the case group and the general live birth population. Consequently, no statistically significant difference was identified for this variable. The occurrence of gastroschisis is independent of pregnancy differences (singleton or multiple births). This finding is consistent with results reported by Oliveira and other studies, reinforcing the evidence that twinning is neither a risk nor a protective factor for the development of this malformation [
32,
33].
In contrast, prematurity emerged as most strongly associated with gastroschisis. While the incidence of preterm births (< 37 weeks) in the general live birth population was 10.7%, this rate rose sharply to 57.7% among gastroschisis cases. This strong correlation corroborates findings from previous investigations [
4,
12,
32] and may be attributed both to medically indicated preterm delivery—aimed at minimizing damage to the exposed intestinal loops due to prolonged contact with amniotic fluid—and to premature rupture of membranes and fetal distress, which are frequently associated with this condition.
Analysis of the mode of delivery revealed that cesarean section was the predominant method among gastroschisis cases, occurring in 84.3% of births. This was significantly higher than in the general population (
p < 0.001; 95% CI: 2.42 – 3.93). Of note, Paraná exhibits a high baseline cesarean rate (63.4%). However, the incidence of cesarean among gastroschisis cases is even more pronounced. This trend toward highly medicalized deliveries is consistent with the broader Brazilian context, as reported by several authors [
32,
33]. In the case of gastroschisis, the preference for surgical delivery may be associated with the need to coordinate immediate postnatal surgical repair, as well as with the high prevalence of prematurity and fetal distress—factors that often prompt the early termination of pregnancy via abdominal delivery.
4.3. Neonatal Characteristics: Race/Ethnicity, 1-Minute Apgar Score, 5-Minute Apgar Score, Birth Weight, and Sex
No statistically significant disparities were identified in terms of
race/ethnicity between the groups analyzed. Similarly, the
sex of the infants with gastroschisis showed no association with the occurrence of the malformation (
p = 0.82; 95% CI: 0.90 – 1.08). These findings are consistent with previous investigations and suggest that the distribution of the condition in Paraná occurs independently of these variables, presenting a homogeneous epidemiological pattern with respect to neonatal demographic profiles [
12,
32,
33].
Newborns with gastroschisis showed a significantly higher frequency of low birth weight (< 2,500 g) compared to the control population (
p < 0.001; 95% CI: 6.82 – 7.80). This finding indicated a sevenfold increased risk of low birth weight in this group, corroborating evidence from the literature [
4,
26,
33]. This disparity may be attributed to the strong association between the malformation and preterm birth. Additionally, it may suggest the occurrence of intrauterine growth restriction (IUGR), a phenomenon frequently linked to gastroschisis due to chronic loss of proteins and nutrients from the exposed bowel loops into the amniotic fluid.
Assessment of neonatal vitality revealed significantly impaired Apgar scores at both the first and fifth minutes among newborns with gastroschisis (
p < 0.001). While the risk of low immediate vitality (1st minute) was four times higher (
RR 4.10), the probability of maintaining scores below 8 at the fifth minute was
nine times higher (
RR 9.28; 95% CI: 7.77–11.10) compared to the control group. These results are consistent with the literature and indicate not only a challenging extrauterine transition but also persistent clinical instability in the first minutes of life. This neonatal vulnerability may reflect inflammatory visceral exposure and the high prevalence of prematurity, requiring immediate interventions and advanced resuscitation support in the delivery room [
32,
33,
34].
4.4. Study Limitations
This study has some limitations. In particular, limitations inherent to the use of secondary databases, which are subject to variations in data quality and potential errors in the diagnostic coding of gastroschisis. However, these limitations were likely mitigated by the population-based nature of the sample, encompasing a substantial volume of records over a twelve-year period (2013–2024). The use of population-based data lends robustness to the findings and minimizes the impact of isolated inconsistencies, allowing for a reliable representation of the epidemiological reality of the malformation in the state of Paraná.
5. Conclusions
This study demonstrated a significant 39.5% reduction in the prevalence of gastroschisis in the state of Paraná between 2013 and 2024. In contrast, the lethality of the malformation remained stable and high, at 36.5%, with nearly all deaths occurring within the first year of life. Although fewer infants with gastroschisis are being born in Paraná, the severity of cases or the clinical management required to prevent deaths remains a challenge.
