1. Why Is It Important to Teach Healthy Life-Style Starting in Childhood?
Childhood obesity represents an ongoing challenge for both primary and secondary prevention in order to avoid adipose tissue overgrowth and its associated complications[
1].
The rising prevalence of pediatric obesity, which is expected to lead to a growing number of adults with long-term metabolic complications, highlights the need for effective strategies to reverse this alarming trend[
2]. In fact, we are already witnessing the detrimental impact of obesity on adult health, to the extent that it has finally been officially recognized as a disease. Italy is the first country in the world to legally acknowledge obesity as a “progressive and relapsing” condition.
On October 1, 2025, the Italian Senate definitively approved Bill No. 1483 (commonly referred to as the “Pella Law,” named after the Forza Italia MP who proposed and co-signed it), which addresses the prevention, treatment, and social inclusion of individuals living with obesity—currently estimated at around six million people in Italy (excluding those who are overweight)[
3].
This landmark decision represents a turning point, not only reflecting growing awareness among the general public, policymakers, and the scientific community, but also laying the foundation for formally recognizing the opportunity to counter the obesity epidemic. It emphasizes the need for a comprehensive, preventive strategy—particularly during childhood, which constitutes the most sensitive and critical window for intervention.
Children and adolescents today are embedded within environments that inadequately support, and often actively undermine, healthy development. These obesogenic settings—characterized by pervasive exposure to energy-dense, nutrient-poor food options and limited opportunities for physical activity—promote sedentary behavior and social disengagement.
Proximity to fast-food vendors near schools has been linked to higher BMI and body fat in pediatric populations[
4].
Globally, the coexistence of obesogenic behaviors (e.g., poor dietary patterns, low physical activity, high sedentary time) remains highly prevalent among adolescents, with 9.8–10.2% concurrently exhibiting three or more such behaviors across multiple countries between 2003 and 2017[
5].
Additionally, a large-scale meta-analysis revealed that neighborhoods with better infrastructure—like bike lanes, sidewalks, and green spaces—are linked to lower childhood obesity rates[
6].
The Mediterranean dietary pattern is widely acknowledged for its favorable impact on health outcomes. Nevertheless, in geographical regions where adherence would apparently be more attainable, such as southern Europe, the prevalence of childhood obesity continues to escalate[
7].
In a cohort of children from Southern Italy, 71.2% showed poor adherence to the Mediterranean diet, 26.5% had moderate adherence, and only 2.3% demonstrated good adherence[
8].
Moreover, obesity etiology extends beyond suboptimal dietary patterns to encompass a broader spectrum of unhealthy lifestyle behaviors—among them, physical inactivity, excessive screen time, and disrupted sleep patterns. These factors not only contribute to reduced adherence to the Mediterranean diet but also exacerbate obesity risk in children aged 5–12 years[
9].
Given this context, there is a compelling need to strengthen preventive strategies through early-life health promotion in pediatric settings. Lifestyle interventions initiated in childhood can have prolonged metabolic benefits, as demonstrated by long-term alterations in biomarkers even years after the initial intervention period[
10].
In summary, contemporary societal and environmental contexts create multiple, reinforcing pressures that foster unhealthy eating, sedentary lifestyles, and social isolation in young populations. Such obesogenic environments represent a significant barrier to pediatric health that demands multifaceted, systemic interventions at the individual and community levels.
2. Modern Paradox: Greater Knowledge, Worse Habits
Before addressing how to educate children and their parents to understand and adhere to a healthy lifestyle, it is important to reflect on how we have reached the current situation. Historically, knowledge of the complications of obesity was far more limited, yet the condition was considerably less prevalent. Today, despite substantial scientific evidence on the health consequences of obesity, its prevalence continues to rise globally, and healthcare professionals often appear to face twice the effort in educating patients and their families about the associated risks[
11].
Knowledge alone, however, is insufficient. Unhealthy behaviors persist as a result of a complex interplay among environmental, biological, psychological, and social factors. Effective interventions therefore require multidimensional strategies, including environmental and policy measures, education, psychological support, more accurate diagnostic approaches, and broad societal change.
As a matter of fact, BMI is often used as an index of anthropometric evaluation but it may mask the true problem of an improper lifestyle, which will become evident with a pathological BMI when it may be too late[
12].
One major barrier is the information overload surrounding diet and health, which is not always grounded in scientific evidence. The spread of dietary fads and misinformation contributes to confusion, making it difficult for the public to distinguish evidence-based recommendations from commercial messaging[
13].
Modern society is characterized by an “obesogenic environment”, where the continuous availability of inexpensive, energy-dense, and highly palatable foods—rich in sugars, fats, and salt—facilitates unhealthy choices[
14]. Food marketing, particularly when directed toward children, strongly influences dietary preferences, while urban lifestyles reduce time for meal preparation and favor reliance on fast foods and processed products[
15].
Although the importance of physical activity is widely recognized, daily life has become increasingly sedentary, dominated by motorized transport, office-based occupations, and screen-based leisure[
16]. Stressful routines and time constraints frequently drive individuals toward quick, immediately rewarding choices. Moreover, chronic stress, insufficient sleep, and sedentary work promote compensatory behaviors such as emotional eating[
17]. Importantly, food is not only a source of nutrition but also of gratification, and changing deeply ingrained habits requires motivation, social support, and tailored strategies—mere awareness of “what is right” is not sufficient[
18].
In response to these challenges, we have developed an updated version of the traditional food pyramid—now reconceptualized as a Mediterranean Lifestyle Tridimensional Pyramid tailored specifically for children and adolescents. This model integrates evidence-based recommendations not only for dietary quality and eating behavoir, but also for physical activity and sleep hygiene[
19]. Furthemore, it illustrates the importance of a well balanced muscle-fat body composition in relation to protective and promotive factors on health[
20]. It aims to enhance relevance, clarity, and accessibility, thereby empowering pediatric clinicians, educators, and caregivers to more effectively promote sustainable healthy lifestyle.
