1. Introduction
Coronary artery bypass grafting (CABG) is the first-line therapy for multivessel coronary artery disease (CAD), especially in complex disease [
1,
2]. Therefore, CABG is the most commonly performed cardiac surgery procedure [
3]. Over the last decades, life expectancy in the Western world has increased significantly, and the number of octogenarians presenting with a multivessel CAD requiring treatment is on the rise [
4]. Older patients, especially those over 80 years of age, pose a particular surgical challenge. They are more likely to have comorbidities such as prior myocardial infarction, prior stroke, atrial fibrillation, heart failure, diabetes mellitus, hypertension or kidney failure, often summarized under the term frailty [
5,
6]. In patients over 80 years of age, the in-hospital mortality rate is increased and major adverse cardiac and cerebrovascular events (MACCE) occur more frequently with conservative as well as interventional and surgical treatment. Additionally, other underlying diseases can complicate the treatment of coronary heart disease [
7,
8,
9].
In 2019, a new surgical approach for complete coronary revascularization in patients with multivessel CAD via a left anterior minithoracotomy (TCRAT) was proposed and introduced [
10]. Since then, the technique has been further developed [
11] towards a standard method for minimally invasive CABG that avoids sternotomy, utilizing established surgical techniques [
11,
12,
13]. Several studies have shown promising in-hospital and midterm outcomes in unselected patients [
12,
13,
14,
15,
16,
17] and equivalence in the rate of organ dysfunctions compared to contemporary standard CABG procedures using a full midline sternotomy [
18,
19]. The reduced surgical trauma by avoiding sternotomy, the facility of faster postoperative recovery without compromising the fundamental principles of complete coronary revascularization at the same time may be particularly beneficial for elderly patients with limited physiological reserves. In this context, this study aimed to evaluate in-hospital and midterm outcomes of TCRAT in patients older than 80 years by analyzing of clinical endpoints including major adverse cardiac and cerebrovascular events (MACCE).
2. Methods
2.1. Patient Selection and Data Collection
Between November 2019 and October 2025, a total of 859 consecutive patients underwent nonemergency isolated CABG via left anterior minithoracotomy on CPB with peripheral cannulation and cardioplegic cardiac arrest (transthoracic aortic cross-clamping) in our institution, using this technique as a default strategy in daily routine. Among them, 82 (9.5%) were octogenarians. The focus of the present study was to investigate the in-hospital and midterm outcomes of this specific subgroup. All patients were discussed in detail in the heart team [
20], including a recommendation according to guideline indications [
2] of which coronary arteries should be grafted. Anatomic complete revascularization was defined as the successful treatment of all significant coronary lesions with a visually estimated diameter stenosis 50% in vessels with reference vessel diameter of 1.5 mm [
2]. Patients younger than 80 years of age, patients undergoing emergency procedure (ie, same-day catheterization and operation), patients with significant atheromatous disease of the ascending aorta, patients with moderate or severe aortic regurgitation, and patients undergoing reoperation were excluded.
2.2. Statistical Analysis
Data were prospectively extracted from patient records and presented as mean ± standard deviation (SD) or number (percentage) and are part of our internal quality assurance documentation. The follow-up data were collected prospectively through telephone interviews, using a structured questionnaire by a study nurse, and acquisition and evaluation of medical findings. Kaplan-Meier graphs were calculated with SPSS version 29.0.0.0 (IBM-SPSS Inc.).
2.3. Definitions of Clinical Events
Perioperative stroke was characterized as a neurological deficit attributed to an acute focal injury of the central nervous system by a vascular cause, including cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage. This definition is in line with the updated definition of stroke for the 21st century from the American Heart Association and American Stroke Association [
21].
According to the Fourth Universal Definition of Myocardial Infarction of the Society for Cardiovascular Angiography and Interventions [
22], postoperative myocardial infarction was defined as an increase in creatine kinase-MB levels within 48 hours after the procedure up to 10 times the local laboratory upper limit of normal or to five times the upper limit of normal with newly occurring Q waves in 2 contiguous leads or a new persistent left bundle branch block.
MACCE were defined as a composite of all-cause-mortality, myocardial infarction, repeat revascularization, and stroke.
2.4. Preoperative Evaluation, Anesthesia and Surgical Technique
The preoperative evaluation, details of induction and implementation of anesthesia and the surgical technique of TCRAT has been described by our group in detail in several recently published studies [
11,
12,
13]. Therefore, the key points are only briefly outlined here.
A preoperative computed tomography (CT) scan, in addition to the standard institutional preoperative examinations, is crucial to screen the ascending aorta, the aortic arch, and major arterial branches, especially the iliac and femoral vessels and to detect anatomical abnormalities or atherosclerotic disease.
