1. Introduction
Benign thyroid nodules are a prevalent clinical finding, and a substantial portion, estimated at 15-25%, are cystic or predominantly cystic in nature[
1]. While the majority of these lesions are small and asymptomatic, giant cysts can expand to cause significant compressive symptoms, including dyspnea, dysphagia, and foreign body sensation, as well as notable cosmetic disfigurement, thereby necessitating intervention. The simplest therapeutic maneuver, fine-needle aspiration, offers immediate symptomatic relief but is fundamentally palliative. The underlying fluid-secreting epithelial lining of the cyst wall remains intact, leading to exceptionally high recurrence rates that can approach 60%~ 80%[
2,
3], thus establishing the clear need for more definitive, ablative therapies.
In the contemporary management of benign thyroid nodules, several minimally invasive techniques have become standard of care. Chemical ablation, most notably percutaneous ethanol injection (PEI), is widely recognized as a first-line treatment for recurrent cystic nodules due to its high efficacy, safety profile, and cost-effectiveness [
4]. The therapeutic mechanism of PEI involves cellular dehydration and protein denaturation, which induces coagulative necrosis of the cyst's epithelial lining and thrombosis of small vessels, ultimately leading to fibrosis and obliteration of the cavity. More recently, polidocanol, a detergent sclerosant with adjunctive anesthetic properties, has emerged as an alternative agent, demonstrating comparable efficacy to ethanol with a potentially superior tolerability profile [
5] . However, for large-volume thyroid cysts, chemical ablation often requires multiple sessions (more than two) to achieve satisfactory results [
4,
6].
Concurrently, thermal ablation modalities, such as radiofrequency ablation (RFA) and laser ablation, have proven highly effective for treating solid thyroid nodules by using heat to induce coagulative necrosis. Their application has been extended to cystic lesions, with evidence demonstrating comparable efficacy to PEI [
7,
8].Despite the success of these techniques, a significant treatment gap exists for giant cystic nodules. The application of thermal ablation in this context is fraught with inherent physical limitations. For large thyroid cystic lesions, even after fluid aspiration, the extensive and irregular nature of the residual cyst wall often renders it challenging to achieve complete and uniform necrosis throughout the entire wall via thermal ablation alone. Consequently, areas of the secretory epithelium, particularly at the margins of the collapsed and irregularly folded cavity, are often undertreated. This phenomenon of "marginal regrowth" is a well-documented cause of treatment failure and nodule recurrence following RFA. Indeed, a large initial nodule volume is consistently identified as one of the most significant independent risk factors for recurrence after thermal ablation. The rapid symptomatic recurrence observed in the patient presented in this report serves as a clinical exemplar of this predictable mode of failure.
This report describes the successful management of a giant, recurrent thyroid cyst after RFA failure using a novel, dual-mechanism approach: polidocanol sclerotherapy combined with prolonged, continuous percutaneous catheter drainage. The purpose of this report is to detail this refined technique, propose a mechanistic rationale for its superiority in such challenging cases, and discuss its potential role in the evolving treatment algorithm for giant benign thyroid cysts.
2. Case Presentation
2.1. Initial History and Failed Intervention
A 59-year-old female presented to our institution with a two-week history of progressively worsening dyspnea and a sensation of pressure in her neck, which was exacerbated when in the supine position. Her symptoms had developed shortly after an intervention at an outside hospital. Two weeks prior to her presentation, she was diagnosed with a large left-sided thyroid cyst measuring approximately 7x6x5 cm. At that time, she underwent an ultrasound-guided procedure involving the aspiration of 110 mL of dark brown, hemorrhagic-appearing fluid, which was immediately followed by a session of radiofrequency ablation (RFA). Despite this treatment, her compressive symptoms not only persisted but recurred with notable rapidity over the ensuing two weeks, prompting her to seek a second opinion at our hospital.
