1. Introduction
Tuberculosis (TB), a preventable infectious disease caused by
M. tuberculosis, remains a major global health problem in Sub-Saharan Africa region (SSA). Prior to coronavirus disease 2019 (COVID-19) pandemic, TB has been the leading cause of death from a single infectious agent [
1]. In addition, a more recent report from the World Health Organization (WHO), covering more than 99% of the world’s population, stipulated that TB ranked second among leading causes of death from a single infectious agent in the year 2022 [
2]. Although some regions of the world have achieved substantial reduction of TB burden, the disease morbidity has increased in developing countries. According to the WHO, TB mortality was 1.6 million in 2022, whereas its prevalence was 10.6 million worldwide, with an increase of over 4% as compared with the previous year [
3,
4].
Because of the HIV pandemic, poverty, the movement of displaced people and the emergence of multi-drug-resistant strains, tuberculosis remains an enormous public health problem in developing countries. Moreover, a previous study showed that in most developing countries, HIV pandemics, diabetes, malnutrition, alcoholism, smoking, contact with active TB, extreme poverty and homelessness are common risk factors identified in relation to TB [
8]. Tuberculosis has been identified as an important cause of morbidity and mortality in Gabon.
In the Republic of Gabon, TB remains a major public health challenge, with Libreville, the capital town, bearing the heaviest burden in the country. Despite international support by the Global Fund, the Gabonese National Tuberculosis Program (NTP) faces various challenges, including low TB detection and low treatment success rates. In 2021, TB detection rate was 42% and the treatment success rate was 57%. Moreover, the HIV positive rate among TB patients was 29%; however, according to the 2022 national TB program of Gabon (NTP) annual report, only one third of TB patients have undergone HIV testing [
5].
A prospective, cross-sectional study on the prevalence of Pulmonary Tuberculosis and Associated Factors among Patients Admitted in the biomedical analysis laboratory of the Amissa Bongo University Hospital Center in Franceville in Gabon showed an overall prevalence rate of 31.72% (98) among 309 patients. The results of the study showed that the prevalence of pulmonary tuberculosis was greatest among males in Franceville and the surrounding area. There were 40 women or 40.82% (95% CI: [0.30 - 0.51]) and 58 men or 59.18% (95% CI: [0.48 - 0.69]). Concerning the risk factors, the 15 - 49 age group, fever, alcohol consumption, smoking, HIV infection, chest pain, night sweats and cough were significant for pulmonary tuberculosis. Consequently, screening for tuberculosis in HIV-positive patients, public awareness and community mobilization should be encouraged This study was conducted of the Amissa Bongo Regional University Hospital in Franceville from 19 June 2021 to 22 January 2022 [
6].
Given the fact that 78% of Gabonese cases were detected in Libreville in 2022, it seemed to be worthful to analyze the spatial distribution and identify the hotspots. Spatial epidemiological studies are increasingly recognized as critical tools for enhancing tuberculosis (TB) program management.
The spatial epidemiology in Tb control can help to identifying geographic hotspots and enabling targeted intervention in areas with the greatest need. Detecting emerging hotspots can trigger rapid response mechanisms. This helps also to understanding transmission dynamics as tuberculosis often spread within household or communities, leading to heterogeneous spatial patterns. By mapping TB burden, health authorities can optimize the placement of diagnostic centers, treatment facilities, and outreach programs. Spatial tools allow for real-time surveillance and trend analysis, helping programs assess the impact of interventions over time. Spatial data can reveal inequities in healthcare access, such as underserved rural or peri-urban areas, guiding efforts to improve universal health coverage. Instead of one-size-fits-all approaches, spatial epidemiology supports precision public health.
It is why the epidemiological surveillance advances search strategies for respiratory symptoms, not only at home but also in social spaces. Spatial analysis, which considers the time and space of diseases, is a useful tool for epidemiological surveillance. [
7].
The question was to know if the tuberculosis cases are homogenously disseminated in Libreville, or they are clustered in some areas. This work aimed to represent the geographical distribution of incident TB cases occurring in Libreville 2022, and MDR-TB cases as well, and identify hotspots areas to inform targeted interventions.
2. Methods
2.1. Design and Settings
This was a descriptive cross-sectional and eco-epidemiological study conducted in Libreville, the capital town of the Republic of Gabon. Gabon has an estimated population of 2,344,720 as of 2022.
In the Gabonese health system, the country is divided into 10 Health Regions, including Libreville (LBV), Ouest, Sud-Est, Centre, Centre-Sud, Sud, Est, Centre-Est, Maritime and Nord region. Libreville is the most populous province, accounting of 44% (1,029,977 inhabitants) of the entire country population.
Libreville is known as the Health Region with highest TB burden in Gabon. This region had detected almost 78% of all Gabonese tuberculosis cases in 2022. Thus, it was selected as the study site. The study covers all new susceptible TB and multidrug-resistant TB (MDR-TB) cases diagnosed in Libreville from January1st through December 2022.
The Libreville Health Region had 12 TB diagnosis and care centers located in hospitals and clinics, namely Nkembo, Hiaobo, HIAA, CHUL, CTA CHUL, PCL, CTA Nkembo, Chumje, PLIST, Nvolane, CS Nzeng-Ayong, and Clinique Privee Pasteur. Almost 98% of tuberculosis cases recorded in Libreville in 2022 were detected in Nkembo and CHUL health centers. Thus, they were selected as the study sites.
2.2. Ethical Consideration, Data Collection and Analysis
All data used in this study are from TB monitoring and surveillance in Gabon; they are anonymous. Thus, informed consent was not required. Study data consisted in medical records from TB treatment centers located at selected health facilities in Libreville.
