1. Introduction
Chronic obstructive pulmonary disease (COPD) is the most frequent chronic noncommunicable disease of the respiratory system and presents a significant health care problem [
1]. Joint analysis of several studies conducted between 2000-2010 demonstrated that global one-year mortality as a consequence of COPD varies from 4% (in people having 45 years or more) to 28% (in people of 65 years or older) [
2].
It has a progressive character and it is combined with the inflammatory reaction of airways to harmful particles or gases. Phenotyping of the patients with COPD is in a significant expansion in the recent years. However, there is no general consensus of the number of phenotypes and precise definition. Moreover, it might be necessary to admit that individual patients can qualify into more than one phenotype [
3]. Guidelines of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) are inadequately applied in practice, everything is made even more difficult with raising complexity of phenotypes and algorithms of COPD, which are difficult to follow in the busy conditions of outpatient clinics. The need to specifically implement and adjust guidelines according to the local needs is more and more recognized. It has resulted in the adoption of national guidelines and positions, in the last couple of years [
1].
The objectives of the conducted investigation were the following:
1. Examination of the influence of the selected clinical and demographic factors (sex, age, serum eosinophil level, type of therapy which the patient uses, alpha-1 antitrypsin level, the findings of the multi-slice computer tomography of the thoracic cavity (MSCT), BMI and smoking – (number of packs/year) on the rate of FEV1 decline,
2. Determination of variability of pulmonary function tests over time in patients with diagnosed COPD,
3. Estimation of correlation of the degree of FEV1 decline with the stages determined according to the GOLD classification [
4], as well as the type of inhalation therapy which the patients used,
4. The estimation of the predictive significance of parameters measured by the body plethysmography test and the respiratory muscle strength test for the rate of decline of FEV1 values in patients with diagnosed COPD.
2. Materials and Methods
The study was designed as prospective; patients at the Pulmonology Clinic of the Clinical Centre of Serbia (CCS) with established diagnosis of chronic obstructive pulmonary disease according to the current criteria of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [
4], were included.
Criteria for inclusion of subjects in investigation: Established diagnosis of COPD, age of subjects of over 18 years, stable phase of the disease: Without exacerbations and without changes in medicament regimen in the period of at least four weeks before the trial.
Exclusion criteria: The administration of systemic corticosteroids in the period of four weeks before the trial, patients with diagnosed neuromuscular disease, patients with spinal column deformity, interstitial lung diseases, lung congestion, respiratory infection.
The following was conducted in all subjects:
1) Gathering of demographic and clinical data using the specially designed questionnaire: sex and age, smoking status: current smoker, former smoker (if the subject stopped smoking a year ago or longer), non-smoker – smoking intensity: presented as the index of pack-year (number of pack-years= years of smoking x number of daily smoked cigarettes), anthropometric examinations: body weight and height were measured. Body mass index – BMI is calculated by division of body weight by height squared (kg/m2) [
5].
2) Analysis of pulmonary function tests: post BD spirometry (the following were measured: forced vital capacity (FVC), forced expiratory volume in the first second (FEV1) and FEV1/FVC ratio), body plethysmography (total lung capacity TLC, residual volume RV, RV/TLC ratio were measured) and respiratory muscle strength test (maximal inspiratory muscle strength – PImax, maximal expiratory muscle strength – PEmax.)
3) Determination of biochemistry analyses: blood sample for the analysis of serum eosinophil level (increased serum eosinophil level Eo ≥ 300 cells/µL) and alpha-1 antitrypsin level (reference value 0.9-2.0 IU).
4) Multislice scanner (MSCT) of the thoracic cavity was performed on all the patients.
All PFTs were performed according to the recommendations for performance of the procedure of the European Respiratory Society [
6]. Analysis of the obtained PFTs values was performed based on the recommendations for the predicted values of the European Respiratory Society [
7].
All the aforementioned pulmonary function tests were repeated after six months of regular therapy administration.
Descriptive statistics was calculated for the basic demographic and clinical significances. Normality of distribution of the subjects was tested by graphical and mathematical method. Continuous variables were presented as the mean values with standard deviations or median with 25 -75 percentile, as needed. Categorical variables were presented in numbers and percentages. Differences between the groups were analysed using Student's t-test for continuous variables (or Mann-Whitney test if the distribution is not normal) and Pearson's chi-square test for categorical variables. Multivariate comparisons were examined by the ANOVA test. Correlation of continuous variables was calculated using Pearson correlation coefficient. The level of significance was set to 0.05. IBM SPSS 21 (Chicago, IL, 2012) package was used for statistical analysis.
