1. Introduction
Advances in machine learning (ML), intelligent systems, and deep learning have enabled a wide range of applications, from efficient information transmission to real-time decision making. Artificial Intelligence (AI) is increasingly transforming communication systems by supporting fast and reliable decision making, behavioral pattern identification, delay reduction, and timely delivery of information records [
1,
2]. In particular, AI has attracted considerable attention in the healthcare domain, where it is used for patient health monitoring, therapeutic response modeling, accurate prediction of clinical events, and rapid decision making through fast and efficient communication protocols [
8].
Extensive research has been carried out in which organizations have adopted new techniques, methods, and schemes in their respective domains to provide efficient, effective, and seamless communication or information transmission [
3,
4,
5]. The integration of smart systems and intelligent devices with traditional record-based applications not only enhances communication but also improves the overall performance of the underlying network. The healthcare sector is widely recognized as one of the most critical domains for modernizing traditional approaches to treatment and record management [
6,
10]. The use of intelligent systems, ML, and AI techniques can provide a broad set of novel solutions and approaches for diagnosis, prediction, and decision-making. Furthermore, the management of patient records, including the preservation of data integrity and privacy, can be strengthened through a variety of ML/AI-based and security-oriented mechanisms [
7,
11].
1.1. Motivation and Objective
A large number of schemes and approaches have been proposed by researchers and practitioners to improve healthcare systems using AI/ML and other intelligent techniques. Existing work has focused on record management, information security, and the secure transmission of patient records. In addition, several schemes have been designed for real-time decision making and accurate prediction while analyzing and collecting raw information from intelligent devices.
However, healthcare scenarios are characterized by highly sensitive and confidential data, and the volume of patient records continues to grow. Handling such a large amount of information is challenging, and generating reliable predictions and sound decisions in this context is both crucial and delicate [
1,
24]. Therefore, there is a clear need for new techniques and methods that make the transmission of records, disease prediction, and real-time decision making more convenient, robust, and efficient.
1.2. Contribution
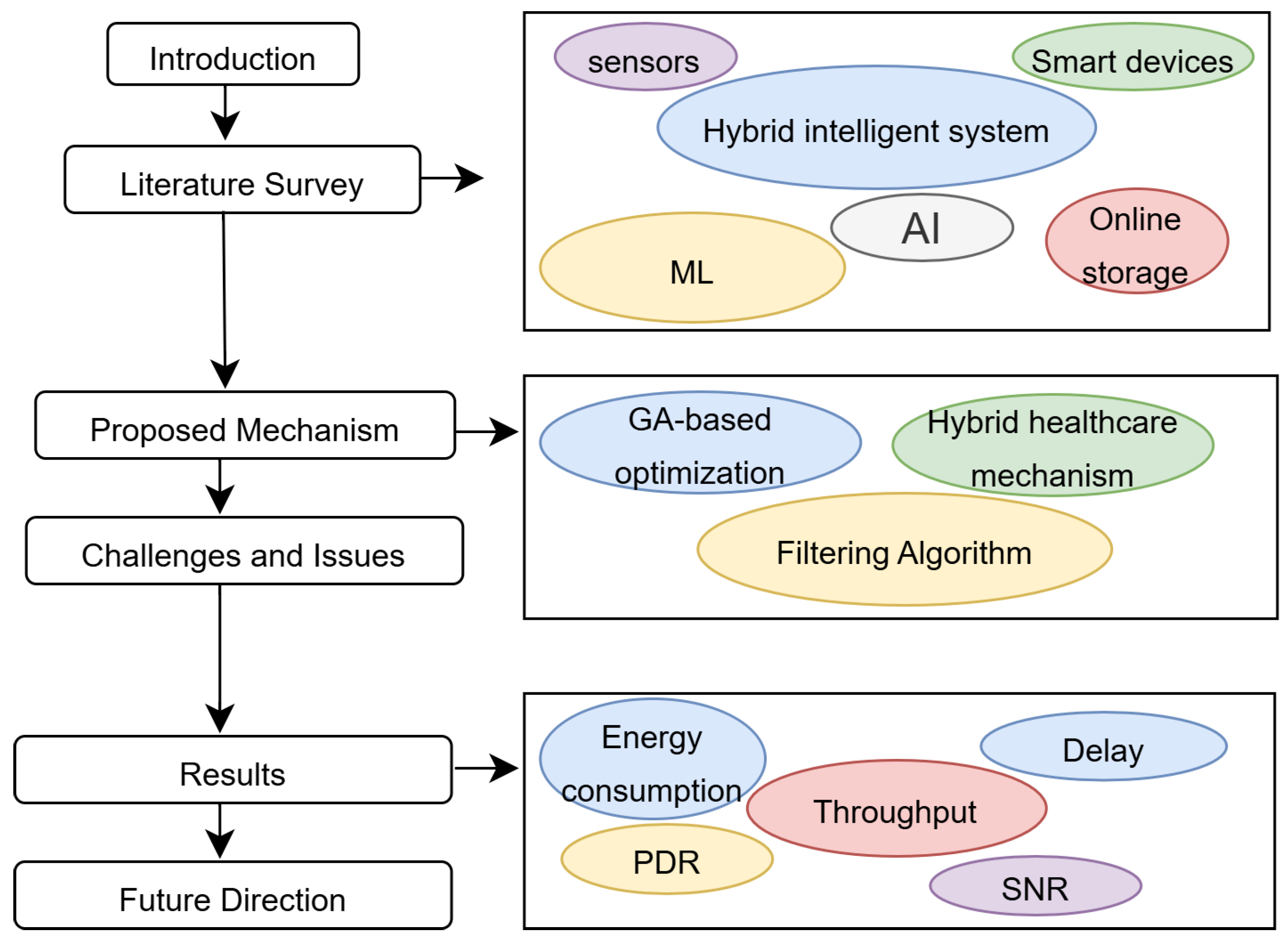
The proposed mechanism integrates an efficient communication and storage framework for medical records by combining a Genetic Algorithm (GA) with a Filtration Mechanism (FM) [
12,
13]. The GA is employed to optimize dynamic parameter generation and to select efficient routing paths, whereas the FM is used to reduce noise and communication delay, thereby enabling smoother information transmission in the network . The general flow of the proposed framework is illustrated in
Figure 1. The main contributions of this work are summarized as follows:
A GA-based optimization module is designed to enhance the information analysis process by filtering out less significant parameters based on their behavior and contribution to the network.
A filtration mechanism is incorporated to improve communication efficiency by reducing noise and communication delay, while simultaneously analyzing the legitimacy and behavior of each communicating device.
The proposed mechanism is extensively evaluated against several performance metrics, including packet delivery ratio, Quality of Service (QoS), throughput, Signal-to-Noise Ratio (SNR), energy consumption, and communication delay.
The remainder of this paper is organized as follows. Section 2 reviews existing schemes for efficient information transmission and storage in smart healthcare environments. Section 3 details the proposed methodology, including pseudo-code and the corresponding flowchart. Section 4 presents the validation and verification of the proposed mechanism against several performance metrics, in comparison with baseline methods. Finally, Section 5 concludes the paper and outlines potential directions for future work.
2. Related Work
This section reviews existing schemes and approaches for efficient and secure healthcare monitoring and patient record management proposed by various researchers.