Ten M&E staff from the NTP were briefed on data collection. Collected data were scanned, then transcribed in prepared excel sheet to create the study database which is available at the Tuberculosis National Programme, Monitoring and evaluation department. Only the 2022 period data coming from Nkembo and CHUL health centers were included in the study.
TB incidence was calculated for the year 2022 at national and regional (Libreville) levels. Furthermore, data were transferred to and analyzed with the use of Q.GIS software (The Ingenuity Centre, Global Geo-Intelligence Solutions Ltd., University of Nottingham), with the technical support of the Gabonese Agency for Space Studies and Observations (AGEOS). Satellite images were developed with the use of a geographic information model.
3. Results
3.1. Incidence of Tuberculosis in the Republic of Gabon and Libreville in the Year 2022
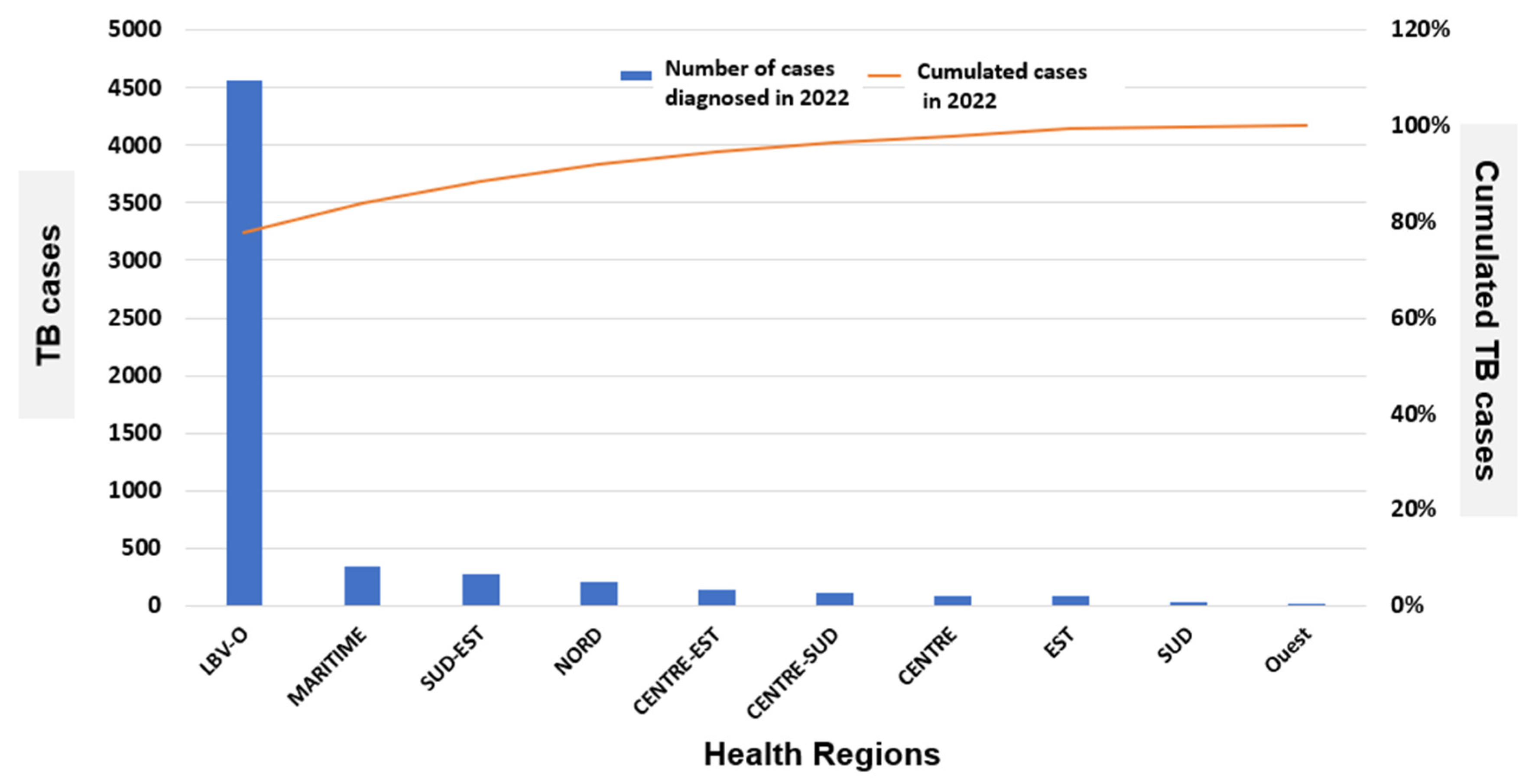