3. Results
The study included 50 patients, 28 (56%) of whom were male and 22 (44%) were female. The average age of the patients was 55.3 ± 8.3. Malnutrition was determined in 4 patients (BMI<20 kg/m2), while excessive weight was measured in 13 patients (BMI 25-29.9 kg/m2) and in 5 of them obesity was detected (BMI ≥30 kg/m2). The number of current smokers was 34, while 16 patients were former smokers. According to the 2022 GOLD classification, none of the patients had criteria for the group I, while most of the patients, 25 of them, were classified in group III (1). The most frequently used therapy was dual bronchodilator therapy (LABA/LAMA in 16 patients), while the least frequently used method was mono-bronchodilator therapy (LAMA in 8 patients). We determined the existence of increased mean value of serum eosinophil count, which was 173.6, and mean value of the serum alpha-1 antitrypsin level was 1.37 IU. No effect of the patient sex or age on the disease progression and the rate of FEV1 decline was determined in our investigation. Smoking status, that is pack/year number in our study had no statistically significant effect on the rate of FEV1 decline, but the value of statistical significance was borderline (p=0.058). The effect of the alpha-1 antitrypsin level on the degree of FEV1 decline was not confirmed, while the reduced value of the measured protein correlated with the values of the body plethysmography test in a statistically significant way. Decline of the body plethysmography test value in patients with measured alpha-1 antitrypsin level below borderline value (TLC p 0.05 ± 0.927, RV p 0.01±0.451, RV/TLC p 0.01±0.556) was determined with statistical significance.
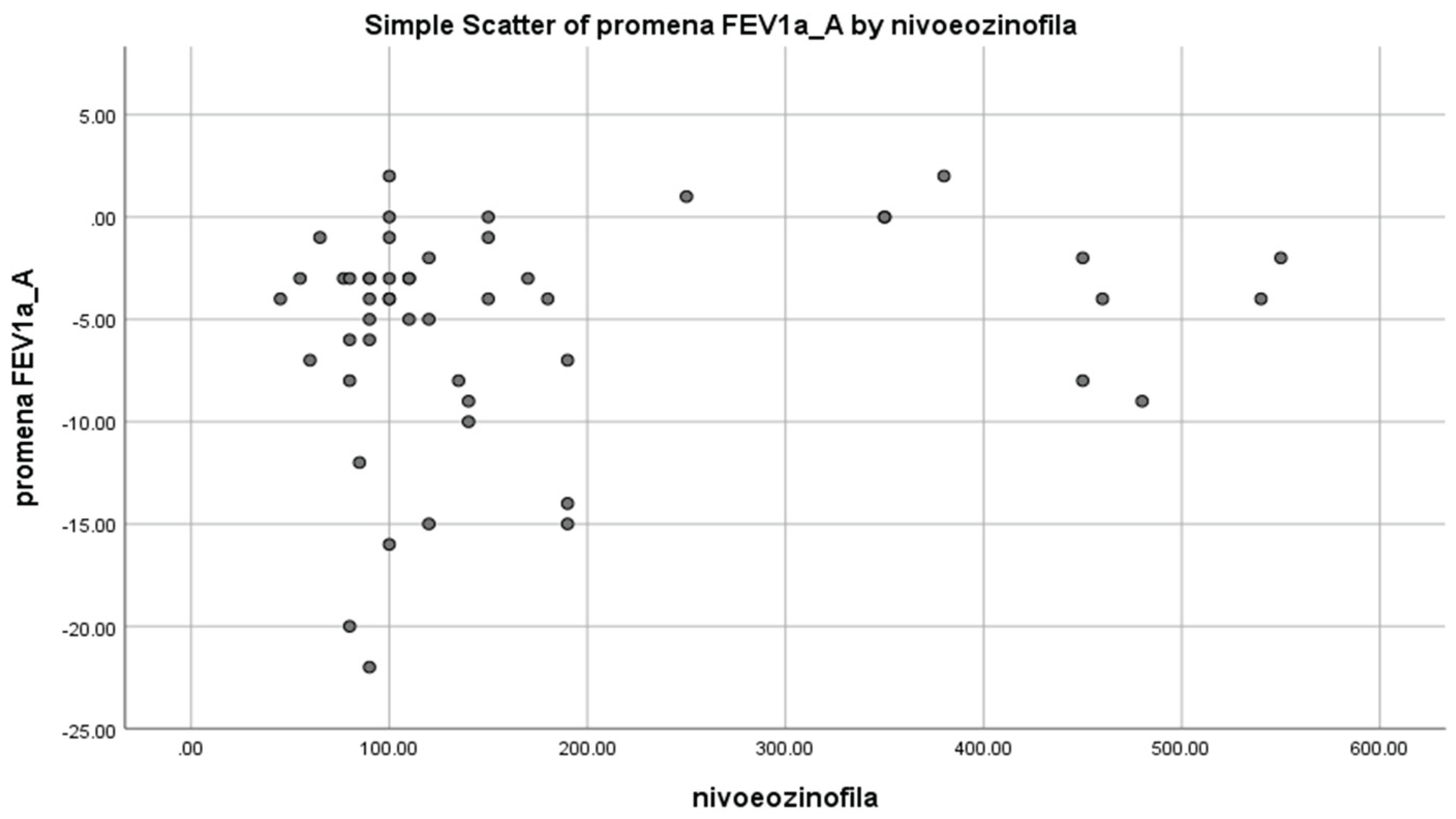
The patients were divided in two groups based on the serum eosinophil count (over 200 (10 patients) and below 200 cells (40 patients)). The patients in whom the level of over 200 eosinophils was determined had statistically significantly lower FEV1 decline in comparison to the patients with lower levels (2.6% vs 6.1%, p=0.026). Due to the small sample size and collinearity, additional stratification of the patients according to the use of inhalation corticosteroids was not possible. (