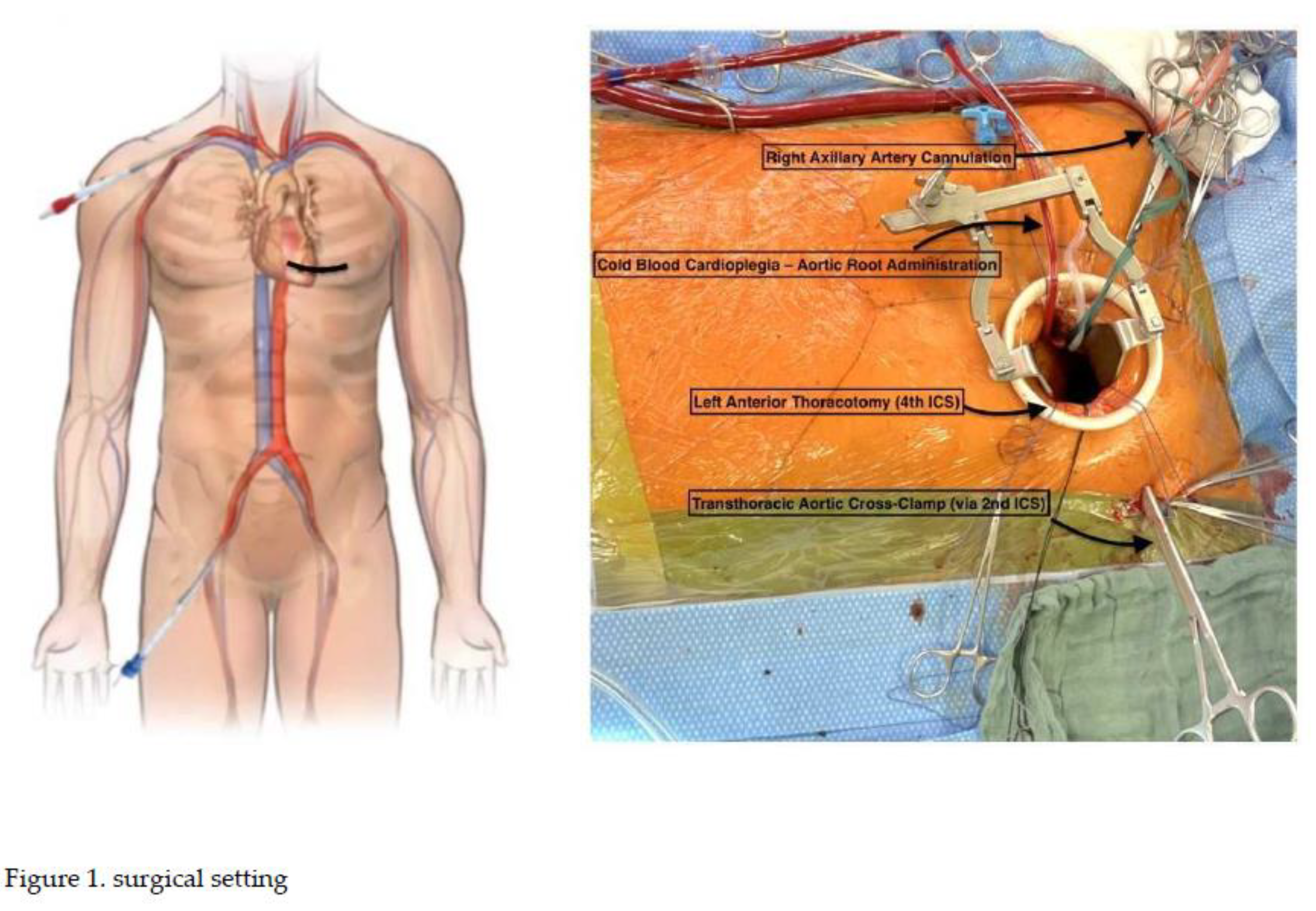
The surgical technique of TCRAT includes three key elements [
10]. First, TCRAT is a sternum-sparing surgical approach by using a left-sided, anterolateral minithoracotomy at the level of the 4th intercostal space. Second, TCRAT is an on-pump technique using a peripheral cannulation strategy. This enables stable circulatory conditions, decompression and intrathoracic rotation of the heart after transthoracic aortic cross-clamp, and induction of cardioplegic cardiac arrest (Figure 1). The third key element are strategic slinging maneuvers around the great intrapericardial vessels. This is a crucial prerequisite for access to all coronary territories and enables optimal conditions for coronary artery bypass grafting, thus enabling complete anatomical revascularization.
2.5. Ethical Standards
This study was approved by the local ethics committee (University of Marburg, file number: 23-172 RS) and conducted in accordance with the ethical standards outlined in the 1964 Declaration of Helsinki and its subsequent amendments. The patients provided informed written consent for the publication of the study data.
3. Results
The study group consisted of 82 consecutive, nonemergency octogenarians (66 men; age 82.7 ± 1.8 years [range 80–88 years]) including patients with severe left ventricular dysfunction (left ventricular ejection fraction [LVEF] ≤ 30: 8.5%), prior myocardial infarction (37.8%), and patients with an elevated European System for Cardiac Operative Risk Evaluation 2 score (EuroSCORE II) above 4 (53.7%). Mean EuroSCORE II was 5.1 ± 2.4. All patients had multivessel CAD, of those 41.5% having a relevant left main stem stenosis. Baseline and clinical parameters are given in
Table 1.
The left internal mammary artery (LIMA) was used in 98.8%, saphenous vein graft (SVG) in 69.5% and radial artery (RA) in 43.9%. 47.6% of all patients received at least 2 arterial grafts. On average, 3.0 distal anastomoses per patient were performed, with a minimum of 2 and a maximum of 5 distal anastomoses. Left anterior descending (LAD) was grafted in 100%, the left circumflex artery (LCX) was grafted in 88%, and the right coronary artery (RCA) was grafted in 72% of all patients. Complete anatomical revascularization was achieved in 96.3%. Mean operative time was 299 ± 64 minutes, mean CPB time was 142 ± 38 minutes, and mean aortic-cross clamp time was 88 ± 31 minutes. Operative characteristics are given in
Table 2.
