1. Investigation Goal
Autism spectrum disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, alongside restricted, repetitive patterns of behavior, interests, or activities (American Psychiatric Association, 2022; Global Burden of Disease Study, 2021; Rebecchi, 2025). Symptoms typically emerge in early childhood and vary widely in severity and presentation (Howlin and Magiati, 2017; Estes et al., 2015; Lai and Weiss, 2017; Lord et al., 2022; Sandbank et al., 2023). Common manifestations include delayed speech, impaired motor coordination, repetitive behaviors, and difficulty interpreting social cues. Over the past three decades, autism prevalence has risen significantly across many countries, prompting extensive research into its etiology and contributing factors (Talantseva et al., 2023). In the United States, the Centers for Disease Control and Prevention (CDC) reported that in 2018, 1 in 44 children were diagnosed with ASD, a sharp increase from earlier estimates: 1 in 150 in 2000, 1 in 88 in 2008, and 1 in 68 in 2016 (Scientific American, 2017; CDC, 2025). This upward trend is not confined to the U.S.; global data compiled by the Global Health Data Exchange show rising autism rates worldwide, although significant variation exists between countries. For example, France and Portugal report some of the lowest rates, at approximately 69.3 and 70.5 per 10,000 people, respectively (World Population Review, 2025; Reuters, 2025). Tracking autism prevalence globally presents challenges due to inconsistent diagnostic criteria, limited resources for assessment in many countries, and underreporting. Autism diagnosis relies on clinical observation rather than objective biomarkers, which complicates cross-national comparisons and epidemiological studies. Despite these limitations, the global rise in autism diagnoses has fueled public concern and scientific inquiry into potential environmental, genetic, and healthcare-related drivers. Among the many hypotheses explored, one of the most contentious is the possible association between early-life vaccine exposure and autism, because of the biological plausibility of vaccine-related neurotoxicity. Tomljenovic and Shaw (2011) argue that aluminum adjuvants, known immune stimulators, may contribute to neuroimmune disorders in genetically vulnerable children. Ramachandran and Grose (2024) document rare but serious neurological adverse events following varicella vaccination, though they emphasize the overall safety of the vaccine. Nath (2023) acknowledges that while modern vaccines are safer than ever, side effects—including those affecting the nervous system—remain a concern and merit ongoing surveillance for supporting safer drug discoveries (Coccia, 2016, 2021). Some recent studies have reignited debate. Mawson and Jacob (2025) reported a statistically significant increase in autism and other neurodevelopmental disorders among vaccinated children in a Florida Medicaid cohort. Their findings suggest that cumulative vaccine exposure, particularly in preterm infants, may warrant further investigation. In this context, Nath (2023) argues that the vaccine manufacturers have legal protection against vaccine side effects. Some experts advocate for personalized vaccine schedules that consider individual risk factors, such as prematurity, genetic predisposition, or family history of neurodevelopmental disorders O(CDC, 2024; Children's Hospital of Philadelphia, 2025).
This debate has persisted for decades, despite a body of scientific literature refuting a causal link (Gulati et al., 2025; Johns Hopkins, 2025; NeuroLaunch, 2025). Gulati et al. (2025) and Miravalle and Schreiner (2014) stress the importance of distinguishing temporal associations from causality. They argue that public misperceptions often arise from coincidental timing between vaccination and the onset of autism symptoms, which typically emerge around the same age as routine immunizations. Doja and Roberts (2006) further emphasize that rigorous epidemiological methods are essential to disentangle these associations and guide evidence-based policy. A comprehensive Danish cohort study involving over one million children found no association between aluminum-containing vaccines and autism or other chronic conditions (Statens Serum Institut, 2025). Similarly, reviews by the CDC and the American Academy of Pediatrics have consistently concluded that vaccine ingredients, including thimerosal and aluminum adjuvants, are not linked to ASD (CDC, 2025; Çatlı and Özyurt, 2025).
