1. Introduction
The exposure to freeze-thaw cycles is known to induce significant morphological and structural modifications in human remains, impacting both gross and histological appearance. The physical process of freezing and thawing inherently disrupts tissue architecture, leading to severe structural damage at the cellular level, often manifesting as muscle fiber contraction and myelin sheath disruption in nervous tissues.[
1,
2] The precise biophysical mechanism underlying these alterations is complex, tough common artifacts have been identified, including ice crystal formation, extracellular fluid accumulation, cellular volume changes, known as shrinkage, and tissue splitting. [
3] It is hypothesized that freezing induces micromorphological changes primarily through osmotic stress. The rate of freezing and membrane permeability dictates the primary mode of damage: rapid freezing and low membrane permeability often cause the entire tissue system to freeze rapidly, whereas slow freezing and high membrane permeability typically lead to significant cellular shrinkage as water is drawn out into the extracellular space. In the latter scenario, hard ice crystals form predominantly in the extracellular matrix. Although the overall volume of tissue cells is reduced due to shrinkage, the formation of these solid ice crystals in the extracellular compartments concurrently increases the total volume of the tissue. [
4] This resultant mechanical stress can critically disrupt cell-to-cell connections.
Subsequent thawing reverse some of these effects. As ice crystals melt, the extracellular solution becomes diluted and highly hypotonic. If cells had previously shrunk, the osmotic gradient drives an influx of water, causing them to swell back toward their original size. Nonetheless, the cell-to-cell connections that were permanently disrupted during the freezing phase do not redevelop. Histologically, this process of cellular shrinkage is commonly described as “karyopyknosis”, this the resultant expanded extracellular areas may be evaluated as “edema”. [
5] Specifically concerning human erythrocytes, their survival during freezing is critically contingent upon the unfrozen fraction and the salt concentration. Alterations in cell volume have been demonstrably shown to exert a profound influence on erythrocyte viability and structural integrity following thawing. [
6]
Awareness of these freeze-thaw artifacts is therefore paramount for accurate interpretation of vitality of a lesion in post-mortem investigations. [
2,
7] The assessment of wound vitality is a critical task in forensic pathology, aiming to definitively establish whether an injury was inflicted ante-mortem, post-mortem. While traditional methods, such as macroscopic examination and routine histological analysis, are used to observe signs of vital reaction (e.g., inflammatory infiltrate or hemorrhage), they are often unreliable due to limitations like operator dependency, staining artifacts, and the non-specificity of findings. Immunohistochemistry (IHC) has gained importance by detecting specific cellular and molecular markers, released or produced by the living organism in response to trauma, such as inflammatory mediators (e.g., cytokines, selectins, chemokines) and stress proteins [
8]. The behavioural standardization of these markers is essential. They can be severely compromised by external factors like decomposition or freezing and thawing cycles, which introduce morphological and chemical artifacts that are challenging to distinguish from true vital reactions. The aim of this paper is to delineate the specific morphological alterations caused by freezing and thawing in cadaveric skin and to systematically determine how these artifacts compromise the accurate post-mortem diagnosis of lesion vitality.
2. Case Report
2.1. Case A
A 67-year-old male cyclist sustained fatal injuries following a rear-end collision with a stationary commercial truck. The entirety of the incident was documented via surveillance footage. Due to subsequent judicial delays, the post-mortem examination was performed 28 days post-mortem, during which time the remains were subjected to two distinct cycles of freezing and thawing for prolonged preservation. The external examination revealed significant traumatic findings, including superficial facial injuries (contusions and lacerations), assessed as having a vital origin, and severe facial trauma was present, characterized by multiple bilateral fractures of the maxillo-malar complex, maxilla, nasal bones, and mandible. Internal findings included fractures of the cervical vertebrae at levels C2, C6, and C7. Notably, the spinal cord appeared macroscopically intact, without evidence of apparent direct traumatic damage. Tissue samples were collected from the upper lip, lower lip, and cervical spinal cord (levels C2, C6, C7) for histological assessment of lesion vitality.
The initial histological investigation using H&E staining failed to reliably demonstrate the presence of extravasated red blood cells at the injury sites, a finding potentially interpreted as a lack of vital reaction. This absence was critically attributed to the severe cellular degradation and osmotic damage induced by the two freeze-thaw cycles. To definitively confirm the vital nature of the observed lesions—a distinction essential for forensic reconstruction—Immunohistochemical staining with anti-human Glycophorin A antibody was employed. The strong positivity observed across all sampled tissues (lips and cervical spinal cord) unequivocally confirmed the presence of antemortem hemorrhage.