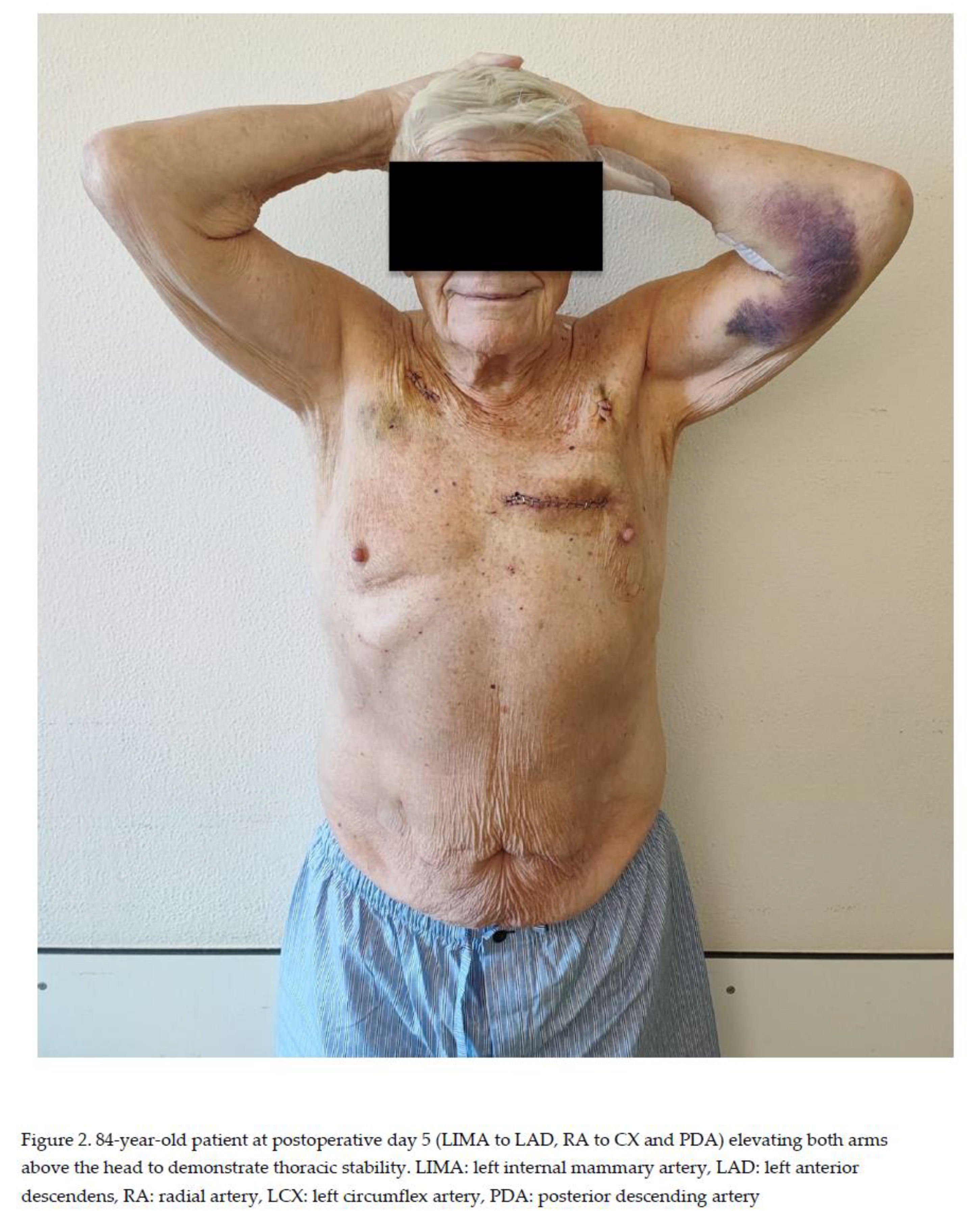
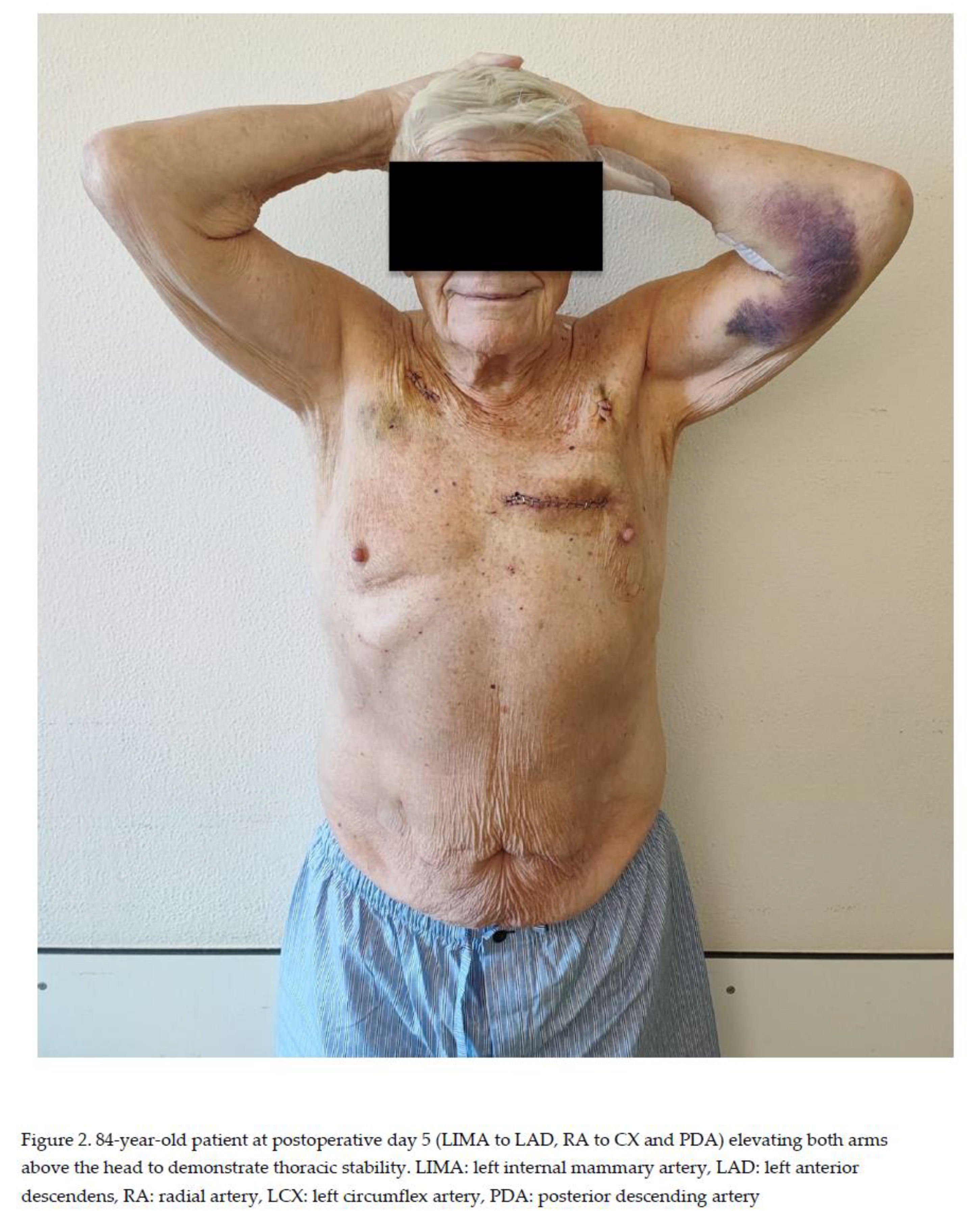
By avoiding a sternotomy, immediate mobilization was possible (Figure 2). 60% of patients left the intensive care unit (ICU) within the first postoperative day. The in-hospital mortality was 1.2%. The in-hospital rate of repeated coronary artery revascularization using percutaneous coronary intervention (PCI) was 1.2%, which was a planned postoperative PCI when the posterior descending artery of the right coronary artery could not be identified intraoperatively. One patient experienced a perioperative stroke (1.2%) with minor clinical impairment. Postoperative adverse events and outcome are given in
Table 3.
