1. Introduction
Verrucous carcinoma is a rare, well-differentiated squamous cell carcinoma(SCC) manifested as an exophytic or papillary projection usually on a mucosal surface [
1].
This tumor is generally recognized as a low-grade malignancy, slow progression, local invasiveness, and low incidence of metastasis. Extraorally, it can occur in any part of the body, a common site being the anogenital region [
2]. Intraorally, the gingiva and buccal mucosa are the common site. Verrucous carcinoma of the lip is clinically quite rare and only several cases of that were reported in the world, diagnosed in only 1 to 3 of every 1,000,000 persons each year [
3].
In contrast, Verruca, a squamous cell papilloma, is a common skin disease with a low recurrence rate even with simple treatment. It typically presents as a soft, pedunculated mass supported on a stem or stalk, with numerous finger-like projections. These projections may vary in length and shape, depending on the accumulation of keratin, a skin-forming protein, around the lesion. Conservative surgical excision, which removes both the head and the base of the lesion, may be performed if treatment is indicated, with recurrence being unlikely.
While malignant transformation from benign verruca is rare, if symptoms do not improve with continuous treatment, surgical removal may be recommended, with subsequent histopathological examination after excision, typically involving a referral from dermatology to plastic surgery.
It's important to note that oral papillomas that show poor response to adequate treatment for more than 3 months should raise suspicion of verrucous carcinoma. In such cases, prompt management of the tumor is essential.
There was a case where a patient initially diagnosed with verruca based on tissue examination was later found to have verrucous carcinoma through surgically excisional biopsy. This underscores the importance of performing complete excisional biopsy of the lesion to avoid the potential misdiagnosis of a benign tumor and subsequent incorrect treatment. Additionally, we report an unusual case of verrucous carcinoma of the lower lip.