2.2. Clinical and Radiological Evaluation at Our Institution
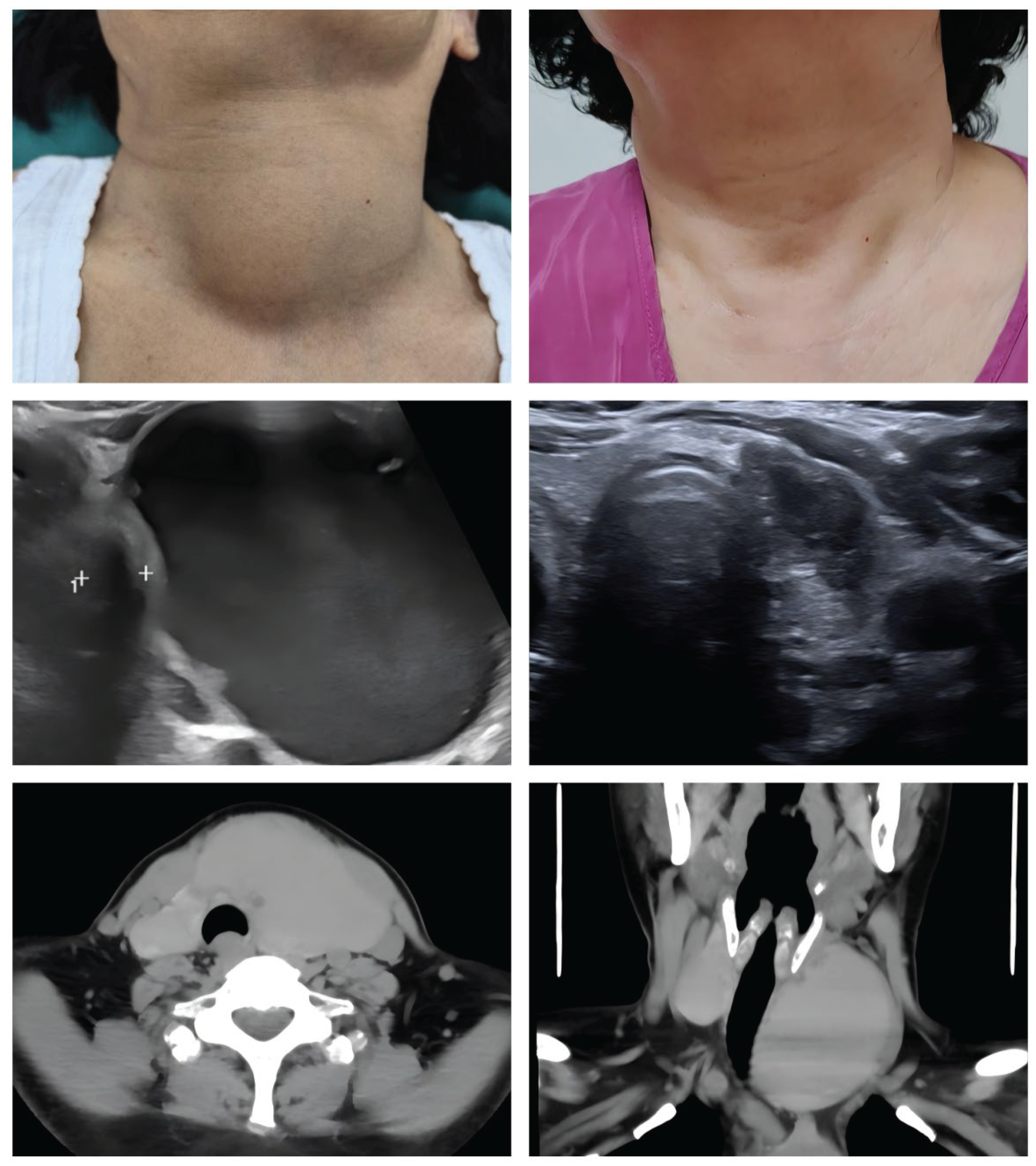
On physical examination, a large and non-tender mass was readily palpable in the left anterior neck, consistent with a large cystic lesion(Figure1A). An ultrasound (US) of the neck was performed, which confirmed the presence of a giant, predominantly cystic lesion originating from the left thyroid lobe (Figure1C). The lesion measured approximately 7x6 cm by US. To better delineate the anatomical relationships and assess the degree of airway compromise, a computed tomography (CT) scan of the neck was obtained. The CT imaging provided a clear depiction of the mass effect, revealing significant rightward deviation and extrinsic compression of the trachea, resulting in noticeable narrowing of the airway lumen (
Figure 1E,F). This finding directly correlated with the patient's primary complaint of dyspnea.