Nevertheless, public skepticism remains and fuels vaccine hesitancy (Moye et al., 2022; WHO, 2025; AACAP, 2022). In light of these divergent perspectives, this study aims to contribute to the ongoing discourse by examining the relationship between early-life vaccine exposure and autism incidence across a sample of countries. Specifically, it investigates whether the number and timing of vaccine doses administered to infants under one year of age are statistically associated with national autism rates per 100,000 population. By analyzing cross-national data, this research seeks to identify patterns that may inform public health strategies and optimize vaccine scheduling. The rationale for focusing on vaccine timing stems from emerging evidence that the infant immune system undergoes rapid development in the first year of life. Maternal antibodies provide initial protection, but adaptive immunity—critical for vaccine efficacy—matures gradually (Heald, 2025; Harvard Health, 2024).
Miravalle and Schreiner (2014) suggest that evaluating whether there is causal link between neurologic disorders and vaccinations, not just temporal association, is critical to addressing public misperception of risk of vaccination. As a consequence, the timing and cumulative exposure of early-life immunizations remain areas of active inquiry and this study endeavors to address some gaps in the existing literature:
- -
Cross-national comparisons of vaccine schedules between advanced countries.
- -
Immunization program schedules to minimize adverse events while maintaining protection against infectious diseases.
In this context, this study research aims to contribute to a more nuanced understanding of vaccine safety and informing public health policy and support the development of safer, more effective vaccination strategies that protect children while addressing parental concerns.
2. Study Design, Methods and Materials
2.1. Sample
The sample under study is based on data of 12 high-income countries by World Population Review (2025) to have a homogeneous sample of countries with healthcare systems that are better at detecting and diagnosing autism than are the healthcare systems of other countries. This data set of homogenous nations with a high gross national income per capita has countries with higher and lower autism rate per 100k people (World Population Review,2025). In particular, Higher Autism rate countries are: Singapore, South Korea, Japan, Australia, Canada, USA, whereas Lower Autism rate countries are: Sweden, Denmark, Norway, Finland, Italy, UK.
2.2. Variables and Sources of Data
The variables used, their definitions and sources are indicated in
Table 1.
2.3. Statistical Analysis Procedure of the Scientific Experiment
The study design focuses on a logical groupings for effective comparison to analyze the relationship between early-life vaccine exposure in infants and autism incidence:
Higher Autism rate countries: Singapore, South Korea, Japan, Australia, Canada, USA
Lower Autism rate countries: Sweden, Denmark, Norway, Finland, Italy, UK
Firstly, the variables in
Table 1 are analyzed with descriptive statistics given by arithmetic mean, standard deviation, skewness and kurtosis to assess the distributions and their normality. Variables with non-normal distribution are transformed into
log-scale, to have a normal distribution for appropriate parametric analyses.
Secondly, the average values of Autism rate 2021 per 100k people, Number of vaccines to infants ≤1 year and Number of doses of vaccines to infants ≤ 1 year, were analyzed using the Independent Samples t-Test to determine whether there was statistical evidence that the associated means over time are significantly different between Western and not-western Macro regions, the two main reference groups. The hypotheses used for the Independent Samples t-Test are:
H’0: µ1 = µ2, the two-population means of groups are equal
H’1: µ1 ≠ µ2, the two-population means of groups are not equal
Thirly, Pearson bivariate correlation between Autism rate 2021 per 100k, and both Number of vaccines to infants ≤1 year and Number of doses of vaccines to infants ≤ 1 year, and partial correlation (controlling Vaccination Rates %), with test of significance with one-tailed is applied. This analysis supports to the next analysis about the estimation of the parameters in a relationship between variables under study.
Thirdly, an analysis of dependence in variables was performed using a series of linear regression models for the overall sample given by 12 countries. The first is a linear model of simple regression that considers the Autism rate 2021 per 100k people as a function of Number of vaccines to infants ≤ 1 year. The basic linear model is:
y = dependent variable (Autism rate 2021 per 100k)
x= explanatory variable: Number of vaccines to infants ≤ 1 year.
