1. Introduction
The incidence of colorectal cancer (CRC) is constantly increasing, but with the introduction of a screening program with adequate bowel preparation, it is expected that the disease will be detected at an early stage with a decrease in the number of patients who, at the time of diagnosis, are in the terminal phase of the disease
Colonoscopy is the gold standard for CRC screening, but its accuracy is related to the high quality of bowel preparation. This study aimed to assess the validity and reliability of existing bowel preparation solutions regarding age, sex, indication, and season of preparation for colonoscopy. Following scientific recommendations, our country has introduced a screening program for colorectal cancer in the general population with the sole aim of early recognition of premalignant and malignant lesions in the curable phase of the disease. The indications for the procedure were different - a search as part of the national screening for colorectal cancer, in patients with various symptoms, preventive colonoscopies, and control colonoscopies. Compared to younger respondents, older respondents had a lower likelihood of having adequate bowel preparation (odds ratio (OR) = 0.98, 95% confidence interval (CI) = 0.97–0.99, p<0.001). In addition, respondents who prepared in winter had less likelihood of having adequate bowel preparation. Compared to PEG, other solutions had a lower probability of adequate bowel preparation. To thoroughly and completely examine the colon, it is necessary to cooperate with the patient and be maximally engaged in preparing the intestine before the examination.
2. Materials and Methods
Participants
A retrospective descriptive analysis was performed on the clinical records of all patients who met the inclusion criteria. We performed a total of 4835 colonoscopies from June 2019 to April 2022, using Pentax colonoscopes of a different generation, without possibility of using the artificial intelligence (AI).
Inclusion criteria were age>18, indicated for colonoscopy from June 2019 to April 2022 (during Covid pandemic). The data comes from the hospital's electronic medical record system, including age, sex, the indication of colonoscopy, risk factors for colonoscopy, day of the week, conscious sedation (pethidine, midazolam) administered by gastroenterology-trained nurse, or propofol sedation administered by an anesthesiologist with or without an anesthesia assistant, diagnosis (irritable bowel disease, tumors, polyps, diverticula, anorectal changes), total colonoscopy time, withdrawal time, and Boston bowel preparation score (BBPS)
We excluded patients with contraindications for colonoscopy: pregnancy, intestinal occlusion, and perforation or threatening perforation (severe inflammation, etc).
Ethical consideration
This study was approved by the Ethics Committee of the Zadar General Hospital (No.01-2529/25-9/25, from 31st of March 2025.). All patients signed an informed consent for a colonoscopy before the exam. Following relevant ethical guidelines, all patient data were anonymized before analysis to protect privacy and confidentiality. As it is a retrospective analysis of existing clinical de-identified data, informed consent of the participants was not required for participation. The study complied with the Declaration of Helsinki and the law regulative on the use of retrospective data in clinical research.
Protocol of bowel preparation
Patients were advised to avoid eating fruits, vegetables, and seeds for five days before the procedure, and to take a bowel cleansing solution after a light lunch the day before the colonoscopy.
For bowel preparation, patients were offered two different solutions:
Solution 1 solution of macrogol 3350 (polyethylene glycol)+ sodium sulfate +sodium chloride + potassium chloride+sodium ascorbate, and ascorbic acid (PEG- Original name: Movi Prep).
Solution 2: bisacodyl + magnesium solution in amount of 3-4 liters
Patients who were examined in an emergency or who were not able to drink a cleansing agent (uncooperative, seriously ill, patients with active rectal bleeding...) were examined without using enemas.