3. The food choice triangle
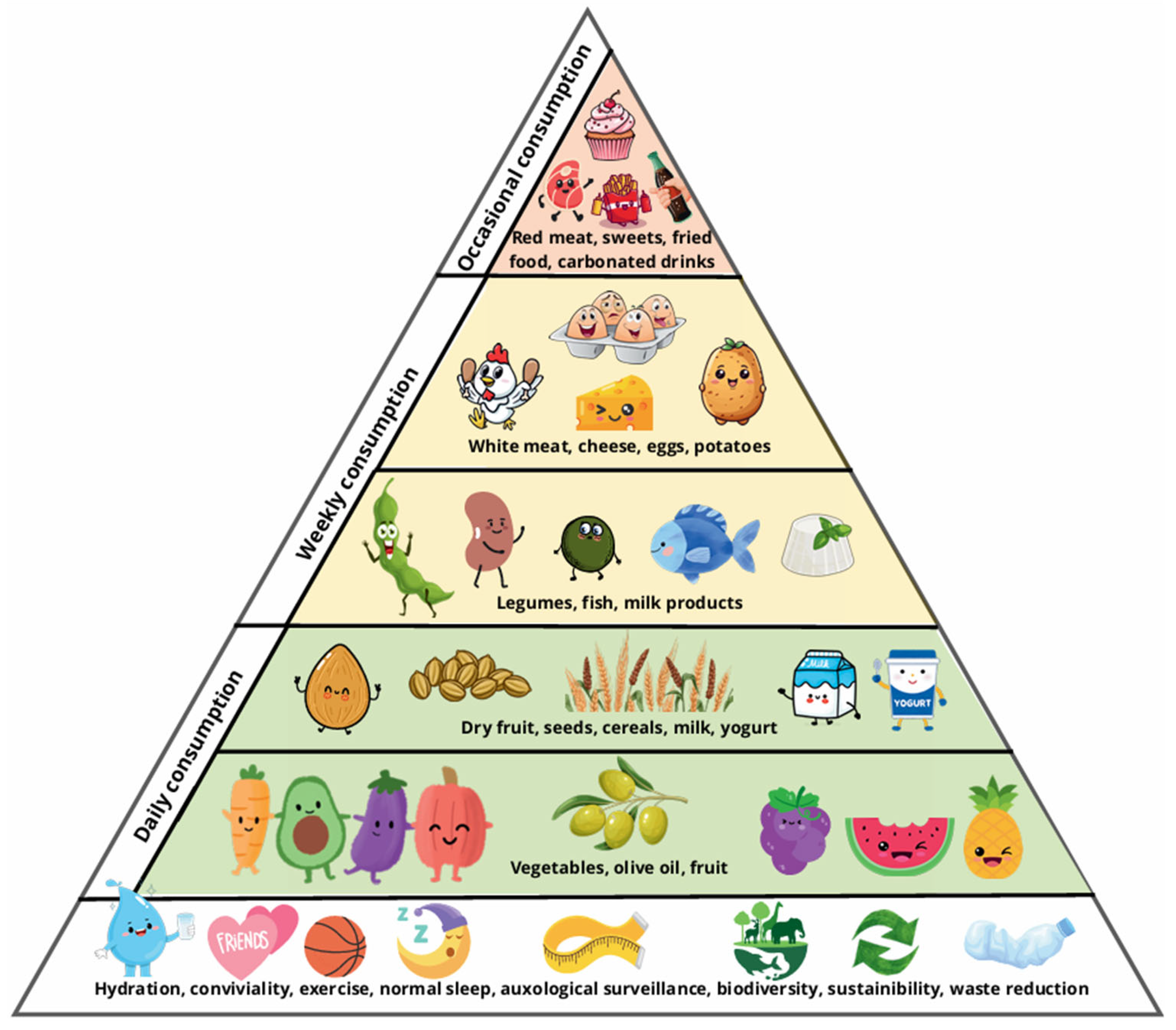
The “Food Choice Triangle” (
Figure 1) of our tridimensional pyramid represents the updated version of the Mediterranean Diet Pyramid proposed by the Italian Society of Human Nutrition (SINU) earlier this year, slightely adapted to pediatric outsetting[
21].
This new model was developed as a tool to support educational activities and public health campaigns promoting a healthy and sustainable diet.
Core values such as biodiversity, environmental sustainability, and waste reduction should be introduced early in life[
22]. Pediatric outpatient visits offer a valuable opportunity to foster awareness and reflection on these topics among children and their families.
The grounds of a healthy lifestyle need to be established during infancy and adolescence, emphasizing key elements such as family meals, adequate sleep patterns, and regular physical activity—particularly in the form of unstructured play and organized sports. It is essential to clearly communicate to both parents and children that age-appropriate sleep duration is not only a primary determinant of healthy cognitive development, longitudinal growth and timely pubertal progression but plays a central role in preventing excessive weight gain[
23].
In this context, the focus in pediatrics should not be solely on weight control, but rather on routine auxological surveillance. This approach facilitates the early identification of abnormal growth trajectories that may signal an increased risk for the development of childhood obesity and represents a crucial window for early intervention[
24].
Water should be promoted as the exclusive beverage of choice, without the addition of flavorings or sweeteners[
25]. Therefore, the consumption of energy drinks among adolescents as well as juices among infants must be discouraged.
The structure of the food choice pyramid—ranging from foods recommended for daily consumption to those intended for occasional intake—remains almost the same in the pediatric setting.
However, in pediatric context it is particularly important to promote nutritional education that raises awareness among children and families of the need to include vegetables daily in both lunch and dinner as a preventative measure against excess weight gain and future metabolic complications[
26].
Furthermore, nutritional requirements change throughout childhood, and during puberty, it is particularly important to ensure sufficient milk consumption as a source of calcium, protein, and other nutrients critical for bone growth and overall development[
27].