2. Case Description
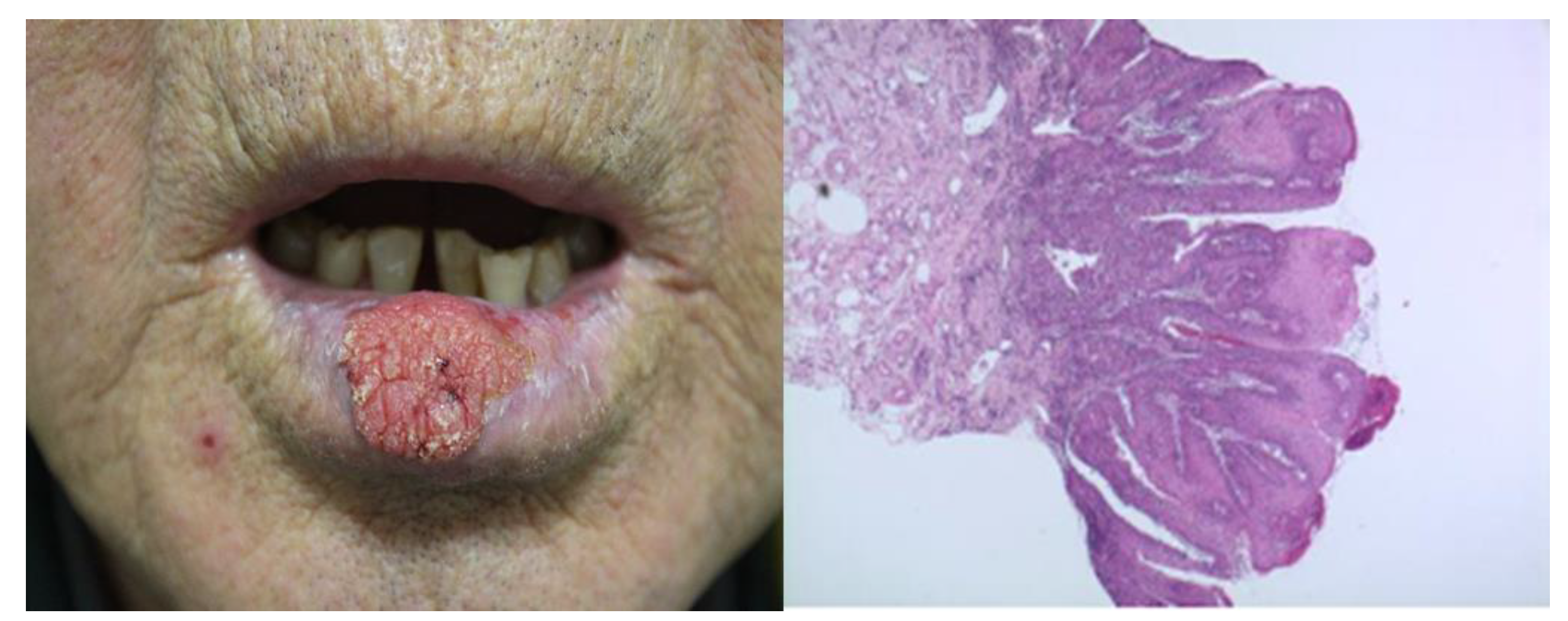
A 75-year-old male patient presented to our department with a tumor on the lower lip, initially diagnosed as a verruca based on a punch biopsy (
Figure 1). However, its size increased after repeated cryotherapy over the course of a year. On physical examination, a cauliflower-shaped exophytic asymptomatic lesion measuring 2.5 cm × 1.7 cm was ob-served in the middle portion of the lower lip (
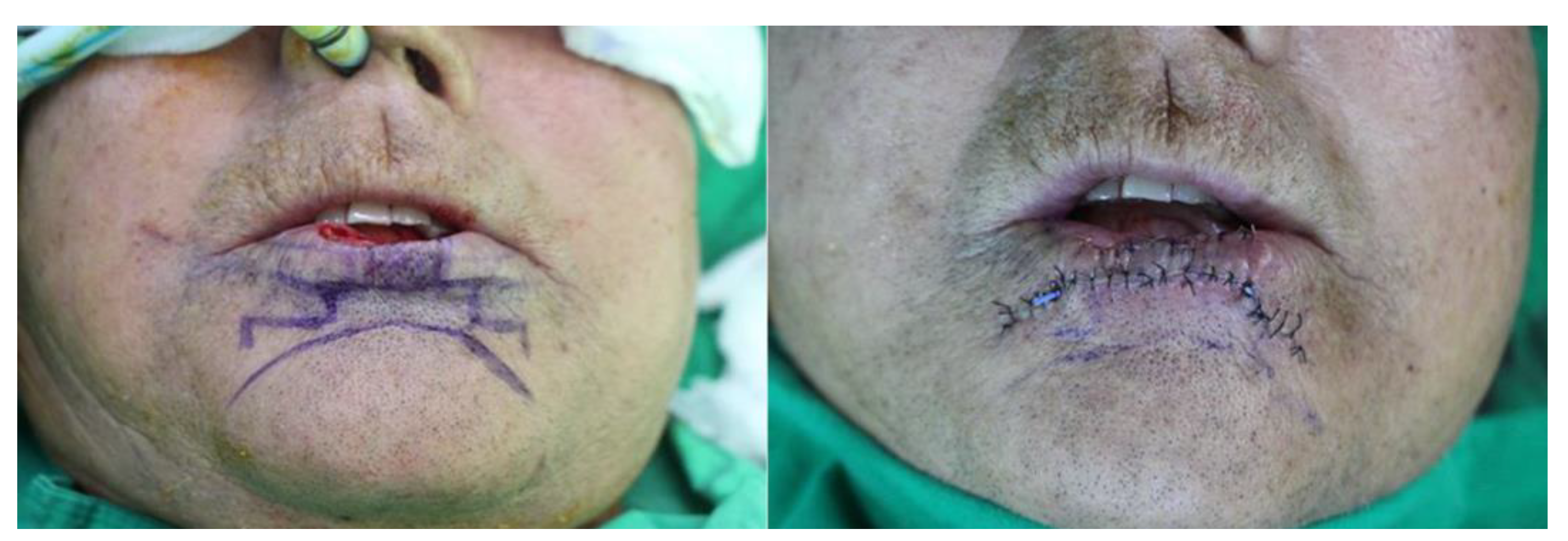
Figure 2). We planned surgery, believing it was not a simple benign lesion. The patient underwent with general anesthesia and na-sotracheal intubation. Frozen biopsy was performed, and the initial result showed a sus-picious lesion in the 9 o'clock direction, indicating potential cancer. Consequently, exten-sive excision was performed, including a safety margin, resulting in a negative margin. This resulted in approximately a 3cm x 2cm defect, unilateral for lateral defects and bilat-eral for central defect. Reconstruction was performed using the step ladder advancement flap technique, which facilitated the restoration of the lip in cases where more than 2/3 of the lip was affected. The procedure involved the excision of two small rectangles situated in a stair-step design, descending from medial to lateral at a 45-degree angle from either side of the base of the defect. Typically, stairs can consist of 2-4 segment. A design with two segments was chosen, and the width of the stairs was adjusted to match the size of the defect. During dissection, it is crucial to avoid the labial artery, and the flap was de-signed to avoid the labiomental crease to preserve the aesthetic unit. Once dissected, the flap was transposed to cover the defect, reaching only the subcutaneous tissue and skin. Subcutaneous tissue repair was performed using vicryl 5-0 and 6-0, while skin repair was done using black silk 6-0 (
Figure 3).