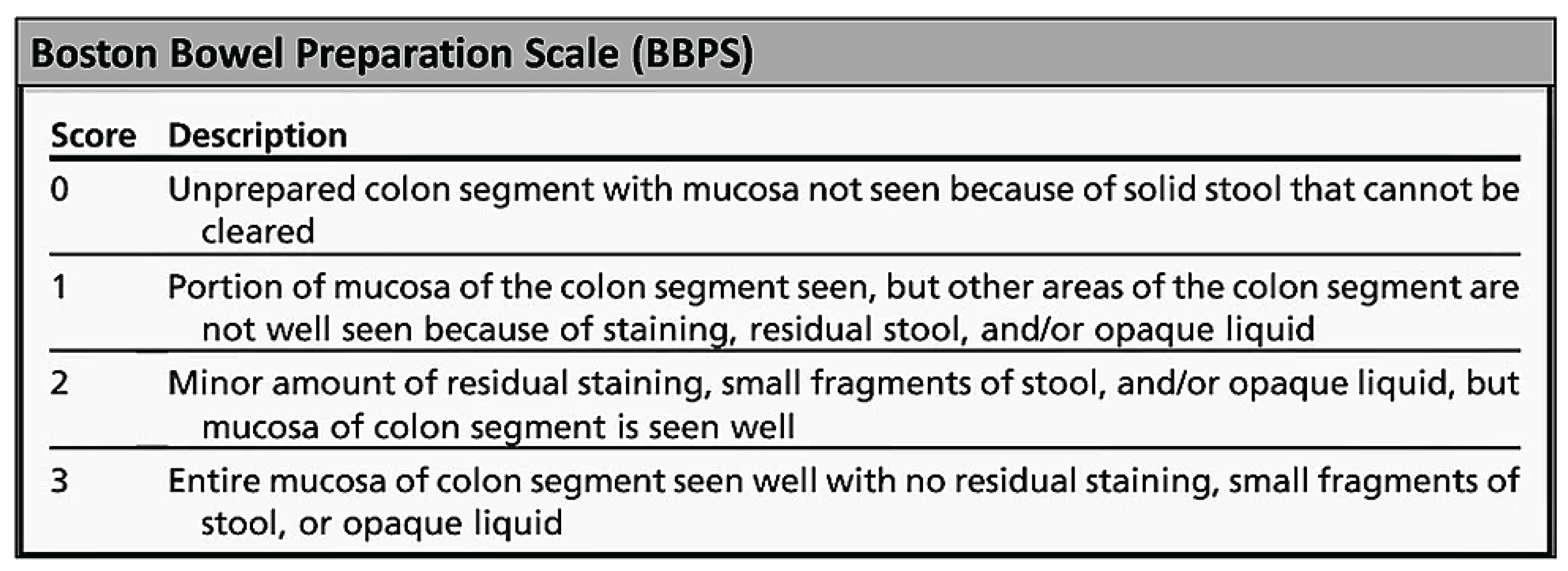
The Boston Bowel Preparation Scale (BBPS), which has been validated in multiple clinical studies, has been used as a basic tool for determining the degree of bowel cleanliness) [
2,
3].The BBPS should be presented in the examination report using the following documentation: right/transverse / left; e.g. = 2/2/3, along with the corresponding total (BBPS = 7). Poorer adenoma detection rate is in correlation with poor bowel preparation (BBPS ≤ 5). [
5].
Figure 1.
Boston Bowel Preparation Scale [
4]. Score - Excellent (BBPS 8-9), Good (BBPS 6-7), Average (BBPS 4-5), Poor (BBPS 0-3)Downloaded from the Internet on February 29, 2024.
Figure 1.
Boston Bowel Preparation Scale [
4]. Score - Excellent (BBPS 8-9), Good (BBPS 6-7), Average (BBPS 4-5), Poor (BBPS 0-3)Downloaded from the Internet on February 29, 2024.
3. Results
Differences by gender, age group, season, day of the week, and bowel preparation solution in the category of quality of bowel preparation(N=4609) (
Table S1).
In the period from 06/2022 to 04/2023 we made a total of 4835 colonoscopies in the general population including hospitalized patients. Total colonoscopy up to the cecum in percentages was 89% (part due to impurity, part abandoned due to pain, stenosis, etc.).
Total number of ileoscopy was 783 (16.2%). The total number of colonoscopies by conscious sedation (pethidine, midazolam) administered by a gastroenterology-trained nurse, or propofol sedation administered by an anesthesiologist with or without an anesthesia assistant, etc, was 259 (5.3%)
Indications for colonoscopy were: national colorectal cancer prevention program (NPP) 237 colonoscopy, preventive colonoscopy 662, different symptomatic reasons (abdominal pain, constipation, etc) 2558, controls in 1378.
After randomization, the total number of colonoscopies undergoing statistical analysis was 4036.
Boston Bowel Preparation Scale was used to evaluate the success of bowel preparation with an overall score of adequate≥ 6, Inadequate 0 – 5.
Data analysis
The statistical analysis was conducted using Statistica 13 (TIBCO Software Inc., 2017) on a sample of 4036 Croatian respondents. The statistical significance was p<0.05.