4. The Daily Food Distribution Triangle
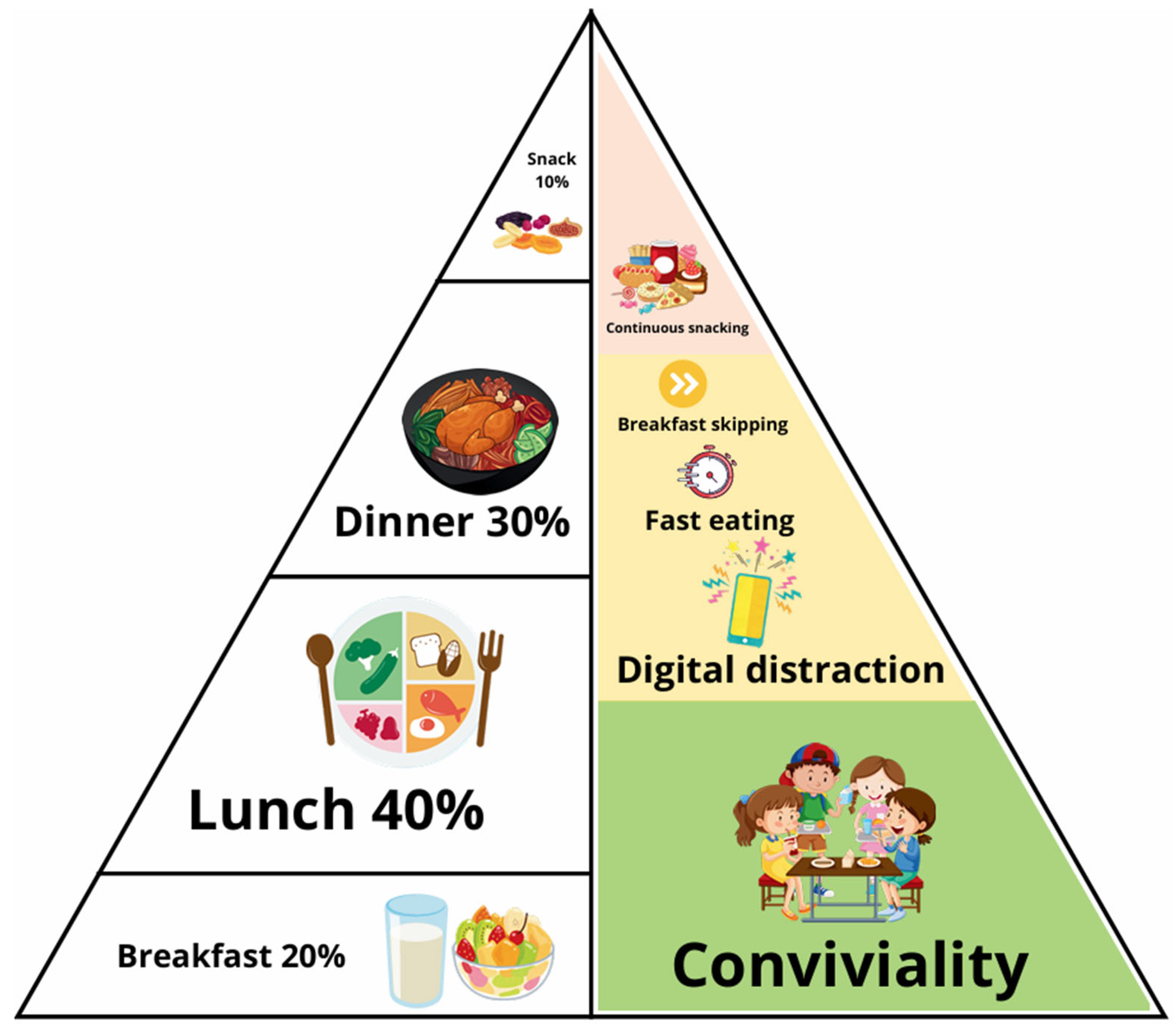
This schematic representation (
Figure 2) is divided into two sections: on the left, it illustrates the recommended daily meal distribution, while on the right, it highlights the most frequent dietary errors.
The recommended dietary pattern consists of five meals per day—breakfast, lunch, dinner, and two snacks. Breakfast is positioned at the base of the diagram, symbolizing its role as the starting point of daily food intake. Notably, breakfast omission is among the most prevalent dietary mistakes[
28].
Lunch constitutes the main caloric intake of the day, whereas breakfast and dinner combined should account for approximately 50% of total daily energy consumption. Snacks should contribute no more than 10% of daily caloric intake[
29].
Children of the kindergarden age might need two snacks due to a physiologically shorter duration of fasting tolerance[
30,
31]. Frequent snacking and rapid eating are identified as key nutritional errors[
32]. Persistent snacking interferes with the physiological postprandial suppression of insulin between meals, while rapid eating compromises the onset of satiety, potentially leading to overeating[
33].
Furthermore, eating while distracted—such as during television viewing, phone use, or other forms of entertainment—reduces meal awareness and satiety perception[
34]. One of the fundamental principles of healthy eating behavior is conviviality, which promotes shared meals, social interaction, and overall psychological well-being.
This visual tool enables patients to clearly recognize how improper meal timing and common eating behaviors contribute to an unhealthy lifestyle.