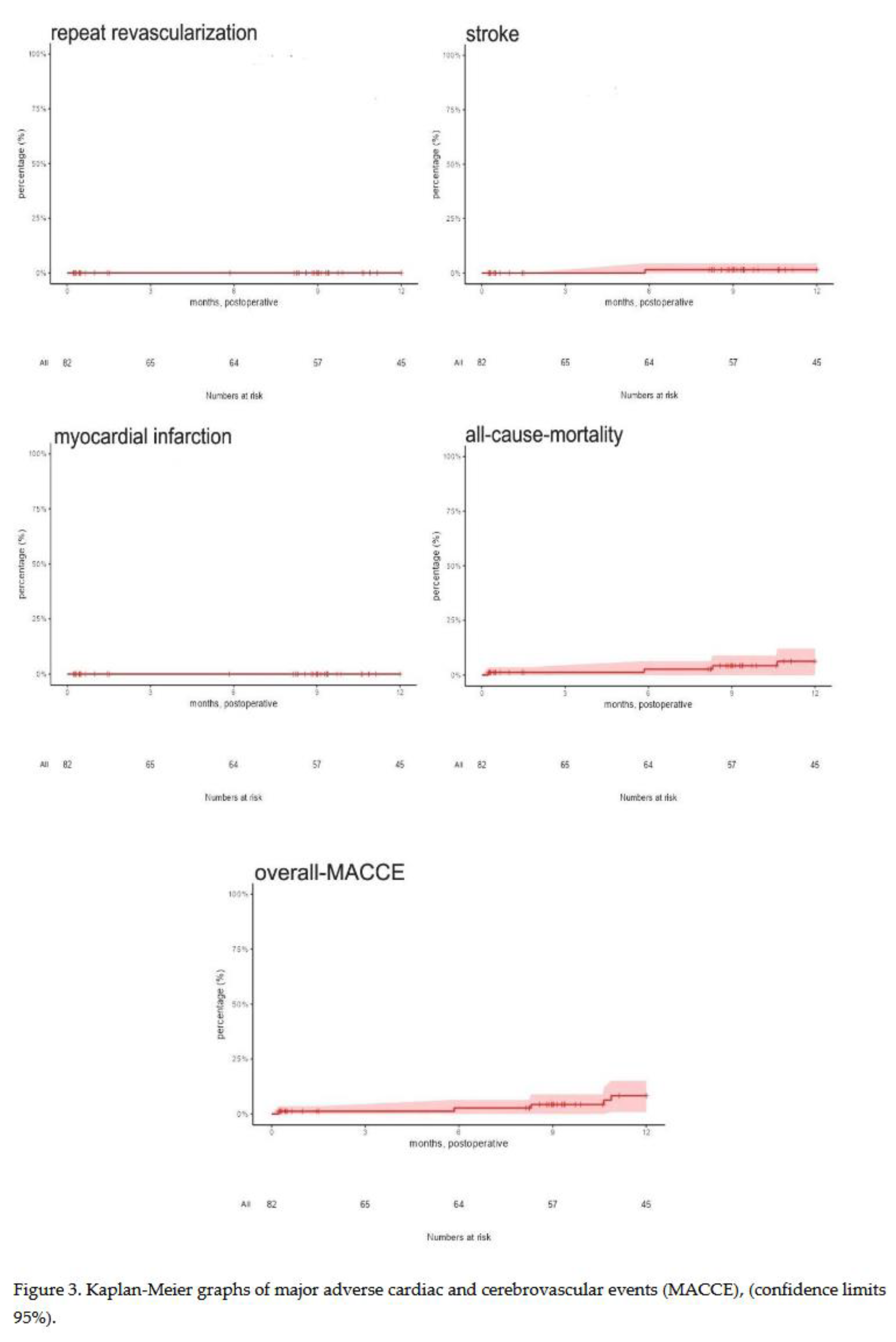
Mean follow-up was 9.1 ± 4.6 months (range 0.23-12.0 months) and was completed to 100%. Median of our follow-up was 12 months (interquartile range 3.7 months). During follow-up, all-cause-mortality was 4.9%, postoperative repeat revascularization was 2.4%, and postoperative stroke was found in 1.2%. No myocardial infarction was observed. Overall MACCE during the observed follow-up was 7.3%. Follow-up data are provided in
Table 4 and in Figure 3.
4. Discussion
This is the first study that investigated the in-hospital and midterm outcomes of octogenarians after minimally invasive multivessel CABG using the TCRAT technique. This patient group is rather underrepresented in many clinical studies, but due to demographic developments in the Western world, it represents a growing and increasingly important patient collective [
4,
7,
23,
24].