2.3. Therapeutic Intervention: Catheter Drainage and Sclerotherapy
Given the failure of the prior thermal ablation and the significant compressive symptoms, a decision was made to proceed with a modified chemical ablation technique. The procedure was performed in an outpatient setting under local anesthesia with the patient positioned supine with neck hyperextension to optimize anterior neck exposure.
The procedural steps were as follows:
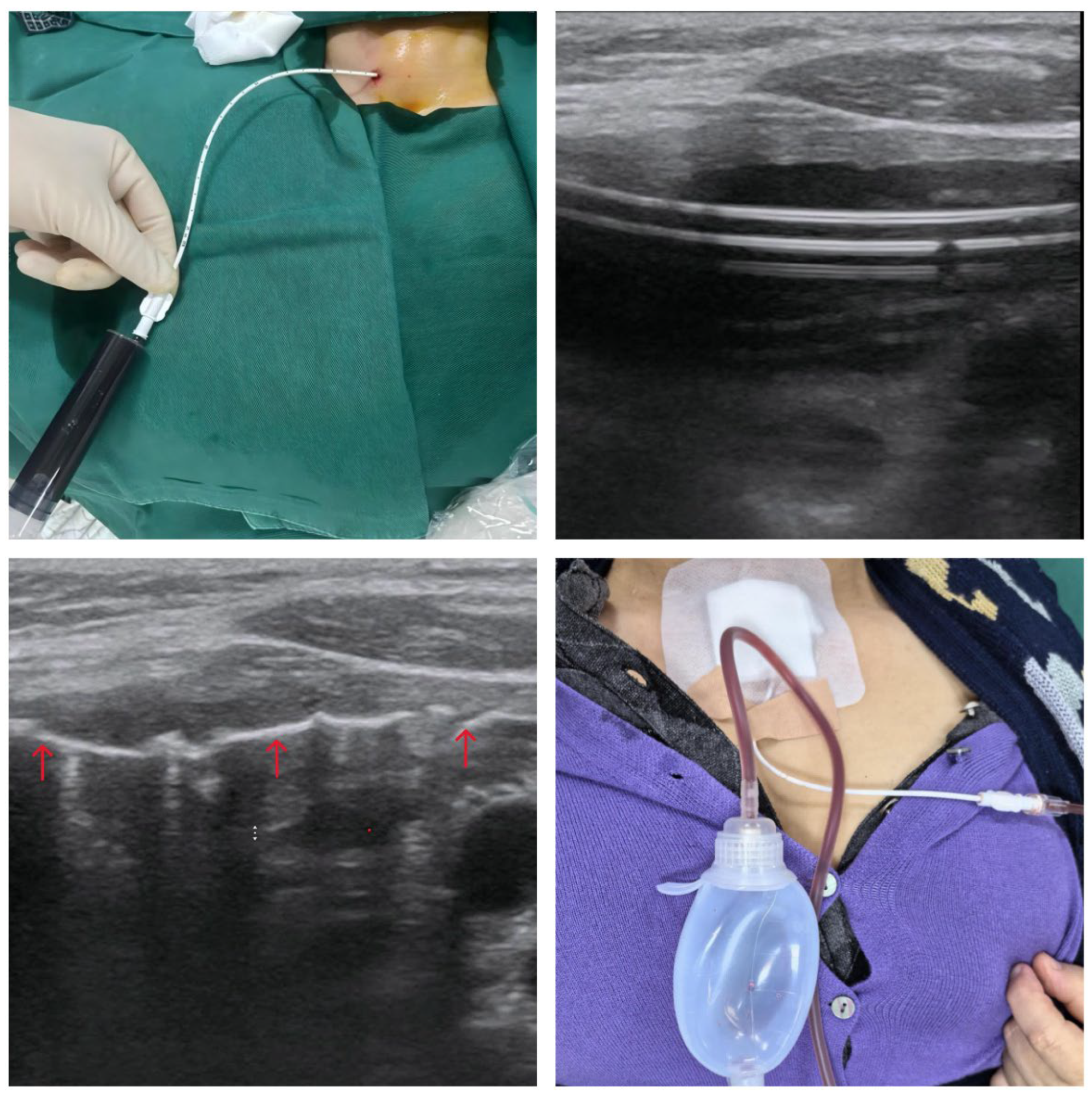
Catheter Placement: Under continuous real-time US guidance, a point of entry was selected on the anterior neck medial to the sternocleidomastoid muscle. After local infiltration with 2% lidocaine, a small 2 mm skin incision was made. A modified trocar system containing a soft, 7-French catheter with multiple side holes was advanced percutaneously into the center of the cyst cavity. The selection of a soft, atraumatic catheter over a rigid metal needle was a deliberate technical choice to minimize the risk of traumatizing the delicate and vascular cyst wall during fluid aspiration and subsequent cyst collapse, thereby reducing the likelihood of iatrogenic hemorrhage.
Aspiration and Lavage: Once the catheter's position within the cyst was confirmed by US, the inner stylet was removed. The catheter was then connected to a 20 mL syringe, and a total of 100 mL of dark fluid was aspirated (
Figure 2A). A sample of the fluid was sent for cytological analysis, which subsequently confirmed the presence of benign follicular cells and hemosiderin-laden macrophages, with no evidence of malignancy. Following complete aspiration, the cyst cavity was repeatedly lavaged with sterile saline until the aspirated fluid became clear. This step was deemed crucial for removing hemorrhagic debris and residual proteinaceous material that could potentially dilute the sclerosant and inhibit its efficacy.Following this, ultrasound could clearly observe the side-hole catheter positioned within the residual cavity(
