Background
The differentials for optic disc oedema are broad and diagnosis is guided by careful and thorough history taking, examination, and further investigations, including imaging. Hypotony is generally defined statistically as intraocular pressure (IOP) below 6.5 mmHg or clinically as when a patient’s IOP is so low that there is resultant visual loss [
1]. It is an uncommon cause of optic disc oedema and may lead to visual loss [
1]. Hypotony can cause maculopathy, chorioretinal folds, vascular tortuosity, and optic disc oedema [
2]. The most common causes include glaucoma surgery, trauma, intraocular inflammation, and the use of IOP-lowering medications [
1]. We report a diagnostically complex case of hypotony-related optic disc oedema and visual decline in a young woman with juvenile idiopathic arthritis (JIA)-associated uveitis, secondary glaucoma, and probable idiopathic intracranial hypertension (IIH). We discuss the concept of the translaminar pressure gradient (TLPG), proposing a dual pathology where acute hypotony precipitated marked optic disc oedema in a patient with probable underlying raised intracranial pressure (ICP).
Case Presentation
Presenting Complaint and History
A 20-year-old Caucasian woman was referred to neuro-ophthalmology with a gradual loss of vision and photopsia in her left eye over several months. There was no associated pain, headache, nausea, vomiting, or postural variation.
Her ocular history was extensive and included HLA-B27-positive JIA, bilateral JIA-associated anterior uveitis, bilateral secondary glaucoma, dense amblyopia in the right eye, bilateral cataract extraction, and probable IIH. One year earlier, she had presented with headaches and papilloedema. Magnetic resonance imaging (MRI) demonstrated posterior scleral flattening with intra-optic nerve head disc protrusion and mild CSF distension of the optic nerve sheaths, consistent with papilloedema. A lumbar puncture (LP), performed while taking acetazolamide (750 mg/day for elevated IOP), recorded an opening pressure of 20 cm H2O. Symptoms improved on acetazolamide and a working diagnosis of IIH was made.
The patient was under ongoing glaucoma care due to chronic IOP elevation secondary to steroid use, uveitis, and aqueous misdirection. Aqueous shunt surgery (Paul tube implantation) had been performed in the left eye the year prior, however, continued to experience fluctuating IOP. She was also under the uveitis team for difficult-to-control uveitis, with her treatment complicated by poor tolerance of systemic immunosuppression (including methotrexate) and failure of multiple biologics. She was receiving infliximab at the time of the clinic.
Over a few months, she had attended multiple ophthalmology clinics (glaucoma, uveitis, and eye casualty) with recurring symptoms of worsening vision in her left eye. Examination at several of these visits showed bilateral optic disc swelling. She had experienced ongoing erratic IOP in the left eye following shunt implantation, with documented spikes up to 52 mmHg and troughs as low as 8 mmHg. During episodes of high IOP, anterior chamber paracentesis was performed to release viscoelastic (Healon). Optic disc swelling appeared to worsen in the left eye at an IOP of 10 mmHg and she was noted to have findings consistent with hypotony maculopathy, such as retinal folds, in the left eye. Her ocular hypotensive medications were stopped, further investigations (including neuroimaging and repeat LP) were arranged, and she was referred to the neuro-ophthalmology team.
Examination Findings
At the neuro-ophthalmology clinic, her visual acuity (VA) was 3/60 unaided (5/60 with pinhole) in the left eye and counting fingers (baseline) in the amblyopic right eye. IOP was 8 mmHg in the left eye and 23 mmHg in the right eye. Examination of the anterior segment of the left eye revealed 0.5+ anterior chamber cells. Fundus examination demonstrated marked optic disc swelling with venous tortuosity, which was significantly worse than on previous reviews. The fundus view was limited in the right eye because of band keratopathy, but demonstrated milder disc swelling.