Figure 1 shows the distribution of TB cases nation-wide and in Libreville in the year 2022. At national level, there were 5,850 TB cases diagnosed, for an annual incidence of 509 per 100,000. In Libreville-Owendo health region, there were 4,560 cases diagnosed in 2022, representing 77.9% of all cases. The remaining 290 TB cases (22.1%) were diagnosed in the other Gabonese Health Regions (
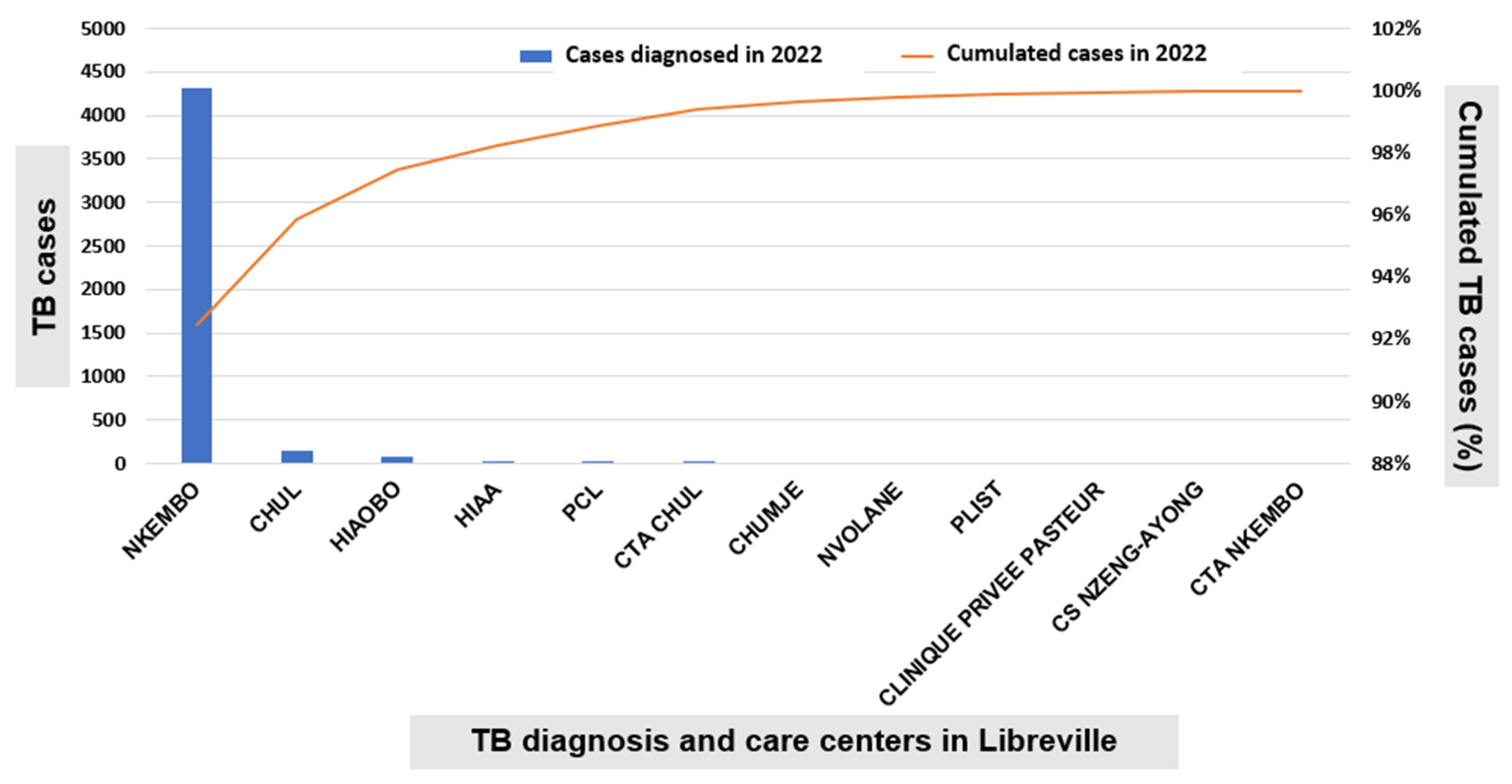
Figure 1). In Libreville, markedly higher number of new TB cases was observed at Nkembo diagnosis and care center, 4,309 out of 4,560 cases (94.5%); followed by CHUL, 157 cases (3.4%) and Hiaobo, 76 cases (1.7%). Other TB diagnosis and care centers of the capital town accounted for less than 50 cases, including HIAA, PCL, CTA Nkembo, Nvolane, CS Nzeng-Ayong, etc. (
Figure 2).