The identified epidemiological profile reveals that gastroschisis in Paraná is strongly associated with maternal vulnerability, predominantly affecting young women under 25 years of age, single mothers without a partner, and those with low educational attainment and insufficient prenatal care. From a clinical obstetric perspective, the condition occurs more frequently in singleton pregnancies, high rates of prematurity, and a remarkably high frequency of cesarean deliveries (84.3%). At the neonatal level, affected infants are at greater risk for low birth weight and compromised immediate vitality, as evidenced by low Apgar scores at both the first and fifth minutes.
These findings underscore the importance of continuous monitoring of epidemiological and mortality trends. Furthermore, public policies focused on reproductive planning, the enhancement of pediatric surgical support, and the improvement of high-complexity neonatal care are urgently needed. Further studies are essential to elucidate the specific etiologies underlying the geographic variations of this condition within the state of Paraná.
Author Contributions
Conceptualization: PAE and MDBC. Methodology: PAE, ACD and MHAB. Formal analysis: PAE, WSS, MPS, and COR. Investigation: PAE, ACD, and SMP. Writing—original draft preparation: PAE and MDBC. Writing—review and editing: PAE, MPS, and MDBC. Visualization: MPS. Supervision: MDBC. All authors have read and approved the final version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
As this study involved secondary data from public domain sources, it did not require approval from an institutional review board.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank the National Council for Scientific and Technological Development (CNPq) for their support in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Annual report ICBDSR. Available online: http://www.icbdsr.org/resources/annual-report/ (accessed on 7 Dec 2025).
- Xie, X.; Pei, J.; Zhang, L.; Wu, Y. Global birth prevalence of major congenital anomalies: A systematic review and meta-analysis. BMC Public Health 2025, 25, 449. [Google Scholar] [CrossRef]
- Nazer Herrera, J.; Karachon Essedin, L.; Cifuentes Ovalle, L.; Assar Cuevas, R. Gastrosquisis: ¿una pandemia con tasas en aumento? Experiencia del estudio colaborativo Latino americano de malformaciones congénitas (ECLAMC) en Chile. Período 1982–2014. Rev Chil Pediatr 2016, 87, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Xu, W.; Li, W.; Chen, Z.; Li, Q.; Liu, Z.; Liu, H.; Dai, L. Descriptive epidemiology of gastroschisis in China from 2007 to 2020: A nationwide surveillance-based study. BMC Pediatr 2024, 24, 584. [Google Scholar] [CrossRef]
- Castilla, E.E.; Mastroiacovo, P.; Orioli, I.M. Gastroschisis: International epidemiology and public health perspectives. Am J Med Genet C 2008, 148C, 162–179. [Google Scholar] [CrossRef]
- Marquart, J.P.; Nie, Q.; Gonzalez, T.; Jelin, A.C.; Broeckel, U.; Wagner, A.J.; Reddi, H.V. Genetics and genomics of gastroschisis, elucidating a potential genetic etiology for the most common abdominal defect: A systematic review. J Dev Biol 2024, 12, 34. [Google Scholar] [CrossRef]
- Allman, R.; Sousa, J.; Walker, M.W.; Laughon, M.M.; Spitzer, A.R.; Clark, R.H. The epidemiology, prevalence and hospital outcomes of infants with gastroschisis. J Perinatol 2016, 36, 901–905. [Google Scholar] [CrossRef]
- Gasparella, P.; Singer, G.; Kienesberger, B.; Arneitz, C.; Fülöp, G.; Castellani, C.; Till, H.; Schalamon, J. The financial burden of surgery for congenital malformations-the Austrian perspective. Int J Environ Res Public Health 2021, 18, 11166. [Google Scholar] [CrossRef]
- Georgeades, C.; Mowrer, A.; Ortega, G.; Abdullah, F.; Salazar, J.H. Improved mortality of patients with gastroschisis: A historical literature review of advances in surgery and critical care from 1960–2020. Children (Basel) 2022, 9, 1504. [Google Scholar] [CrossRef]
- Wesonga, A.; Situma, M.; Lakhoo, K. Reducing gastroschisis mortality: A quality improvement initiative at a Ugandan Pediatric Surgery Unit. World J Surg 2020, 44, 1395–1399. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Torres, V.M.; Salinas-Torres, R.A.; Cerda-Flores, R.M.; Martínez-de-Villarreal, L.E. Prevalence, mortality, and spatial distribution of gastroschisis in Mexico. J Pediatr Adolesc Gynecol 2018, 31, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Egger, P.A.; de Souza, M.P.; Riedo, C. de O.; Dutra, A. de C.; da Silva, M.T.; Pelloso, S.M.; Carvalho, M.D.B. Gastroschisis annual incidence, mortality, and trends in extreme Southern Brazil. J Pediatr (Rio J) 2022, 98, 69–75. [Google Scholar] [CrossRef]
- IBGE. Paraná | Cities and states. Available online: https://www.ibge.gov.br/cidades-e-estados/pr.html (accessed on 10 Dec 2025).