Ezz et al. [
16] proposed a transparent and secure information transmission framework that integrates smart contracts with zero-knowledge proofs. The authors focused on promoting ethical AI in healthcare by governing information flows within the network, and validated their scheme in terms of patient privacy and data security. Su et al. [
17] introduced a high-fidelity radar dataset designed to preserve patient privacy during data sharing and storage. Their work explicitly incorporates occlusion scenarios to study and mitigate data leakage, thereby improving the applicability of radar-based sensing in real-world healthcare environments. The authors further monitored personal identity and behavioral patterns of patients in critical care rooms. Aravena et al. [
18] proposed a surgical prioritization framework that combines reinforcement learning with digital twins, demonstrating substantial improvements over traditional scheduling strategies. Their results indicate reduced waiting time, lower surgical risk, and improved utilization of healthcare resources.
Pradhan et al. [
19] presented an AI-assisted healthcare system leveraging 5G technology to enhance communication and information transmission in the network. They examined how AI and 5G can be jointly utilized in intelligent healthcare systems and showed improvements in average communication time as well as reductions in computational cost when adopting smart healthcare techniques. Alruwaili et al. [
20] integrated AI with transparent technologies such as blockchain and deep convolutional neural networks (CNNs) to enable a secure smart healthcare system. The authors investigated security risks associated with transmitting information over the network and evaluated the framework using benchmark medical datasets. They also highlighted the use of Jellyfish search optimization to address multiple optimization concerns. Akter et al. [
21] proposed a federated-learning-based privacy-preserving mechanism using edge intelligence for smart healthcare systems. They provided a theoretical convergence bound for federated learning and validated their approach on recent benchmark datasets such as STL-10, MNIST, CIFAR-10, and COVID-19 chest X-ray images.
Siddiqui et al. [
22] developed a Markov-process-based queuing model for smart healthcare mechanisms. Their approach aims to enhance overall quality of service in healthcare by improving patient care workflows and disease diagnosis processes, and they further assessed the use of blockchain systems in the context of smart healthcare. Mishra and Singh [
23] discussed the significance of integrating smart technologies for planning and managing medical care facilities to provide better patient care. They also outlined several challenges and opportunities in achieving higher standards associated with Healthcare 5.0. Patil et al. [
24] proposed a blockchain-based framework for preventing cyberattacks while managing medical records in smart healthcare systems. The authors evaluated their mechanism in terms of response time, demonstrating the effectiveness of Hyperledger-based smart contracts when compared with several existing approaches and mechanisms.
Table 1.
Summary of Related Work and Limitations.
Table 1.
Summary of Related Work and Limitations.
| Author Name |
Description |
Limitation |
| Ezz et al. [16] |
The authors have proposed a transparent and secure information transmission integrating smart contract and zero-knowledge proofs. |
The authors have targeted ethical AI in healthcare. |
| Su et al. [17] |
The authors have proposed a high-fidelity radar dataset for ensuring privacy of patients. |
The complexity and increased cost while ensuring the security in the network. |
| Aravena et al. [18] |
The authors have proposed a surgical prioritization scheme while integrating reinforcement learning and digital twins. |
The integration of AI and digital twins may enhance the storage overhead. |
| Pradhan et al. [19] |
The authors have proposed an AI-assisted healthcare system using 5G technology for improving the communication and transmission. |
There is a delay while transmitting the information in the network. |
| Alruwaili et al. [20] |
The authors have integrated the AI and transparent techniques such as blockchain and deep CNN. |
The block verification delays the communication process. |
| Akter et al. [21] |
The authors have generated a federated learning based privacy mechanism using edge intelligence for smart healthcare systems. |
The proposed mechanism enhanced the storage overhead in the network |
| Siddiqui et al. [22] |
The authors have proposed a Markov process model using a queuing system for smart healthcare mechanisms. |
The communication process may further delay the transmission process. |
| Mishra and Singh [23] |
The authors have discussed the significance of integrating smart technology for managing and planning |
The integration of processes enhances the complexity and cost of communication |
| Patil et al. [24] |
The authors have proposed a blockchain-based framework for preventing cyberattacks while managing the records |
The block verification delay further increase the communication delay in the network. |
2.1. Problem Statement
The number of efficient and effective smart healthcare approaches while ensuring the secure transmission of information along with data storage and transmission is proposed by several existing researchers/scientists. Though several schemes have been proposed focusing on integrating intelligent and smart healthcare schemes in traditional data analysis and diagnosis of medical records. It is further needed to propose an efficient way of processing and analysis of records in the healthcare systems.
3. Proposed Approach
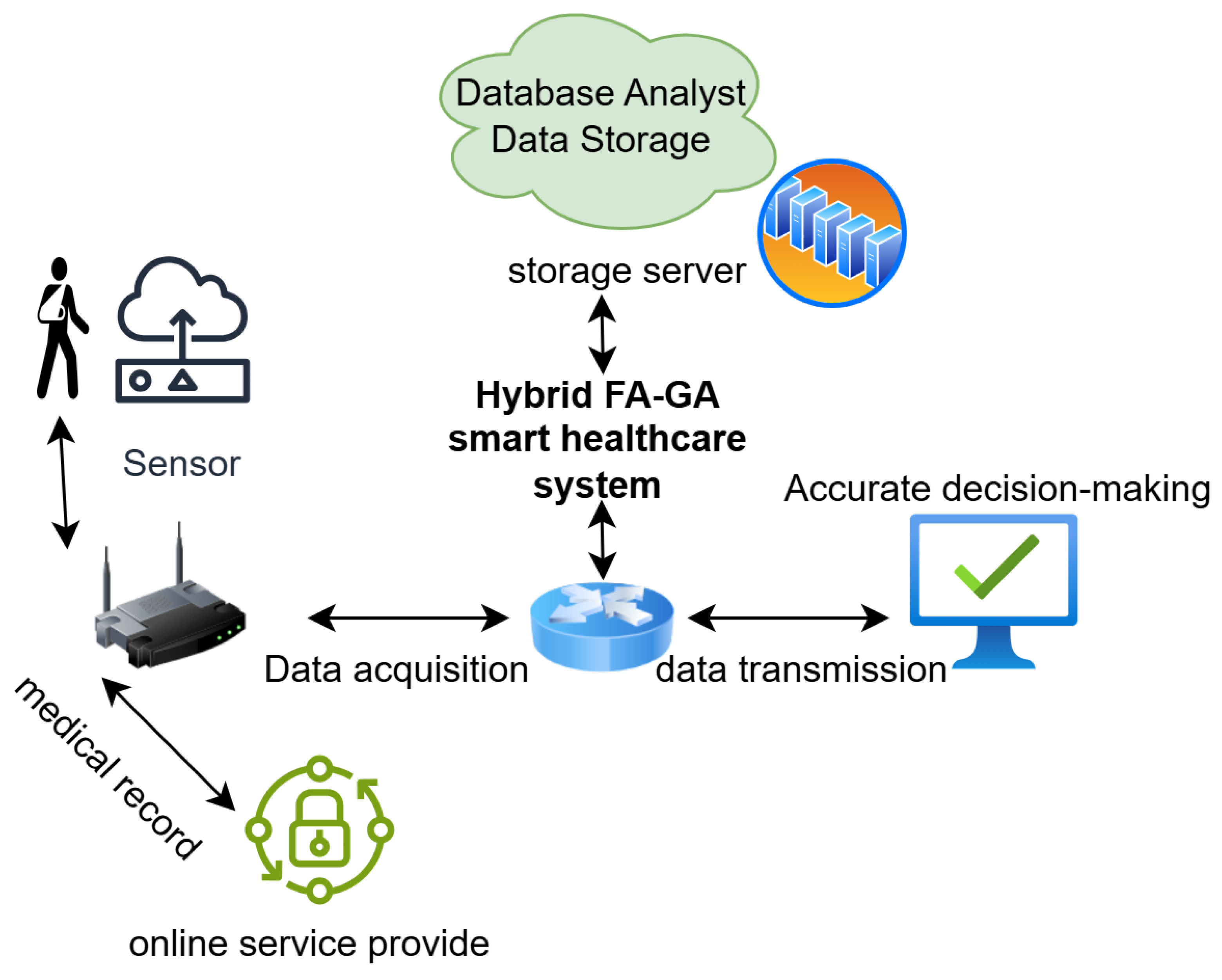
The aim of this manuscript is to propose an efficient and effective smart healthcare mechanism integrating a genetic algorithm for optimizing the dynamic optimization and filtering algorithm for noise reduction. As intelligent devices generates tons of information in every hour, it is further necessary to filter the significant information from the received data for providing an efficient transmission of information. Genetic algorithm is used to filter or select the routing parameters for filtering out the transmission power and energy consumption of each communicating device. In addition, filtration mechanism adapt the wireless fluctuating conditions along with reducing the noise distortion and communication delay.