Compared to important landmark studies such as the Syntax (Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease) trial [
25], the FAME 3 (Fractional Flow Reserve versus Angiography for Multivessel Evaluation) trial [
26] and the first and so far only published study on in-hospital and midterm results using the TCRAT technique, the present study shows an increased operative risk in the group of octogenarians when analyzing baseline characteristics. This is reflected by a mean EuroSCORE II of 5.1 and a proportion of over 50% of patients with an EuroSCORE II greater than 4. A recently published meta-analysis of CABG and PCI in octogenarians with left main or multivessel CAD reported comparable baseline characteristics to our data [
24].
Substantial benefit from surgical compared to interventional coronary revascularization is most pronounced in patients with multivessel CAD, diabetes mellitus, and with reduced LVEF [
2]. Added to this, CABG patients often experience high comorbidity and surgical risk—this applies in particular to the group of octogenarians. In the present study, we included octogenarians with diffuse multivessel CAD requiring complex coronary surgery, with very low LVEF, obesity and chronic obstructive pulmonary disease and with high surgical risk.
All coronary arteries with a diameter exceeding 1.5 mm and a luminal reduction of 50% or more should be grafted [
2] to achieve a complete anatomical revascularization. According to this definition, a complete anatomical revascularization was accomplished in 96.3% in our study. The number of grafts performed in patients with multivessel CAD often is considered as an indirect parameter for the completeness of revascularization [
27]. The average number of grafts performed in the present study was 3.0, which compares well to the average number of 3.0 grafts reported for conventional CABG in the German Heart Surgery Report 2023 [
28] and is consistent with the data from the only study published to date on midterm results after minimally invasive CABG using the TCRAT technique in an all-comer population [
13]. According to recent revascularization guidelines [
2], we achieved a multi-arterial graft configuration in more than 47%, despite the advanced patient age.
In our study, the in-hospital mortality rate was 1.2%, which compares favorably with the mortality rate of 2.1% reported by several studies in current CABG patients overall and the reported 30-day mortality rate of 4% to 16.8% in the octogenarian group [
9,
29,
30,
31].
The stroke rate for CABG in octogenarians is reported to be between 1.3% for off-pump procedures and 2.4% for on-pump procedures [
32]. However, the data are inconsistent. A recently published multicenter study showed no difference in stroke rates between on-pump and off-pump procedures in this specific group of patients [
9]. The same applies to the perioperative rate of acute renal failure, postoperative dialysis, or sepsis. In the present study, we found a perioperative stroke rate of 1.2%, which is comparable to the reported off-pump results and lower than the reported results for on-pump procedures. A possible explanation for this low stroke rate could be the peripheral arterial cannulation strategy [
33] combined with a preoperative CT scan. In summary, the present study shows an in-hospital MACCE rate of 3.7%. This is exceptionally low compared to reported data of 10-13% [
4,
34].
The reported 1-year follow-up results of the groundbreaking myocardial revascularization trials of the recent decades [
35], like the SYNTAX [
25] and the FAME 3 [
26] trial, are in line with the findings in our study. However, our study included significantly older patients with a higher surgical risk profile. The SYNTAX trial reported a 1 year follow-up MACCE rate between 12.9% and 15.5%, depending on the SYNTAX score. Compared to that, the FAME 3 trial reported a MACCE rate of 6.9% after 1 year. The observed MACCE rate of 7.3% after a mean follow-up period of 9.1 months is favorably and competitive compared to the trials mentioned above of conventional bypass surgery using full midline sternotomy. The DuraGraft Registry [
36], a recently published multicenter registry study, prospectively examined the clinical outcome after contemporary conventional CABG and reported a MACCE rate of 7.8% after 1 year. These results are consistent with our findings, despite the increased risk profile in our patient population. Comparing the results of our follow-up with the results of studies focusing on octogenarians, an increased 1-year mortality between 6.7% and 10.5% and a MACCE rate of 14.5% are reported [
8,
34].
Based on our findings, minimally invasive, sternum-sparing CABG using the TCRAT technique emerges as a robust and safe option for the treatment of multivessel CAD that warrant its active considerations, especially in octogenarians. The decision to operate should take into account the patient’s overall condition, mobility, and comorbidities. Age plays an important, but not the only, role.
Study Limitations
There are several limitations of our study.
The present study is a prospective, single-center study to investigate a recently introduced surgical approach and its results in a special group of patients. There is a certain patient selection because octogenarians who showed severe calcifications of the ascending aorta or need for emergency surgery were not included in the present study. The number of patients studied is relatively small. Larger patient numbers could allow for more precise and meaningful analyses. Furthermore, mean follow-up of 9.1 months was only midterm. Longer follow-up periods are necessary to further assess the role of TCRAT in this particular patient collective.
Despite all limitations, the results of the present study are relevant to further advance the development of treatment processes for multivessel CAD disease in old age.
In conclusion, TCRAT enables complete coronary artery revascularization in multivessel CAD without sternotomy and can be safely performed in octogenarians. Both in-hospital and midterm results were favorable and comparable to contemporary outcomes of conventional CABG in elderly patients.
Author Contributions
Conceptualization, Christian Sellin and Hilmar Dörge; Methodology, Christian Sellin; Validation, Christian Sellin, Marius Grossmann, Hilmar Dörge and Volodymyr Demianenko; Formal analysis, Christian Sellin, Hilmar Dörge and Volodymyr Demianenko; Investigation, Christian Sellin, Marius Grossmann, Ahmed Belmenai, Margit Niethammer, Hilmar Dörge and Volodymyr Demianenko; Data curation, Christian Sellin and Ahmed Belmenai; Writing—original draft, Christian Sellin and Volodymyr Demianenko; Writing—review & editing, Christian Sellin, Margit Niethammer, Hilmar Dörge and Volodymyr Demianenko; Visualization, Christian Sellin; Supervision, Marius Grossmann, Hilmar Dörge and Volodymyr Demianenko; Project administration, Christian Sellin.
Funding
There was no funding for this study.
Institutional Review Board Statement
This study was approved by the local ethics committee (University of Marburg, file number: 23-172 RS, approval date: 28 December 2025) and conducted in accordance with the ethical standards outlined in the 1964 Declaration of Helsinki and its subsequent amendments.