Figure 1)
Based on the findings on the MSCT, the patients were stratified in two groups (thickening of the interstitium and fibrous changes (n = 29) AND low attenuation with signs of emphysema (n=21)). The examination of correlation of the thoracic cavity MSCT findings with the rate of FEV1 decline and the values of other, in the study applied pulmonary function tests was done by the t-test for independent samples and the results were presented in
Table 1.
The deterioration of the pulmonary tissue and the development of changes in the lung parenchyma as a consequence of chronic inflammation lead to the significant reduction of values of parameters measured by the body plethysmography test. Namely, thickening of interstitium and fibrous changes in pulmonary parenchyma negatively correlate in a significant way with the values of TLC, RV and RV/TLC, that is significant reduction of the values was determined. The significance of the initial MSCT findings for the rate of FEV1 decline was not determined.
Table 2 shows the movement of the mean value of parameters obtained through the pulmonary function tests during the 6-month follow-up period during which the patients used the recommended inhalation therapy.
| Variables |
Initial tests
N=50
(% of the predicted value, MV±SD) |
Follow-ups
N=50
(% of the predicted value, MV±SD) |
Difference between the initial and final value
(decline of % points)
|
| FVC |
79.7± 20.44 |
70.7±20 |
9.04 ±10.09 |
| FEV1 |
45.14±16.10 |
39.74±14.88 |
5.40 ±5.35 |
| FEV1/FVC |
45.50±12.97 |
45.08±12.64 |
0.42 ±3.85 |
| TLC |
82.28±13.11 |
74.76±14.46 |
7.52 ±5.71 |
| RV |
95.02±22.41 |
95.04±34.20 |
0.02 ±18.51 |
| RV/TLC |
111.96±19.60 |
119.96±38.49 |
8 ±28.01 |
| Pimax |
57.02±16.19 |
44.88±15.23 |
12.14 ±6.95 |
| Pemax |
62.34±16.02 |
52.48±17.23 |
9.86 ±6.81 |
It was determined that there was significant reduction of FVC values of 9.04%±10.09, as well as of FEV1 values for 5.40%±5.35 in the observed six-month period. Reduction of TLC for 7.52%±5.71 was also observed. Significant decline of respiratory muscle strength was also registered, PImax was reduced for 12.14%±6.5, and PEmax for 86±6.81 in the observed period.