Figure 2B); this is safer than a metal needle. This is because a metal needle tip risks accidentally puncturing normal tissue, causing re-bleeding, or its tip may become displaced, preventing re-entry into the cavity and leading to risks associated with the drug injection.
Sclerotherapy: A sclerosant foam was prepared using the Tessari method by vigorously mixing 4 mL of 3% polidocanol solution with 24 mL of room air between two syringes connected by a three-way stopcock. The resulting microfoam was then slowly injected into the completely collapsed cyst cavity via the indwelling catheter. Real-time US imaging confirmed the uniform distribution of the hyperechoic foam throughout the cavity, ensuring complete and intimate contact with the entire surface area of the secretory epithelial lining (
Figure 2C).
Prolonged Drainage: After the sclerosant injection, the catheter was secured to the skin with a suture and a sterile dressing. The distal end of the catheter was capped and sealed for the initial 24 hours. This dwell time was intended to maximize the contact period between the polidocanol and the cyst wall to ensure complete chemical ablation. After 24 hours, the catheter was connected to a portable negative pressure drainage bottle to facilitate continuous, active drainage of post-procedural fluid (
Figure 2D).
2.4. Post-Procedural Course and Follow-Up
The patient tolerated the procedure exceptionally well. On the evening of the procedure, she developed a transient, low-grade fever of 37.9°C, which promptly resolved with a single dose of oral ibuprofen. She reported minimal discomfort at the insertion site and, importantly, experienced no voice changes, dysphagia, or other complications.