Furthermore, given that approximately 98% of TB cases reported in Libreville in the year 2022 were diagnosed at two health settings that organized TB services, namely Nkembo and CHUL, only those data (cases) were considered and analyzed using Q.GIS software. The latter was used to produce the geographical distribution of TB and MDR-TB cases according by county of residence of the patients.
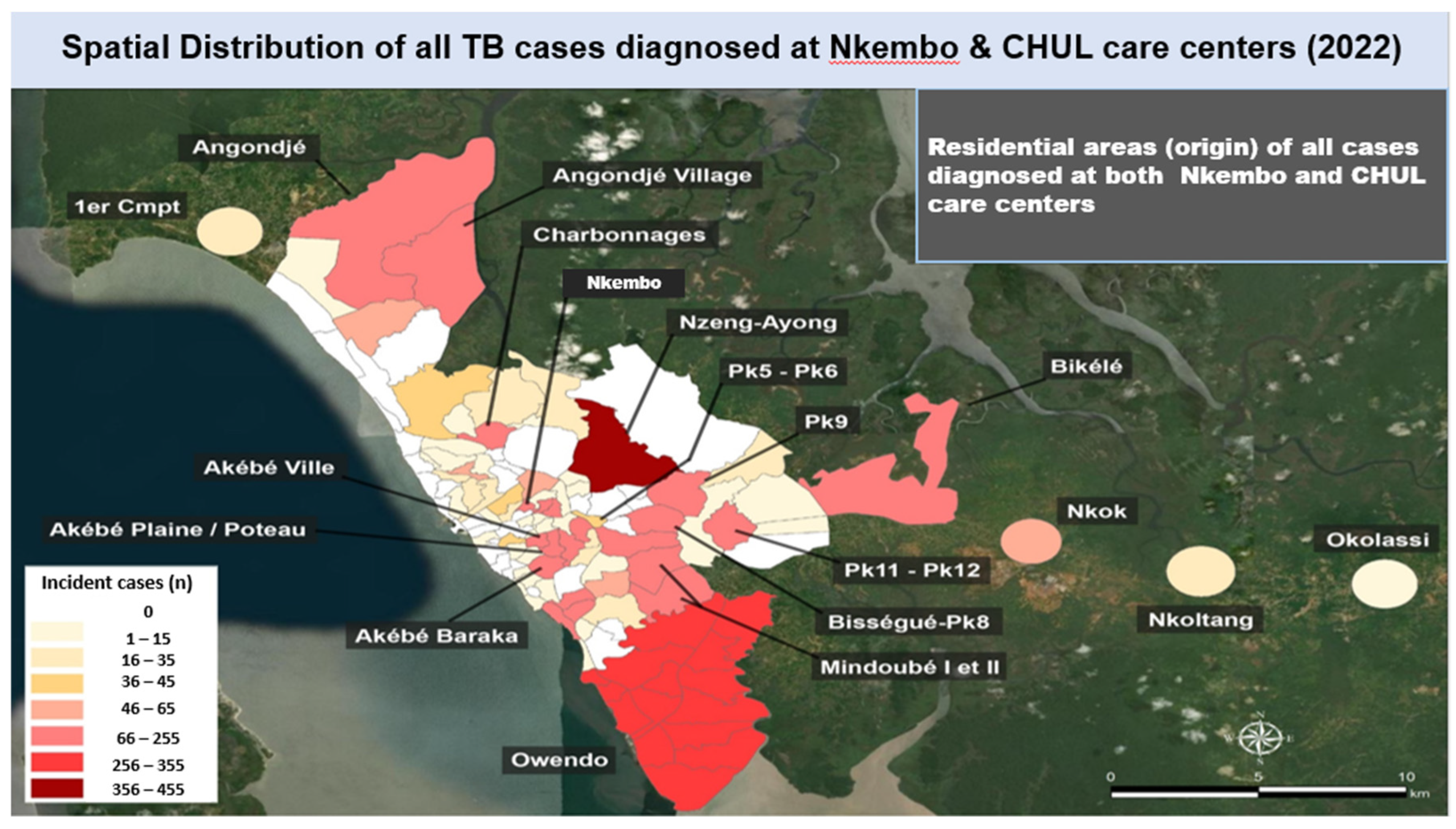
3.2. Spatial Distribution of TB Cases Diagnosed in 2022 in Libreville
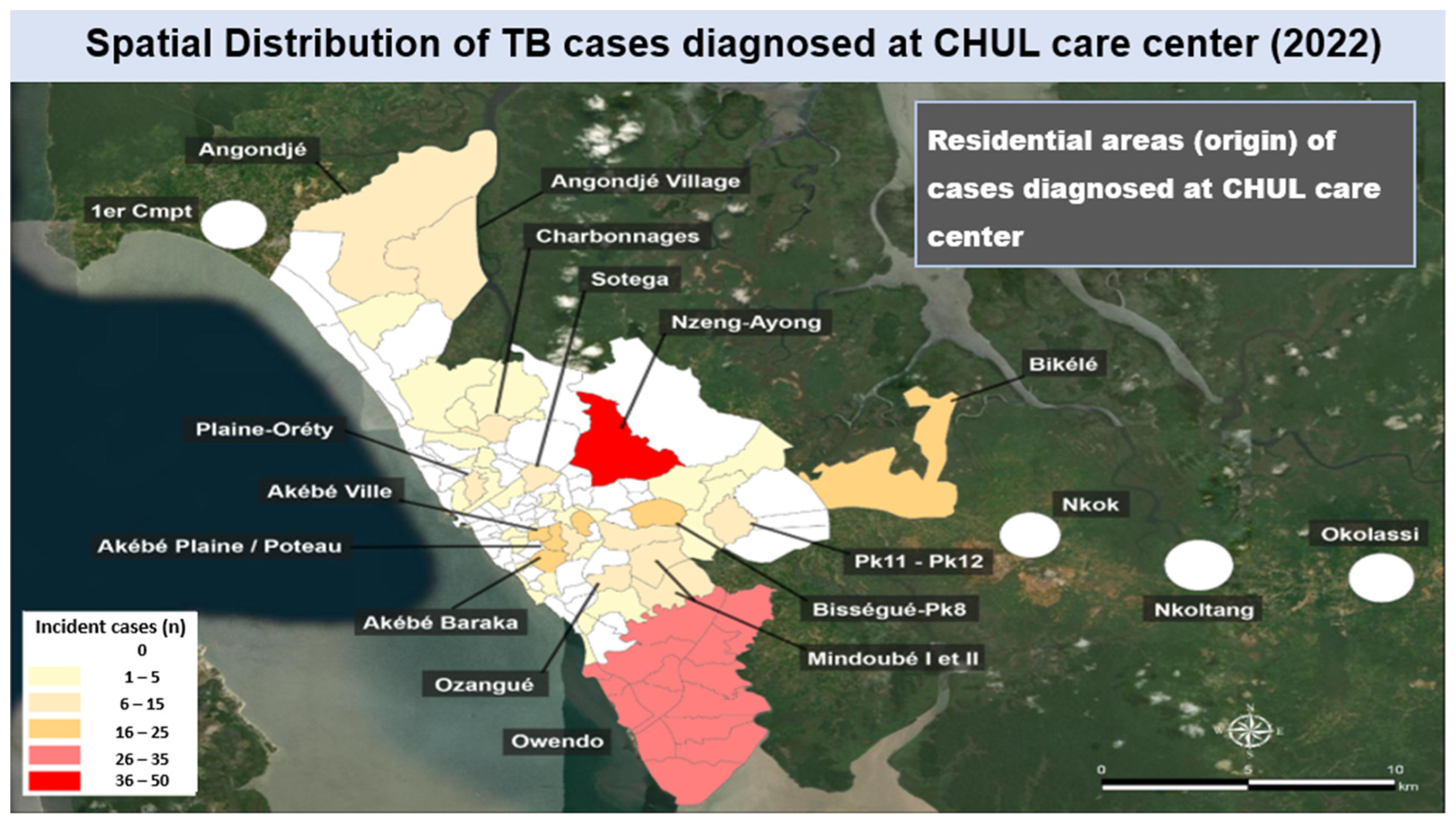
Spatial mapping of incident cases by county of residence showed that a large majority of the TB cases diagnosed at CHUL care center in 2022 were from Nzeng-Ayong county (range: 36 -50 cases) and Owendo (range: 26-35 cases) (
Figure 3); other TB cases originated from counties having less that accounted for less than 26 cases of patients who visited CHUL care center, such as Bikele, Bissegue-Pk8, Akebe Ville, Akebe Baraka, Ozangue, Sotega, Plaine-Orety, Charbonnages, Angondje, Angondje village, etc.