α = constant
β = regression coefficient
i= countries
u = error term
The models is extended with a multiple regression considering assesses the Autism rate 2021 per 100k on explanatory variables given by both Number of vaccines to infants ≤ 1 year and % vaccination rate for Diptheria, Tetanus, and Pertussis, Measles and Polio disease. The specification of the
log-log model is:
where:
y = Autism rate 2021 per 100k, dependent variable
x1= Number of vaccines to infants ≤ 1 year
x2= Vaccination rate for Diptheria, Tetanus, and Pertussis, Measles and Polio diseases
ut =error term
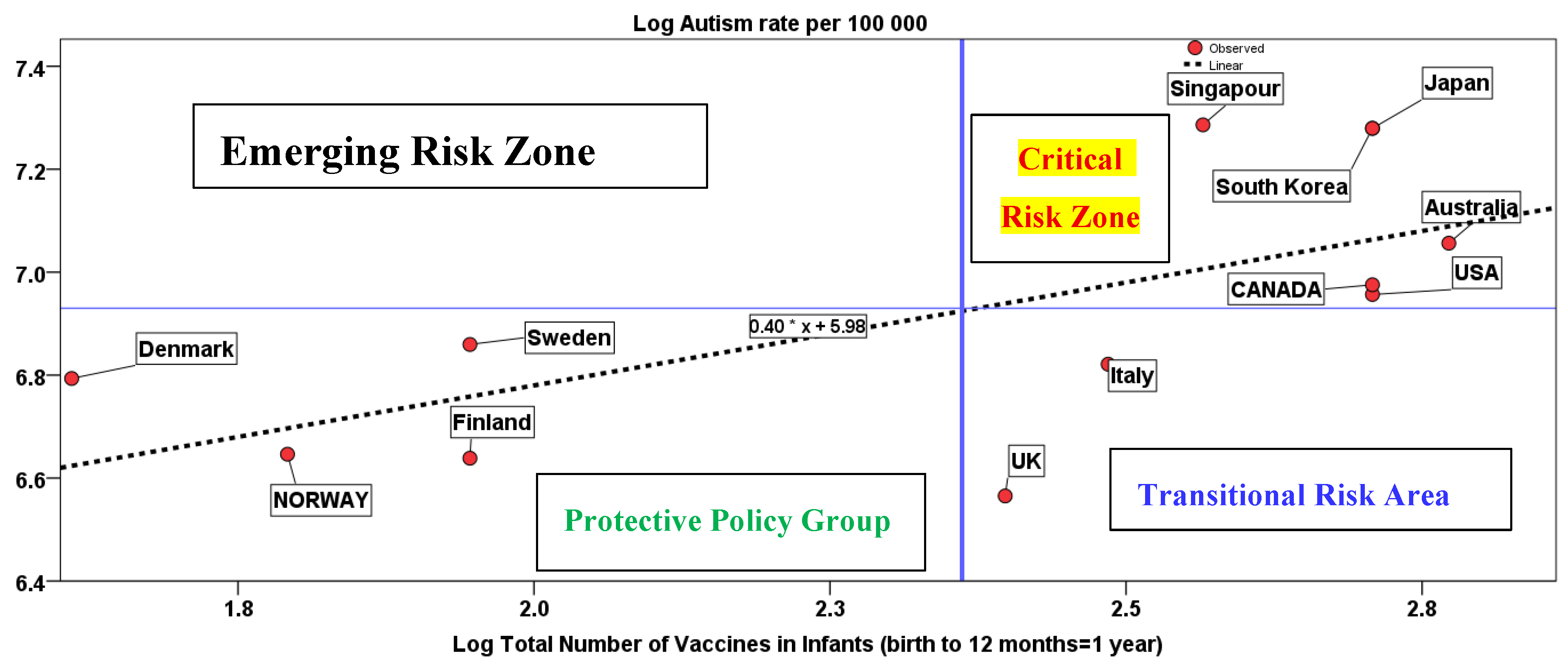
Graphical representation of the regression line is basic lo locate countries in the space, also considering a vertical and horizontal line based on average values of variables. These lines create 4 quadrants. Each quadrant is labeled with a policy implications:
- ▪
Critical Risk Zone – High vaccine exposure and possible high autism rates
- ▪
Protective Policy Group – Low vaccine exposure and low autism rates
- ▪
Transitional Risk Zone – High vaccine exposure but currently low autism rates
- ▪
Emerging Risk Group –Low vaccine exposure, High autism rates.