Informed Consent Statement
The patients provided informed written consent for the publication of the study data.
Abbreviations
The following abbreviations are used in this manuscript:
| CABG |
coronary artery bypass grafting |
CAD
CPB |
coronary artery disease
cardiopulmonary bypass |
| CT |
сomputed tomography |
ICU
LAD
LCX |
intensive care unit
left anterior descending
left circumflex artery |
LIMA
LVEF |
left internal mammary artery
left ventricular ejection function |
MACCE
PCI |
major adverse cardiac and cerebrovascular events
percutaneous coronary intervention |
RA
RCA |
radial artery
right coronary artery |
SD
SVG
TCRAT |
standard deviation
saphenous vein graft
total coronary revascularization via left anterior thoracotomy |
References
- Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, Domanski MJ, Farkouh ME, Flather M, Fuster V, Hlatky MA, Holm NR, Hueb WA, Kamalesh M, Kim YH, Mäkikallio T, Mohr FW, Papageorgiou G, Park SJ, Rodriguez AE, Sabik JF 3rd, Stables RH, Stone GW, Serruys PW, Kappetein AP. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018 Mar 10;391(10124):939-948. Epub 2018 Feb 23. Erratum in: Lancet. 2018 Aug 11;392(10146):476. doi: 10.1016/S0140-6736(18)31740-9. PMID: 29478841. [CrossRef]
- Sousa-Uva M, Neumann FJ, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2019 Jan 1;55(1):4-90. PMID: 30165632. [CrossRef]
- Kim KM, Arghami A, Habib R, Daneshmand MA, Parsons N, Elhalabi Z, Krohn C, Thourani V, Bowdish ME. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2022 Update on Outcomes and Research. Ann Thorac Surg. 2023 Mar;115(3):566-574. Epub 2023 Jan 6. PMID: 36623634. [CrossRef]
- Rustenbach CJ, Sandoval Boburg R, Radwan M, Haeberle H, Charotte C, Djordjevic I, Wendt S, Caldonazo T, Saqer I, Saha S, Schnackenburg P, Serna-Higuita LM, Doenst T, Hagl C, Wahlers T, Schlensak C, Reichert S. Surgical Outcomes in Octogenarians with Heart Failure and Reduced Ejection Fraction following Isolated Coronary Artery Bypass Grafting-A Propensity Score Matched Analysis. J Clin Med. 2024 Aug 6;13(16):4603. PMID: 39200745; PMCID: PMC11354336. [CrossRef]
- Batty J, Qiu W, Gu S, Sinclair H, Veerasamy M, Beska B, Neely D, Ford G, Kunadian V; ICON-1 Study Investigators. One-year clinical outcomes in older patients with non-ST elevation acute coronary syndrome undergoing coronary angiography: An analysis of the ICON1 study. Int J Cardiol. 2019 Jan 1;274:45-51. Epub 2018 Sep 28. PMID: 30287058. [CrossRef]
- Richter D, Guasti L, Walker D, Lambrinou E, Lionis C, Abreu A, Savelieva I, Fumagalli S, Bo M, Rocca B, Jensen MT, Pierard L, Sudano I, Aboyans V, Asteggiano R. Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute Cardio Vascular Care (ACVC), Association of Cardiovascular Nursing and Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG) Aorta and Peripheral Vascular Diseases, WG e-Cardiology, WG Thrombosis, of the European Society of Cardiology, European Primary Care Cardiology Society (EPCCS). Eur J Prev Cardiol. 2022 Feb 19;29(1):216-227. PMID: 34270717. [CrossRef]
- Picheta W, Góra B, Kachel M, Forszpaniak M, Kolarczyk-Haczyk A, Dudek M, Sawicki F, Buszman P, Gierlotka M, Gąsior M, Milewski K. Clinical presentation and outcomes of acute myocardial infarction with vs. without st elevation in octogenarians. Cardiol J. 2025 Sep 22. Epub ahead of print. PMID: 40981748. [CrossRef]
- Davoodi S, Najafi MS, Vakili-Basir A, Jalali A, Karimi Z, Shahmohamadi E, Dashtkoohi M, Ayati A, Hadizadeh A, Momtahan S, Shirzad M, Bagheri J. Coronary artery bypass grafting in octogenarians: a nomogram for predicting all-cause mortality. J Cardiothorac Surg. 2024 Oct 3;19(1):586. PMID: 39363338; PMCID: PMC11448455. [CrossRef]
- Amber Malhotra, Md. Anamul Islam, Kyle A. McCullough, John B. Eisenga, Giuseppe Tavilla, Ramachandra Reddy, Daniel Beckles, Thomas d’Amato, Robert L. Smith, Charles S. Roberts, Michael J. Mack, J. Michael DiMaio. Coronary Revascularization Surgical Techniques and Outcomes in Octogenarians: A Multicenter Retrospective Matched Study. J. Card. Surg 2025. [CrossRef]
- Babliak O, Demianenko V, Melnyk Y, Revenko K, Pidgayna L, Stohov O. Complete Coronary Revascularization via Left Anterior Thoracotomy. Innovations. 2019;14(4):330-341. [CrossRef]
- Dörge H, Sellin C, Belmenai A, Asch S, Eggebrecht H, Schächinger V. Novel concept of routine total arterial coronary bypass grafting through a left anterior approach avoiding sternotomy. Heart Vessels. 2022 Aug;37(8):1299-1304. Epub 2022 Feb 5. PMID: 35122494; PMCID: PMC9239964. [CrossRef]