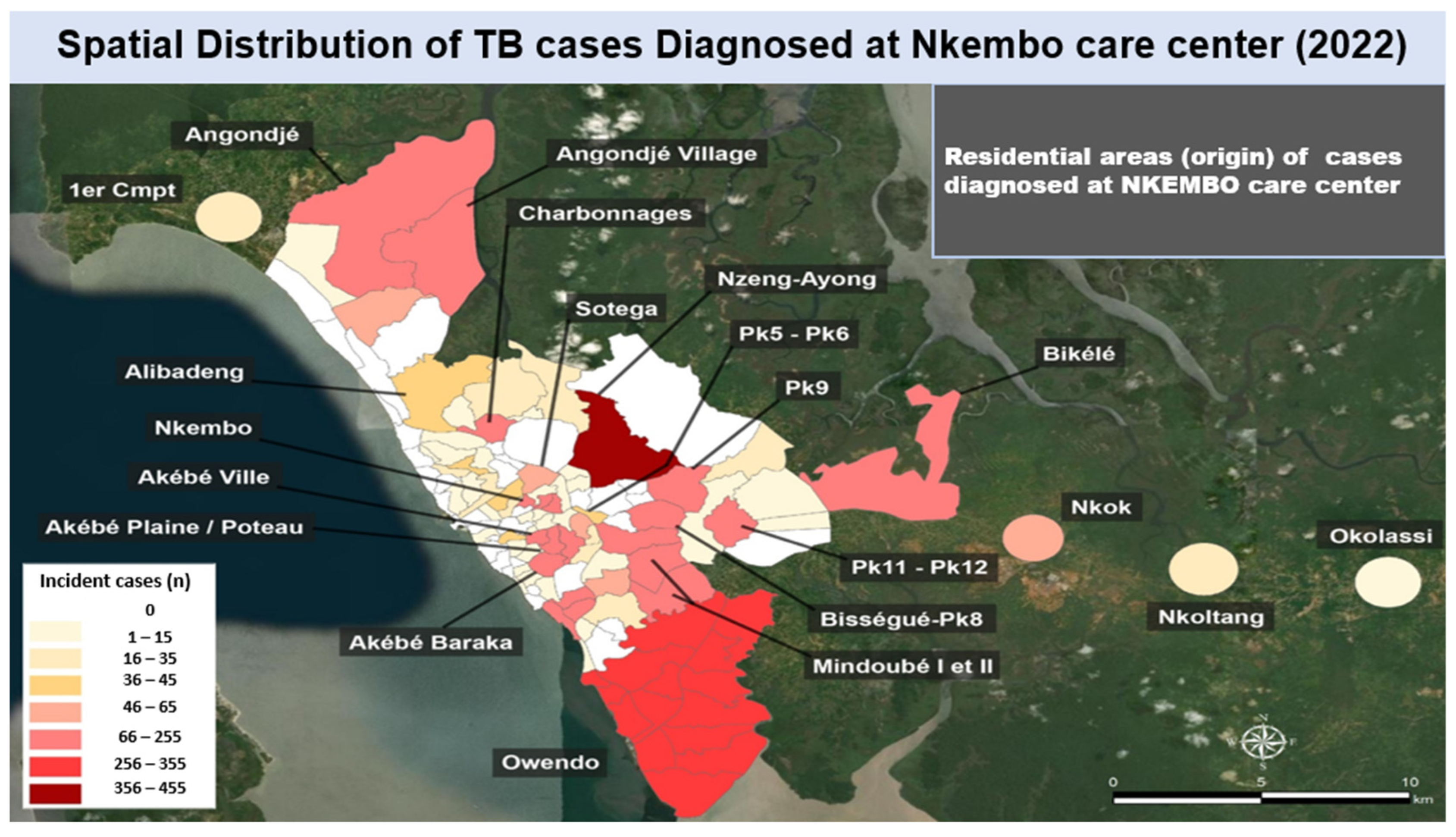
When considering TB cases diagnosed at Nkembo care center, markedly higher number of TB patients were from Nzeng-Ayong county (range: 356-455 cases), Owendo (range: 256-355 cases), followed by Nkembo county, Akebe ville, Akebe Baraka, Akebe Plaine/plateau, Angondje, Angondje village, Charbonnages, Bikele, Pk11, Pk12, Pk9, Mindoube I, Mindoube II (66-255 cases), Sotega and Nkok (46-65 cases). Other counties accounted for less than 45 TB cases, (
Figure 4 and
Figure 5).