The largest change of FEV1 values in the observed six-month period was determined in the group of patients who were in the beginning of the investigation classified in the moderate COPD stage (GOLD2 stage) according to the GOLD criteria, while, as expected, FEV1 change was smaller in patients with the GOLD3 stage and the change was smallest in patients with GOLD4 stage. Due to the small number of subjects no stratification of the GOLD2 stage patients according to the type of therapy they used was performed.
In the conducted investigation it was determined that the type of inhalation therapy which the patients used during the trial had influence on the change of the RV value, while it did not have a significant influence on the other parameters of the spirometry testing (FVC, FEV1, FEV1/FVC, FEF50%, FEF75%, MMEF%) (
Table 3).
Influence of the respiratory muscle strength on FEV1 values was also examined, as well as the ratio of the aforementioned tests after six months. Statistically significant reduction of the FEV1 values was found in patients who, at the beginning of the study, had smaller value measured for both groups of respiratory muscles: inspiratory (0.033±0.303 initial testing, 0.021±0.326 follow-up testing) and expiratory muscles (0.047±0.285 initial testing, 0.066±0.262 follow-up testing).
Predictive potential of the body plethysmography test for the decline of FEV1 value was also examined. It was determined that the degree of hyperinflation measured by the body plethysmography was a significant marker of the rate of FEV1 decline. Spearman's rank correlation found a statistically significant correlation between high RV (0.019±0.330) and RV/TLC (0.002±0.429) values as a marker of the present hyperinflation, measured at the beginning of the study, and the degree of decline of FEV1 value which was determined at the beginning and the end of the study.
4. Discussion
FEV1 has a central place in the diagnostics and follow-up of COPD. Through longitudinal follow-up of the patients with COPD, phenotypes with fast decline of pulmonary function (“fast decliner”) can be precisely profiled. Recommendation of the current guidelines is that follow-up of these patients must last at least 2 years.
Our investigation has shown that the respiratory muscles strength is a significant predictor of the rate of the FEV1 decline. It has also been noticed that the higher degree of hyperinflation influences faster FEV1 decline, and the influence of the blood eosinophil level on the degree of FEV1 decline was also determined. On the other hand, no correlation between the findings of parenchymatous changes on the thoracic cavity MSCT and changes of FEV1 value over time was found. Also, the alpha-1 antitrypsin level in our study did not influence the FEV1 decline, but correlation of this protease inhibitor with the values of parameters measured with the body plethysmography test was determined. The question arises whether the use of FEV1 value as the only parameter of the pulmonary function in classification of the COPD patients is a relevant criterion, as well as whether its value should be one of the main factors for the decision on the timely administration of the therapy. In several studies conducted so far, the limitations of spirometry testing with the aim of follow-up of COPD progression were highlighted. Guidelines of the Global Initiative for Chronic Obstructive Lung Disease do not recommend the application of spirometry as the only test for follow-up of the patients ever since 2017, because even with its good sensitivity this test has low specificity [
8]. Further work is certainly needed on the investigation of spirometry diagnostic stability, and potentially of currently valid lower limit of the normal finding as well.
Muscle weakness in COPD develops primarily due to malnourishment connected with biochemical, anatomical and physiological changes, then due to muscle atrophy caused by physical inactivity, reduction of the vascularisation of the muscle mass, but also due to blood oxygenation reduction, steroid induced myopathy, as well as lung hyperinflation with increased residual volume. Therefore, there is a clear need for implementation of protocols which would include principles of application of nutritive supplements, which should be primary intervention in patients with low body weight. In systematic review article of RenataI Figueiredo et al., it was found that training of only inspiratory muscles in patients with COPD led to the successful improvement of the findings of breathing function, with significant improvement of FEV1 values (FEV1 (0.08, 95% CI 0.02–0.13)), but without influence on the degree of dyspnoea and quality of life [
9]. The degree of FEV1 decline was significantly higher in patients with increased RV/TLC compared to those who had a lower value of RV/TLC parameter determined (54.2 mL/year versus 10.7 mL/year, p<0.001). In the study by Wook Kim et al., which included 310 patients, hyperinflation at rest and emphysema had a statistically significant correlation with exacerbations(HR = 1.71, 95% CI = 1.26-2.33) and mortality(HR = 3.75, 95% CI = 1.81-7.73). Sakhamuri and Seemungal have suggested that there is a gap in the GOLD guidelines from 2020. In their opinion, the inclusion of parameters of hyperinflation (TLC, IC, RV and RV/TLC), but also of diffusion capacity (DLCO), in the COPD diagnostic criteria is required, because they are independently correlated with exacerbations and/or mortality. We demonstrated in our investigation that the patients with a determined value over 200 eosinophils had a statistically significantly lower FEV1 decline. In the large cohort of former and current smokers with wide range of COPD severity, large concentrations of eosinophils in sputum were a better biomarker than larger concentrations in blood, for identification of subgroups of patients with a more severe disease form, more frequent exacerbations and poorer thoracic cavity MSCT findings. Eosinophils in blood were not a reliable biomarker for seriousness or degree of COPD exacerbations. We have established in our study that the application of inhalation corticosteroids leads to RV reduction, but given the number of subjects, the aforementioned conclusion should be taken with caution. There is plenty of evidence in favour of efficacy of double bronchodilation (LAMA+LABA) in the improvement of symptoms and outcomes of the stable phase of the disease and of combined therapy (LABA+ICS) in prevention of exacerbations [
10,
11,
12].