The indwelling catheter remained in place for a total of four days. During this period, it continuously drained a significant volume of serosanguinous fluid, representing the inflammatory exudate produced in response to the chemical sclerosis. The daily drainage volumes were meticulously recorded: 60 mL on day one (after the initial 24-hour dwell period), 45 mL on day two, 28 mL on day three, and 5 mL on day four. The total volume of inflammatory exudate drained via the catheter was 138 mL, a volume even greater than the initial cystic fluid aspirated. On the fourth post-procedural day, with the drainage having diminished to a negligible amount, the catheter was removed.
At her three-month and one-year follow-up visit, the patient was completely asymptomatic. The dyspnea and neck pressure had fully resolved, and there was no palpable or visible mass in her neck (Figure1B). A follow-up US examination was performed, which demonstrated a dramatic and successful outcome. The previously giant cyst had resolved into a small, irregular, hypoechoic area , showing no evidence of fluid reaccumulation (Figue1D).
3. Discussion
This case report details a successful, novel approach to a challenging clinical problem: a giant, symptomatic thyroid cyst that recurred rapidly after failure of a primary thermal ablation therapy. The success of our modified sclerotherapy protocol is rooted in a clear understanding of the failure mechanisms of conventional treatments and the deliberate application of principles designed to counteract them. The discussion that follows will deconstruct the initial RFA failure, elucidate the mechanistic advantages of the combined chemical sclerosis and prolonged drainage technique, and propose its place in the clinical management of such lesions.
3.1. Analysis of RFA Failure: A Predictable Outcome for a Giant Cyst
The failure of the initial RFA treatment was not an unexpected or anomalous event but rather a predictable consequence of the inherent physical and technical limitations of applying thermal energy to a lesion of this magnitude. The primary mechanism of recurrence is regrowth from undertreated tissue at the nodule margins. In a giant cyst with an initial volume exceeding 100 mL, the surface area of the epithelial lining is vast. Even after aspiration, the cavity collapses into an irregular space with numerous folds and crevices. A standard RFA electrode creates a predictable, typically elliptical, zone of thermal coagulation. It is technically infeasible for such a fixed geometry to conform perfectly to the irregular, extensive surface of the collapsed cyst wall. Consequently, significant portions of the secretory epithelium inevitably receive a sublethal thermal dose, allowing them to survive and resume fluid production, leading to recurrence. Furthermore, any residual fluid within the cavity acts as a potent "heat sink," actively dissipating the thermal energy delivered by the electrode. This effect prevents the surrounding tissue from reaching and maintaining the necrotizing temperatures required for irreversible cell death, further contributing to incomplete ablation and treatment failure.
3.2. The Mechanistic Superiority of Chemical Sclerotherapy for Cystic Lesions
In stark contrast to the line-of-sight and geometric constraints of thermal energy delivery, a liquid or foam sclerosant possesses a distinct physical advantage. Once injected, it flows to fill the entire volume of the collapsed and irregular cavity, ensuring comprehensive and uniform contact with 100% of the target secretory epithelium. This guarantees a more complete and homogeneous ablative effect across the entire cyst wall.
Polidocanol, the agent used in this case, is an ideal sclerosant for this application. As a detergent, its primary mechanism of action is the disruption of the cell membrane lipid bilayer, leading to rapid cell lysis and protein denaturation. This action is not dependent on achieving a specific temperature and is effective upon contact. Furthermore, polidocanol has known anesthetic properties, which may contribute to enhanced patient comfort and lower procedural pain scores compared to ethanol, which is known to cause a significant burning sensation [
6]. Its efficacy in treating benign cystic thyroid nodules has been shown to be comparable to that of ethanol, making it a safe and effective choice [
5,
9].