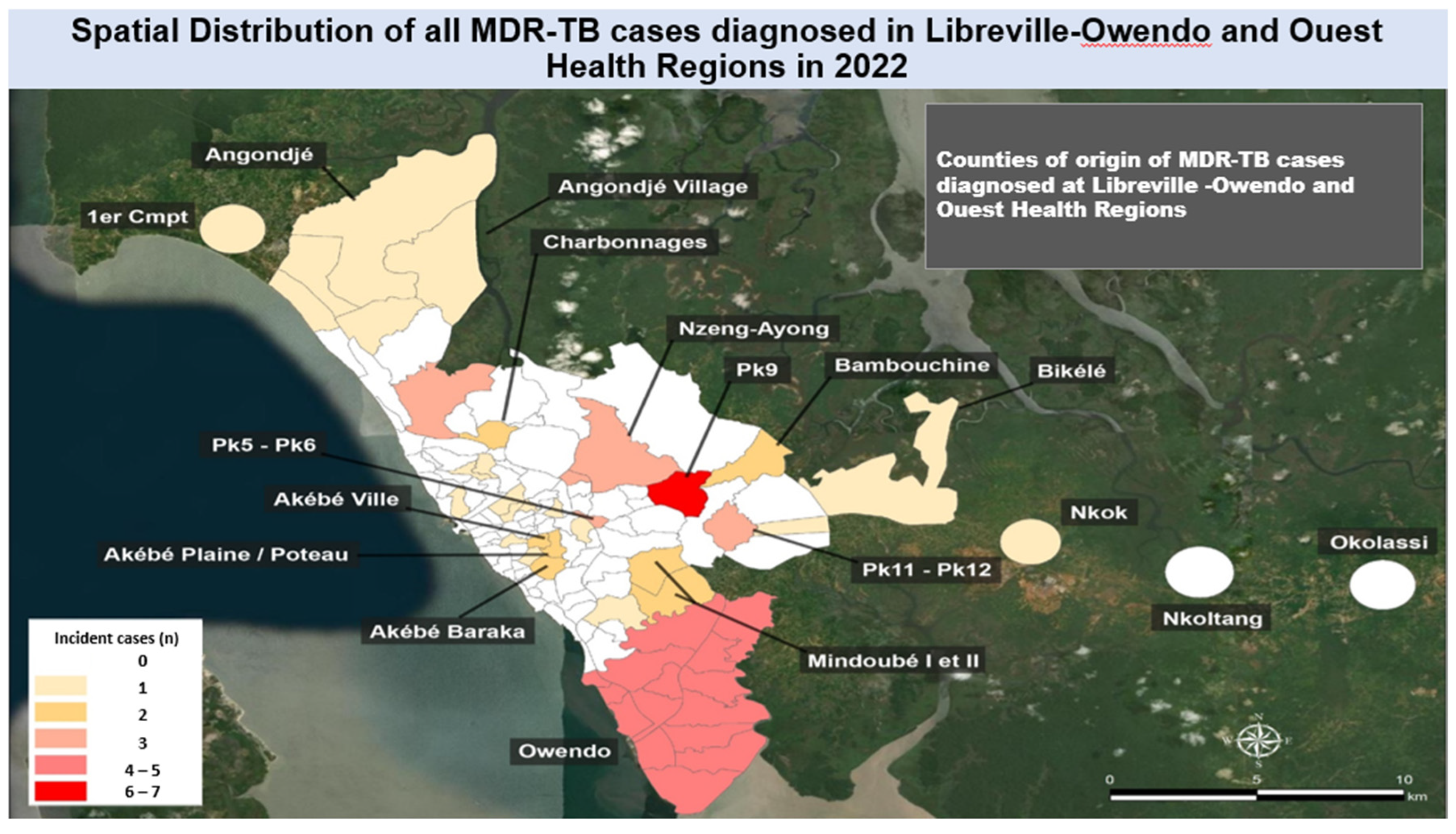
3.3. Distribution of Multi-Drug-Resistant Tuberculosis Cases in Libreville in 2022
Of all 66 newly diagnosed MDR-TB cases nationwide in 2022, Libreville accounted for 62.1% (41 cases) of them, for an annual incidence of 26.7 per 100,000. The mapping of all cases from Libreville showed that a relatively higher number of MDR-TB cases were from Pk9 county, which accounted for 14.6% (6 cases) of the cases, followed by Owendo, 9.7% (4 cases). The other counties of the capital Libreville accounted for less than 4 MDR-TB cases, including Nzeng-Ayong, Charbonnages as shown in
Figure 6.
4. Discussion
Findings
This work searched to identify high disease burden areas and perform the spatial mapping of TB and MDR-TB cases diagnosed in 2022 in Libreville, Republic of Gabon, in order to enhance national strategies for TB control. It was observed that the capital Libreville had the highest number of new TB cases; and most of the cases were diagnosed at Nkembo and CHUL treatment centers. Geographically, new susceptible TB cases were highly concentrated at Nzeng-Ayong and Owendo counties.
The work showed also that the majority of TB-MDR were from Pk9 county and Owendo. The emergence of MDR-TB hampers the efforts to control TB [
6], particularly in TB endemic countries such as those in the WHO central Africa subregion, including the Republic of Gabon.
The Republic of Gabon is known as one of the high-burden countries not only for TB but also for MDR-TB, which has triggered efforts to establish both molecular surveillance and clinical care capacity nationwide in recent years [
8,
9,
10]. In Gabon, resistance to Rifampicin has been estimated to be 33% among newly infected patients [
11]. Other previous studies have shown that resistance to fluoroquinolone medication is due to gyrase (gyrA) mutations in this central African country. The presence of gyrA mutations in a TB patient helps to predict not only the presence, but also the level of fluoroquinolone resistance, which allows care givers to adapt the drug regimen to Mycobacterium tuberculosis strain that causes individual infection [
12].