In the descriptive analysis, mean and standard deviation were used for numerical variables, while absolute number and percentage were used for categorical variables. In the bi-variate analyses, the chi-square test was used to examine the differences between variables for categorical variables, while the Student's t-test and ANOVA were used for numerical variables. The Pearson correlation coefficient was used to examine the relationship between variables.
The multivariate analysis included linear and logistic regression to assess the relationship between the variables. In the linear regression models, the quality of bowel preparation using the BBPS scale and withdrawal time were used as dependent variables. The predictors for these two models were age, gender, indication for colonoscopy (preventive and control examinations were referent group, RG); risk factors (no risk was the RG), season (summer was RG), the timing of bowel preparation (day before the examination was RG), bowel cleansing procedure (the working day was RG), bowel preparation medication (PEG solution was the reference group), premedication or sedation (no was RG), irritable bowel disease, tumor, polyp, diverticulum, anorectal changes, and adequate bowel preparation (no was RG). Logistic regression models were used to predict the probability of adequate bowel preparation and complete colonoscopy. The prior regression model described the predictors and the reference groups, while beta was converted to OR (odds ratio) with a 95% confidence interval.
Characteristics of the study group (
Table 1.)
The average age of the respondents was 62 (M=62; SD=14.0). Respondents aged between 61 and 75 were the most strongly represented, with a total of 43.9% (
Table 1.). Women (53.7%) and men (46.3%) were approximately equally represented in the sample. The most common indications for colonoscopy was symptomatic (53.2%). The respondents were mostly risk-free for colonoscopy (96.3%) and without sedation (94.4 %). A certain percentage of subjects had irritable bowel disease (4.4 %), tumors (4.8 %), polyps (22.9 %), diverticula (24.8 %) and anorectal changes (59.8%).
The respondents were mainly examined in winter (30.6%) and spring (29.1%). The number of colonoscopies was evenly distributed across the days of the week. Bowel preparation was carried out the day before the examination (93.4%), with solution 1 (PEG).
The overall quality of bowel preparation (BPPS score) was 6.2, while the average quality of colon preparation ranged from 1.7 for the right colon, 2.1 for the transverse colon, and 2.4 for the left colon. Quality of bowel preparation was adequate (BBPS≥6) in 3268 (70.9%) patients, while it was inadequate (BBPS ≤5) in 1341 (29.1%) patients. Excellent bowel preparation was in (BBPS 8–9) 1473 (32.0%), good (BBPS 6–7) in 1795 (38.9%), poor (BBPS 4–5) in 715 (15.5%) and inadequate (BBPS 0–3) in 626 (13.6%) patients. The withdrawal time was 8.7±2.7 minutes, while the complete colonoscopy was performed in 87.9% of the subjects (
Table 1).
Differences in bowel preparation quality according to respondents' characteristics (
Table 2.)
No statistically significant difference was found between men and women about the level of bowel preparation (p=0.176). Subjects under 45 years of age (M=6.7±2.0) showed a statistically significant better level of quality of bowel preparation than older subjects (M=6.1±2.0), p<0.001). Older subjects had a lower level of bowel preparation quality (p<0.001) (
Table 2.).
Subjects who underwent colonoscopy in summer had a better degree of quality of bowel preparation (6.4±2.1), while they were least prepared in winter (6.1±2.0), p=0.002. Respondents with the colonoscopy performed on Thursday had the best bowel preparation score (6.4±2.0) and the lowest on Friday (6.0±2.0), p=0.001. Respondents who had performed bowel preparation on Sunday had a higher degree of bowel preparation (6.4±2.0) than on weekdays (6.2±2.1), p=0.008 (
Table 2.)
Subjects with a preventive indication for colonoscopy showed a statistically significantly better degree of bowel preparation (6.6±1.8), compared to symptomatic (6.1±2.1) and control subjects (6.2±2.0), p<0.001. PEG showed the best bowel preparation effect compared to the other preparations (6.4±1.9), while the enema showed the worst results (3.9±2.3), p<0.001 (
Table 2.).
The differences by age group, gender, season, day of the week, and bowel preparation solution in the category of quality of bowel preparation (inadequate (0–3), poor (4–5), good (6–7), excellent (8–9)) are shown in Supplementary
Table 1.