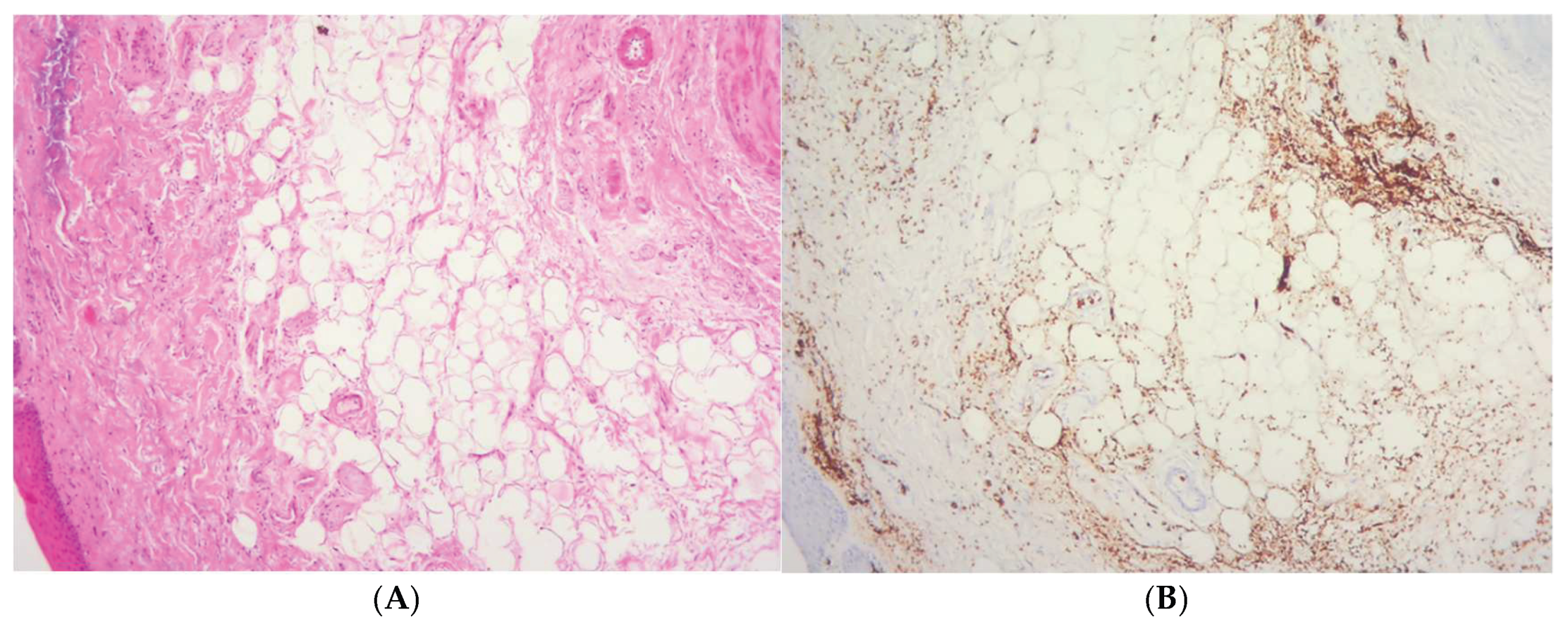
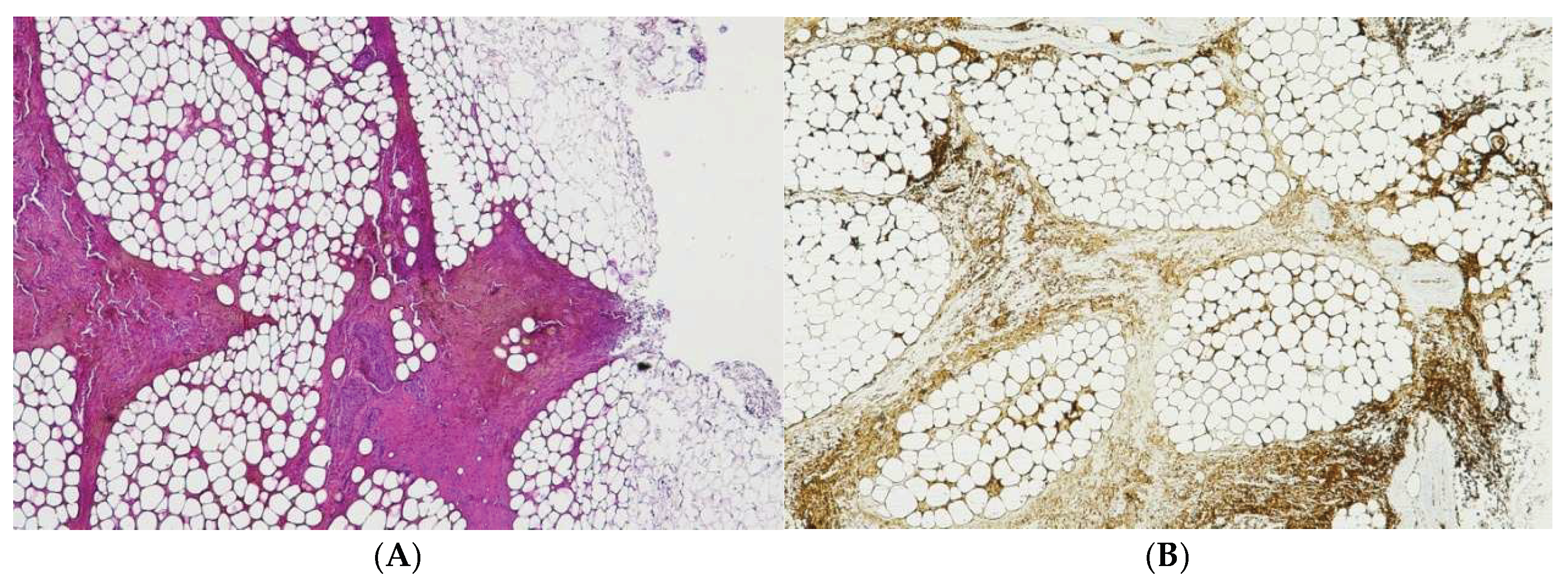
Figure 1.
(A) Histological H&E staining of cutaneous tissue of a macroscopic area of discoloration in which Red Blood Cells (RBC) cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
Figure 1.