3.3. The Core Innovation: The Role of Prolonged Catheter Drainage
The most significant and innovative aspect of the described technique is the integration of prolonged, continuous catheter drainage. This element addresses a critical, often overlooked, driver of treatment failure in standard sclerotherapy: the body's own inflammatory response. This modification transforms the procedure into a dual-mechanism solution that addresses both the primary cause of the cyst (the secretory lining) and the secondary cause of recurrence (inflammatory fluid reaccumulation).
The rationale is straightforward. Chemical sclerosis is, by design, a controlled chemical injury. This injury invariably triggers an acute inflammatory response, characterized by the influx of inflammatory cells and the production of a protein-rich serosanguinous exudate. In this case, the volume of this exudate (138 mL) was substantial, exceeding the volume of the original cystic fluid. In a standard sclerotherapy procedure where the sclerosant is aspirated after a short dwell time or left in situ without drainage, this inflammatory fluid would rapidly reaccumulate within the cavity. This re-expansion prevents the opposing, denuded surfaces of the cyst wall from making contact. The resulting "dead space" inhibits the crucial processes of adhesion, granulation tissue formation, and ultimately, fibrosis. This can lead to a "false recurrence," where the cyst refills not with original fluid but with inflammatory exudate, or a true recurrence, as the separated walls fail to fibrose and obliterate the potential space.
By placing a drainage catheter and connecting it to a negative pressure system, this inflammatory exudate is actively and continuously evacuated. This action forces the treated, inflamed walls of the cyst into direct and sustained apposition. This physical contact is the essential catalyst for the final stage of healing: the formation of a fibrotic scar that permanently obliterates the cyst cavity. This principle is not new to interventional medicine but represents a logical, cross-disciplinary application of a proven concept. The successful use of percutaneous catheter drainage combined with sclerosis is a well-established and highly effective technique for managing large, symptomatic, and recurrent cysts in other organs, most notably the liver and kidneys[
10,
11].
3.4. A Proposed New Treatment Algorithm
Based on the successful outcome in this challenging case, it is reasonable to propose a refined treatment algorithm for giant benign thyroid cysts (>5cm in diameter or >40 mL in volume). For such lesions, particularly in cases of recurrence or failure of a prior therapy like RFA or PEI, the combination of chemical sclerotherapy with prolonged catheter drainage should be strongly considered. This approach offers a minimally invasive, highly effective, and cost-efficient alternative to more aggressive options, such as surgical thyroid lobectomy, which carries risks of general anesthesia, scarring, hypothyroidism, and potential injury to the recurrent laryngeal nerve or parathyroid glands. This technique can transform a difficult clinical scenario into a manageable procedure that can be performed on an outpatient or short-stay basis, offering a high probability of durable success.
3.5. Limitations
The primary limitation of this report is that it is based on the experience of a single case. While the outcome was excellent and the mechanistic rationale is strong, the efficacy and safety of this technique cannot be generalized without further evidence. The promising results reported here require validation in a larger, prospective case series or, ideally, a randomized controlled trial comparing this combined technique against single-session sclerotherapy for the treatment of giant thyroid cysts.
4. Conclusions
The combination of polidocanol sclerotherapy with prolonged percutaneous catheter drainage is a novel, safe, and exceptionally effective treatment for giant symptomatic benign thyroid cysts, particularly in the challenging setting of recurrence after failed RFA. The success of this technique is attributable to its dual-mechanism approach. It not only ensures comprehensive chemical ablation of the fluid-secreting epithelium but also actively manages the subsequent inflammatory exudate to promote maximal apposition of the cyst walls. This leads to rapid and durable fibrosis, providing rapid and sustained relief of the patient's compressive symptoms while enhancing the therapeutic effect. This protocol provides a robust and logical solution to the primary drivers of treatment failure in these difficult-to-manage lesions. This technique represents a significant and logical refinement of existing sclerotherapy protocols and warrants further investigation as a first- or second-line therapy in the management of giant benign thyroid cysts.