5. The Muscle-Adipose Tissue Triangle
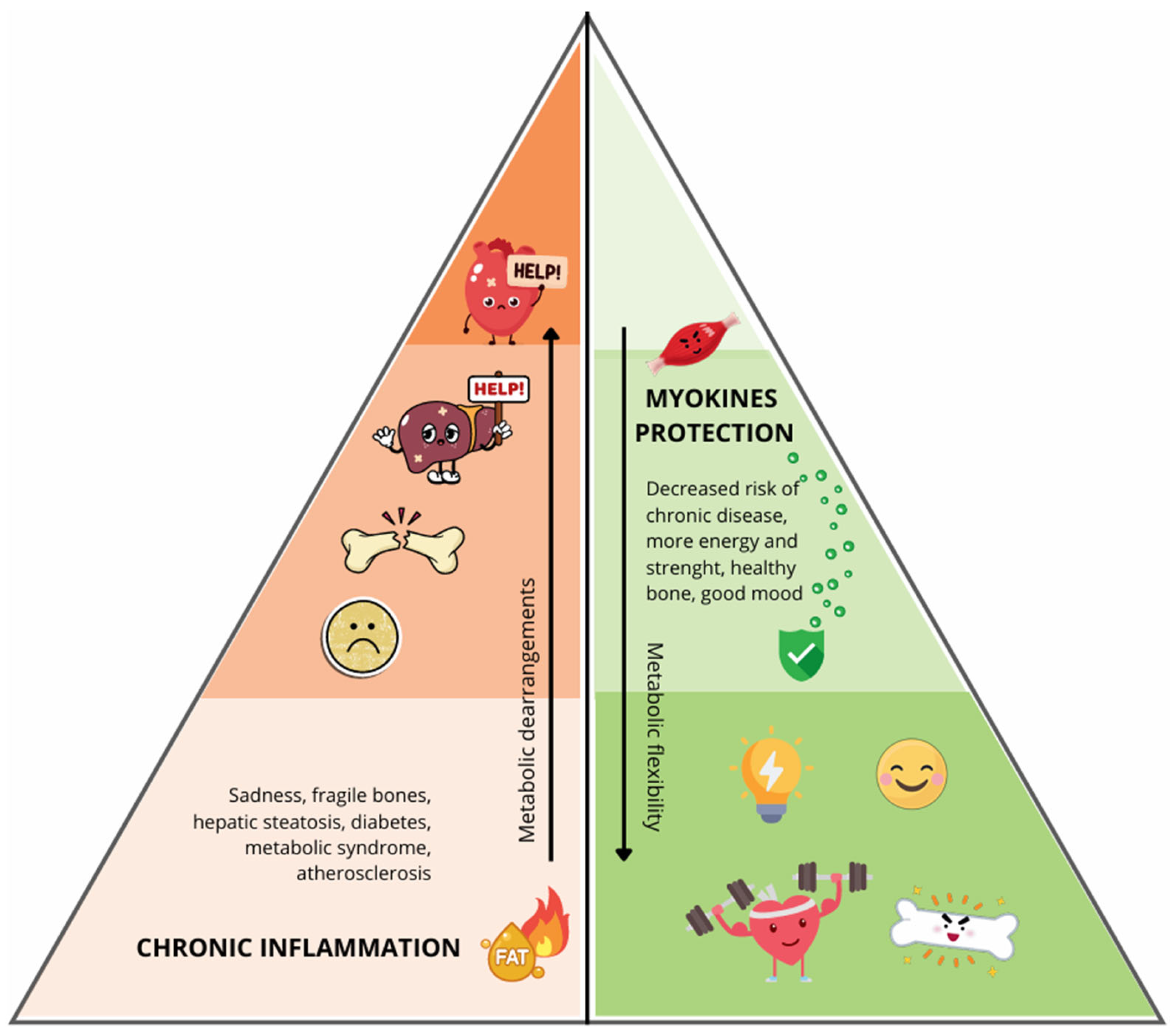
This schematic figure (
Figure 3) illustrates the balance between skeletal muscle and adipose tissue, two metabolically active compartments whose interaction plays a critical role in determining health trajectories from early life. A bipartite colour gradient is employed: on the right side, muscle tissue (green), varying from deep green at the base—indicating high muscle mass—to pale green/white at the apex—indicating low muscle mass; on the left, adipose tissue (red), moving from white at the base—minimal fat stores—to deep red at the apex—excessive adiposity.
The base of the figure is the physiological ideal state, characterised by high muscle mass and low fat mass. As well known, disfunctional adipose tissue in obesity perpetuates chronic low-grade inflammation via hypertrophic adipocytes and immune cell infiltration, thereby driving systemic insulin resistance and metabolic disease[
35].
Skeletal muscle, now recognised as an endocrine organ, contributes to metabolic flexibility via myokine release; these myokines enhance glucose uptake, promote lipid oxidation, improve insulin sensitivity, and mitigate chronic low-grade inflammation[
36].
In contrast, the apex of the image represents metabolic dysregulation, a state marked by low muscle mass together with excessive adiposity. Consequences include systemic insulin resistance, dyslipidemia, elevated blood pressure, and increased visceral fat deposition. These derangements are associated with elevated risk for obesity, type 2 diabetes, and cardiovascular disease. Childhood adiposity has been shown through Mendelian randomization to causally contribute to future adult coronary heart disease, myocardial infarction, heart failure, and atrial fibrillation[
37].
Beyond these metabolic effects, adequate muscle mass correlates with reduced fatigue, increased physical energy, and improved mood regulation—factors especially important when educating children about healthy lifestyle habits. Excess adipose tissue is also frequently linked to diminished vitality and an increased predisposition to low mood, compounding the adverse health profile.
In children with overweight/obesity but preserved muscle strength, anthropometric and cardiovascular risk markers are lower than in those with low strength, even when fat mass is similar[
38].
By juxtaposing these two extremes, the figure highlights the importance of maintaining an appropriate ratio of muscle to fat mass. This conceptual framework may serve as an effective pedagogical tool for children, emphasising that regular physical activity and balanced nutrition not only support long-term metabolic health, but also promote daily well-being, energy, and emotional resilience.
It is therefore essential to underscore that daily physical exercise is not only important for reducing adipose tissue, but—more critically—for preserving and enhancing skeletal muscle mass, whose endocrine activity exerts a fundamental protective role in maintaining metabolic homeostasis[
39].