(A) Histological H&E staining of cutaneous tissue of a macroscopic area of discoloration in which Red Blood Cells (RBC) cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
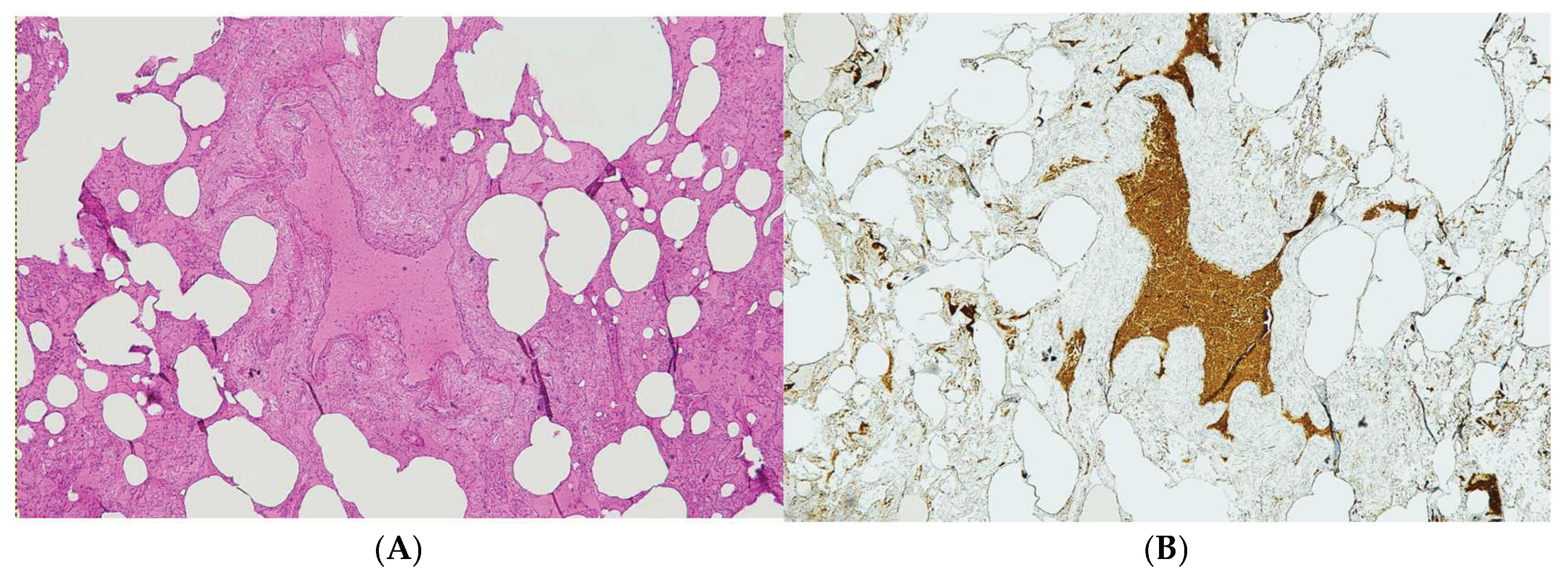
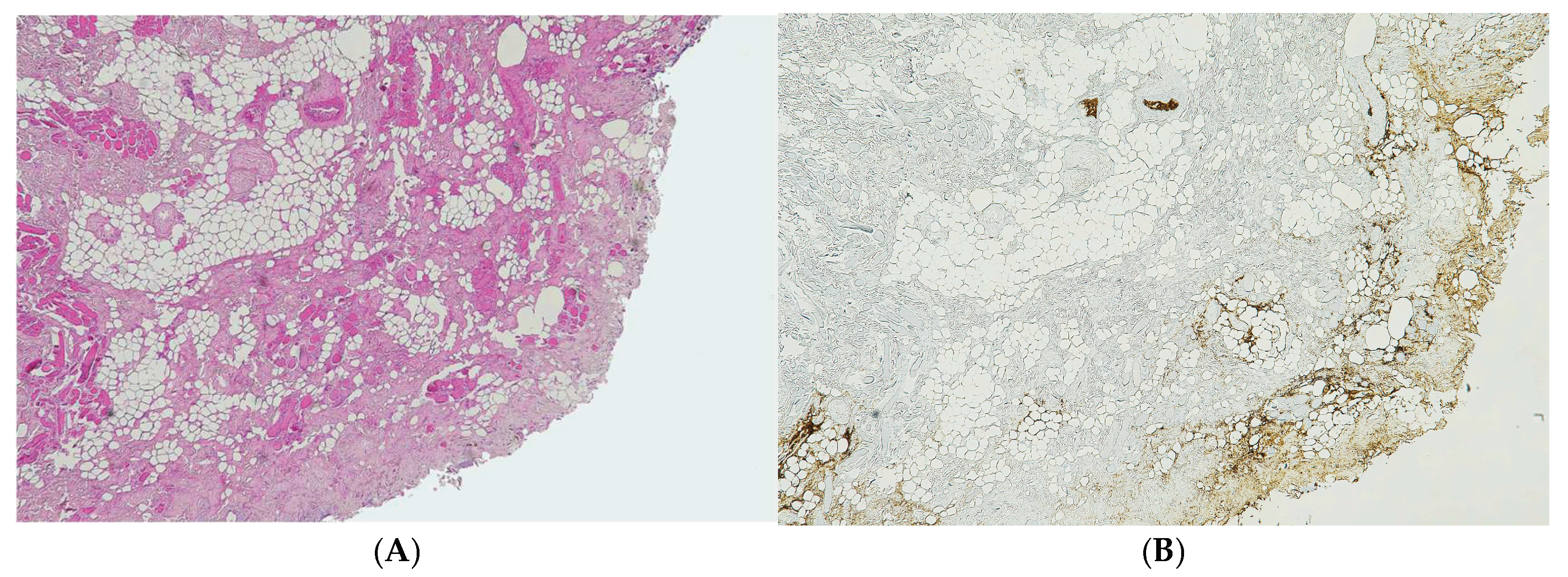
Figure 2.
(A) Histological H&E staining of pulmonary tissue in which can be detected the presence of a vessel with RBCs and eosinophilic areas suspicious of hemorrhagic edema. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample is negative for RBCs extravasation, showing RBCs exclusively inside vessels.
Figure 2.
(A) Histological H&E staining of pulmonary tissue in which can be detected the presence of a vessel with RBCs and eosinophilic areas suspicious of hemorrhagic edema. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample is negative for RBCs extravasation, showing RBCs exclusively inside vessels.