Subjects who received conscious sedation (pethidine, midazolam) administered by a gastroenterology-trained nurse, or propofol sedation administered by an anesthesiologist had the highest quality of bowel preparation (7.2±1.7), p<0.001). Subjects with Chron's disease (7.2±1.8) had significantly better bowel preparation quality, while patients with tumors had poorer (5.2±1.7), p<0.001). No statistically significant difference in bowel preparation was found between subjects with and without polyps (p=0.105). Subjects with hemorrhoids and other anorectal changes had statistically significantly higher quality of bowel preparation (6.4±1.9) than subjects without hemorrhoids (5.9±2.2), p<0.001).
Subjects with adequate bowel preparation had a significantly higher degree of cleanliness (7.3±1.1) than subjects with inadequate bowel preparation (3.6±1.3), p<0.001. Subjects with complete colonoscopy had better bowel preparation (6.6±1.7) when compared to those with incomplete colonoscopy (3.1±1.7), p<0.001 (
Table 2.).
Relationship between quality of bowel preparation and characteristics of the study group (
Table 3)
The linear regression model confirms that older respondents have a lower quality of bowel preparation (β=-0.03, p=0.001). Respondents who had a colonoscopy in summer had a better quality of bowel preparation when compared to autumn(β=-0.03, p=0.009), winter (β=-0.03, p=0.004), and spring (β=0.04, p<0.001), The linear regression model did not confirm that the solution senna was better compared to Movi Prep (PEG), while Enema (β=-0.07, p<0.001) and Bisacodyl (β=-0.06, p<0.001) showed a lower impact on the quality of bowel preparation compared to MoviPrep (PEG) (
Table 3.).
A better quality of bowel preparation was found in subjects who received premedication (β=0.04, p<0.001), in subjects with Chron's disease (β=0.03, p<0.001), diverticulitis (β=0.02, p=0.043) and anorectal changes (β=0.03, p=0.002), while those with a tumor were associated with poor quality of bowel preparation (β=-0.02, p=0.010). There was no association between polyposis and quality of bowel preparation (β=-0.01, p=0.122).
Adequate bowel preparation was associated with better quality of bowel preparation (β=0.78, p<0.001). Longer withdrawal time is positively associated with the symptomatic indication for colonoscopy (β=0.06, p<0.001), spring (β=0.07, p<0.001), bowel preparation on Sunday (β=0.04, p=0.002) and polyposis (β=0.12, p<0.001). A negative association was found with bisacodyl (β=-0.08, p<0.001), ulcerative colitis (β=-0.03, p=0.027), and anorectal changes (β=-0.19, p<0.001).
A longer withdrawal time was associated with a better quality of bowel preparation (β=0.15, p<0.001), (
Table 3.).
Predicting Adequate Bowel Preparation and Total Colonoscopy Completion (
Table S2)
Compared to younger respondents, older respondents had a lower likelihood of having adequate bowel preparation (odds ratio (OR) = 0.98, 95% confidence interval (CI) = 0.97–0.99, p<0.001). In addition, respondents who prepared in winter had less likelihood of having adequate bowel preparation (OR = 0.74; 95% CI = 0.60–0.91; p = 0.004) than those who prepared in summer. Compared to PEG, other solutions had a lower likelihood of adequate bowel preparation (Senna solution (OR = 0.57; 95% CI = 0.34–0.96; p = 0.035), enema (OR = 0.22; 95% CI = 0.14–0.36; p<0.001), bisacodyl (OR = 0.35; 95% CI = 0.20–0.61; p<0.001). Longer withdrawal time is associated with lower odds of adequate bowel preparation (OR = 0.94; 95% CI = 0.92–0.97; p<0.001) (
Table S2.).
Lower odds of a complete colonoscopy were associated with older age (OR = 0.99; 95% CI = 0.98–1.00; p = 0.041), female (OR = 0.77; 95% CI = 0.57–0.90; p = 0.004), symptomatic indication (OR = 0.54; 95% CI = 0.42–0.68; p<0.001), patient with enema (OR = 0.36; 95% CI = 0.22–0.58; p<0.001), bisacodyl (OR = 0.24; 95% CI = 0.13–0.45; p<0.001) and tumor (OR = 0.22; 95% CI = 0.14–0.34; p<0.001).Higher odds for total colonoscopy associated with polyposis (OR = 1.43; 95% CI = 1.06–1.91; p=0.018) and with longer withdrawal time (OR = 1.27; 95% CI = 1.22–1.33; p<0.001).The odds ratio for completeness of colonoscopy was OR = 27.91; 95% CI = 0.92–0.97; p<0.001, indicating that those with adequate bowel preparation were 27.9 times more likely to have a total colonoscopy than those with inadequate bowel preparation, (
Table S2.).