6. The Health Benefit-Risk Triangle
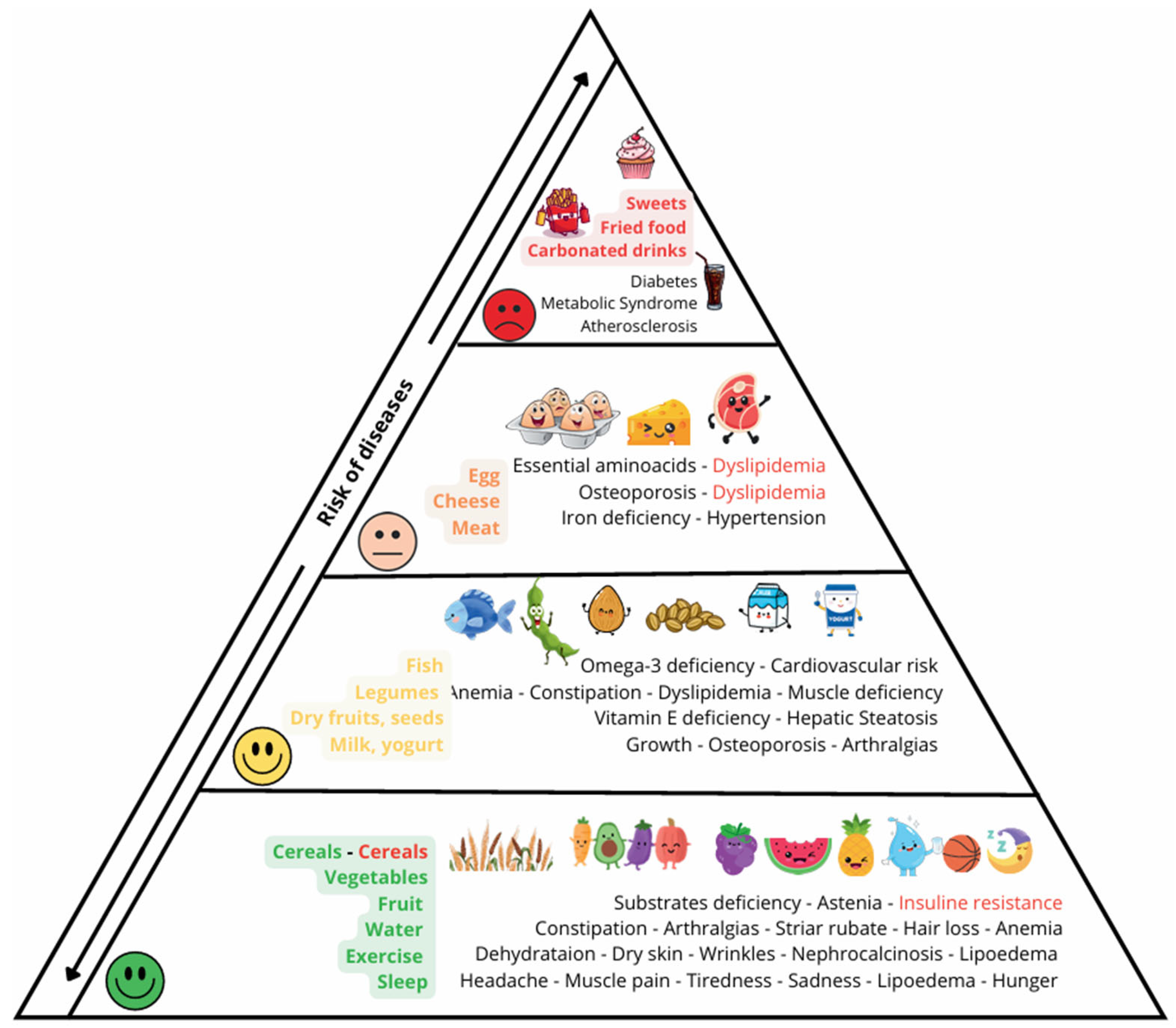
In this triangle (
Figure 4), the protective effects of a healthy lifestyle are explicitly contrasted with the pathological consequences of an unhealthy one. The figure aims to depict signs and symptoms in accessible terms even to younger children, while retaining scientific accuracy.
At the base of the triangle (depicted in green), the positive effects of regular physical activity and a normalized sleep-wake cycle are emphasized. These include prevention of headaches, myalgia, depressive mood, and excessive hunger, as well as mitigation of lipedema risk[
40].
The role of adequate hydration is illustrated in relation to dry skin, wrinkling, nephrocalcinosis, and lipedema. The importance of fruit and vegetable consumption is shown with respect to skin integrity, prevention of striae rubrae, and reduction in hair loss. The scheme also considers cereal intake in its bimodel way: insufficiency may lead to substrate deficiency and inadequate energy supply, whereas excessive or improper cereal consumption is indicated as a contributor to insulin resistance and metabolic dysregulation.
In the intermediate region of the triangle (depicted in yellow), the benefits of milk and dairy products for longitudinal growth are presented. Particular attention is given to growth failure in both obese and undernourished children, for whom achieving genetic target height may not be assured. Observational evidence (Project Viva) shows that early childhood consumption of higher-fat cow’s milk was not associated with increased adiposity in adolescence and may be inversely associated with overweight/obesity risk[
41]. Moreover, umbrella reviews suggest milk intake more often associates with benefits than harms for outcomes like bone health, metabolic syndrome, and cardiovascular disease[
42]. Dietary calcium importance for bone health is thus supported. Nuts and seeds are noted for their high vitamin E content and a potential protective effect against hepatic steatosis. Fish intake, or the lack thereof, is portrayed in terms of omega-3 deficiency and its associated cardiovascular risk: long-chain polyunsaturated fatty acids have been shown to have protective effects in childhood cardiovascular risk profiles[
43].
The upper portions of the triangle (depicted in orange and red) serve to illustrate that, while healthy nutrition plays a crucial role in protecting from disease and maintaining a good health state, its positive effects may be overridden by over-eating highly flavorful processed foods which induce metabolic and cardiovascular disease.
However, children and parents can be reminded that taste is modificable and inducible by offering high quality food taste might change and high processed food not be graft[
44].
The visual stratification helps the patient to appreciate the degree of health risk exposure, and to understand how, over time, persistent unhealthy lifestyle factors can impair long-term health.
7. How to Use the Tridimensional Pyramid in an Outpatient Setting
The three-dimensional pyramid model enables clinicians, nurses, and dietitians to communicate the significance of a healthy lifestyle—comprising nutrition, eating behaviours, and physical activity—and its implications for health outcomes.
By presenting the standing pyramid to patients and their families, the educator indicates that the base, comprising the lower halves of the first three faces, represents the health-promoting factors. It can be readily explained that adherence to these foundational “rules” supports the development of a favourable metabolic age profile, overall well-being, and long-term good health. As one ascends the faces of the pyramid, adverse lifestyle habits become more evident, and these are depicted as accelerating metabolic ageing.
If these adverse habits continue unchecked, the pyramid metaphorically becomes unstable and may collapse. This instability serves to demonstrate to patients and families that health is severely threatened by unhealthy lifestyle choices, leading over time to metabolic and cardiovascular disease, as portrayed on the fourth face of the pyramid.
Finally, the collapse of the pyramid, which can no longer remain stable when supported only at its apex, exposes a 5th face (
Figure 5) — corresponding to the pyramid’s base — that summarises the pillars of health that the patient must consistently uphold in daily life in order to preserve long-term health summarized with the slogan “keep your health standing up”.