2.2. Case B
An elderly female was found dead inside her residence. Initially, the circumstantial information and evidence gathered framed the case among the deaths due to natural causes. During a preliminary inspection of the body, however, we noticed multiple suspicious ecchymoses on the woman’s upper limbs and face, along with a mark on the right upper limb compatible with acupuncture. Samples of these lesions were collected for histological examinations. The autopsy was then suspended due to criminal procedural issues, and the corpse was stored in a refrigerated environment at -20 °C. The post-mortem examination was then completed after more than a month and revealed the presence of further dubious areas of a reddish coloration. We proceeded to collect multiple tissue samples for histological investigations.
The suspected ecchymotic areas collected during the preliminary assessment were subjected to routine H&E staining and unequivocally confirmed the presence of extravased red blood cells.
Conversely, samples collected after the freeze-thaw cycle were negative for red blood cells with H&E staining. The immunohistochemical staining with anti-GPA antibody was then employed with positivity on most of the samples.
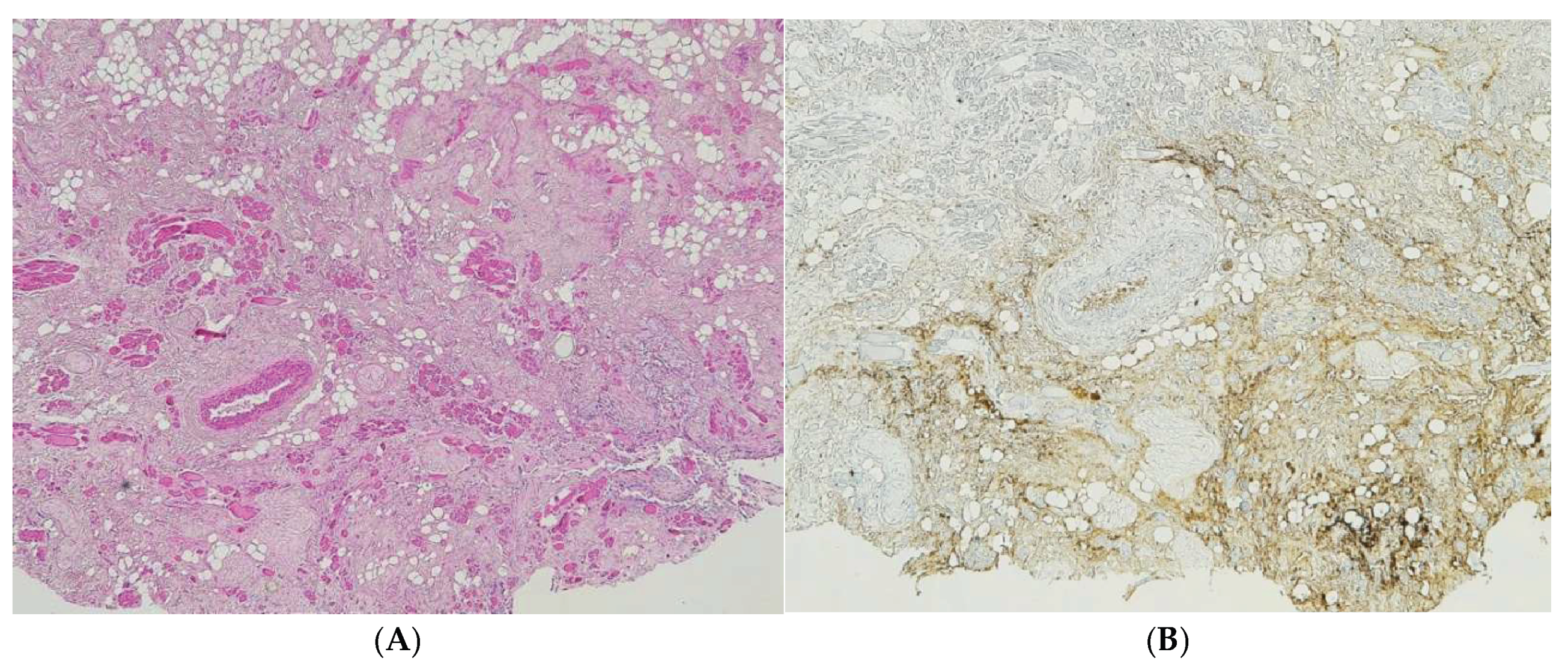
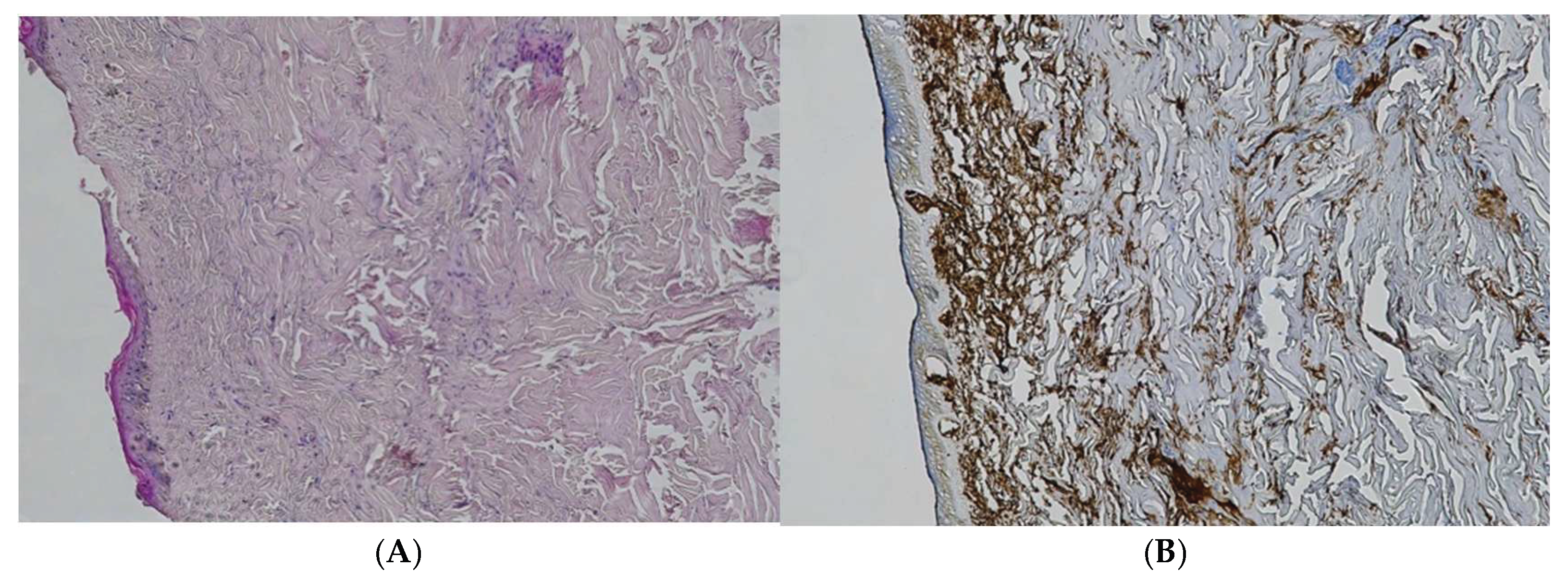
Figure 3.