4. Discussion
Zadar General Hospital attracts about 170,000 patients, which is 4.85% of the total population of the Republic of Croatia (about 3.5 million). The objective of this study was to assess the validity and reliability of existing bowel preparation solutions about age, sex, indication, season, and day at week of preparation for colonoscopy. Following scientific recommendations, our country has introduced a screening program for colorectal cancer in the general population with the sole aim of early recognition of premalignant and malignant lesions in the curable phase of the disease. The indications for the procedure were different - a search as part of the national screening for colorectal cancer, in patients with various symptoms, preventive colonoscopies, and control colonoscopies. Boston Bowel Preparation Scale was used to evaluate the success of bowel preparation with an overall score of Adequate ≥ 6, Inadequate 0 – 5.
We hypothesized that people's different activities, and food-taking habits in different seasons contribute to the quality of bowel preparation varied in different seasons. Also, we hypothesized that gender isn't an independent risk factor for quality in bowel preparation. A similar study was performed by Liu Shi and Co in 2023 [
6]. Male gender, inpatient status, and spring season were the independent risk factors for inadequate bowel preparation [
6]. Results in our study are different - no statistically significant difference was found between men and women about the level of bowel preparation (p=0.176), and subjects who underwent colonoscopy in summer had a better degree of quality of bowel preparation (6.4±2.1), while they were least prepared in winter (6.1±2.0), p=0.002. There is no adequate explanation for this kind of different results. We may speculate that there are differences in food-taking habits, between the Chinese and Croatian populations.
That age was a key factor in predicting poor bowel preparation in hospitalized patients.For every 10-year increase in age, the odds of having poor bowel preparation increased by 1.29 [
7].In our study, compared to younger respondents, older respondents had a lower likelihood of having adequate bowel preparation (odds ratio (OR) = 0.98, 95% confidence interval (CI) = 0.97–0.99, p<0.001). Subjects under 45 years of age (M=6.7±2.0) showed a statistically significant better level of quality of bowel preparation than older subjects (M=6.1±2.0), p<0.001). Older subjects had a lower level of bowel preparation quality (p<0.001) (
Table 2.).
Propofol or conscious sedation led to no difference in colonoscopy related quality metrics. [
9]. In our study, subjects who received conscious sedation (pethidine, midazolam) administered by a Gastroenterology-trained nurse, or propofol sedation administered by an anesthesiologist had the highest quality of bowel preparation (7.2±1.7), p<0.001). Subjects with Chron's disease (7.2±1.8) had significantly better bowel preparation quality. The reason for this result is probably the motivation of the patients, as they are young people suffering from inflammatory bowel diseases, which require frequent colonoscopy check-ups.
Monday had the highest rate of inadequate preparation (BBPS < 6) compared to other days of the week. Post-holiday procedures were not associated with poor bowel preparation [
10].In our study, patients with the colonoscopy performed on Thursday had the best bowel preparation score (6.4±2.0) and the lowest on Friday (6.0±2.0), p=0.001. Patients who performed bowel preparation on Sunday had a higher degree of bowel preparation (6.4±2.0) than on weekdays (6.2±2.1), p=0.008 (
Table 2.).
5. Conclusions
In Europe, in 2022, according to the European Cancer Information System (ECIS), there were an estimated 361,986 new cases of colorectal cancer. Among them, there are almost 10,000 patients with Post-Colonoscopy Colorectal Cancer (PCCR). The main causes of PCCR are missed lesions like adenomas, short withdrawal-observation time, rectal retroflection, differences between endoscopist's skill, fatigue, and attention of team, but inadequate bowel preparation is the leading reason for PCCR and missing adenoma. In an era where artificial intelligence is making a big entrance into colonoscopy, an adequately prepared bowel is the first step in reliably detecting small lesions and distinguishing adenomas from lesions that need to be resected. This is especially important for lesions in the left colon. According to Michael F Kaminski and Co, key performance measures – minimum target are: rate of adequate bowel preparation of ≥90% and cecal intubation rate of≥90% [
8].