3.1. System Workflow
Figure 2 presents the workflow of the proposed mechanism integrating FA and GA consisting of several components for smooth data transmission and communication for smart healthcare network.
Data Collection and Acquisition: The information is collected from the sensors that are placed in patient room by collecting the signals such as BP, glucose, ECG, movement of patient, temperature of room etc.
Data Pre-processing: The raw information collected from the sensors is passed through LMS filter in order to remove the noise ad motion artifacts in order to eliminate the interference.
GA optimization: The GA selects the optimal routing path by measuring the transmission power, nature, behavior, channel allocation and minimum delay required to process the record.
Integrated FA and GA: The GA process only those records received from the FA after noise reduction and less communication delay devices/sensors in order to optimize the communication process after each epoch.
Data transmission: The optimized record is further transmitted by the devices to their edge servers by performing real-time data analysis.
Looping: The network conditions are continuously recorded by updating the channel noise and filtration process of each record.
The LMS adaptation rule
for optimizing the information by reducing the noise is further processed as:
Where, is filter weight vector, is optimized route, is error signal and is input vector received from the sensors.
Further, GA function (F) is further computed as:
Where, D is delay, SNR is Singal-to-Noise Ration, E stands for energy and PLR stands for packet loss ratio.
The pseudo code of above integrated mechanism is further presents in Algorithm 1.
|
Algorithm 1:Integrated FA and GA for smart healthcare communication in the network |
-
Require:
Devices as , signals , GA parameters as , routing path, Transmission power and fitness weights
-
Ensure:
Efficient and cleaned signal of information to the edge - 1:
Deploy the FA with default weights as
- 2:
The GA initialized the population - 3:
for all device in Population size - 4:
Generate chromosome as routing, ,
- 5:
Estimate the fitness as
- 6:
Apply the GA by choosing the probability of mutation, crossover, repair by evaluating the F(child) - 7:
Select the best chromosome for final population |
The GA distribution of output along with filtration mechanism adaption is further presented in Algorithm 2.
|
Algorithm 2:Distribution and Adaptation of GA and LMS outputs |
-
Require:
Devices as , signals , GA parameters as , routing path, Transmission power and fitness weights
-
Ensure:
an Efficient and clean signal of information to the edge - 1:
-
Devices send the best chromosome by selecting the optimal routing path to IoMT device as:
Where, RT is the routing table, Tx is the transmission time, is weight and filtered device
- 2:
Filtration process further adopts the sample paths running on each device d as:
- 3:
Further error rate is defined as:
- 4:
Filtration adaptation rule is further applied as:
|
4. Performance Analysis
The proposed is further validated against the existing baseline approaches over GA and FM approaches. While performing the implementation, the chromosomes are represented as a mixture of integer genes as routing path, channel ID, transmission power, and initial weights. The fitness estimation is further computed as speed, an analytical estimator using path statistics and probe packet generation. Further, constraints are handled as a penalty function for infeasible chromosomes exceeding the power budget. For validating the proposed approach, the population size is considered as 30-100 devices, generation are defined as GenMax between 50-200, crossover rate is considered between , filtration length is defined between .
4.1. Baseline Approaches
The proposed mechanism is validated against several performance-based metrics such as packet delivery ration, Quality of Service (QoS), throughput, Signal to Noise Ration (SNR) , energy consumption, and communication delay against two considered existing approaches as EA1 and EA2. Alruwaili et al. [
20] have integrated the AI and transparent techniques such as blockchain and deep CNN while enabling a smart healthcare system that is considered as EA1. The authors have examined the security risks while communicating the information over network along with executing the benchmark medical datasets. The authors have further highlighted the Jellyfish search optimization by measuring several concerns. Whereas Mishra and Singh [
23] considered as EA2 have discussed the significance of integrating smart technology for managing and planning the medical care facilities for enhancing the better care of patients. The authors have further discussed several challenges along with achieving the higher standards of healthcare 5.0. Both are approaches are further considered in comparison of PA validation and verification over several parameters.
4.2. Evaluating Metrics
The performance metrics are further considered as discussed below for simulation and experimentation of proposed and existing approaches.
End-to-End Delay: it is defined as the average latency time required per successfully receiving of packets by the device.
Where, and are defined as receiving and sending of information i in the network and is defined as the number of successful receiving of packets.
Packet Delivery Ratio: It is defined as the ratio of number of packets received versus number of packets sent by the device d.
Throughput: It is defined as the useful data successfully received by the device d per unit of time.
Where stands for observation time.
Energy Consumption: It is defined as the amount of energy required to transmit information from one device to another.
4.3. Results and Discussion
This section presents the graphs generated over several discussed parameters in comparison of existing and proposed approaches.