We maintained a full liquid diet for 2 days and applied ointment without dressing due to the lesion's location. As no other complications such as bleeding or hematoma occurred, the drain was removed. A soft diet was initiated after 3 days. All stitches were re-moved, and the patient was discharged after 7 days.
3. Results
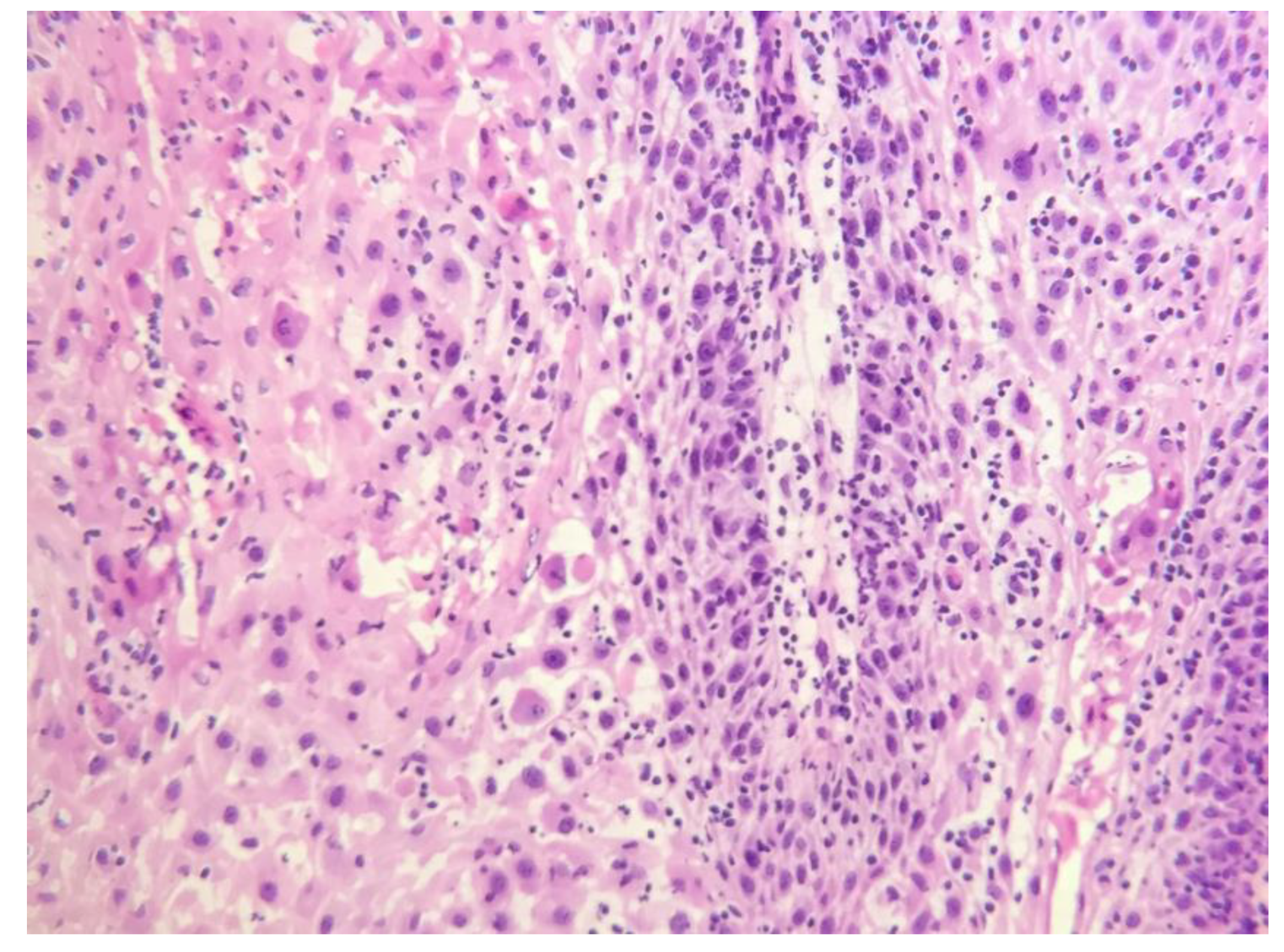
Histopathological examination of the specimen from the permanent biopsy revealed a proliferation of well-differentiated epithelium with minimal atypia at the epithelial connective tissue interface (
Figure 4). Cleft-like spaces lined by a layer of parakeratin extended from the surface deep into the lesion. These findings were consistent with verrucous carcinoma.