(A) Histological H&E staining of cutaneous tissue of a macroscopic area of discoloration sampled during the second phase of the autopsy, dubious of RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
Figure 3.
(A) Histological H&E staining of cutaneous tissue of a macroscopic area of discoloration sampled during the second phase of the autopsy, dubious of RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
3. Materials and Methods
Accurately distinguishing between vital (antemortem) and postmortem lesions is fundamental and critical in forensic autopsies and criminal investigations. The initial step in this assessment is to determine the presence of erythrocyte extravasation in the surrounding tissues. This is conventionally performed using hematoxylin and eosin (H&E) staining. However, in cadavers subjected to freeze-thaw cycles, this standard technique may fail to reliably detect such extravasation.
To establish a standardized approach for evaluating lesions in such modified tissue, we utilized samples from 10 autopsy cases involving traumatic deaths. We employed both histochemical and immunohistochemical staining techniques to assess lesion vitality. An anti-GPA monoclonal antibody was used as an indirect marker for red blood cells. This specificity is crucial, as it avoids the diffusion artifacts common with markers such as hemoglobin, which can passively diffuse from blood vessels into surrounding tissues, creating false positives.
For each case, skin samples exhibiting coloration indicative of ecchymosis were collected. From each sample, a tissue ribbon was immediately excised and processed using a 10% formalin solution, sliced, and stained with H&E (Group 1). This group served as the positive control. The remaining tissue was then frozen at -20 °C. After a 15-day interval, these samples were thawed, a second tissue ribbon was excised, processed identically to Group 1, and subsequently with the anti-GPA monoclonal antibody (Group 2). Following an additional 15-day period, the samples were subjected to a second freeze-thaw cycle and processed and stained as described for Group 2 (Group 3).
The tissues from all three groups were then subjected to microscopic examination, and the results from the experimental groups (Group 2 and Group 3) were systematically compared to the control group (Group 1).
To validate the diagnostic specificity of the anti-GPA antibody and confirm the absence of non-specific binding, an additional sample of adjacent, macroscopically undamaged skin tissue was processed identically to the experimental groups and utilized as a negative tissue control (Group 4).
4. Results
Histological examinations using H&E staining were initially performed to microscopically assess the presence and extent of red blood cell extravasation, a classic indicator of lesion vitality.
In the control group (T0), which comprised fresh, unfrozen tissue samples, H&E staining unambiguously demonstrated diffuse hemorrhagic infiltration within the dermal layer across all investigated specimens. This confirmed the baseline presence of antemortem trauma. The analysis of samples subjected to a single freeze-thaw cycle (T1) revealed a notable degradation in the diagnostic reliability of H&E staining, evidenced by a diminished or equivocal visualization of extravased erythrocytes compared to the control. Crucially, however, the immunohistochemical analysis using the anti-human GPA monoclonal antibody yielded unequivocally positive results, albeit indirect, for RBCs in all Group 2 samples. The impact of the artifacts became pronounced in tissues exposed to two freeze-thaw cycles (T2). In this cohort, H&E staining was rendered unreliable, often failing to detect or unambiguously identify the presence of red blood cells due to severe cellular degradation and morphological alterations. Despite this significant post-mortem artifact, the specificity and resilience of the GPA staining technique persisted, as it yielded positive detection of RBC membrane material in every sample tested.