Statical analyses are done with SPSS software 29.00.
3. Empirical Evidence
Descriptive statistics in
Table 2 shows that the first group of countries has an average rate of autism of 1273.33 per 100,000 people, called higher autism rate countries, vs. the second group that has an average rate of autism of 834.44 per 100k. Higher autism rate countries have also an average of 14.83 Number of vaccines to infants ≤ 1 year, average of 19.67 Number of doses of vaccines to infants ≤ 1 year and average of 95% vaccination rate for diseases: Diptheria, Tetanus, and Pertussis, Measles and Polio. These average values are higher than countries with Lower Autism Rate Countries having an average of 8.00 Number of vaccines to infants ≤ 1 year, average of 9.33 Number of doses of vaccines to infants ≤ 1 year and average of 94.56% vaccination rate.
Since
p-value < .01 of the Independent Samples Test in
Table 3 is less than significance level
α = 0.05, this statistical analysis can reject the null hypothesis, and conclude that the mean of variables for the group of higher autism rate countries is significantly different and higher than second group including countries with lower autism rate per 100k people.
Bivariate correlation in
Table 4 shows that Autism rate 2021 per 100k has a high significant positive with Number of vaccines to infants ≤1 year (
r=0.66,
p-value<
0.05) and Number of doses of vaccines to infants ≤ 1 year (
r=0.65,
p<
0.05): higher Number of vaccines and doses to infants to infants ≤1 year are positively associated with Autism rate 2021 per 100k (for normality of distributions see table 1A in Appendix) Since this value can be affected by general vaccination rate, Partial correlation in
Table 5 (controlling percentage of vaccination rate for Diptheria, Tetanus, and Pertussis, Measles and Polio diseases) reveals a (positive) relationship that is stronger: autism rate has a high significant positive with Number of vaccines to infants ≤1 year (
r=0.87,
p-value<
0.001) and Number of doses of vaccines to infants ≤ 1 year (
r=0.79,
p<
0.01).
Parametric estimate of the linear model as function of time in
Table 6 (
log-log model) shows that a 1% increase in the Number of vaccines to infants ≤ 1 year, it increases the level of autism rate by 0.40% (
p-value 0.05). Multivariate regression also in table 6 shows stronger results. Partial coefficient of Number of vaccines to infants ≤ 1 year (controlling Vaccination rate for Diptheria, Tetanus, and Pertussis, Measles and Polio diseases) suggests that a 1% increase, it increases the autism rate per 100k by 0.47 (
p-value 0.001). The coefficient R
2 of linear models explains about 81% of the variance in the data. The
F ratio of the variance explained by the model to the unexplained variance is significant (
p-value<0.001), then predictors reliably predicts response variable (i.e., autism rate). These results seems to show a main relation of autism rates increases and the driver of number of vaccines to infants ≤ 1 year.
Figure 1 shows the graphical representation of the relation of autism rate on number of vaccines to infants ≤ 1 year with the location of countries under study.
Figure 1 also has a vertical and horizontal line indicating average values. These lines create 4 quadrants. Countries are concentrated in two main quadrants.