Our study showed that Libreville had the highest MDR-TB incidence in 2022. The distribution of new MDR-TB cases within Libreville in 2022 according to area of residence showed that most cases were from Pk9, followed by Owendo, Nzeng-Ayong and Charbonnages counties.
A nationwide retrospective study that analyzed aggregate TB data (2014-2021) in Gabon showed high prevalence of MDR-TB, and most patients were young (25-35 years) [
13] Another study by Assiana and colleagues [
14] in 2020, showed a relatively high MDR-TB prevalence of 379 cases per 100,000 in the Gabonese population.
Explaining Factors
According to the programme review report organized in 2020, Gabon was among the two countries with the highest tuberculosis incidence in the Central Africa subregion. But the programmatic performance was low as seen above.
This study case in Libreville is showing the limited decentralization of tuberculosis program since 98% of patients are caring by the two health facilities. The report mentioned that Libreville had only four (4) tuberculosis diagnostic and treatment centers for near than 1 million inhabitants. This means that 250,000 individuals covered by health center. It is too high since WHO was recommending 50000-100000 by health facility. The small number of tuberculosis health facilities and the hospital centric health system in Gabon are the factors explaining why the patients residing in Nzeng Ayong, Owendo and PK9 were obliged to come to Nkembo and CHUL health centers to reach out tuberculosis care.
Giving the socio-determinants factors in Gabon, the WHO Global report identified four factors which were HIV, alcohol use disorders, undernutrition and diabetes in total of 6310 new tuberculosis cases in 2022. From them, HIV was accounting for more than half new tuberculosis cases (3600) followed by alcohol for a quarter of tuberculosis cases (1500). The remaining 1210 new tuberculosis cases were divided between undernutrition and diabetes. In the overcrowded counties with a high level of poverty, like Nzeng Ayong, Owendo and PK9, undernutrition, HIV and alcohol use disorders are commun. Those risk factors can explain why tuberculosis is most prevalent in these counties. Nzeng-Ayong and Owendo have been reported to be characterized by poverty, which may justify, at least partially, the high TB incidence in those areas.
The same no-published study was conducted in Cameroon in 2022, especially in Yaoundé and Douala cities. Almost 8000 tuberculosis cases folders were gathered in 62 health facilities. The quarter of them were from Laquintinie hospital (1110) in Douala and Jamot hospital (930) in Yaounde. The same methodology was used. And the result showed that hotspots areas were the overcrowded areas with high-risk behavior for sexual and alcohol use disorders. The study was conducted by the National Tuberculosis Program with the WHO support. The aim was to identify the hotspots areas and strengthen public health interventions, including the community involvement. The hotspots areas found were Nkomkana, Awae, Odza in Yaounde and Newbell and Boko in Douala. These are all the overcrowded areas. Moreover, there is a prison in Nkomkana [
15].
In the hotspot’s areas, some relevant interventions can be implemented, such as the community awareness campaigns followed by the community testing. For this, DRC’s NTP had used the combination of computed assisted X-ray and GeneXpert for the suspected tuberculosis cases. The results were impressive. These campaigns involve community-based strategies, including door-to-door screening and education by community relays, mobile screening units, and community health posts [
16]. Another intervention is to set up a tuberculosis diagnosis and treatment service in the county’s health facility. In the first time, this health facility can be responsible of treatment while waiting for some equipment for diagnosis. In the meantime, it is recommended to strengthen community support to fight against stigma and discrimination in those kinds of areas.
To improve these kinds of studies, it is better on the first hand to initiate operational research on the outcomes of the intervention implementations in the hotspot’s areas as done in DRC [
17]. On the other hand, it is preferable to conduct an observational cohort-study to follow the diagnosed tuberculosis cases in the timely manner in their original counties. So, we can get a real-time case tracking.
Spatial Tuberculosis Surveillance
Given this and the higher risk of development of disease a few months after infection, many active case-finding strategies focus on the screening of close contacts of the index case, such as people living in the same household, coworkers or school classmates. These strategies have a two-fold purpose—they contribute to early diagnosis of the disease (among contacts of the index case) and identify healthy individuals who can benefit from TB preventive therapies. Taken together, these strategies significantly prevent many TB cases from happening.
Considering the study done by D. Nguema, the spatial analysis highlighted the surprising variability in TB incidence rates (for all cases and in those smear-positive) at the ward level (up to 10 times differences in some wards compared to others). [
18].
Descriptive epidemiological analysis coupled with geographic surveillance is meaningful if the results can be translated into concrete actions or interventions such as targeted case finding, preventive strategies in high-transmission areas.
For National TB Programs to realize this benefit at scale, they should consider routinely collecting and analyzing spatial variables for patients screened, tested and treated for TB so that this information can be woven into real-time TB surveillance platform.
A similar study [
7] was conducted in the municipality of Belém, Pará, in Brazil using data on 1,134 new cases of TB diagnosed in individuals aged ≥60 years from 2011 to 2015.The data were analyzed using SaTScan software. The analysis of the spatiotemporal dynamics of TB in the municipality showed that the high-risk areas included the most densely populated neighborhoods, highlighting the priority of these areas for disease control measures. Spatial analysis can be used to guide more effective interventions according to the characteristics of the location and the local population.
Strengths and Limitations
The current study is strengthening the need to integrate the spatial surveillance in the tuberculosis programme implementation. Clearly, the study has identified the hotspots counties in Libreville and will help the NTP to be more efficient in the resources allocation to handle the disease burden.
The current study is limited by the retrospective methodology used to collect data. It is preferred to get the spatial data on a progressive manner. This can help to implement specific interventions on the same time. Geo-referenced data can be populated right after the diagnosis establishment.