- TabNet, W. 3.3. Congenital anomaly or defect in live births—SINASC. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sinasc/Anomalias/anomabr.def (accessed on 23 Nov 2025).
- TabNet, W. 3.3: Fetal Deaths – Paraná. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/fet10pr.def (accessed on 30 Nov 2025).
- Resolution No. 510; Brazilian National Health Council, 2016. Available online: https://www.gov.br/conselho-nacional-de-saude/pt-br/atos-normativos/resolucoes/2016/resolucao-no-510.pdf/view (accessed on 23 Nov 2025).
- Schuh, J.M.; Cabacungan, E.; Wagner, A.J. Birth prevalence of gastroschisis in the United States: 2016-2022. Pediatrics 2025, 155, e2024068696. [Google Scholar] [CrossRef]
- de Souza, S.; Nihei, O.K.; Pestana, C.R. High prevalence of gastroschisis in Brazilian triple side border: A socioenvironmental spatial analysis. PLOS One 2021, 16, e0247863. [Google Scholar] [CrossRef] [PubMed]
- Togneri, R.M.; Wanderley, H.Y.C.; Rodrigues, M. do C. de S.; Barreto, I.H.A.; Queiroz, R.C.M.; Pagotti, M.D.; Fragoso, A.X.; Rebouças, R.G.O.; Pereira, A.L.A. de S.T.; Bortolini, E.R.; et al. Gastroschisis: Incidence and associated factors. Child and Adolescent Development: Scientific Evidence and Theoretical-Practical Considerations 2020, 1, 603–618. [Google Scholar] [CrossRef]
- Jones, A.M.; Isenburg, J.; Salemi, J.L.; Arnold, K.E.; Mai, C.T.; Aggarwal, D.; Arias, W.; Carrino, G.E.; Ferrell, E.; Folorunso, O.; et al. Increasing prevalence of gastroschisis--14 States, 1995-2012. MMWR Morb Mortal Wkly Rep 2016, 65, 23–26. [Google Scholar] [CrossRef]
- Li, N.; Chen, Y.L.; Li, J.; Li, L.L.; Jiang, C.Z.; Zhou, C.; Liu, C.X.; Li, D.; Gong, T.T.; Wu, Q.J.; et al. Decreasing prevalence and time trend of gastroschisis in 14 cities of Liaoning Province: 2006–2015. Sci Rep 2016, 6, 33333. [Google Scholar] [CrossRef]
- Mustafa, H.J.; Zargarzadeh, N.; Moss, K.L.; Abiad, M.; Gray, B.; Aagaard, K.M.; Buchmiller, T.L.; Perrone, E.E.; Shamshirsaz, A.A. Decreasing trend of gastroschisis prevalence in the United States from 2014 through 2022: Is attributed to declining birth rates in young, high-risk gravidae. Eur J Obstet Gynecol Reprod Biol X 2025, 25, 100374. [Google Scholar] [CrossRef] [PubMed]
- Brazilian Ministry of Health recommends best practices for preventing adolescent pregnancy; Ministry of Health. Available online: https://www.gov.br/saude/pt-br/assuntos/noticias/2025/fevereiro/ministerio-da-saude-orienta-boas-praticas-para-prevencao-da-gravidez-na-adolescencia (accessed on 16 Dec 2025).