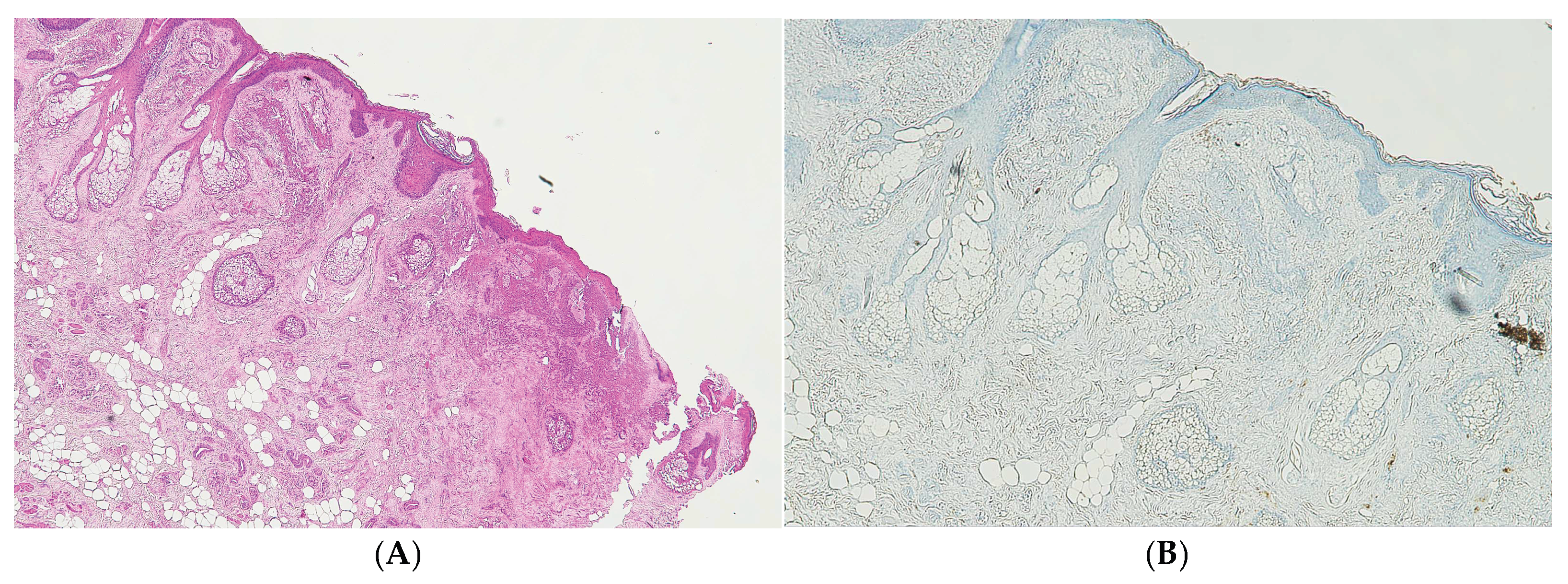
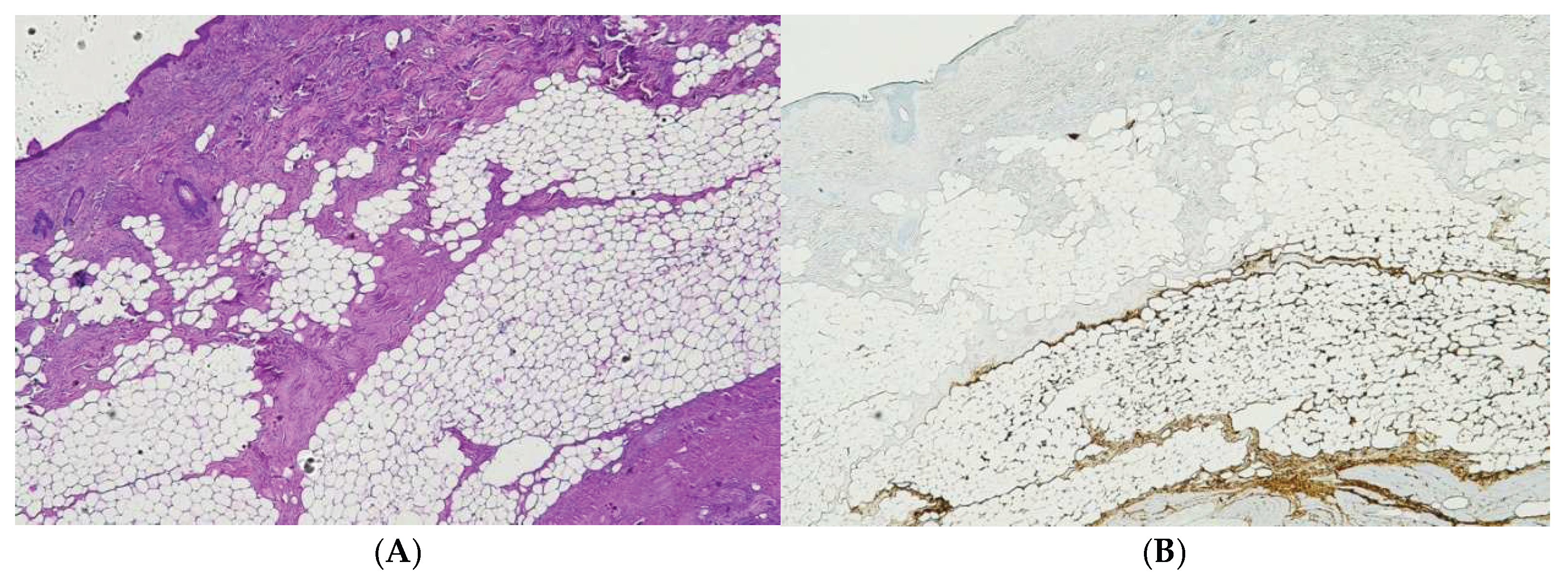
Figure 4.
(A) Histological H&E staining of cutaneous tissue of Group 4 in which can be detected the presence of a vessel with RBCs and areas suspicious for RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample is negative for RBCs extravasation, showing RBCs exclusively inside vessels.
Figure 4.
(A) Histological H&E staining of cutaneous tissue of Group 4 in which can be detected the presence of a vessel with RBCs and areas suspicious for RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample is negative for RBCs extravasation, showing RBCs exclusively inside vessels.
Figure 5.
(A) Histological H&E staining of cutaneous tissue of Group 0, positive for RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation.
Figure 5.
(A) Histological H&E staining of cutaneous tissue of Group 0, positive for RBCs extravasation. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation.
Figure 6.
(A) Histological H&E staining of cutaneous tissue of Group 1, dubious for RBCs extravasation. Some areas show the presence of eosinophilic pigment. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
Figure 6.
(A) Histological H&E staining of cutaneous tissue of Group 1, dubious for RBCs extravasation. Some areas show the presence of eosinophilic pigment. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody, positive for RBCs extravasation. The sample shows the presence RBCs in some of the areas that were marked as dubious in the H&E staining.
Figure 7.
(A) Histological H&E staining of cutaneous tissue of Group 2 in which RBCs cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample shows extensive presence RBCs extravasation.
Figure 7.
(A) Histological H&E staining of cutaneous tissue of Group 2 in which RBCs cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample shows extensive presence RBCs extravasation.
Figure 8.
(A) Histological H&E staining of cutaneous tissue of Group 2 in which RBCs cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample shows extensive presence RBCs extravasation.