Clinical follow-up indicated complete healing of the lesion, with oral competence observed and no recurrence or complications noted at the 18-month follow-up (
Figure 5).
4. Discussion
Verruca, a squamous cell papilloma, is caused by infection with the human papillomavirus (HPV). The HPV subtypes most often found in oral squamous cell papilloma are HPV-6 and HPV-11. These subtypes are not associated with malignancy or precancer [
4]. When the papillomas are found on the skin they are more commonly referred to as warts or verruca. Squamous cell papillomas may also occur on many other parts of the body.
Oral papillomas are painless and may be left untreated. They appear not to change in size, spread to other parts of the oral cavity, or turn into malignant tumors. If treatment is indicated then conservative surgical excision that removes the head and the base of the lesion may be performed. Recurrence is unlikely. The exact etiology of the condition is unknown, though it is associated with human papillomavirus infection, chronic infection, traumatic scars, tobacco, and chemical carcinogens [
5].
If a verruca is identified as a benign tumor, appropriate treatments such as cryo-therapy should lead to symptom improvement. However, if there is no response to continuous treatment and the lesion persists or recurs in the same area, it is important to consider the possibility of malignancy, and a surgical biopsy may be necessary for diagnosis [
6,
7].
Verrucous carcinoma is a subtype of well differentiated squamous cell carcinoma. This tumor is distinct in its slow growth and no metastatic potential [
8]. But this lesion can be locally destructive despite its deceptively benign clinical behavior if not treated [
9]. It is predominantly seen in elderly males over the sixth decade [
10,
11]. This tumor may occur in several locations in the head and neck with the most common sites being the oral cavity (55.9%) [
12]. Because it is unusual and can be difficult to diagnose, the treatment may be delayed. Verrucous carcinoma is usually exophytic papillary in nature with pebbled surface. But it may always not appear as typical appearance.
The etiology of verrucous carcinoma is not completely established, although a few studies have shown an association with prior injuries, scars, and chronic inflammation [
13,
14]. Tobacco use, including snuff, is also associated with the development of verrucous carcinoma. Human papillomavirus (HPV) has also been implicated as a cause of verrucous carcinoma [
15]. Therefore, clinically suspecting verrucous carcinoma warrants obtaining a smoking history, inquiring about previous medical conditions, and considering HPV virus testing to aid in diagnosis.
Microscopically this tumor is characterized by predominant exophytic overgrowth of well-differentiated keratinizing epithelium having minimal atypia associated with in-tense chronic inflammatory infiltrate. The pathological diagnosis of verrucous carcinoma is not so difficult. However, in some cases, small or superficial biopsy specimens may only exhibit hyperkeratosis, acanthosis and papillomatosis. Therefore, in some cases, verrucous carcinoma, appearing benign with "pushing" borders and an intact basement mem-brane, can be mistaken for a benign lesion histologically. Deeper and adequate biopsy specimens, along with a sufficient volume, must be obtained whenever verrucous carcinoma is suspected for a definitive diagnosis. In fact, multiple biopsies are sometimes recommended for diagnosing verrucous carcinoma [
16].
Once a diagnosis of verrucous carcinoma has been established, complete resection of the tumor is considered as the treatment of choice. Verrucous carcinoma has a good prognosis when treated early with local excision. Extensive lesions, however, may require more-aggressive procedures. It is important to diagnose accurately the verrucous carcinoma for preventing the most extensive involvement of adjacent areas and/or wide surgical resection of the tumor [
17].
5. Conclusions
Verrucous carcinoma is a subtype of SCC and is a very rare disease. On the other hand, benign disease such as verruca are relatively common. Typically, treatment for such benign diseases identified through biopsy is straightforward. However, if there is no improvement despite continuous treatment, consideration should be given to surgical complete excision for both treatment and diagnosis. Since diagnosis relies on biopsy, there's a risk of persisting with incorrect treatment without considering other conditions.