- Calderon, M.G.; Santos, E.F.S.; de Abreu, L.C.; Raimundo, R.D. Increasing prevalence, time trend and seasonality of gastroschisis in São Paulo state, Brazil, 2005-2016. Sci Rep 2019, 9, 14491. [Google Scholar] [CrossRef]
- Krishnapura, S.R.; McNeer, E.; Dupont, W.D.; Patrick, S.W. County-level atrazine use and gastroschisis. JAMA Netw Open 2024, 7, e2410056. [Google Scholar] [CrossRef] [PubMed]
- Bilibio, J.P.; Beltrão, A.M.; Vargens, A.C.; Gama, T.B.; Lorenzzoni, P.L. Gastroschisis during gestation: Prognostic factors of neonatal mortality from prenatal care to postsurgery. Eur J Obstet Gynecol Reprod Biol 2019, 237, 79–84. [Google Scholar] [CrossRef]
- Miranda da Silva Alves, F.; Miranda, M.E.; de Aguiar, M.J.B.; Bouzada Viana, M.C.F. Nutritional management and postoperative prognosis of newborns submitted to primary surgical repair of gastroschisis. J Pediatr (Rio J) 2016, 92, 268–275. [Google Scholar] [CrossRef]
- Esteche, C.M.G.D.C.E.; Araujo Júnior, E.; Esteche, B.D.C.E.; Rodrigues, L.O.B.; Carvalho, F.H.C.; Rolo, L.C. Factors associated with death in newborns with gastroschisis: a retrospective cohort study from a single reference center. Rev Assoc Med Bras 2025, 71, e20241999. [Google Scholar] [CrossRef]
- Global PaedSurg Research Collaboration. Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: A multicentre, international, prospective cohort study. Lancet 2021, 398, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Lausten-Thomsen, U.; Hedley, P.L.; Conway, K.M.; Løfberg, K.M.; Johansen, L.S.; Romitti, P.A.; Christiansen, M. Gastroschisis prevalence and co-occurring malformations among Danish live births during 1994–2021: A nationwide register-based study. J Pediatr Surg 2024, 59, 161931. [Google Scholar] [CrossRef]
- Kidane, S.; Shamebo, S.D.; Ntaganda, E.; Petroze, R.T.; McNatt, Z.; Wong, R.; Rabideau, M. Exploring the lived experiences of parents caring for infants with gastroschisis in Rwanda: The untold story. PLOS Glob Public Health 2022, 2, e0000439. [Google Scholar] [CrossRef] [PubMed]
- Regadas, C.T.; Escosteguy, C.C.; Fonseca, S.C.; Pinheiro, R.S.; Coeli, C.M. Trends in prevalence of gastroschisis in Brazil from 2007 to 2020: A national population-based cross-sectional study. Birth Defects Res 2023, 115, 633–646. [Google Scholar] [CrossRef]
- Oliveira, J.B.; Russi, K.; Kosinski, S.; Shiguihara, G.F.; Poliseli, L.; Seba, G.; da costa, K.M. Epidemiology of congenital diaphragmatic hernia, esophageal atresia, and gastroschisis in South Brazil. J Neonatal Surg 2023, 12, 13. [Google Scholar] [CrossRef]
- Maria Muniz, V.; Lima Netto, A.; Bresciani Salaroli, L.; Zandonade, E. Gastroschisis in Brazil within a global context. J Hum Growth Dev 2022, 32, 83–91. [Google Scholar] [CrossRef]
Figure 1.
Annual Incidence of Gastroschisis in Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Figure 1.
Annual Incidence of Gastroschisis in Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Figure 2.
Annual Incidence of Gastroschisis in the Health Macroregions of Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Figure 2.
Annual Incidence of Gastroschisis in the Health Macroregions of Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Figure 3.
Trend in Gastroschisis Case Fatality Rate in Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Figure 3.
Trend in Gastroschisis Case Fatality Rate in Paraná, Brazil, 2013–2024. Source: SINASC/SUS, 2013–2024.
Table 1.
Annual Incidence and Mortality Rates of Gastroschisis in Paraná, Brazil (2013–2024).
Table 1.
Annual Incidence and Mortality Rates of Gastroschisis in Paraná, Brazil (2013–2024).
| Annual Incidence in Paraná |
Mortality in Paraná |
| Year |
Cases |
Live Births |
Rate x |
Deaths |
Rate x |
Months |
Months |
| |
10,000 |
10,000 |
0 - 12 |
> 12 |
| 2013 |
61 |
155,758 |
3.92 |
23 |
37.70% |
1.48 |
23 |
0 |
| 2014 |
59 |
159,915 |
3.69 |
24 |
40.70% |
1.5 |
23 |
1 |
| 2015 |
44 |
160,947 |
2.73 |
21 |
47.70% |
1.3 |
20 |
1 |
| 2016 |
53 |
155,066 |
3.42 |
22 |
41.50% |
1.42 |
22 |
0 |
| 2017 |
43 |
157,701 |
2.73 |
12 |
27.90% |
0.76 |
12 |
0 |
| 2018 |
35 |
156,201 |
2.24 |
12 |
34.30% |
0.77 |
12 |
0 |
| 2019 |
36 |
153,469 |
2.35 |
17 |
47.20% |
1.11 |
15 |
2 |
| 2020 |
42 |
146,291 |
2.87 |
7 |
16.70% |
0.48 |
7 |
0 |
| 2021 |
29 |
141,976 |
2.04 |
6 |
20.70% |
0.42 |
6 |
0 |
| 2022 |
29 |
140,637 |
2.06 |
12 |
41.40% |
0.85 |
12 |
0 |
| 2023 |
29 |
139,836 |
2.07 |
14 |
48.30% |
1 |
14 |
0 |
| 2024 |
31 |
130,930 |
2.37 |
9 |
29.00% |
0.69 |
9 |
0 |
| 2013-2024 |
491 |
1,798,727 |
2.73 |
179 |
36.50% |
1 |
175 (97.7%) |
4 (2.2%) |
Table 2.