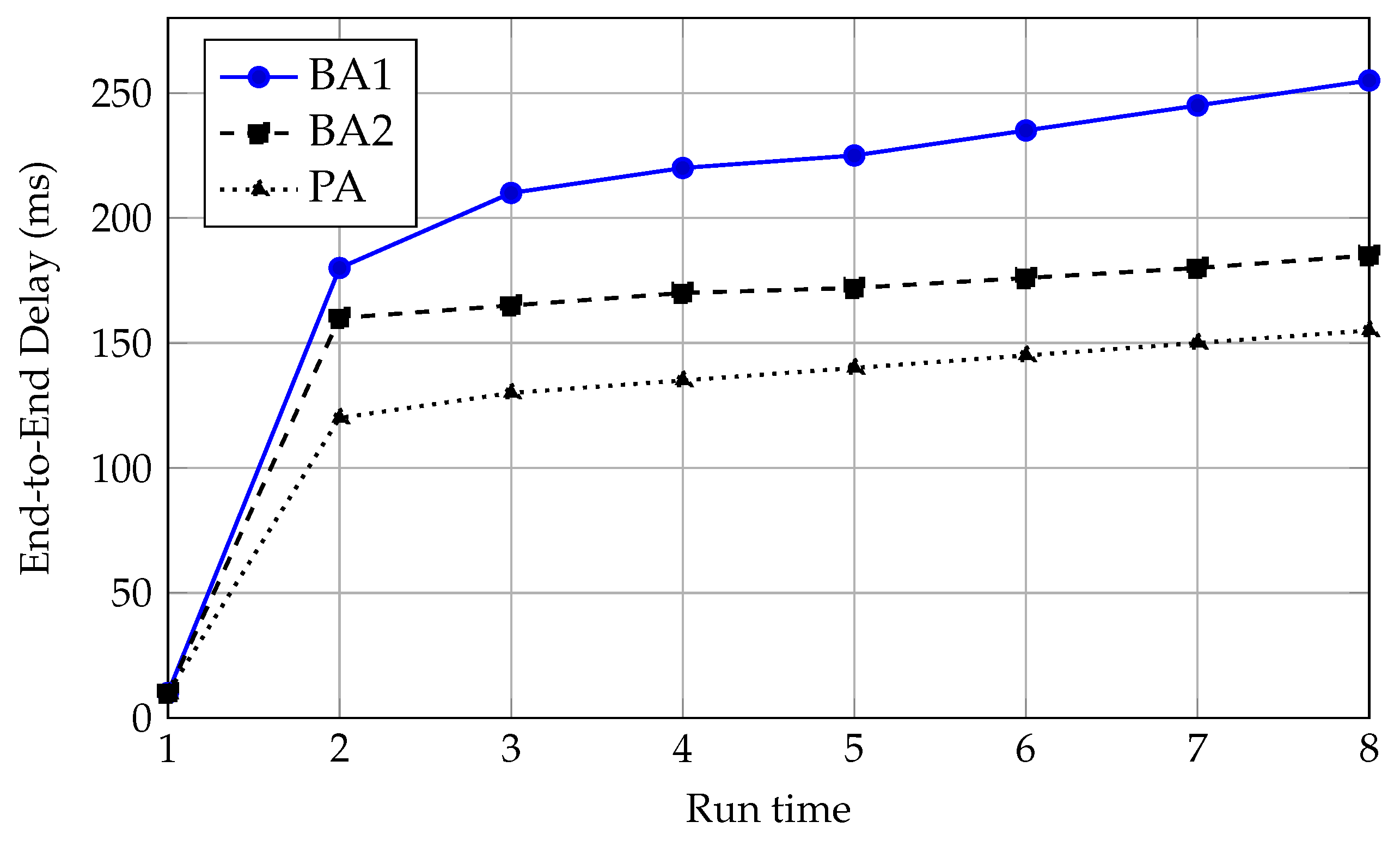
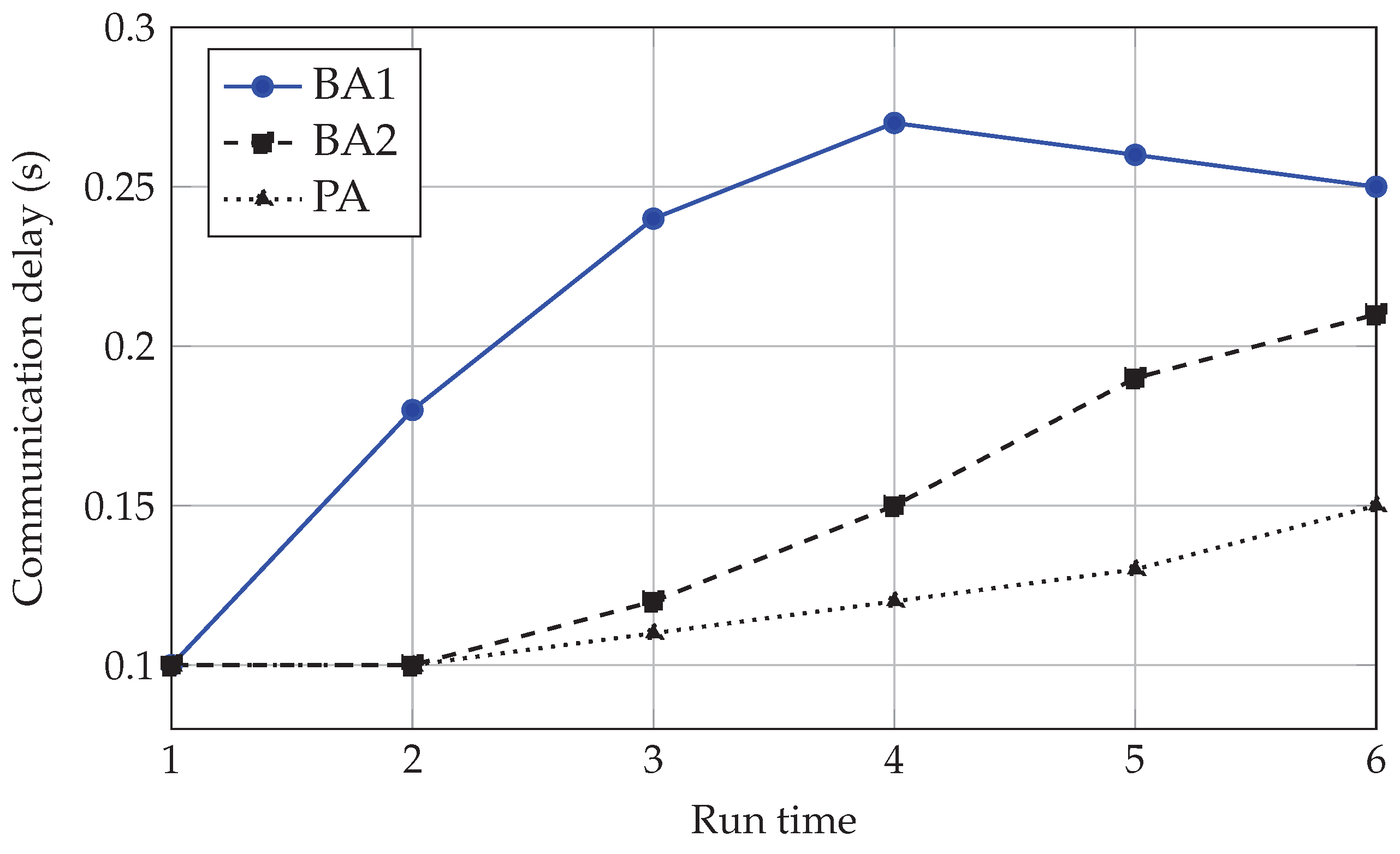
Figure 3 presents the end-to-end delay graph means the amount of time required to receive the packet by a device d in the network. The delay in the case of the proposed mechanism is very less compared to existing approaches, as the proposed mechanism reduces the noise and also filters the unnecessary parameters required to analyse the behaviour of a communicating device in the network.
Figure 3.
End-to-end delay versus run time for baseline approaches (BA1, BA2) and proposed approach (PA).
Figure 3.
End-to-end delay versus run time for baseline approaches (BA1, BA2) and proposed approach (PA).