In our daily clinical practice we see that patients with moderate COPD stage use the prescribed inhalation therapy rarely or not at all. In our investigation we established that the most pronounced FEV1 decline was in patients in whom moderate COPD stage, GOLD2 stage, was diagnosed. In a multicentre randomized clinical study, which included 841 patients with the diagnosis of COPD, who were classified in GOLD1 and GOLD2 stage of the disease, it was demonstrated that the administration of tiotropium resulted in preservation of higher FEV1 values than placebo during 24 months [
13].
5. Conclusions
Prospective investigation conducted at the CCS Pulmonology Clinic included 50 patients with the COPD diagnosis and had an aim to establish the influence of various factors on the FEV1 change during the 6-month follow-up period. It was established that in patients with alpha-1-antitrypsin below the borderline value there was a statistically significant reduction of the values of parameters obtained through the body plethysmography test, TLC, RV and RV/TLC, compared to the patients who had normal alpha-1 antitrypsin levels. At the same time, a statistically significant reduction was observed in parameters obtained by the body plethysmography test, TLC, RV and RV/TLC, in patients who had the existence of thickening of interstitium and fibrous changes in the lung parenchyma described in the thoracic cavity MSCT, compared to the patients who had emphysema changes as dominant in the thoracic cavity MSCT.
In patients who had blood eosinophil levels higher than 200 cells in the conducted investigation, pointing to the possible protective effect of ICS application in patients with the increased blood eosinophil count.
During the 6-month follow-up period and regular use of recommended inhalation therapy, significant reduction of values of lung function parameters was found for FEV1 and FVC, while the other parameters did not significantly change over time. The TLC value on body plethysmography also showed significant reduction during the six-month period compared to other parameters, pointing to the possible significance of body plethysmography tests in follow-up of patients with COPD.
In the conducted investigation, the strength of respiratory muscles, inspiratory and expiratory, showed significant reduction during the six-month follow-up period, pointing that the respiratory muscle strength test might also have an impact among the tests which are conducted as obligatory in all the patients with COPD. The investigation determined that there was a statistically significant reduction of the FEV1 values in patients who at the begging of the study had lower value measured for both groups of respiratory muscles: inspiratory and expiratory muscles, pointing to the predictive significance of the respiratory muscle strength for the FEV1 value reduction.
The largest FEV1 decline was shown in patients who were classified in GOLD2 stage compared to the patients who were classified in GOLD3 or 4 stages.
The conducted investigation did not show that the type of administered inhalation therapy (LABA/ICS, LAMA/LABA/ICS, LAMA/LABA, LAMA) showed significant influence on FEV1 decline, which was the primary objective of the investigation. However, the administration of ICS in combinations LABA/ICS and LAMA/LABA/ICS was statistically significantly correlated with RV value reduction over time, pointing to the significance of ICS administration in RV reduction, that is reduction of hyperinflation.
Moreover, a statistically significant correlation was established between high values of RV and RV/TLC, measured at the begging of the study, and the degree of FEV1 decline. Which indicates that the initially present hyperinflation is one of the most significant factors which predict fast reduction of FEV1 value.
With this approach, we want to start treatment of the disease in the early stages, improve profitability, reduce possible unwanted effects and provide effective treatment.