Suggested directions for future research are delve deeper into the public health implications of these findings. This involves analysis from socioeconomic, environmental, population density, and healthcare accessibility perspectives.
5. Conclusion
This work consisted in mapping TB and MDR-TB cases in Libreville and provides valuable insights into the spatial distribution of the disease, revealing that Nzeng-Ayong and Owendo counties were the high TB morbidity burden areas, whereas Pk9 was the hotpots of MDR-TB in Libreville.
The findings call for the PNLT to prioritize public health interventions in these areas to improve case detection, treatment adherence, and ultimately, to reduce the burden of TB and MDR-TB in Libreville. Further investigations are indispensable to determine other possible factors that might elucidate the increased TB morbidity in Libreville.
Author Contributions
CMM and FL designed the fieldwork; SMG and FL collected the data; NRN, MNM and JLN analyzed and interpreted the data; CMM, NRN, GNA and NM drafted the manuscript; CMM, TH and JLN proofread the manuscript.
Availability of data
Data collected belong to the Gabonese National Tuberculosis Program, and related information can be obtained upon request to the authors (FL, CMM, NRN).
Ethical approval and consent to participate
No applicable.
Consent for publication
All authors read the final version of the manuscript and agreed for its publication.
Acknowledgments
The authors would like to thank all the staff of WHO-Libreville office and National Tuberculosis Program, Gabon.
Conflicts of Interest
The authors have no conflict of interest.
References
- Lange C, Dheda K, Chesov D, Mandalakas AM, Udwadia Z, Horsburgh Jr CR. Management of drug-resistant tuberculosis. The Lancet 2019; 394(10202): 953-966. PMID: 31526739. [CrossRef]
- The World Health Organization. Global tuberculosis report 2023. Available from:Global Tuberculosis Report 2023 (who.int).
- Park PG, Fatima M, An T, Moon YE, Woo SK, Youn H et al. Current development of therapeutic vaccines for the treatment of chronic infectious diseases. Clin Exp Vaccine Res. 2024; 13(1): 21-27. PIMD: 38362373. [CrossRef]
- National tuberculosis program (PNLT). Rapport annuel 2022 (report in French, unpublished).
- National tuberculosis program (PNLT) Report. Review of the national tuberculosis program (PNLT), 2022 (report in French, unpublished).
- Thiéry Ndong Mba et al, Prevalence of Pulmonary Tuberculosis and Associated Factors among Patients Admitted to the Amissa Bongo University Hospital Center in Franceville, Gabon; Journal of Biosciences and Medicines, 2023, 11, 160-173;. [CrossRef]
- Mesquita CR et al., Spatial analysis studies of endemic diseases for health surveillance: Application of scan statistics for surveillance of tuberculosis among residents of a metropolitan municipality aged 60 years and above; Ciência & Saúde Coletiva, 26(Supl. 3):5149-5156, 2021;. [CrossRef]
- Zhong Y, Xie H, Cai F, Liu M, Gan H, Tang Z et al. Global burden of multidrug-resistant tuberculosis in children and adolescents. Pediatr Res. 2025 (article In Press); [CrossRef]
- Bélard S, Remppis J, Bootsma S, Janssen S, Kombila DU, Beyeme JO, et al. Tuberculosis treatment outcome and drug resistance in Lambaréné, Gabon: a prospective cohort study. Am J Trop Med Hyg. 2016; 95: 472–480.
- Agbo Abdul JBPA, Adegbite BR, Ndanga MED, Edoa JR, Mevyann RC, Mfoumbi GRAI et al. Resistance patterns among drug-resistant tuberculosis patients and trends-over-time analysis of national surveillance data in Gabon, Central Africa. Infection 2022; 51(3): 697-704.
- Kombila UD, Boulingui CM, N’gomanda F, Mavoungou JVM, Ngea Epossi CBH, Bivigou N et al. Pre-extensively and extensively drug-resistant tuberculosis in Libreville, Gabon (published in French). Revue des Maladies Respiratoires 2024; 41(8): 542-548.
- Global tuberculosis report 2021. Geneva: World Health Organization; 2021. Available at: Global tuberculosis report 2021 (accessed on 2025/06/30).
- Kabir S, Tahir Z, Mukhtar N, Sohail M, Saqalein M, Rehman A. Fluoroquinolone resistance and mutational profile of gyrA in pulmonary MDR tuberculosis patients. BMC Pulm Med. 2020; 20: 138.
- Abdul AJBPA, Adegbite BR, Ndanga MED, Edoa JR, Mevyann RC, Mfoumbi GRAI et al. Resistance patterns among drug-resistant tuberculosis patients and trends-over-time analysis of national surveillance data in Gabon, Central Africa. Infection 2023; 51(3): 697-704. PIMD: 36307576. [CrossRef]
- Assiana DOE, Abdul JBPA, Linguissi LSG, Epola M, Vouvoungui JC, Mabiala A et al. Epidemiological profile of multi-drug resistant and extensively drug-resistant Mycobacteriun tuberculosis among Congolese patients. Ann Clin Microbiol Antimicrob. 2021; 20(1): 84.
- 2022; 16. WHO, Incidence and Spatial Mapping of Tuberculosis and Multidrug-resistant Tuberculosis in Cameroon, in 2022 (unpublished report).
- 20 November; 17. USAID, Improving Early Tuberculosis Detection in the Democratic Republic of Congo, USAID MEDICINES, TECHNOLOGIES, AND PHARMACEUTICAL SERVICES (MTAPS) PROGRAM, November 2023.
- D. NGUENHA and all, Spatial epidemiology for tuberculosis surveillance: a relevant add-on to routine surveillance. INT J TUBERC LUNG DIS 23(3):278–279 Q 2019 The Union. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).