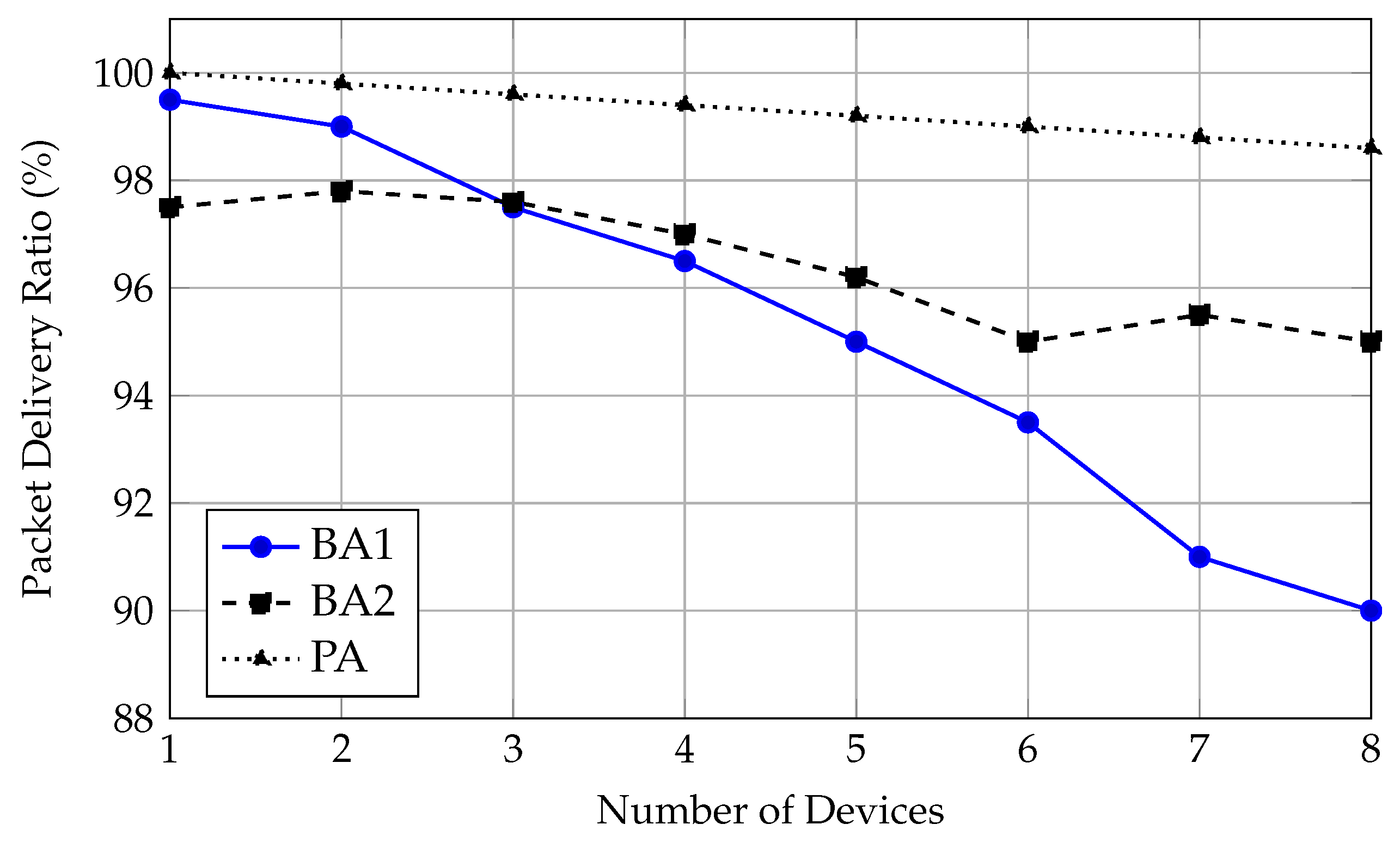
Figure 4.
Packet delivery ratio versus number of devices for baseline approaches (BA1, BA2) and the proposed approach (PA).
Figure 4.
Packet delivery ratio versus number of devices for baseline approaches (BA1, BA2) and the proposed approach (PA).
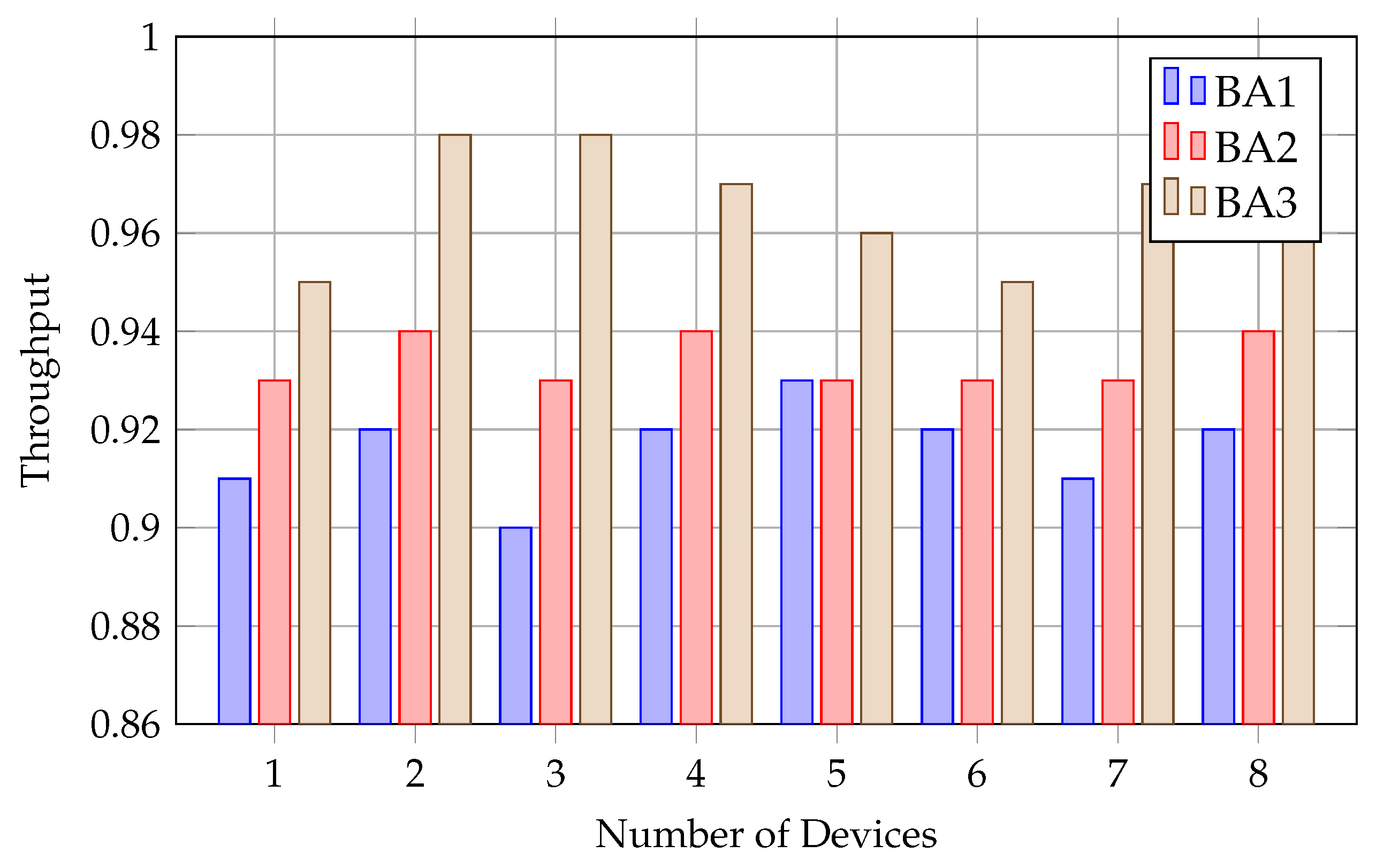
Figure 5 presents the throughput. The proposed mechanism outperforms the existing approaches because of filtering out the noise and unnecessary parameters while transmitting and sending of records in the network. The optimal selection of parameters further selects the best suited path for transmission of packets in the network.