Author Contributions
All authors contributed to the article equaly. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and Ethics Committee of Clinic for Pulmonology, University Clinical Centre of Serbia.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We would like to thank all the clinical staff of Department of funcional diagnostics of Clinic for Pulmolonogy, University Clinical Centre of Serbia.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
COPD
GOLD
WHO
RF
FVC
FEV1
MSCT
BMI
TLC
RV
PImax
Pemax |
chronic obstructive pulmonary disease
Global Initiative for Chronic Obstructive Lung Disease
World Health Organization
respiratory function
forced vital capacity
forced expiratory volume in the first second,
multislice scanner of the thoracic cavity
body mass index
total lung capacity
residual volume
maximal inspiratory muscle strength
maximal expiratory muscle strength |
References
- Plaza, V.; Álvarez, F.; Calle, M.; Casanova, C.; Cosío, B.G.; López-Viña, A.; de Llano, L.P.; Quirce, S.; Román-Rodríguez, M.; Soler-Cataluña, J.J.; et al. Consensus on the Asthma–COPD Overlap (ACO) Between the Spanish COPD Guidelines (GesEPOC) and the Spanish Guidelines on the Management of Asthma (GEMA). Arch. De Bronc- 2017, 53, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Rycroft, C.; Heyes, A.; Lanza, L. ; Karin Epidemiology of chronic obstructive pulmonary disease: a literature review. Int. J. Chronic Obstr. Pulm. Dis. 2012, 7, 457–494. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Lamprecht, B.; Ramírez, A.S.; Martinez-Camblor, P.; Kaiser, B.; Alfageme, I.; Almagro, P.; Casanova, C.; Esteban, C.; Soler-Cataluña, J.J.; et al. Mortality prediction in chronic obstructive pulmonary disease comparing the GOLD 2007 and 2011 staging systems: a pooled analysis of individual patient data. Lancet Respir. Med. 2015, 3, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2025. Available from: https://goldcopd.org/2025-gold-report/. Accessed: 2025 Sep 09.
- Koblizek, V.; Chlumsky, J.; Zindr, V.; Neumannova, K.; Zatloukal, J.; Zak, J.; Sedlak, V.; Kocianova, J.; Zatloukal, J.; Hejduk, K.; et al. Chronic Obstructive Pulmonary Disease: Official diagnosis and treatment guidelines of the Czech Pneumological and Phthisiological Society; a novel phenotypic approach to COPD with patient-oriented care. Biomed. Pap. 2013, 157, 189–201. [Google Scholar] [CrossRef] [PubMed]
- MURRAY, John F.; NADEL, J. Textbook of respiratory medicine. 1987. P:90-132.
- Baydur, A.; Behrakis, P.; Zin, W.; Jaeger, M.; Milicemili, J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982, 126, 788–791. [Google Scholar] [PubMed]
- REILLY, John J.; SILVERMAN, Edwin K.; SHAPIRO, Steven D. Chronic obstructive pulmonary disease. Harrisons Principles of Internal Medicine, 2005, 16.2: 1547, 1700-1707.
- Gosker, H.R.; Wouters, E.F.; van der Vusse, G.J.; Schols, A.M. Skeletal muscle dysfunction in chronic obstructive pulmonary disease and chronic heart failure: underlying mechanisms and therapy perspectives. Am. J. Clin. Nutr. 2000, 71, 1033–1047. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.I.N.; Azambuja, A.M.; Cureau, F.V.; Sbruzzi, G. Inspiratory Muscle Training in COPD. Respir. Care 2020, 65, 1189–1201. [Google Scholar] [CrossRef] [PubMed]
- Terzano, C.; Ceccarelli, D.; Conti, V.; Graziani, E.; Ricci, A.; Petroianni, A. Maximal respiratory static pressures in patients with different stages of COPD severity. Respir. Res. 2008, 9, 8–8. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, Y.; Tsutsumi, M.; Nakata, H.; Tsunenari, T.; Maeda, H.; Yokoyama, M. Relationship Between Respiratory Muscle Strength and Lean Body Mass in Men With COPD. Chest 1995, 107, 1232–1236. [Google Scholar] [CrossRef] [PubMed]
- Steuten, L.M.; Creutzberg, E.C.; Vrijhoef, H.J.; Wouters, E.F. COPD as a multicomponent disease: Inventory of dyspnoea, underweight, obesity and fat free mass depletion in primary care. Prim. Care Respir. J. 2006, 15, 84–91. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).