Although verrucous carcinoma is rare, it can occur on the lips, albeit less frequently. In cases where it might be mistaken for verruca, complete excision and a secondary diagnosis through frozen biopsy should be considered, as demonstrated in the aforementioned case. Given its malignant nature, complete excision is the primary treatment principle for verrucous carcinoma. Subsequently, reconstruction options should be tailored to the patient's needs, considering both functional and aesthetic criteria.
Institutional Review Board Statement
This case report was reviewed and approved by the Institutional Review Board of Inje University Haeundae Paik Hospital (IRB No. 2024-04-017), and all data were anonymized prior to submission.
Informed Consent Statement
Written informed consent for publication of the patient’s clinical details and images was obtained from the patient.
References
- Ackerman, LV. Verrucous carcinoma of the oral cavity. Surgery 1948, 23, 670–678. [Google Scholar] [PubMed]
- Bouquot, JE. Oral verrucous carcinoma: Incidence in two US populations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 86, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Kumar RBC, Raj AC. Verrucous carcinoma of lip: An unusual presentation. Amrita J. Med. 2012, 8, 40–42. [Google Scholar]
- Shroyer KR, Greer RO, Fankhouser CA, McGuirt WF, Marshall R. Detection of human papillomavirus DNA in oral verrucous carcinoma by polymerase chain reaction. Mod. Pathol. 1993, 6, 669–672. [Google Scholar]
- Lübbe J, Kormann A, Adams V, et al. HPV-11- and HPV-16-associated oral verrucous carcinoma. Dermatology 1996, 192, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Fliss DM, Noble-Topham SE, McLachlin M, et al. Laryngeal verrucous carcinoma: A clinicopathologic study and detection of human papillomavirus using polymerase chain reaction. Laryngoscope 1994, 104, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Strojan P, Smid L, Cizmarevic B, Zagar T, Auersperg M. Verrucous carcinoma of the larynx: Determining the best treatment option. Eur. J. Surg. Oncol. 2006, 32, 984–988. [Google Scholar] [CrossRef] [PubMed]
- Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol. 2009, 45, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Koch BB, Trask DK, Hoffman HT, et al. ; Commission on Cancer, American College of Surgeons; American Cancer Society. National survey of head and neck verrucous carcinoma: Patterns of presentation, care, and outcome. Cancer 2001, 92, 110–120. [Google Scholar] [CrossRef]
- Waskowska J, Koszowski R, Raczkowska-Siostrzonek A, Stemplewska K. Verrucous carcinoma of the tongue: A rare case study. Cent. Eur. J. Med. 2012, 7, 145–148. [Google Scholar]
- Oliveira DT, de Moraes RV, Fiamengui Filho JF, Fanton Neto J, Landman G, Kowalski LP. Oral verrucous carcinoma: A retrospective study in São Paulo Region, Brazil. Clin. Oral Investig. 2006, 10, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Miller ME, Martin N, Juillard GF, Bhuta S, Ishiyama A. Temporal bone verrucous carcinoma: Outcomes and treatment controversy. Eur. Arch. Otorhinolaryngol. 2010, 267, 1927–1931. [Google Scholar] [CrossRef] [PubMed]
- Kwon HB, Choi YS, Lee JH, et al. Treatment of verrucous carcinoma of the lower lip with topical imiquimod (Aldara®) and debulking therapy. Ann. Dermatol. 2011, 23 (Suppl. 1), S68–S71. [Google Scholar] [CrossRef] [PubMed]
- Zielonka E, Goldschmidt D, de Fontaine S. Verrucous carcinoma or epithelioma cuniculatum plantare. Eur. J. Surg. Oncol. 1997, 23, 86–87. [Google Scholar] [CrossRef] [PubMed]
- Noble-Topham SE, Fliss DM, Hartwick RW, et al. Detection and typing of human papillomavirus in verrucous carcinoma of the oral cavity using the polymerase chain reaction. Arch. Otolaryngol. Head Neck Surg. 1993, 119, 1299–1304. [Google Scholar] [CrossRef] [PubMed]
- Orvidas LJ, Olsen KD, Lewis JE, Suman VJ. Verrucous carcinoma of the larynx: A review of 53 patients. Head Neck 1998, 20, 197–203. [Google Scholar] [CrossRef]
- Kang CJ, Chang JT, Chen TM, Chen IH, Liao CT. Surgical treatment of oral verrucous carcinoma. Chang Gung Med. J. 2003, 26, 807–812. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).