Establishing a strong and effective channel of communication between the healthcare provider and the pediatric patient is fundamental to promoting healthy behavioral change. This process requires direct, distraction-free interaction, with the food pyramid placed centrally to serve as a shared point of reference. The clinician should engage the child in a structured yet empathetic dialogue, inquiring about their daily habits, such as the frequency of vegetable consumption, breakfast routines, snack choices, and physical activity levels. Building rapport also involves tailoring the conversation to the child’s developmental stage and interests, demonstrating empathy toward their individual challenges, social context, and the pressures they may face in everyday life. Nutritional and lifestyle recommendations must be personalized: for example, in a child with highly unstructured eating habits, who refuses vegetables and consumes only sugary drinks, the initial goal should be small and achievable—such as improving hydration by gradually replacing sweetened beverages with water. Similarly, for children unable to access organized sports, it is important to convey that physical activity can be achieved through informal, everyday movement. While artificial intelligence tools may assist in providing information and suggestions, they cannot replace the human elements of trust, empathy, and personalized care that underpin the educator–child relationship[
45].
8. Concusions
It is now evident that there is a pressing need to develop a large-scale tool for disseminating information on healthy lifestyles and promoting both primary and secondary prevention of obesity.
This three-dimensional pyramid enables health educators to emphasise clearly each component of a healthy lifestyle. During any given educational session, one face of the pyramid may be examined in greater detail, while always recognising its interdependence with the entire model. With this tool, we aim to offer clinicians an accessible and innovative means of promoting health from infancy onwards.
In parallel with the widespread increase in childhood obesity, pediatric clinics are increasingly encountering normal-weight children who present with an unfavorable lean-to-fat mass ratio and laboratory findings indicative of metabolic dysfunction, such as hypertriglyceridemia and hypercholesterolemia. This underscores the fact that being within a normal weight range does not necessarily equate to being metabolically healthy. Therefore, it is essential to promote healthy lifestyle habits—including balanced nutrition and regular physical activity—not only among overweight or obese children but also among those with normal weight and their families. Adherence to a healthy lifestyle should be regarded as a universal standard of care, and appropriate health education must be provided to all pediatric patients.
The new law on obesity sets as its primary objective the establishment of a National Program for the Prevention and Treatment of Obesity, supported by a dedicated and progressively increasing allocation of public funds over the coming years. These resources will be used to finance public awareness campaigns and nutrition education in schools and among the general population, promote physical activity, and support the training of healthcare professionals.
We firmly believe that the tool we propose will prove to be extremely useful, as it will support the launch of public information campaigns, targeted training for healthcare professionals (including general practitioners, pediatricians, and National Health Service personnel), and a variety of school-based, community, and local-level initiatives. These efforts aim to prevent obesity, raise public awareness, and promote healthy lifestyles.
Author Contributions
Conceptualization, project administration, A.M. (corresponding author): conceived the structure of the review; Writing original draft preparation, G.D.P.; Writing, review and editing, A.M. G.T. I.B. M.P and N.P.; Visualization, A.D.L. created the original figures used in the manuscript. Supervision, F.C. - validation - critically reviewed and revised the manuscript for intellectual content and clarity. All authors made substantial contributions to the conception or drafting of the work, have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data was created.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhang, X.; Liu, J.; Ni, Y.; Yi, C.; Fang, Y.; Ning, Q.; Shen, B.; Zhang, K.; Liu, Y.; Yang, L.; et al. Global Prevalence of Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2024, 178, 800. [Google Scholar] [CrossRef]
- Park, H.; Choi, J.E.; Jun, S.; Lee, H.; Kim, H.S.; Lee, H.A.; Park, H. Metabolic Complications of Obesity in Children and Adolescents. Clin. Exp. Pediatr. 2024, 67, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Gazzetta Ufficiale della Repubblica Italiana Law No. 149 of 3 October 2025. Provisions for the prevention and treatment of obesity; 2025.
- Filgueiras, M.D.S.; Pessoa, M.C.; Bressan, J.; Fogal Vegi, A.S.; Do Carmo, A.S.; Albuquerque, F.M.D.; Gardone, D.S.; Novaes, J.F.D. Characteristics of the Obesogenic Environment around Schools Are Associated with Body Fat and Low-Grade Inflammation in Brazilian Children. Public Health Nutr. 2023, 26, 2407–2417. [Google Scholar] [CrossRef]
- Fan, H.; Zhang, X. Prevalence of and Trends in the Co-Existence of Obesogenic Behaviors in Adolescents From 15 Countries. Front. Pediatr. 2021, 9, 664828. [Google Scholar] [CrossRef] [PubMed]
- Jia, P.; Shi, Y.; Jiang, Q.; Dai, S.; Yu, B.; Yang, S.; Qiu, G.; Yang, S. Environmental Determinants of Childhood Obesity: A Meta-Analysis. Lancet Glob. Health 2023, 11, S7. [Google Scholar] [CrossRef]