Investigations
Neuroimaging was reassuring, with no evidence of optic nerve enhancement or mass lesion. Imaging appearances were suggestive of IIH. A repeat LP demonstrated normal opening pressure of 20 cm H
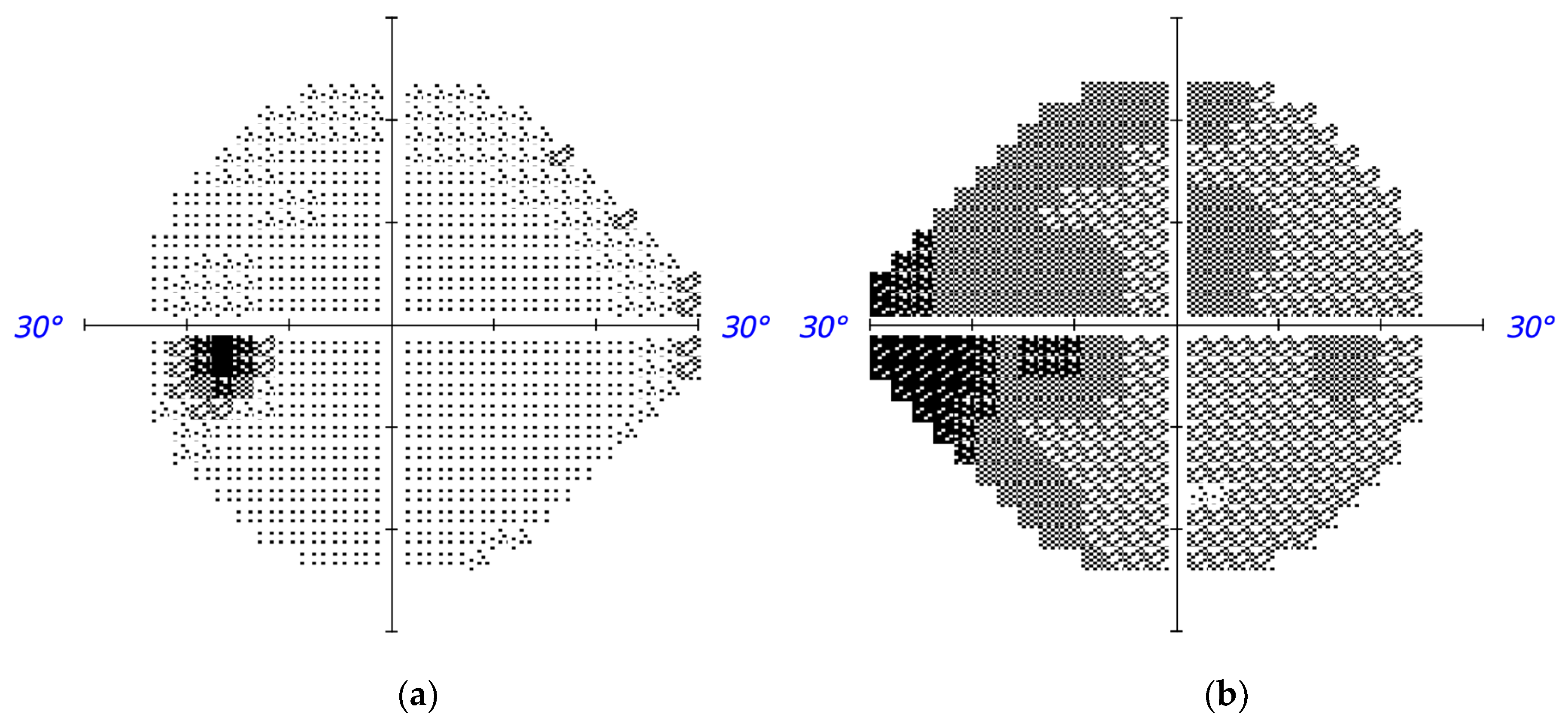
2O; oligoclonal bands were present in both the CSF and serum, indicating a systemic inflammatory