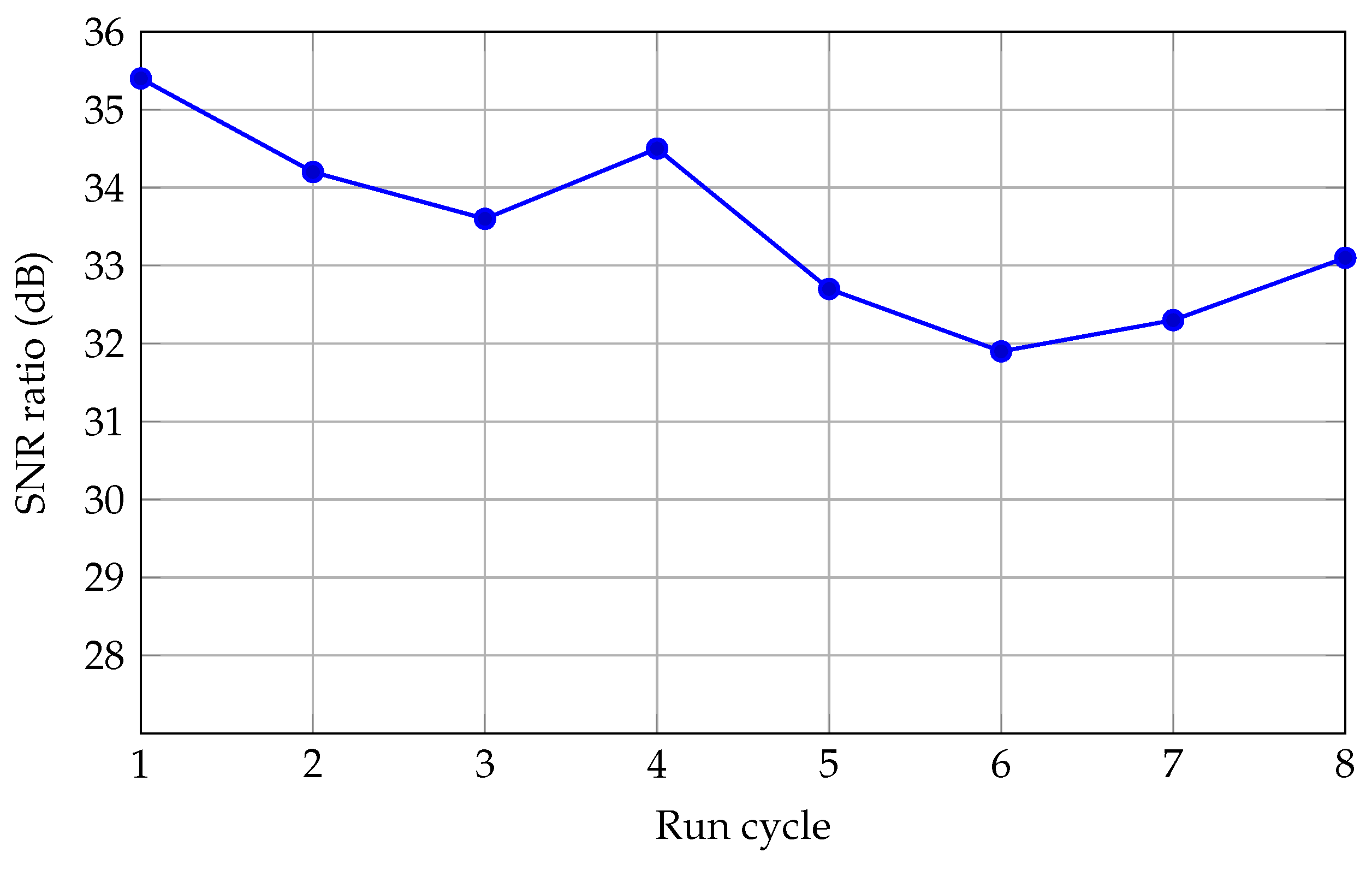
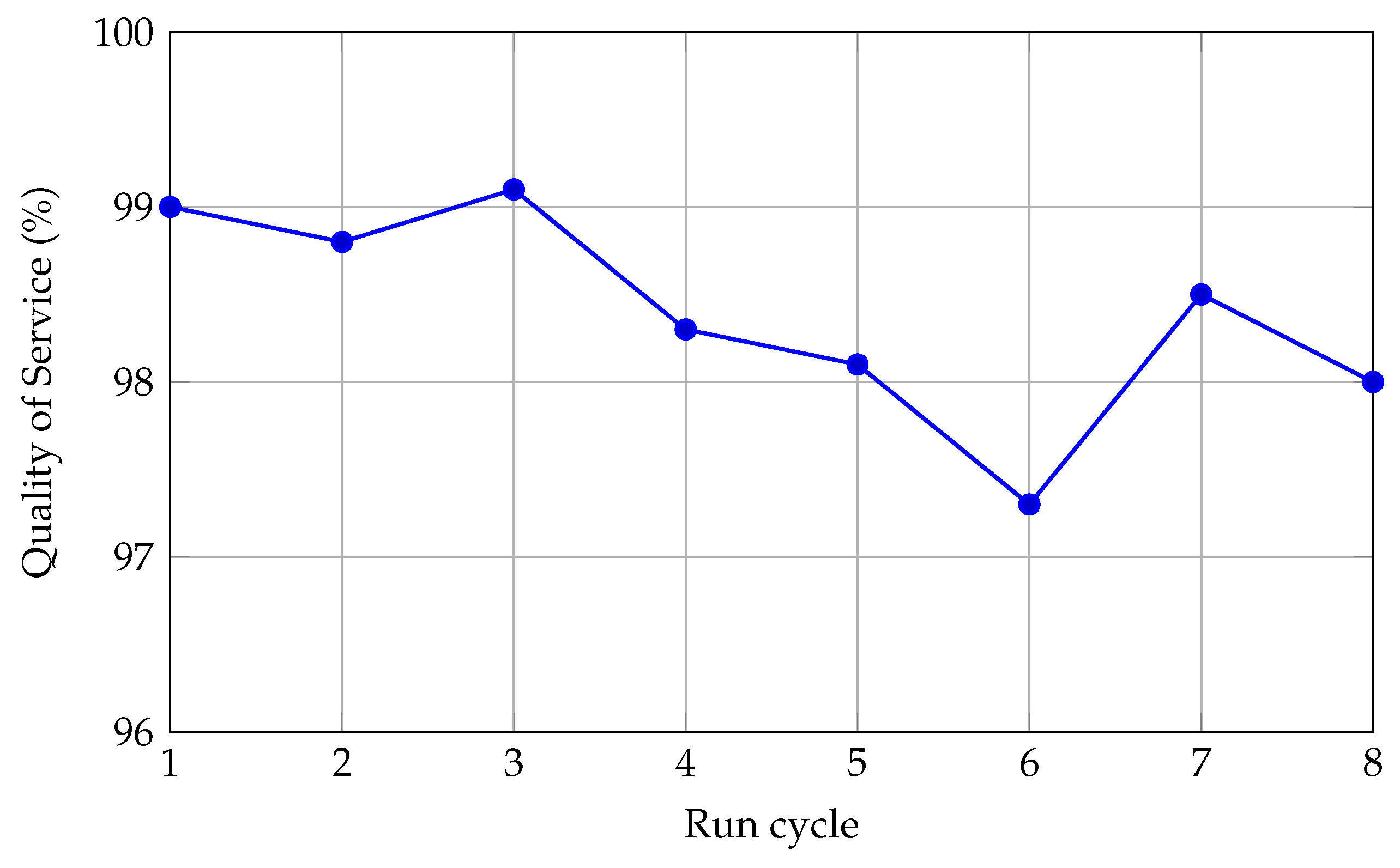
Further,
Figure 7 and
Figure 6 present the QoS and SNR of the proposed mechanism over 10 run cycles, showing the continuous improvement in quality while sending the records and noise reduction because of the involvement of the filtration mechanism.