Annual Incidence and Mortality Rates and Trends of Gastroschisis in Paraná and Its Health Macroregions (MRs), 2013–2024.
Table 2.
Annual Incidence and Mortality Rates and Trends of Gastroschisis in Paraná and Its Health Macroregions (MRs), 2013–2024.
| Trends in Annual Incidence of Gastroschisis by Health Macroregion (MR) of Paraná |
|---|
| Location |
Regression Model |
R² |
p-value |
Trend |
| Paraná |
y = 0.0142x2 - 57.409x + 58120 |
0.97 |
< 0.001 |
↓ |
| Northern MR |
y = -0.0053x3 + 31.859x2 - 64395x + 4E+07 |
0.74 |
0.029 |
↓ |
| Northwestern MR |
y = -0.0373x2 + 150.78x - 152178 |
0.75 |
0.116 |
↑↓ |
| Eastern MR |
y = 0.0074x3 - 44.869x2 + 90516x - 6E+07 |
0.95 |
0.020 |
↓↑ |
| Western MR |
y = -0.0144x3 + 87.34x2 - 176313x + 1E+08 |
0.85 |
0.002 |
↓ |
| Case fatality |
| Paraná |
y = 0.0013x3 - 7.9755x2 + 16097x - 1E+07 |
0.83 |
0.452 |
↑↓↑ |
Table 3.
Maternal Characteristics: Maternal Age, Marital Status, Years of Education, and Prenatal Care Visits in Paraná, Brazil, 2013–2024.
Table 3.
Maternal Characteristics: Maternal Age, Marital Status, Years of Education, and Prenatal Care Visits in Paraná, Brazil, 2013–2024.
| Characteristic |
Cases |
Live births |
Rate per 10,000 live births |
p-value |
| 95% CI |
|---|
| Maternal Age |
| 10 to 19 years |
196 |
39.9% |
242,160 |
13.5% |
8.09 |
5.61 |
|
< 0.001 |
| 20 to 24 years |
182 |
37.1% |
431,038 |
24.0% |
4.22 |
2.73 |
(1.95 - 2.15) |
| > 25 years old |
113 |
23.0% |
1,125,514 |
62.6% |
1.00 |
|
|
|
| Ignored |
0 |
|
15 |
|
|
|
|
|
| Maternal Marital Status |
| Without a partner |
289 |
59.1% |
760,583 |
42.5% |
3.80 |
< 0.001 |
| With a partner |
200 |
40.9% |
1,027,672 |
57.5% |
1.95 |
(1.29 - 1.49) |
| Ignored |
2 |
|
9981 |
|
|
|
|
|
| Maternal Education |
| < 12 years of education |
428 |
87.7% |
1,327,122 |
74.1% |
3.23 |
< 0.001 |
| > 12 years of education |
60 |
12.3% |
463,535 |
25.9% |
1.29 |
(1.14 – 1.22) |
| Ignored |
3 |
|
7,579 |
|
|
|
|
|
| Prenatal Visits |
| < 7 visits |
124 |
25.3% |
281,751 |
15.7% |
4.40 |
< 0.001 |
| > 7 visits |
366 |
74.7% |
1,513,253 |
84.3% |
2.42 |
(1.38 – 1.87) |
| Ignored |
1 |
|
3,232 |
|
|
|
|
|
| Total |
491 |
1,798,727 |
|
|
|
|
Table 4.
Pregnancy Characteristics: Type of Pregnancy, Gestational Age, and Mode of Delivery in Paraná, Brazil, 2013–2024.
Table 4.