Compared to younger respondents, older respondents had a lower likelihood of adequate bowel preparation. In addition, respondents who were prepared in winter had less adequate bowel preparation. Compared to PEG, other solutions had a lower likelihood of adequate bowel preparation. To thoroughly and completely examine the colon, it is necessary to cooperate with the patient and be maximally engaged in preparing the intestine before the examination. To achieve adequate bowel preparation, a conversation with the patient is required with a thorough interpretation of the need to follow the dietary instructions, and the need to drink the cleansing solution in an adequate way and at an adequate time. The target group is patients 50+, preparation during summer and recommendation for using PEG solution.
The present study was a single-center retrospective study. The findings of the present study need to be validated by multi-center prospective studies.
Author Contributions
All authors have contributed to and approved the final version of the manuscript. The respective roles of each author are the following: all authors: study concept and design; IK: data analysis; MLj: interpretation of results; MRR: drafting the manuscript; all authors: critical revision of the manuscript for valuable intellectual content.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Zadar General Hospital (No.01-2529/25-9/25, from 31st of March 2025.).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset analysed in this study is available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI |
artificial intelligence |
| BBPS |
Boston bowel preparation score |
| CI |
confidence interval |
| CRC |
colorectal cancer |
| ECIS |
European Cancer Information System |
| GI |
Gastro intestinal |
| OR |
odds ratio |
| PCCR |
Post Colonoscopy Colorectal Cancer |
| PEG |
polyethylene glycol |
| RG |
referent group |
References
- Roshandel, G.; Ghasemi-Kebria, F.; Malekzadeh, R. Colorectal cancer: Epidemiology, Risk Factors, and Prevention. Cancers. 2024, 16(8), 1530. [CrossRef]
- Lai, E.J.; Calderwood A.H.; Doros, G.; Fix, O.K.; Jacobson, B.C. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. GastrointestEndosc. 2009;69(3 Pt 2):620-5. [CrossRef]
- Calderwood, A.H.; Schroy, P.C 3rd.; Lieberman, D.A.; Logan, J.R.; Zurfluh, M.; Jacobson, B.C. Boston Bowel Preparation Scale scores provide a standardized definition of adequate for describing bowel cleanliness. GastrointestEndosc. 2014;80(2):269-76.
- Mahadev, S.; Green, P.H.; Lebwohl, B. Rates of Suboptimal Preparation for Colonoscopy Differ Markedly Between Providers: Impact on Adenoma Detection Rates. J. Clin. Gastroenterol. 2015;49(9):746-50.
- Parmar, R.; Martel, M.; Rostom, A.; Barkun, A.N. Validated Scales for Colon Cleansing: A Systematic Review. Am. J. Gastroenterol. 2016;111(2):197-204. [CrossRef]
- Shi, L.; Liao, F.; Liao, W.; Zhu, Y.; Chen, Y.; Shu, X. Risk factors for inadequate bowel preparation before colonoscopy: a retrospective cohort study. B.M.C. Gastroenterol. 2023;23(1):204. [CrossRef]
- McNabb-Baltar, J.; Dorreen, A.; Al Dhahab, H.; Fein, M.; Xiong, X.; O' Byrne, M.; Ait, I.; Martel, M.;Barkun, A.N. Age Is the Only Predictor of Poor Bowel Preparation in the Hospitalized Patient. Can. J. Gastroenterol. Hepatol. 2016;2016:2139264.
- Kaminski, M.F.; Thomas-Gibson, S.; Bugajski, M.; Bretthauer, M.; Rees, C.J.; Dekker, E.; Hoff, G.; Jover, R.; Suchanek, S.;Ferlitsch, M.;et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2017;49(4):378-97.
- Rahman, S.; Cipriano, L.E.; McDonald, C.; Cocco, S.; Hindi, Z.; Chakraborty, D.; French, K.; Siddiqi, O.;Brahmania, M.; Wilson, A.;et al. Propofol sedation does not improve measures of colonoscopy quality but increase cost - findings from a large population-based cohort study. EClinicalMedicine. 2024;70:102503.
- Rebhun, J.; Pagani, W.; Xia, Y.; Shuja, A. Effect of the Weekend on Bowel Preparation Quality in Outpatient Colonoscopies. Dig. Dis. Sci.2022;67(4):1231-7. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).