process consistent with JIA rather than demyelinating disease. Visual fields (VFs) showed stable amblyopic suppression scotoma in the right eye and no significant VF defects in the left eye (
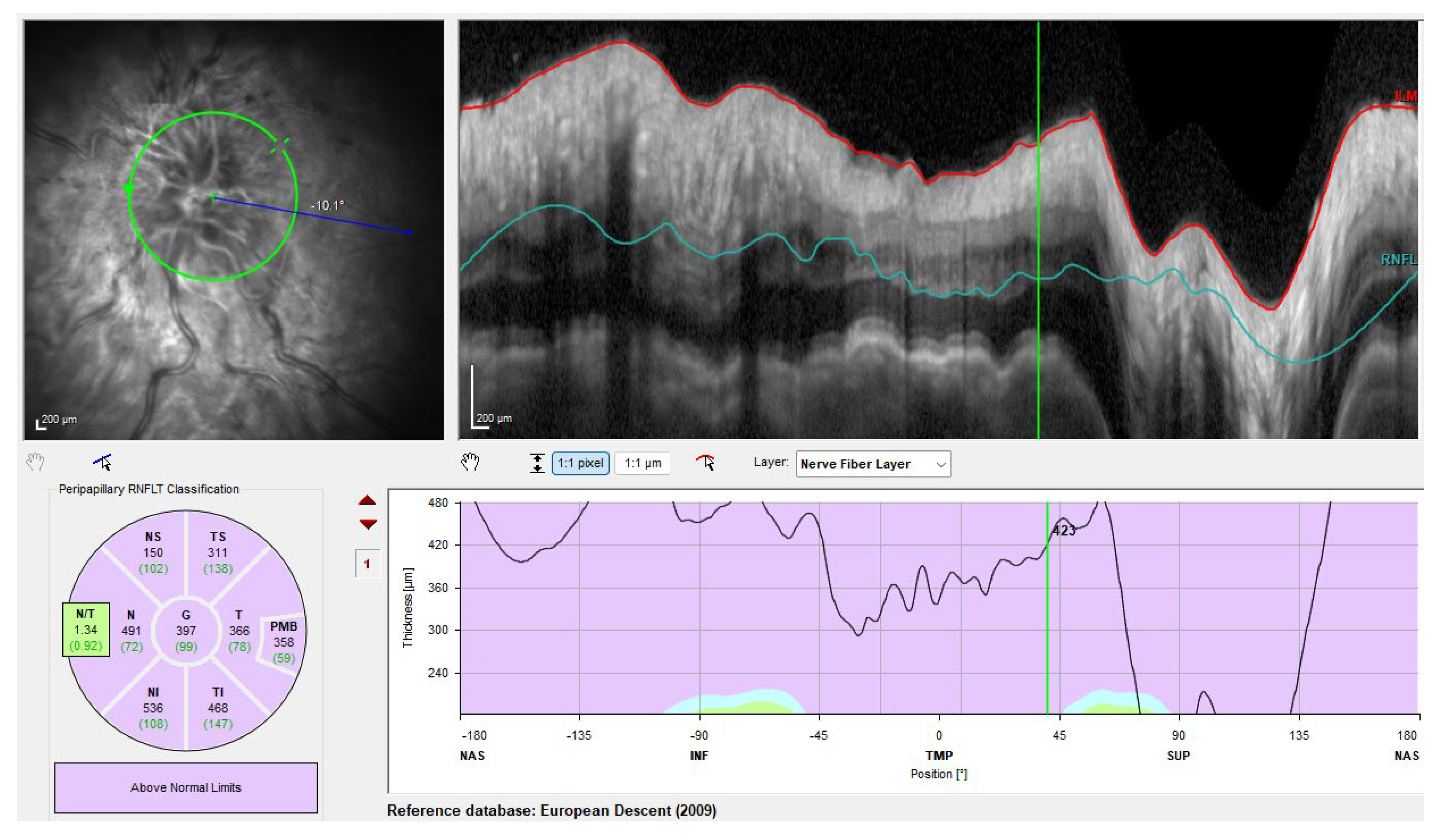
Figure 1). Optical coherence tomography (OCT) revealed a significantly swollen left optic disc (
Figure 2).