- Sellin C, Asch S, Belmenai A, Mourad F, Voss M, Dörge H. Early Results of Total Coronary Revascularization via Left Anterior Thoracotomy. Thorac Cardiovasc Surg. 2023 Sep;71(6):448-454. Epub 2022 Nov 11. Erratum in: Thorac Cardiovasc Surg. 2023 Sep;71(6):e1. doi: 10.1055/s-0043-1768041. PMID: 36368676; PMCID: PMC10480014. [CrossRef]
- Sellin C, Belmenai A, Niethammer M, Schächinger V, Dörge H. Sternum-sparing multivessel coronary surgery as a routine procedure: Midterm results of total coronary revascularization via left anterior thoracotomy. JTCVS Tech. 2024 Jun 3;26:52-60. PMID: 39156523; PMCID: PMC11329208. [CrossRef]
- Babliak O, Demianenko V, Marchenko A, Babliak D, Melnyk Y, Stohov O, Revenko K, Pidgayna L. Left anterior minithoracotomy as a first-choice approach for isolated coronary artery bypass grafting and selective combined procedures. Eur J Cardiothorac Surg. 2023 Aug 1;64(2):ezad182. PMID: 37144954. [CrossRef]
- Demirsoy E, Mavioglu I, Dogan E, Gulmez H, Dindar I, Erol MK. The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers. J Clin Med. 2023 Aug 31;12(17):5663. PMID: 37685730; PMCID: PMC10488478. [CrossRef]
- Arslanhan G, Özcan ZS, Şenay Ş, Baştopçu M, Koçyiğit M, Değirmencioğlu A, Alis D, Alhan C. Robot-Assisted Minimally Invasive Multivessel Coronary Bypass Guided by Computerized Tomography. Innovations (Phila). 2024 Jan-Feb;19(1):30-38. Epub 2023 Dec 19. PMID: 38111997. [CrossRef]
- Demirkıran T, Akyol FB, Özdem T, Hacızade E, Kubat E, Erol G, Kadan M, Karabacak K. Total coronary revascularization via left anterior thoracotomy: Comparison of early- and mid-term results with conventional surgery. Turk Gogus Kalp Damar Cerrahisi Derg. 2024 Oct 30;32(4):402-411. PMID: 39651056; PMCID: PMC11620525. [CrossRef]
- Sellin C, Laube S, Demianenko V, Balan R, Dörge H, Benoehr P. Renal Outcome in Patients Undergoing Minimally Invasive Total Coronary Revascularization via Anterior Minithoracotomy Compared to Full Median Sternotomy Coronary Artery Bypass Grafting. J Clin Med. 2024 Sep 12;13(18):5418. PMID: 39336904; PMCID: PMC11432697. [CrossRef]
- Sellin C, Sand U, Demianenko V, Schmitt C, Schäfer B, Schier R, Doerge H. Comparison of Pulmonary Outcome in Minimally Invasive (TCRAT) and Full Sternotomy CABG. Thorac Cardiovasc Surg. 2025 Apr;73(3):185-190. Epub 2024 Aug 2. PMID: 39095028. [CrossRef]
- Bonzel T, Schächinger V, Dörge H. Description of a Heart Team approach to coronary revascularization and its beneficial long-term effect on clinical events after PCI. Clin Res Cardiol. 2016 May;105(5):388-400. Epub 2015 Oct 27. PMID: 26508415. [CrossRef]
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV; American Heart Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Council on Nutrition, Physical Activity and Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013 Jul;44(7):2064-89. Epub 2013 May 7. Erratum in: Stroke. 2019 Aug;50(8):e239. doi: 10.1161/STR.0000000000000205 PMID: 23652265; PMCID: PMC11078537. [CrossRef]
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018 Nov 13;138(20):e618-e651. Erratum in: Circulation. 2018 Nov 13;138(20):e652. doi: 10.1161/CIR.0000000000000632 PMID: 30571511. [CrossRef]
- Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry). Am J Cardiol. 2002 Apr 1;89(7):791-6. PMID: 11909560. [CrossRef]
- Kirov H, Caldonazo T, Riedel LL, Tasoudis P, Moschovas A, Diab M, Färber G, Doenst T. Comparing outcomes between coronary artery bypass grafting and percutaneous coronary intervention in octogenarians with left main or multivessel disease. Sci Rep. 2023 Dec 15;13(1):22323. PMID: 38102297; PMCID: PMC10724226. [CrossRef]
- Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, Leadley K, Dawkins KD, Mohr F. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010 Jun 22;121(24):2645-53. Epub 2010 Jun 7. PMID: 20530001. [CrossRef]
- Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, Davidavičius G, Kalinauskas G, Mansour S, Kharbanda R, Östlund-Papadogeorgos N, Aminian A, Oldroyd KG, Al-Attar N, Jagic N, Dambrink JE, Kala P, Angerås O, MacCarthy P, Wendler O, Casselman F, Witt N, Mavromatis K, Miner SES, Sarma J, Engstrøm T, Christiansen EH, Tonino PAL, Reardon MJ, Lu D, Ding VY, Kobayashi Y, Hlatky MA, Mahaffey KW, Desai M, Woo YJ, Yeung AC, Pijls NHJ; FAME 3 Investigators. Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med. 2022 Jan 13;386(2):128-137. Epub 2021 Nov 4. PMID: 34735046. [CrossRef]
- Chikwe J, Lee T, Itagaki S, Adams DH, Egorova NN. Long-Term Outcomes After Off-Pump Versus On-Pump Coronary Artery Bypass Grafting by Experienced Surgeons. J Am Coll Cardiol. 2018 Sep 25;72(13):1478-1486. PMID: 30236310. [CrossRef]
- Beckmann A, Meyer R, Eberhardt J, Gummert J, Falk V. German Heart Surgery Report 2023: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg. 2024 Aug;72(5):329-345. Epub 2024 Jul 30. PMID: 39079552. [CrossRef]