- Kanellopoulou, A.; Giannakopoulou, S.-P.; Notara, V.; Antonogeorgos, G.; Rojas-Gil, A.P.; Kornilaki, E.N.; Konstantinou, E.; Lagiou, A.; Panagiotakos, D.B. The Association between Adherence to the Mediterranean Diet and Childhood Obesity; the Role of Family Structure: Results from an Epidemiological Study in 1728 Greek Students. Nutr. Health 2021, 27, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Rutigliano, I.; Mansueto, M.L.; Canestrale, R.; Giorgio, R.; Sacco, M.; Pastore, M.R. Children’s Diet Assessed with the Mediterranean Diet Index: The Finding of New Eating Habits and Their Impact on a Cohort of Italian Children. Ann. Ist. Super. Sanita 2024, 60, 179–183. [Google Scholar] [CrossRef]
- Masini, A.; Dallolio, L.; Sanmarchi, F.; Lovecchio, F.; Falato, M.; Longobucco, Y.; Lanari, M.; Sacchetti, R. Adherence to the Mediterranean Diet in Children and Adolescents and Association with Multiple Outcomes: An Umbrella Review. Healthcare 2024, 12, 449. [Google Scholar] [CrossRef]
- Zarei, I.; Eloranta, A.-M.; Klåvus, A.; Väistö, J.; Lehtonen, M.; Mikkonen, S.; Koistinen, V.M.; Sallinen, T.; Haapala, E.A.; Lintu, N.; et al. Eight-Year Diet and Physical Activity Intervention Affects Serum Metabolites during Childhood and Adolescence: A Nonrandomized Controlled Trial. iScience 2024, 27, 110295. [Google Scholar] [CrossRef]
- Kerr, J.A.; Patton, G.C.; Cini, K.I.; Abate, Y.H.; Abbas, N.; Abd Al Magied, A.H.A.; Abd ElHafeez, S.; Abd-Elsalam, S.; Abdollahi, A.; Abdoun, M.; et al. Global, Regional, and National Prevalence of Child and Adolescent Overweight and Obesity, 1990–2021, with Forecasts to 2050: A Forecasting Study for the Global Burden of Disease Study 2021. The Lancet 2025, 405, 785–812. [Google Scholar] [CrossRef]
- Zapata, J.K.; Azcona-Sanjulian, M.C.; Catalán, V.; Ramírez, B.; Silva, C.; Rodríguez, A.; Escalada, J.; Frühbeck, G.; Gómez-Ambrosi, J. BMI-Based Obesity Classification Misses Children and Adolescents with Raised Cardiometabolic Risk Due to Increased Adiposity. Cardiovasc. Diabetol. 2023, 22, 240. [Google Scholar] [CrossRef]
- Segado Fernández, S.; Jiménez Gómez, B.; Jiménez Hidalgo, P.; Lozano-Estevan, M.D.C.; Herrera Peco, I. Disinformation about Diet and Nutrition on Social Networks: A Review of the Literature. Nutr. Hosp. 2025. [Google Scholar] [CrossRef] [PubMed]
- Petridi, E.; Karatzi, K.; Magriplis, E.; Charidemou, E.; Philippou, E.; Zampelas, A. The Impact of Ultra-Processed Foods on Obesity and Cardiometabolic Comorbidities in Children and Adolescents: A Systematic Review. Nutr. Rev. 2024, 82, 913–928. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.K.; Christiansen, P.; Finlay, A.; Jones, A.; Maden, M.; Boyland, E. A Systematic Review and Meta-analysis of the Effect of Digital Game-based or Influencer Food and Non-alcoholic Beverage Marketing on Children and Adolescents: Exploring Hierarchy of Effects Outcomes. Obes. Rev. 2023, 24, e13630. [Google Scholar] [CrossRef]
- Christian, H.E.; Adams, E.K.; Moore, H.L.; Nathan, A.; Murray, K.; Schipperijn, J.; Trost, S.G. Developmental Trends in Young Children’s Device-Measured Physical Activity and Sedentary Behaviour. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 97. [Google Scholar] [CrossRef] [PubMed]
- Breda, M.; Belli, A.; Esposito, D.; Di Pilla, A.; Melegari, M.G.; DelRosso, L.; Malorgio, E.; Doria, M.; Ferri, R.; Bruni, O. Sleep Habits and Sleep Disorders in Italian Children and Adolescents: A Cross-Sectional Survey. J. Clin. Sleep Med. 2023, 19, 659–672. [Google Scholar] [CrossRef]
- Abdoli, M.; Scotto Rosato, M.; Cipriano, A.; Napolano, R.; Cotrufo, P.; Barberis, N.; Cella, S. Affect, Body, and Eating Habits in Children: A Systematic Review. Nutrients 2023, 15, 3343. [Google Scholar] [CrossRef]
- Peng, Z.; Wen, L.M.; Lau, P.W.C. Effectiveness of a Parent-Based eHealth Intervention on Physical Activity, Dietary Behaviors, and Sleep in Preschoolers: Randomized Controlled Trial. J. Med. Internet Res. 2025, 27, e70886. [Google Scholar] [CrossRef]
- Rota, M.; Morales-Suárez-Varela, M.; Donzelli, G. Effect of the Mediterranean Diet on BMI and Body Composition: A Preliminary Pre-Post Intervention Study in Pediatric Overweight Patients. Nutrition 2025, 139, 112878. [Google Scholar] [CrossRef]
- Sofi, F.; Martini, D.; Angelino, D.; Cairella, G.; Campanozzi, A.; Danesi, F.; Dinu, M.; Erba, D.; Iacoviello, L.; Pellegrini, N.; et al. Mediterranean Diet: Why a New Pyramid? An Updated Representation of the Traditional Mediterranean Diet by the Italian Society of Human Nutrition (SINU). Nutr. Metab. Cardiovasc. Dis. 2025, 35, 103919. [Google Scholar] [CrossRef]
- Teixeira, B.; Afonso, C.; Rodrigues, S.; Oliveira, A. Healthy and Sustainable Dietary Patterns in Children and Adolescents: A Systematic Review. Adv. Nutr. 2022, 13, 1144–1185. [Google Scholar] [CrossRef] [PubMed]
- Grimaldi, M.; Bacaro, V.; Natale, V.; Tonetti, L.; Crocetti, E. The Longitudinal Interplay between Sleep, Anthropometric Indices, Eating Behaviors, and Nutritional Aspects: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 3179. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Toh, J.Y.; Natarajan, P.; Cai, S.; Ong, Y.Y.; Descarpentrie, A.; Lioret, S.; Bernard, J.Y.; Müller-Riemenschneider, F.; Godfrey, K.M.; et al. Trajectories of Lifestyle Patterns from 2 to 8 Years of Age and Cardiometabolic Risk in Children: The GUSTO Study. Int. J. Behav. Nutr. Phys. Act. 2024, 21, 9. [Google Scholar] [CrossRef]