In the bottom-left quadrant, countries with lower number of vaccines administrated to infants less than 1 year and lower incidence of autism rate (Norway, Denmark, Finland, Sweden). In contrast, countries in the upper right quadrant have both higher number of vaccines administrated to infants ≤ 1 year (above the mean) and higher incidence (above the mean) of autism rate per 100k (Australia, Canada, USA, Singapore, Japan, South Korea). Italy and UK are the only countries in the bottom-right quadrant but it seems that they have a behaviour towards the convergence in countries with high autism rates. The results presented in
Figure 1 can be used to categorize countries as follows to suggest health policy implications:
Critical Risk Zone (Upper-right):High Vaccine Exposure–High Autism Incidence. Countries in this group show a concerning correlation between early-life vaccine intensity and elevated autism incidence.
Emerging Risk Zone (Upper-left)– –Low Vaccines/High Autism Rates. Although not currently populated, this quadrant would represent countries with low vaccine exposure but unexpectedly high autism rates—warranting further investigation.
Protective Policy Countries III (bottom-left) –Low Vaccines/Low Autism Rates. These countries demonstrate a potentially protective effect of lower early-life vaccine exposure, with correspondingly lower autism rates.
Transitional Area (bottom-right) –High Vaccines/Low Autism Rates. Countries like Italy and UK may currently show low autism rates despite high vaccine exposure, but trends suggest possible convergence toward higher risk zone—requiring close monitoring and policy reassessment.
4. Discussion and Public Health Implications
Building on the introduction’s exploration of autism spectrum disorder (ASD) and its rising global prevalence (American Psychiatric Association, 2022; Talantseva et al., 2023; Grosvenor et al., 2024), this study investigates whether early-life vaccine exposure—specifically the number and timing of vaccines administered to infants under one year—is statistically associated with national autism rates.
A significant gap in the existing literature on autism and vaccine exposure lies in the lack of cross-national, data-driven analyses that examine the timing and intensity of early-life vaccinations in relation to autism prevalence. Most prior studies have focused on single-country cohorts or have explored vaccine safety in general terms, often emphasizing the absence of a causal link between vaccines and autism (Gulati et al., 2025; Çatlı and Özyurt, 2025; Doja and Roberts, 2006). While these studies are basic, they rarely investigate whether variations in vaccine scheduling and dosage intensity across countries might correlate with autism incidence. This study addresses that gap by conducting a comparative analysis across multiple countries, examining whether the number and timing of vaccines administered to infants ≤1 year are statistically associated with national autism rates per 100,000 people. The results presented in Tables2 through 6 and
Figure 1 provide a data-driven perspective on this complex issue.
Figure 1 offers a compelling visual representation of these relationships. Countries are plotted based on their autism rates and number of vaccines to infants ≤1 year, with average lines dividing the graph into four quadrants. The study provides robust evidence of a positive association between vaccine intensity and autism rates—even after controlling for general vaccination coverage. Hence, the stronger partial correlations and regression coefficients in this study suggest that vaccine intensity may be a contributing factor to autism prevalence. These findings echo concerns raised by Tomljenovic and Shaw (2011), who argued that aluminum adjuvants in vaccines may contribute to neuroimmune disorders. Ramachandran and Grose (2024) also documented rare neurological adverse events following varicella vaccination, while Nath (2023) emphasized that despite improved safety profiles, vaccines are not without neurological side effects. Instead, Miravalle and Schreiner (2014) stressed the importance of distinguishing temporal associations from causality, noting that autism symptoms often emerge around the same age as routine vaccinations. Mawson and Jacob (2025) similarly found increased neurodevelopmental disorders among vaccinated children in a Florida Medicaid cohort, supporting the need for further investigation into cumulative exposure effects. However, the results diverge from the broader scientific consensus, which maintains that vaccines do not cause autism (Gulati et al., 2025; Çatlı and Özyurt, 2025; Doja and Roberts, 2006).