- Lemaire A, Soto C, Salgueiro L, Ikegami H, Russo MJ, Lee LY. The impact of age on outcomes of coronary artery bypass grafting. J Cardiothorac Surg. 2020 Jul 1;15(1):158. PMID: 32611349; PMCID: PMC7328264. [CrossRef]
- Attia RQ, Katumalla E, Cyclewala S, Rochon M, Marczin N, Raja SG. Do in-hospital outcomes of isolated coronary artery bypass grafting vary between male and female octogenarians? Interact Cardiovasc Thorac Surg. 2022 Jun 1;34(6):958-965. PMID: 34718583; PMCID: PMC9159460. [CrossRef]
- Ozen A, Unal EU, Songur M, Kocabeyoglu SS, Hanedan O, Yilmaz M, Turkcan BS, Cicekcioglu F, Kaplan S, Birincioglu CL. Coronary artery bypass grafting in the octogenarians: should we intervene, or leave them be? J Geriatr Cardiol. 2015 Mar;12(2):147-52. PMID: 25870618; PMCID: PMC4394330. [CrossRef]
- Altarabsheh SE, Deo SV, Rababa’h AM, Lim JY, Cho YH, Sharma V, Jung SH, Shin E, Markowitz AH, Park SJ. Off-pump coronary artery bypass reduces early stroke in octogenarians: a meta-analysis of 18,000 patients. Ann Thorac Surg. 2015 May;99(5):1568-75. Epub 2015 Mar 17. PMID: 25791924. [CrossRef]
- Sellin C, Belmenai A, Demianenko V, Grossmann M, Dörge H. Direct Axillary Artery Cannulation as Standard Perfusion Strategy in Minimally Invasive Coronary Artery Bypass Grafting. J Cardiovasc Dev Dis. 2025 Jan 18;12(1):31. PMID: 39852309; PMCID: PMC11766195. [CrossRef]
- Khan MR, Kayani WT, Ahmad W, Manan M, Hira RS, Hamzeh I, Jneid H, Virani SS, Kleiman N, Lakkis N, Alam M. Effect of increasing age on percutaneous coronary intervention vs coronary artery bypass grafting in older adults with unprotected left main coronary artery disease: A meta-analysis and meta-regression. Clin Cardiol. 2019 Nov;42(11):1071-1078. Epub 2019 Sep 5. PMID: 31486094; PMCID: PMC6837018. [CrossRef]
- Ruel M, Falk V, Farkouh ME, Freemantle N, Gaudino MF, Glineur D, Cameron DE, Taggart DP. Myocardial Revascularization Trials. Circulation. 2018 Dec 18;138(25):2943-2951. PMID: 30566019. [CrossRef]
- Sandner S, Misfeld M, Caliskan E, Böning A, Aramendi J, Salzberg SP, Choi YH, Perrault LP, Tekin I, Cuerpo GP, Lopez-Menendez J, Weltert LP, Böhm J, Krane M, González-Santos JM, Tellez JC, Holubec T, Ferrari E, Doros G, Vitarello CJ, Emmert MY; Registry Investigators; European DuraGraft Registry investigators’. Clinical outcomes and quality of life after contemporary isolated coronary bypass grafting: a prospective cohort study. Int J Surg. 2023 Apr 1;109(4):707-715. PMID: 36912566; PMCID: PMC10389413. [CrossRef]
Table 1.
Baseline and clinical parameters.
Table 1.
Baseline and clinical parameters.
| Variables |
n=82
n (%)
|
| Age (years) |
82.7±1.8 (80-88) |
| Male |
66 (80.5%) |
| BMI (kg/m²) |
26.5±3.1 (20.1-35.4) |
| Hypertension |
80 (97.6%) |
| Diabetes mellitus |
20 (24.4%) |
| Chronic lung disease |
6 (7.3%) |
| Current smoker |
5 (6.1%) |
Peripheral or cerebrovascular
arterial disease |
64 (78.5%) |
| Creatinine (mg/dl) |
1.2±0.6 (0.7-6) |
EuroSCORE II (%)
EuroSCORE II ≥4 |
5.1±2.4 (1.5-17.5)
44 (53.7%) |
LVEF (%)
LVEF ≤ 30 |
49.2±9.1 (20-55)
7 (8.5%) |
| 2-vessel disease |
14 (17.1%) |
| 3-vessel disease |
68 (82.9%) |
| Left main stenosis >50% |
34 (41.5%) |
| Prior NSTEMI |
31 (37.8%) |
| Prior PCI |
19 (23.2%) |
Table 2.
Operative characteristics.
Table 2.
Operative characteristics.
| Variables |
n=82
n (%)
|
Aortic cross-clamp time, min
Median
IQR |
88±31 (22-162)
89
44 |
CPB time, min
Median
IQR |
142±38 (56-243)
142
49 |
Operative time, min
Median
IQR |
299±64 (164-480)
301
143 |
| Number of distal anastomoses |
3.0±0.9 (2-5) |
Conduits
LIMA
RA
SVG |
81 (98.8%)
36 (43.9%)
57 (69.5%) |
| Complete arterial revascularization |
25 (30.5%) |
| Multiple arterial revascularization |
39 (47.6%) |
| Complete anatomical revascularization |
78 (95.1%) |
Table 3.
In-hospital outcome.
Table 3.
In-hospital outcome.
| Variables |
n=82
n (%)
|
| Rethoracotomy |
6 (7.3%) |
| ARF requiring dialysis |
3 (3.7%) |
| Pneumonia |
1 (1.2%) |
| New onset of atrial fibrillation |
7 (8.5%) |
ICU length of stay, days
Median
IQR |
2.7±4.8 (1-37)
1
1 |
In-hospital length of stay, days
Median
IQR |
13.0±10.9 (6-71)
9
5 |
| Stroke |
1 (1.2%) |
| Myocardial infarction |
0 (0.0%) |
Postoperative PCI
Of these planned procedures |
1 (1.2%)
1 (1.2%) |
| In-hospital mortality |
1 (1.2%) |
| In-hospital MACCE |
3 (3.7%) |
Table 4.
Midterm follow-up data.
Table 4.
Midterm follow-up data.
| Variables |
n=82
n (%)
|
| Stroke |
1 (1.2%) |
| Myocardial infarction |
0 (0.0%) |
| Postoperative PCI |
2 (2.4%) |
| Cardiac mortality |
1 (1.2%) |
| All-cause-mortality |
4 (4.9%) |
| Overall MACCE |
6 (7.3%) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).