Diagnosis
The presence of bilateral disc swelling, with significantly more marked optic disc swelling in the left eye, prompted investigation for causes of intracranial and ocular disease. The working differentials included causes of raised ICP such as space-occupying lesion and IIH, uveitis-related optic nerve inflammation, optic neuritis, and hypotony-related optic disc oedema. No structural intracranial cause for disc swelling was found. Optic neuritis was largely ruled out by negative neuroimaging, reassuring VFs, and CSF findings consistent with systemic inflammation.
The consensus was that the patient’s recent hypotony episodes were the primary driver of visual decline and marked optic disc oedema in her left eye. The less severe bilateral disc swelling was attributed to probable underlying IIH. The normal LP opening pressure may have reflected technical factors (e.g., multiple passes) and/or natural diurnal ICP fluctuations [
3]. The patient was urgently referred to the glaucoma team for management of hypotony.
Treatment and Outcome
The patient underwent revision of the left aqueous shunt. The previous tube was replaced and the anterior chamber was reformed with Healon to stabilise the IOP. Postoperative results were positive with IOP rising to 32 mmHg in the left eye, VA improving to 6/12 unaided (6/9.5 with pinhole), and fundus exam and OCT demonstrating notable improvement in left eye optic disc oedema. The clinical improvement following intervention supported the diagnosis of hypotony maculopathy as the primary cause of this patient’s symptoms.
Discussion
This case highlights the diagnostic complexity of distinguishing hypotony-related optic disc oedema from other differentials in a patient with a complex ocular history, including JIA-associated uveitis and probable IIH. In this patient, recent glaucoma shunt surgery, fluctuating IOP with episodes of low IOP, and recurrent inflammation placed her at high risk for hypotony-associated complications. We hypothesise the presence of dual pathologies in this case: the presence of underlying IIH with concurrent hypotony resulting in papilloedema and marked left optic disc swelling. Surgical revision and restoration of IOP led to marked anatomical and visual improvement. Failure to address hypotony can result in irreversible macular and optic nerve changes and permanent visual loss [
1].
The TLPG, defined as the pressure differential across the lamina cribrosa (LC), is a key determinant of optic nerve head biomechanics [
4]. It reflects the balance between IOP and cerebrospinal fluid pressure (CSFP) [
4]. When IOP exceeds CSFP, posterior LC displacement contributes to glaucomatous cupping, whereas CSFP dominance (from raised ICP or reduced IOP) causes anterior displacement and optic disc oedema [
4,
5]. Experimental work has further clarified the mechanisms of hypotony-related swelling. In primate models, hypotony induced fluid leakage from the choriocapillaris into peripapillary tissues, leading to disc oedema [
6]. Minckler and Bunt demonstrated that IOP reduction disrupts axoplasmic transport, with constriction of axonal bundles at the lamina cribrosa and Bruch’s membrane contributing to swelling [
7]. Inflammatory processes, such as JIA-associated uveitis, may further increase vascular permeability and tissue fragility, exacerbating hypotony-related disc changes. In our case, a sharp fall in IOP shifted the TLPG in favour of CSFP, resulting in anterior LC displacement and optic disc oedema. We speculate that optic nerve oedema may occur at a relatively higher IOP in a patient with raised ICP because of the TLPG effect. This could explain her worsening of disc swelling even at IOPs of 10 mmHg.
In patients with inflammatory eye disease, particularly children or young adults with JIA-associated uveitis, the risk of hypotony is increased because of chronic inflammation resulting in decreased aqueous humour production by the ciliary body [
1]. Studies report hypotony in up to 15.6% of patients with JIA-associated uveitis, with bilateral disease, longer uveitis duration, and more severe disease associated with higher risk of developing ocular hypotony [
8,
9]. In these studies, immunosuppression was associated with a lower risk of hypotony, suggesting that control of inflammation may reduce the risk of hypotony in JIA-associated uveitis [
8,
9]. This patient had a complex history of difficult-to-control uveitis, which may have exacerbated or increased the risk of hypotony. Monitoring for hypotony and its complications along with aggressive control of inflammation is therefore essential in this cohort.