The results here can be important for several reasons:
They challenge the assumption that vaccine coverage alone is the key variable, suggesting that vaccine intensity and timing in infants having less than 1 year may also play a role in neurodevelopmental outcomes.
They offer a new framework for categorizing countries based on inter-relationships between autism rates and vaccine exposure, which can guide targeted health policy interventions.
They provide actionable insights for health policymakers, who can use these findings to reassess immunization program schedules, especially for vulnerable populations such as preterm infants or those with genetic predispositions.
In short, the study contributes to a more nuanced understanding of vaccine safety, supporting evidence-based public health strategies that balance disease prevention with neurodevelopmental well-being.
4.1. Explanation of Possible Causes in Relation Under Study
This study provides new insights into possible contributors to high autism rates in certain countries, particularly focusing on the role of early-life vaccine exposure. By analyzing cross-national data, the research identifies a statistically significant association between the number and timing of vaccines administered to infants under one year of age and national autism incidence rates. Countries such as the United States and Japan, which fall into the Critical Risk Zone (
Figure 1), exhibit both high vaccine dose intensity and elevated autism rates—suggesting a potential link that warrants further exploration. In these countries, infants receive an average of 15 different vaccines and about 20 doses within the first year of life, compared to 8 vaccines and 9 doses in countries with lower autism rates. The statistical analyses consistently show that increased vaccine dose intensity is positively associated with autism rates. These findings do not imply causality but suggest that the concentration and timing of vaccine administration, particularly in the first 4-6 months, may be a contributing factor in countries with high autism prevalence. Several mechanisms may explain this association. The infant immune system is still developing during the first year of life, and exposure to multiple immunological stimuli in a short timeframe could potentially influence neurodevelopment in vulnerable populations (Tomljenovic & Shaw, 2011; Nath, 2023). Moreover, countries like the U.S. and Japan have highly standardized and intensive immunization schedules, which may not account for individual risk factors such as prematurity, genetic predisposition, or family history of neurodevelopmental disorders (Mawson & Jacob, 2025). Autism disorders is also higher in some countries that administer the first vaccines at birth (e.g., Usa, Canada, Australia), and in the first year of infants also vaccines for varicella, hepatitis B (e.g., Usa, Canada, Australia, Japan, etc.) and Japanese encephalitis (e.g., Japan and South Korea). These results are important for health policymakers. They suggest that revisiting vaccine scheduling—such as delaying certain doses beyond 3 months and reducing the concentration of vaccines in the first year—could be a prudent strategy, especially for at-risk infants. Countries in the Protective Policy Cluster (e.g., Norway, Denmark, Finland) demonstrate lower autism rates and less intensive vaccine schedules, offering potential models for safer immunization practices. In short, while vaccines are essential for preventing infectious diseases, this study highlights the need for revising immunization program schedules, reducing vaccine intensity in the first year, and more personalized and developmentally sensitive vaccine policies. Future research should also explore biological mechanisms related to fragile immune system in infants and long-term outcomes to better understand how vaccine intensity and timing may interact with neurodevelopmental disorders.
4.2. Contribution of This Study for Improving Public Health Policy in Vaccination Schedules
This study makes a significant contribution to public health by identifying a statistically significant association between early-life vaccine intensity and national autism rates. One of the key policy-relevant findings is that delaying the administration of certain vaccines beyond the first 3 months, and reducing the number of vaccines in the first year, may help mitigate autism risk—particularly in vulnerable populations. This approach aligns with best practices observed in Nordic countries, where vaccine schedules are more spaced out and autism rates are comparatively lower. Importantly, the study also opens the perspective to considering sex differences in autism prevalence. Research such as Loomes et al. (2017) have shown that males are significantly more likely to be diagnosed with autism than females, suggesting that biological susceptibility may differ by sex. This implies that vaccine scheduling could be further personalized, with greater caution applied to male infants who have an immune system with some natural differences compared to female infants and may be more neurologically sensitive during early development.