Pregnancy Characteristics: Type of Pregnancy, Gestational Age, and Mode of Delivery in Paraná, Brazil, 2013–2024.
| |
Cases |
Live births |
Rate per 10,000 live births |
p-value |
| |
95% CI |
| Type of Pregnancy |
|
|
|
|
|
|
|
|
| Singleton |
476 |
97.7% |
1,755,235 |
97.7% |
|
2.71 |
|
0.94 |
| Twin |
11 |
2.3% |
41,467 |
2.3% |
|
2.65 |
|
0.53 – 1.77 |
| Ignored |
4 |
|
1,534 |
|
|
|
|
|
| Gestational Age |
|
|
|
|
|
|
| < 37 weeks |
275 |
57.3% |
191,329 |
10.7% |
14.37 |
< 0.001 |
| > 37 weeks |
205 |
42.7% |
1,591,637 |
89.3% |
1.29 |
4.93 – 5.76 |
| Ignored |
11 |
|
15270 |
|
|
|
|
|
| Mode of Delivery |
|
|
|
|
|
|
|
|
| Cesarean |
412 |
84.3% |
1,139,411 |
63.4% |
3.62 |
< 0.001 |
| Vaginal |
77 |
15.7% |
657,799 |
36.6% |
1.17 |
1.27 - 1.38 |
| Ignored |
2 |
|
1,028 |
|
|
|
|
|
| Total |
491 |
|
1,798,727 |
|
|
|
|
|
Table 5.
Neonatal Characteristics: Race/Ethnicity, 1-Minute Apgar Score, 5-Minute Apgar Score, Birth Weight, and Sex in Paraná, Brazil, 2013–2024.
Table 5.
Neonatal Characteristics: Race/Ethnicity, 1-Minute Apgar Score, 5-Minute Apgar Score, Birth Weight, and Sex in Paraná, Brazil, 2013–2024.
| |
Cases |
Live births |
Rate per 10,000 live births |
p-value |
| |
95% CI |
| Race/ethnicity |
|
|
|
|
|
|
| White |
363 |
74.5% |
1,315,351 |
73.9% |
2.76 |
0.78 |
| |
|
|
|
|
|
|
|
| Black |
10 |
2.1% |
48,074 |
2.7% |
2.08 |
0.70 - 2.48 |
| |
|
|
|
|
|
|
|
| Yellow |
2 |
0.4% |
6,535 |
0.4% |
3.06 |
0.88 |
| |
|
|
|
|
|
|
|
0.22 - 3.62 |
| Brown |
112 |
23.0% |
405,317 |
22.8% |
2.76 |
0.99 |
| |
|
|
|
|
|
|
|
0.80 - 1.23 |
| Indigenous |
0 |
0.0% |
5,793 |
0.3% |
0.00 |
0.21 |
| |
|
|
|
|
|
|
|
undefined |
| Ignored |
4 |
|
17,166 |
|
|
|
|
|
| Apgar Score (1 min) |
|
|
|
|
|
|
| 0 to 7 |
244 |
49.8% |
217,341 |
12.1% |
11.23 |
< 0.001 |
| 8 to 10 |
246 |
50.2% |
1,576,090 |
87.9% |
1.56 |
3.75 – 4.49 |
| Ignored |
1 |
|
4,805 |
|
|
|
|
|
| Apgar Score (5 min) |
|
|
|
|
|
|
| 0 to 7 |
97 |
19.8% |
38308 |
2.1% |
25.32 |
< 0.001 |
| 8 to 10 |
392 |
80.2% |
1755435 |
97.9% |
2.23 |
7.77 – 11.10 |
| Ignored |
2 |
|
4493 |
|
|
|
|
|
| Weight |
|
|
|
|
|
|
| < 2,500 g |
313 |
63.7% |
157,052 |
8.7% |
19.93 |
< 0.001 |
| > 2,500 g |
178 |
36.3% |
1,641,093 |
91.3% |
1.08 |
6.82 – 7.80 |
| Ignored |
0 |
|
91 |
|
|
|
|
|
| Sex |
|
|
|
|
|
|
|
|
| Male |
247 |
50.7% |
921,144 |
51.2% |
2.68 |
0.82 |
| Female |
240 |
49.3% |
876,922 |
48.8% |
2.74 |
0.90 - 1.08 |
| Ignored |
4 |
|
170 |
|
|
|
|
|
| Total |
491 |
|
1,798,727 |
|
|
|
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).