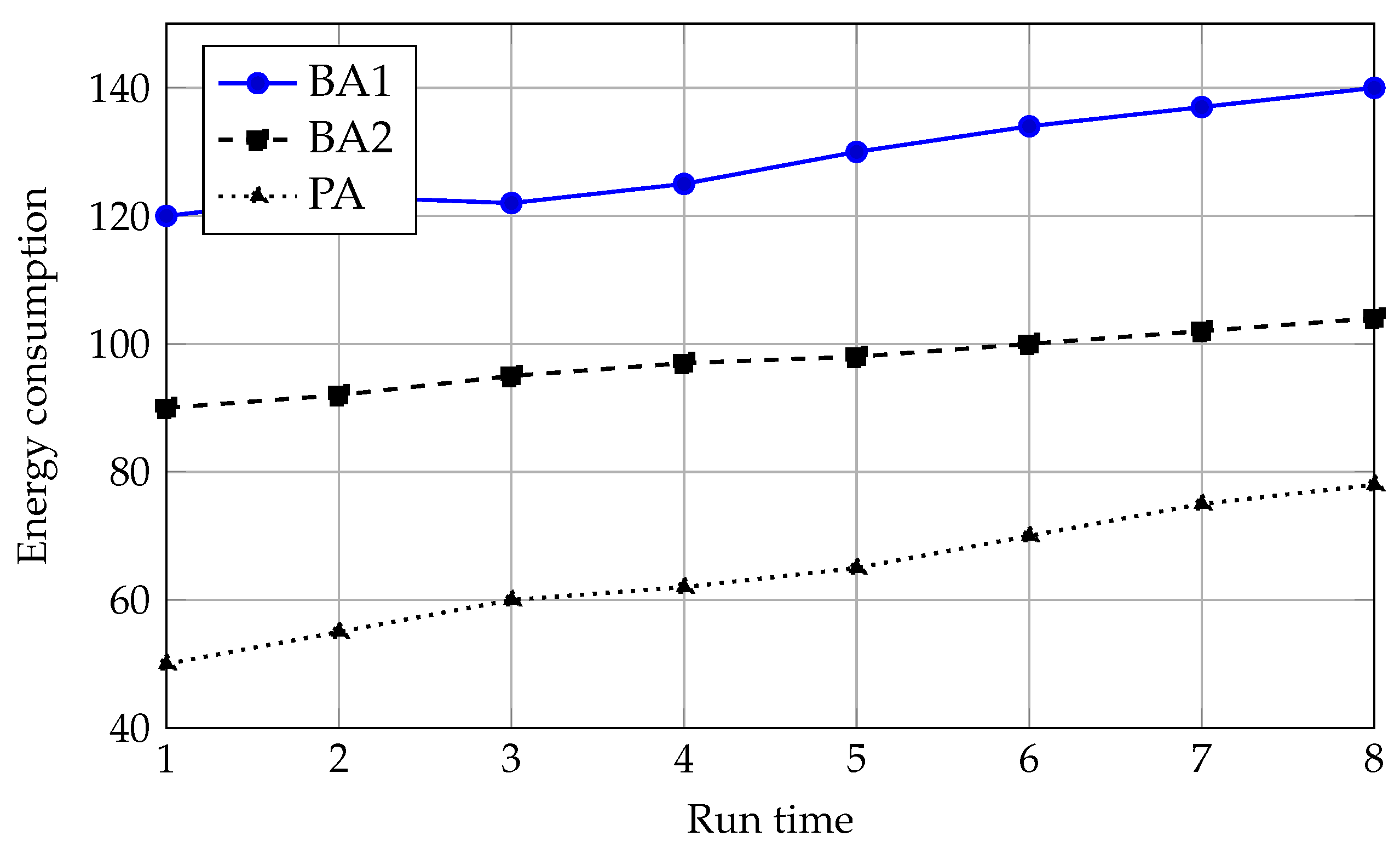
Furthermore,
Figure 8 presents the energy consumption of the proposed mechanism in comparison of existing approaches. The integration of FA and GA an efficient and smooth transmission of information while collecting the raw data from intelligent devices.
In addition,
Figure 9 presents the communication delay while transmitting the information among devices. The involvement of ideal behavioral devices in the network provides less communication delay compared to devices that can’t be analyzed at the initial stage.
4.4. Summary
The integration of GA and FA enhanced the communication efficiency in the smart healthcare system by optimizing the routing paths, network conditions, transmission power and reduced noise while transmitting the information in the network. The hybrid proposal ensures the less-delay, efficient throughput, SNR ratio, energy consumption and better packet delivery ratio in comparison of conventional approaches. The proposed mechanism offer an intelligent and robust communication framework while collecting the raw information of the patient by continuous monitoring, recourse constraint and emergency alerts.
5. Robustness and Sensitivity Analysis
In this section, we investigate the robustness of the proposed GA and two-level filtering framework with respect to key algorithmic and network parameters. Specifically, we study the sensitivity of the main performance indicators (end-to-end delay, packet delivery ratio, throughput, SNR, and energy consumption) to the GA hyperparameters, the LMS filter configuration, and the network size.
5.1. Sensitivity to GA Hyperparameters
The GA configuration strongly influences convergence speed and the quality of the selected routing solutions. We varied the population size between 30 and 100 individuals and the maximum number of generations, GenMax, between 50 and 200, while keeping the crossover and mutation rates within the ranges used in
Section 4. The results show that, although the absolute values of delay and energy consumption slightly change with the GA configuration, the proposed framework consistently outperforms EA1 and EA2 in all tested settings. This indicates that the performance gains are not limited to a narrow hyperparameter configuration but are robust to reasonable changes in the GA setup.
5.2. Effect of LMS Filter Parameters
To analyze the impact of the filtration stage, we varied the LMS filter length between 8, 16, and 32 taps and adjusted the step size within a stable range. Increasing the filter length leads to improved SNR and QoS at the cost of a modest increase in computational complexity per sensor node. Importantly, even with the smallest filter length, the two-level filtration scheme significantly improves the PDR and reduces the end-to-end delay compared to the baseline approaches, confirming that the filtration stage is a key contributor to the observed performance improvements.
5.3. Scalability with Network Size
Finally, we examined the scalability of the proposed mechanism by increasing the number of IoMT devices from 50 to 150 under higher traffic loads. While all schemes experience an increase in delay and a slight degradation in PDR as the network becomes denser, the GA and filtration-based framework exhibits a slower performance degradation than EA1 and EA2. This behavior can be attributed to the adaptive selection of routing paths based on delay, SNR, energy, and packet loss ratio. These findings demonstrate that the proposed system can support larger smart healthcare deployments while maintaining acceptable QoS levels.
6. Conclusions
This work presented an automated smart healthcare communication mechanism that combines a two-level filtering scheme with a multi-objective Genetic Algorithm to address key challenges in IoMT-based healthcare networks, namely noisy physiological signals, constrained energy resources and stringent latency requirements. At the sensing layer, an adaptive LMS-based filtration mechanism was employed to mitigate channel noise and motion artefacts, thereby improving the quality of physiological signals before transmission. At the network layer, the GA was used to optimize routing paths and transmission parameters by simultaneously considering delay, SNR, energy consumption and packet loss, resulting in more reliable and resource-aware data delivery.
The integrated framework was validated through simulation and compared against two state-of-the-art smart healthcare approaches. The proposed mechanism consistently achieved lower end-to-end delay and communication latency, higher packet delivery ratio and throughput, improved SNR and QoS, and reduced energy consumption. These improvements stem from the joint effect of denoising at the signal level and selective, GA-driven routing at the network level, which together ensure that legitimate, high-quality medical records are transmitted through the most suitable paths.
From a practical perspective, the proposed system can support continuous patient monitoring, early detection of anomalies and prioritization of high-risk cases in smart healthcare environments, particularly where many heterogeneous devices generate large volumes of data. By reducing false alarms and communication overhead, the framework has the potential to improve responsiveness and reliability in clinical decision-making.
Future work will focus on extending the proposed framework with end-to-end security and privacy mechanisms, such as lightweight authentication, access control and privacy-preserving data sharing, to better protect sensitive medical records. In addition, validating the approach on real-world clinical datasets and deploying it on testbed IoMT platforms will be important to assess scalability, interoperability and robustness under realistic operating conditions, and to integrate the mechanism more tightly with existing healthcare information systems.