Figure 8.
(A) Histological H&E staining of cutaneous tissue of Group 2 in which RBCs cannot be identified. (B) Immunohistochemical staining of cutaneous tissue with anti-GPA monoclonal antibody. The sample shows extensive presence RBCs extravasation.
Table 1.
This table summarizes the results of the experimental study.
Table 1.
This table summarizes the results of the experimental study.
| Subject |
T0 (H&E) |
T1 (H&E) |
T1 (GPA) |
T2 (H&E) |
T2 (GPA) |
| 1 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 2 |
Positive |
Inconclusive |
Positive |
Negative |
Positive |
| 3 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 4 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 5 |
Positive |
Inconclusive |
Positive |
Negative |
Positive |
| 6 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 7 |
Positive |
Inconclusive |
Positive |
Negative |
Positive |
| 8 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 9 |
Positive |
Negative |
Positive |
Negative |
Positive |
| 10 |
Positive |
Inconclusive |
Positive |
Negative |
Positive |
5. Discussion
The accurate distinction between vital and postmortem lesions remains a cornerstone of forensic pathology and determinant in criminal investigations. The accuracy of this determination not only directs the reconstruction of events but profoundly influences the final legal judgement. In routine practices, the approach still relies on macroscopic examination and routine histological analysis, which search for classic signs of vital reaction (e.g., inflammatory infiltrate, fibrin deposition, or collagen retraction). However, as widely acknowledged in the literature, these methods exhibit significant limitations: standard histology is prone to operator dependency, potential staining artifacts, and critically, the non-specificity of findings, as similar alterations can sometimes manifest in non-vitally injured tissues. To overcome these deficiencies, modern forensic pathology has integrated more sensitive and specific techniques. Immunohistochemistry, based on antigen-antibody reaction, has taken a prominent role by enabling the localization and quantification of molecular markers released in response to trauma, such as inflammatory mediators (cytokines, chemokines) and cellular stress proteins. [
8,
9]
A significant and often underappreciated complication arises when cadavers are subjected to freeze-thaw cycles prior to autopsy. This process has been demonstrated to induce profound histological artifacts, and, therefore, false negatives that can effectively obscure or eliminate critical investigative evidence. In cases of violent death, the capacity to confirm a hemorrhagic lesion’s vital origin is pivotal to directing the course of the forensic investigation. The unreliability of the H&E staining in these compromised corpses is hypothesized to result from severe shrinkage and structural disruption of erythrocyte microstructures caused by osmotic stress during the freeze-thaw process.
While literature addressing the histological artifacts of freeze-thaw cycles is not as extensive as desirable, significant alterations have been consistently reported. Freezing induces major changes, including the loss of cellular affinity for routine stains, extracellular fluid accumulation, cellular shrinkage, tissue clefts/fractures, hemolysis, and hematin formation. More subtle alterations include the loss of bronchial cilia and the increased prominence of collagen in alveolar septa and meninges. [
3,
10] The most consistently observed artifacts are the expansion of extracellular spaces and pronounced cell shrinkage. Organs with high fluid content and cellular density, such as the heart and liver, are often the most significantly impacted. Generally, strong basophilic nuclear staining and hemolysis are widespread across most tissues. [
11,
12]
We investigated two cases in which macroscopic examination showed the presence of ecchymosis and excoriations. However, routine histological investigation of the skin lesions failed to identify the presence of red blood cells in the subcutaneous tissue. Microscopic examination of these samples revealed characteristic freeze-thaw artifacts, including extracellular space expansion, tissue clefts, and cellular shrinkage. Furthermore, karyopyknosis and vacuolization of the epidermis, consistent with observations by Tabata et al., were evident in the H&E-stained sections. [
13] The unequivocal demonstration of the diagnostic limitation of routine Hematoxylin and Eosin staining for evaluating wound vitality due to cryopreservation artifacts in this case provided the rationale for an experimental study. This subsequent research aimed to define and standardize the application of the Glycophorin A immunomarker as a robust and specific alternative for identifying erythrocytes in samples compromised by repeated freeze-thaw cycles.
To overcome the diagnostic limitations-imposed freeze-thaw artifacts, immunohistochemical staining with an anti-human GPA monoclonal antibody should be used. Glycophorin (GPA, GPB, GPC, and GPD) are a family of transmembrane proteins that constitute approximately 2% of the total RBC membrane proteins mass, with GPA being the predominant species. GPA is an ideal marker because its localization to the cell membrane provides high specificity for erythrocyte remnants, unlike cytoplasmic markers (e.g., hemoglobin) which can diffuse into surrounding tissue following cell rupture. Clinical medicine uses GPA antibodies extensively to identify erythroid precursors, and this application is highly transferable to forensic pathology for the reliable identification of RBCs in compromised tissues. [
14]
Previous forensic studies have validated the utility of immunohistochemistry in bodies subjected to tissue-altering conditions. Research on corpses dying from hypothermia demonstrated that certain antigen identification remains possible despite tissue alteration. [
3,
10,
11] Specifically, Baldari et al. confirmed that anti-human GPA antibodies effectively detect RBCs across different postmortem intervals, indicating robustness against general degradation. [
15] Furthermore, Cattaneo et al. successfully employed GPA antibodies to identify clots and RBC residues on bone fracture margins, establishing a positive GPA reaction as strongly indicative of a vital reaction. [
16] Consequently, anti-human GPA antibodies are increasingly recognized as a reliable marker for investigating erythrocytic residues in poorly preserved or compromised tissues.