Author Contributions
Zhaoyue Li: Writing – original draft (lead); formal analysis (supporting); investigation (equal); writing – review and editing (equal). Anyang Liu: Conceptualization (lead); methodology (lead); investigation (equal); supervision (lead); writing – review and editing (equal).All authors have read and agreed to the published version of the manuscript.:
Funding
This research received no external funding.
Institutional Review Board Statement
This case report was conducted in accordance with the Declaration of Helsinki as revised in 2013. The Institutional Review Board of Beijing Tsinghua Changgung Hospital reviewed this case and determined that it was exempt from formal ethical approval due to its nature as a retrospective single case report.
Informed Consent Statement
Written informed consent was obtained from the patient for the medical procedure and for the publication of this case report and any accompanying images.
Data Availability Statement:The data supporting this case report are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank the patient for consenting to the publication of this case.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PEI |
Percutaneous Ethanol Injection |
| RFA |
Radiofrequency Ablation |
References
- Yang C, Hsu Y, Liou J. Efficacy of Ethanol Ablation for Benign Thyroid Cysts and Predominantly Cystic Nodules: A Systematic Review and Meta-Analysis[J]. Endocrinol Metab (Seoul), 2021, 36(1):81-95. [CrossRef]
- Choi WJ, Baek JH, Choi YJ, et al. Management of cystic or predominantly cystic thyroid nodules: role of simple aspiration of internal fluid[J]. Endocr Res, 2015, 40(4):215-219. [CrossRef]
- Bennedbaek FN, Hegedüs L. Treatment of recurrent thyroid cysts with ethanol: a randomized double-blind controlled trial[J]. J Clin Endocrinol Metab, 2003, 88(12):5773-5777. [CrossRef]
- Deandrea M, Trimboli P, Creanza A, et al. Long-term follow-up of cystic thyroid nodules treated with percutaneous ethanol injection (PEI) using two different approaches[J]. Eur J Endocrinol, 2020, 183(5):489-495. [CrossRef]
- Gong X, Wang F, Du H, et al. Comparison of Ultrasound-Guided Percutaneous Polidocanol Injection Versus Percutaneous Ethanol Injection for Treatment of Benign Cystic Thyroid Nodules[J]. J Ultrasound Med, 2018, 37(6):1423-1429. [CrossRef]
- Reverter JL, Alonso N, Avila M, et al. Evaluation of efficacy, safety, pain perception and health-related quality of life of percutaneous ethanol injection as first-line treatment in symptomatic thyroid cysts[J]. BMC Endocr Disord, 2015, 15:73. [CrossRef]
- Sung JY, Kim YS, Choi H, et al. Optimum first-line treatment technique for benign cystic thyroid nodules: ethanol ablation or radiofrequency ablation?[J]. AJR Am J Roentgenol, 2011, 196(2):W210-214. [CrossRef]
- Sung JY, Baek JH, Kim KS, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study[J]. Radiology, 2013, 269(1):293-300. [CrossRef]
- Gong X, Zhou Q, Wang F, et al. Efficacy and Safety of Ultrasound-Guided Percutaneous Polidocanol Sclerotherapy in Benign Cystic Thyroid Nodules: Preliminary Results[J]. Int J Endocrinol, 2017, 2017:8043429. [CrossRef]
- Zerem E, Imamović G, Omerović S. Percutaneous treatment of symptomatic non-parasitic benign liver cysts: single-session alcohol sclerotherapy versus prolonged catheter drainage with negative pressure[J]. Eur Radiol, 2008, 18(2):400-406. [CrossRef]
- Zerem E, Imamovíc G, Omerovíc S. Symptomatic simple renal cyst: comparison of continuous negative-pressure catheter drainage and single-session alcohol sclerotherapy[J]. AJR Am J Roentgenol, 2008, 190(5):1193-1197. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).