- Zborowski, M.; Skotnicka, M. The Role of Hydration in Children and Adolescents—A Theoretical Framework for Reviewing Recommendations, Models, and Empirical Studies. Nutrients 2025, 17, 2841. [Google Scholar] [CrossRef]
- Pastore, M.N.; Bonfiglio, C.; Tatoli, R.; Donghia, R.; Pesole, P.L.; Giannelli, G. Optimal Vegetable Intake for Metabolic-Dysfunction-Associated Steatotic Liver Disease (MASLD) Prevention: Insights from a South Italian Cohort. Nutrients 2025, 17, 2477. [Google Scholar] [CrossRef]
- Hidayat, K.; Zhang, L.-L.; Rizzoli, R.; Guo, Y.-X.; Zhou, Y.; Shi, Y.-J.; Su, H.-W.; Liu, B.; Qin, L.-Q. The Effects of Dairy Product Supplementation on Bone Health Indices in Children Aged 3 to 18 Years: A Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2023, 14, 1187–1196. [Google Scholar] [CrossRef]
- Wang, K.; Niu, Y.; Lu, Z.; Duo, B.; Effah, C.Y.; Guan, L. The Effect of Breakfast on Childhood Obesity: A Systematic Review and Meta-Analysis. Front. Nutr. 2023, 10, 1222536. [Google Scholar] [CrossRef]
- Jaeger, V.; Koletzko, B.; Luque, V.; Ferré, N.; Gruszfeld, D.; Gradowska, K.; Verduci, E.; Zuccotti, G.V.; Xhonneux, A.; Poncelet, P.; et al. Distribution of Energy and Macronutrient Intakes across Eating Occasions in European Children from 3 to 8 Years of Age: The EU Childhood Obesity Project Study. Eur. J. Nutr. 2023, 62, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Van Veen, M.R.; Van Hasselt, P.M.; De Sain-van Der Velden, M.G.M.; Verhoeven, N.; Hofstede, F.C.; De Koning, T.J.; Visser, G. Metabolic Profiles in Children During Fasting. Pediatrics 2011, 127, e1021–e1027. [Google Scholar] [CrossRef]
- Parmar, K.; Mosha, M.; Weinstein, D.A.; Riba-Wolman, R. Fasting Ketone Levels Vary by Age: Implications for Differentiating Physiologic from Pathologic Ketotic Hypoglycemia. J. Pediatr. Endocrinol. Metab. 2023, 36, 667–673. [Google Scholar] [CrossRef]
- Xue, H.; Maguire, R.L.; Liu, J.; Kollins, S.H.; Murphy, S.K.; Hoyo, C.; Fuemmeler, B.F. Snacking Frequency and Dietary Intake in Toddlers and Preschool Children. Appetite 2019, 142, 104369. [Google Scholar] [CrossRef]
- Fogel, A.; Goh, A.T.; Fries, L.R.; Sadananthan, S.A.; Velan, S.S.; Michael, N.; Tint, M.-T.; Fortier, M.V.; Chan, M.J.; Toh, J.Y.; et al. Faster Eating Rates Are Associated with Higher Energy Intakes during an Ad Libitum Meal, Higher BMI and Greater Adiposity among 4·5-Year-Old Children: Results from the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) Cohort. Br. J. Nutr. 2017, 117, 1042–1051. [Google Scholar] [CrossRef]
- Garg, D.; Smith, E.; Attuquayefio, T. Watching Television While Eating Increases Food Intake: A Systematic Review and Meta-Analysis of Experimental Studies. Nutrients 2025, 17, 166. [Google Scholar] [CrossRef]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose Tissue Inflammation and Metabolic Dysfunction in Obesity. Am. J. Physiol.-Cell Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef]
- Calcaterra, V.; Magenes, V.C.; Bianchi, A.; Rossi, V.; Gatti, A.; Marin, L.; Vandoni, M.; Zuccotti, G. How Can Promoting Skeletal Muscle Health and Exercise in Children and Adolescents Prevent Insulin Resistance and Type 2 Diabetes? Life 2024, 14, 1198. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Tang, Y.; Zhou, J.; Tian, Y.; Chen, F.; Li, G.; Huang, H.; Huang, H.; Zhou, L. Childhood Adiposity and Risk of Major Clinical Heart Diseases in Adulthood: A Mendelian Randomization Study. J. Am. Heart Assoc. 2024, 13, e035365. [Google Scholar] [CrossRef]
- Albornoz-Guerrero, J.; Zapata-Lamana, R.; Reyes-Molina, D.; Cigarroa, I.; García Pérez De Sevilla, G.; García-Merino, S. Overweight/Obese Schoolchildren with Low Muscle Strength Have a Lower Cardiorespiratory Capacity and Greater Cardiovascular Risk: Results of the School Health Survey of the Extreme South of Chile 2019. Children 2021, 8, 734. [Google Scholar] [CrossRef]
- Van Der Heijden, G.-J.; Wang, Z.J.; Chu, Z.; Toffolo, G.; Manesso, E.; Sauer, P.J.J.; Sunehag, A.L. Strength Exercise Improves Muscle Mass and Hepatic Insulin Sensitivity in Obese Youth. Med. Sci. Sports Exerc. 2010, 42, 1973–1980. [Google Scholar] [CrossRef]
- Berman, L.J.; Weigensberg, M.J.; Spruijt-Metz, D. Physical Activity Is Related to Insulin Sensitivity in Children and Adolescents, Independent of Adiposity: A Review of the Literature. Diabetes Metab. Res. Rev. 2012, 28, 395–408. [Google Scholar] [CrossRef] [PubMed]
- McGovern, C.; Rifas-Shiman, S.L.; Switkowski, K.M.; Woo Baidal, J.A.; Lightdale, J.R.; Hivert, M.-F.; Oken, E.; Aris, I.M. Association of Cow’s Milk Intake in Early Childhood with Adiposity and Cardiometabolic Risk in Early Adolescence. Am. J. Clin. Nutr. 2022, 116, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, X.; Xu, Y.; Yang, J.; Du, L.; Li, K.; Zhou, Y. Milk Consumption and Multiple Health Outcomes: Umbrella Review of Systematic Reviews and Meta-Analyses in Humans. Nutr. Metab. 2021, 18, 7. [Google Scholar] [CrossRef] [PubMed]
- Capra, M.E.; Stanyevic, B.; Giudice, A.; Monopoli, D.; Decarolis, N.M.; Esposito, S.; Biasucci, G. Long-Chain Polyunsaturated Fatty Acids Effects on Cardiovascular Risk in Childhood: A Narrative Review. Nutrients 2023, 15, 1661. [Google Scholar] [CrossRef]
- Strzelecka, I.; Łyszczarz, A.; Szpak, A.; Kolarzyk, E. Taste Preferences of Preschoolers and Parents’ Contribution to Shaping Their Children’s Eating Habits in the Context of Obesity Development. Ann. Agric. Environ. Med. 2022, 29, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Kao, T.-S.A.; Ling, J.; Vu, C.; Hawn, R.; Christodoulos, H. Motivational Interviewing in Pediatric Obesity: A Meta-Analysis of the Effects on Behavioral Outcomes. Ann. Behav. Med. 2023, 57, 605–619. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).