In alignment with the current literature, our study provides concrete evidence that immunohistochemical analysis using anti-human Glycophorin A antibodies successfully identified hemorrhage in skin samples after both one and two freeze-thaw cycles. This finding is significant given the limited research specifically detailing the effect of freeze-thaw cycles on erythrocyte integrity in situ. Ishiguro et al.’s work on RBCs in saline demonstrated rupture due to freezing damage, supporting the physical mechanism that leads to the disappearance of visible red blood cells in H&E sections. [
17]
The practical necessity for this research is highlighted by the procedural technicalities within judicial systems, such as the Italian system, which may mandate repeated cycles of freezing and thawing—particularly in medical malpractice judicial autopsies—to ensure meticulous evidence preservation prior to expert examination. Forensic experts must therefore be acutely aware of the severe freeze-thaw phenomenon and the pivotal diagnostic superiority of IHC with GPA in these challenging cases.
This study successfully validates the use of GPA staining to accurately evaluate the vitality of skin wounds despite severe freeze-thaw induced artifacts. However, because skin is not the only organ affected, further studies are critically needed to empirically determine the applicability and efficacy of GPA immunohistochemical staining in other organs, especially those most susceptible to freeze-thaw damage (e.g., heart, liver), to establish a truly comprehensive and standardized protocol for compromised forensic samples.
6. Conclusions
The results of the present study have the potential to make significant contributions to the field of forensic pathology. Procedural technicalities may necessitate that a corpse undergo repeated cycles of freezing and thawing prior to an autopsy. In the event of prolonged preservation, post-mortem changes have the potential to obscure evidence of traumatic injuries. The use of immunohistochemical staining using anti-human Glycophorin A antibody to detect the presence of red blood cells is therefore critical in such investigations.
Author Contributions
Conceptualization, N.I and M.D.P.; methodology, E.T.; software, S.G.; validation, N.I., E.T. and M.D.P.; formal analysis, S.G.; investigation, S.G.; resources, N.I.; data curation, N.I.; writing—original draft preparation, N.I.; writing—review and editing, M.D.P.; visualization, M.D.P.; supervision, E.T.; project administration, N.I.; funding acquisition, M.D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author(s).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
GP: Glycophorin
H&E: Hematoxylin and Eosin
IHC: Immunohistochemistry
RBC: Red Blood Cell
T: time |
References
- Menz, L.J. Structural changes and impairment of function associated with freezing and thawing in muscle, nerve, and leucocytes. Cryobiology 1971, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, E.; Bonasoni, M.P.; Bardaro, M.; Russello, G.; Carretto, E.; Zerbini, A.; Gargano, G.; Pelotti, S. Postmortem histological freeze–thaw artifacts: a case report of a frozen infant and literature review. Forensic Sci Med Pathol 2023. [Google Scholar] [CrossRef] [PubMed]
- Baraibar, M.A.; Schoning, P. Effects of freezing and frozen storage on histological characteristics of canine tissues. J Forensic Sci 1985, 30, 439–447. [Google Scholar] [CrossRef]
- Schäfer, A. Th.; Kaufmann, J.D. What happens in freezing bodies? Forensic Science International 1999, 102, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Tabata, N.; Funayama, M.; Ikeda, T.; Azumi, J.; Morita, M. On an accident by liquid nitrogen — histological changes of skin in cold. Forensic Science International 1995, 76, 61–67. [Google Scholar] [CrossRef]
- Mazur, P.; Cole, K. Contact between shrunken red cells as a factor in freezing injury. Cryobiology 1988, 25, 510–511. [Google Scholar] [CrossRef]
- Micozzi, M. Experimental Study of Postmortem Change Under Field Conditions: Effects of Freezing, Thawing, and Mechanical Injury. Journal of Forensic Sciences 1986, 31, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Manetti, A.C.; Iacoponi, N.; Mezzetti, E.; Turillazzi, E.; Di Paolo, M.; La Russa, R.; Frati, P.; Fineschi, V. State-of-the-Art on Wound Vitality Evaluation: A Systematic Review. IJMS 2022, 23, 6881. [Google Scholar] [CrossRef] [PubMed]
- Casse, J.-M.; Martrille, L.; Vignaud, J.-M.; Gauchotte, G. Skin wounds vitality markers in forensic pathology: An updated review. Med Sci Law 2016, 56, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Baraibar, M.A.; Schoning, P. Microscopic diagnosis from frozen canine tissues. J Forensic Sci 1986, 31, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Pechal, J.L.; Schmidt, C.J.; Jordan, H.R.; Benbow, M.E. Frozen: Thawing and Its Effect on the Postmortem Microbiome in Two Pediatric Cases. Journal of Forensic Sciences 2017, 62, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Kozawa, S.; Kakizaki, E.; Yukawa, N. Autopsy of two frozen newborn infants discovered in a home freezer. Legal Medicine 2010, 12, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Knight, B.; Saukko, P.J. Knight’s forensic pathology, Fourth edition; CRC Press, Taylor & Francis Group: Boca Raton, 2016. [Google Scholar]
- Sadahira, Y.; Kanzaki, A.; Wada, H.; Yawata, Y. Immunohistochemical identification of erythroid precursors in paraffin embedded bone marrow sections: spectrin is a superior marker to glycophorin. J Clin Pathol 1999, 52, 919–921. [Google Scholar] [CrossRef] [PubMed]
- Baldari, B.; Vittorio, S.; Sessa, F.; Cipolloni, L.; Bertozzi, G.; Neri, M.; Cantatore, S.; Fineschi, V.; Aromatario, M. Forensic Application of Monoclonal Anti-Human Glycophorin A Antibody in Samples from Decomposed Bodies to Establish Vitality of the Injuries. A Preliminary Experimental Study. Healthcare 2021, 9, 514. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, C.; Andreola, S.; Marinelli, E.; Poppa, P.; Porta, D.; Grandi, M. The Detection of Microscopic Markers of Hemorrhaging and Wound Age on Dry Bone: A Pilot Study. American Journal of Forensic Medicine & Pathology 2010, 31, 22–26. [Google Scholar] [CrossRef]
- Ishiguro, H.; Rubinsky, B. Mechanical Interactions between Ice Crystals and Red Blood Cells during Directional Solidification. Cryobiology 1994, 31, 483–500. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).