Conclusion
To our knowledge, there are no other reports describing hypotony maculopathy presenting with marked optic disc oedema in the context of secondary glaucoma, JIA-associated uveitis, and probable IIH. The overlapping risk factors in this young adult created a challenging diagnostic landscape. This case demonstrates that hypotony-related optic disc oedema may occur at relatively higher IOPs in patients with underlying raised ICP due to the TLPG effect. The dramatic visual recovery following surgical intervention reinforces the importance of timely recognition of hypotony-related disc oedema and prompt correction of hypotony, as delayed intervention can lead to irreversible optic nerve and macular damage.
Author Contributions
Conceptualisation, Wei Jia Liu and Jasvir Virdee.; clinical care of patient and acquisition of data, Jasvir Virdee.; interpretation of clinical and imaging findings, Wei Jia Liu and Jasvir Virdee.; writing—original draft preparation, Wei Jia Liu.; writing—review and editing, Wei Jia Liu and Jasvir Virdee.; supervision, Jasvir Virdee. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from the patient involved in this case study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
All relevant data supporting the findings of this case report are included within the article. Additional data are not publicly available due to patient confidentiality.
Acknowledgments
The authors would like to acknowledge the University Hospital Southampton Ophthalmology department for their support in the clinical care of the patient and the acquisition of ophthalmic investigations.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| JIA |
Juvenile idiopathic arthritis |
| IOP |
Intraocular pressure |
| IIH |
Idiopathic intracranial hypertension |
| TLPG |
Translaminar pressure gradient |
| CSF |
Cerebrospinal fluid |
| VA |
Visual acuity |
| VF |
Visual field |
| OCT |
Optical coherence tomography |
| LP |
Lumbar puncture |
| CSFP |
Cerebrospinal fluid pressure |
| LC |
Lamina cribrosa |
References
- Thomas, M; Vajaranant, TS; Aref, AA. Hypotony Maculopathy: Clinical Presentation and Therapeutic Methods. Ophthalmol Ther. 2015, 4(2), 79–88. [Google Scholar] [CrossRef] [PubMed]
- Costa, VP; Arcieri, ES. Hypotony maculopathy. Acta Ophthalmol Scand. 2007, 85(6), 586–597. [Google Scholar] [CrossRef] [PubMed]
- Machiele, R; Frankfort, BJ; Killer, HE; Fleischman, D. Problems in CSF and ophthalmic disease research. Front Ophthalmol. 2022, 2, 845173. [Google Scholar] [CrossRef] [PubMed]
- Villarruel, JM; Li, XQ; Bach-Holm, D; Hamann, S. Anterior lamina cribrosa surface position in idiopathic intracranial hypertension and glaucoma. Eur J Ophthalmol. 2017, 27(1), 55–61. [Google Scholar] [CrossRef] [PubMed]
- Berdahl, JP; Yu, DY; Morgan, WH. The translaminar pressure gradient in sustained zero gravity, idiopathic intracranial hypertension, and glaucoma. Med Hypotheses 2012, 79(6), 719–724. [Google Scholar] [CrossRef] [PubMed]
- Floyd, BB; Minckler, DS. Increased vascular permeability in disc swelling produced by ocular hypotony. Exp Eye Res. 1983, 36(1), 3–13. [Google Scholar] [CrossRef] [PubMed]
- Minckler, DS; Bunt, AH. Axoplasmic transport in ocular hypotony and papilledema in the monkey. Arch Ophthalmol. 1977, 95(8), 1430–1436. [Google Scholar] [CrossRef] [PubMed]
- Böhm, MR; Tappeiner, C; Breitbach, MA; Zurek-Imhoff, B; Heinz, C; Heiligenhaus, A. Ocular Hypotony in Patients With Juvenile Idiopathic Arthritis-Associated Uveitis. Am J Ophthalmol. 2017, 173, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Moradi, A; Stroh, IG; Reddy, AK; Hornbeak, DM; Leung, TG; Burkholder, BM; et al. Risk of Hypotony in Juvenile Idiopathic Arthritis-Associated Uveitis. Am J Ophthalmol. 2016, 169, 113–124. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).