Author Contributions
Conceptualization, G.R.,H.S., C.A.K., R.D., M.C.G; Methodology, G.R.,H.S., C.A.K., R.D., M.C.G; Software, G.R.,H.S., R.D., M.C.G; Validation, G.R.,H.S., R.D., M.C.G; Formal Analysis, G.R.,H.S., C.A.K., R.D., M.C.G; Investigation, G.R.,H.S., C.A.K., R.D., M.C.G; Resources, G.R.,H.S., C.A.K., R.D., M.C.G; Data Curation, G.R.,H.S., C.A.K., R.D., M.C.G; Writing—Original Draft, G.R.,H.S., C.A.K., R.D., M.C.G; Writing—Review and Editing, G.R.,H.S., C.A.K., R.D., M.C.G; Visualization, G.R.,H.S., C.A.K., R.D., M.C.G; Supervision, G.R.,H.S., C.A.K., R.D., M.C.G; Project Administration, G.R.,H.S., C.A.K., R.D., M.C.G; Funding Acquisition, G.R., M.C.G
Funding
The Open Access (OA) fee for this paper was funded by the University of Liverpool.
Institutional Review Board Statement
This research was deemed not to require the University’s Ethical Committee approval, as it does not fall under any of the cases requiring ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mazhar, T.; Irfan, H. M.; Haq, I.; Ullah, I.; Ashraf, M.; Shloul, T. A.; Elkamchouchi, D. H. Analysis of challenges and solutions of IoT in smart grids using AI and machine learning techniques: A review. Electronics 2023, 12(1), 242. [Google Scholar] [CrossRef]
- Mondal, R. S.; Akter, L.; Bhuiyan, M. N. A. Integrating AI and ML techniques in modern microbiology. Applied IT & Engineering 2025, 3(1), 1–10. [Google Scholar] [CrossRef]
- Shaheen, M. Y. Applications of Artificial Intelligence (AI) in healthcare: A review. In ScienceOpen Preprints; 2021. [Google Scholar]
- Valavanidis, A. Artificial intelligence (ai) applications; Department of Chemistry, National and Kapodistrian University of Athens: University Campus Zografou, 15784, 2023. [Google Scholar]
- Konya, A.; Nematzadeh, P. Recent applications of AI to environmental disciplines: A review. Science of The Total Environment 2024, 906, 167705. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Liu, J.; Evans, R.; Song, Y.; Ma, J. Factors influencing the adoption of health information standards in health care organizations: a systematic review based on best fit framework synthesis. JMIR medical informatics 2020, 8(5), e17334. [Google Scholar] [CrossRef]
- Ghanem, M.C.; Salloum, S. Integrating AI-driven deep learning for energy-efficient smart buildings in Internet of Thing-based Industry 4.0. Babylonian Journal of Internet of Things 2025, 2025(7), 121–130. [Google Scholar] [CrossRef]
- Farzaan, M.A.; Ghanem, M.C.; El-Hajjar, A.; Ratnayake, D.N. AI-powered system for an efficient and effective cyber incidents detection and response in cloud environments. IEEE Transactions on Machine Learning in Communications and Networking, 2025. [Google Scholar]
- Ghanem, M.C.; Almeida Palmieri, E.; Sowinski-Mydlarz, W.; Al-Sudani, S.; Dunsin, D. Weaponized iot: a comprehensive comparative forensic analysis of hacker raspberry pi and pc kali linux machine. IoT 2025, 6(1), 18. [Google Scholar] [CrossRef]
- Khanijahani, A.; Iezadi, S.; Dudley, S.; Goettler, M.; Kroetsch, P.; Wise, J. Organizational, professional, and patient characteristics associated with artificial intelligence adoption in healthcare: A systematic review. Health Policy and Technology 2022, 11(1), 100602. [Google Scholar] [CrossRef]
- Vadisetty, R.; Polamarasetti, A. 9 AI/Decision ML-Driven Support Clinical and Medical Imagining; Technologies, Practices, and Management: Sustainable Healthcare Systems in Africa, 2025; p. 154. [Google Scholar]
- Sivaprasad Yerneni, K.; Ravi Teja, A.; Sri Harsha, K.; Naresh Kiran Kumar Reddy, Y. Towards Proactive Cloud Security: A Survey on ML and Deep Learning-Based Intrusion Detection Systems. J Contemp Edu Theo Artific Intel 2025, JCETAI–116. [Google Scholar]
- Prasad, T.V.K.P.; Sujatha, G.; Satish, T.; Rao, N.B. Protection of Sensitive Information Utilizing AutoML and Merkel Tree based on AONT-EHR. In Algorithms in Advanced Artificial Intelligence; CRC Press, 2025; pp. 23–29. [Google Scholar]
- Sharma, S.; Kumar, V. Application of genetic algorithms in healthcare: a review. In Next generation healthcare informatics; 2022; pp. 75–86. [Google Scholar]
- Mirza, S.S.; Ur Rahman, M.Z. Efficient adaptive filtering techniques for thoracic electrical bio-impedance analysis in health care systems. Journal of Medical Imaging and Health Informatics 2017, 7(6), 1126–1138. [Google Scholar] [CrossRef]
- Ezz, M.; Alaerjan, A.S.; Mostafa, A.M. Ethical AI in Healthcare: Integrating Zero-Knowledge Proofs and Smart Contracts for Transparent Data Governance. Bioengineering 2025, 12(11), 1236. [Google Scholar] [CrossRef]
- Su, Y.; Hou, H.; Lan, H.; Ma, C.Z.H. A High-Fidelity mmWave Radar Dataset for Privacy-Sensitive Human Pose Estimation. Bioengineering 2025, 12(8), 891. [Google Scholar] [CrossRef]
- Silva-Aravena, F.; Morales, J.; Jayabalan, M. e-Health strategy for surgical prioritization: a methodology based on Digital Twins and reinforcement learning. Bioengineering 2025, 12(6), 605. [Google Scholar] [CrossRef]
- Pradhan, B.; Das, S.; Roy, D.S.; Routray, S.; Benedetto, F.; Jhaveri, R.H. An AI-assisted smart healthcare system using 5G communication. IEEE Access 2023, 11, 108339–108355. [Google Scholar] [CrossRef]
- Alruwaili, F. F.; Alabduallah, B.; Alqahtani, H.; Salama, A. S.; Mohammed, G. P.; Alneil, A. A. Blockchain enabled smart healthcare system using jellyfish search optimization with dual-pathway deep convolutional neural network. IEEE Access 2023, 11, 87583–87591. [Google Scholar] [CrossRef]
- Akter, M.; Moustafa, N.; Lynar, T.; Razzak, I. Edge intelligence: Federated learning-based privacy protection framework for smart healthcare systems. IEEE Journal of Biomedical and Health Informatics 2022, 26(12), 5805–5816. [Google Scholar] [CrossRef]
- Siddiqui, S.; Fatima, S.; Ali, A.; Gupta, S. K.; Singh, H. K.; Kim, S. Modelling of queuing systems using blockchain based on Markov process for smart healthcare systems. Scientific Reports 2025, 15(1), 17248. [Google Scholar] [CrossRef]
- Mishra, P.; Singh, G. Healthcare 5.0: Smart and Connected Healthcare Systems for Sustainable Smart Cities. In Sustainable Smart Cities 2.0: Enabling Research Toward SDG 11; Springer Nature Switzerland: Cham, 2025; pp. 251–289. [Google Scholar]
- Patil, S. M.; Dakhare, B. S.; Satre, S. M.; Pawar, S. D. Blockchain-based privacy preservation framework for preventing cyberattacks in smart healthcare big data management systems. Multimedia Tools and Applications 2025, 84(22), 25547–25566. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).