Hence, for policymakers, the implications for public health policies can be:
Reassess vaccine schedules to reduce vaccine intensity in the first year of life.
Delay non-critical vaccines until after 4–6 months, when the infant immune system is more mature.
Monitor sex-specific responses to vaccine exposure and consider tailored approaches.
Adopt best practices from countries with lower autism rates and more gradual immunization schedules.
By integrating these findings into public health strategies, governments can maintain high immunization coverage while potentially reducing autism risk—supporting both infectious disease prevention and neurodevelopmental health.
5. Conclusions and Prospects
This study offers a critical contribution to the ongoing discourse on vaccine safety and neurodevelopment by identifying a statistically significant association between early-life vaccine intensity and national autism rates. Its findings challenge conventional assumptions and open new perspective of vaccination policies in infants for thinking about how vaccines are administered to infants under one year of age. Traditionally, vaccine schedules have prioritized early protection against infectious diseases, with many doses concentrated in the first 1 to 12 months of life. While this approach has been effective in reducing morbidity and mortality from preventable illnesses (Nath, 2023), the study suggests that such intensity may have unintended neurodevelopmental consequences—particularly in countries like the United States and Japan, which show both high vaccine counts and elevated autism rates. By comparing countries with different vaccine schedules and autism prevalence, the research highlights the potential benefits of delaying certain vaccines beyond the first 3 months and reducing the number of vaccines administered in the first year. Countries such as Norway and Finland, which follow more gradual immunization schedules, demonstrate lower autism rates and may serve as models for best practices in health policies of immunization program schedule. These findings, of course, do not argue against vaccination but rather advocate for more developmentally sensitive scheduling, especially during the critical early months of immune system and brain development. Moreover, the study encourages a shift toward personalized vaccine strategies. Recognizing that autism prevalence differs by sex—with males being more frequently diagnosed (Loomes et al., 2017)—it suggests that vaccine timing might be tailored to account for biological susceptibility. This could involve closer monitoring of male infants or adjusting schedules based on individual risk factors such as prematurity or family history of neurodevelopmental disorders. In essence, the larger significance of this research lies in its potential to inform safer, more effective vaccine policies. The study suggests a balanced approach that maintains high immunization coverage while minimizing neurodevelopmental risks. This paradigm shift in vaccination policies for infants less than 1 year could lead to improved public trust, better health outcomes, and more responsive public health systems (Chaufan and Hemsing, 2024; Benati and Coccia, 2022; Kargı et al., 2023; Kargı, and Coccia, 2024; Magazzino et al., 2022; Coccia, 2022, 2023).
5.1. Theoretical Implications of This Study for Improving National Immunization Schedules
This study offers important theoretical implications for the global generalization of vaccine scheduling practices, particularly in the context of reducing autism incidence. By identifying a statistically significant association between early-life vaccine intensity and national autism rates, it challenges the one-size-fits-all approach to infant immunization and encourages a more developmentally sensitive framework. Countries like Norway and Finland serve as exemplary models. They maintain high vaccination coverage while administering fewer vaccines and doses to infants under one year of age. Their schedules are more gradual, often delaying non-critical vaccines until after 4–6 months, allowing the infant immune and neurological systems more time to mature. These countries also report lower autism rates, suggesting that their policies may offer a protective effect. The theoretical implication is that timing and concentration of vaccine exposure—not just coverage—are critical variables in shaping neurodevelopmental outcomes. Generalizing these findings worldwide implies a shift toward adaptive vaccine scheduling, where immunization programs are tailored to the developmental needs of infants. This includes:
Delaying certain vaccines beyond the first 3 months, especially for non-life-threatening diseases.
Reducing the number of vaccines administered in the first year, without compromising overall protection.
Considering sex-based biological differences, as males are more frequently diagnosed with autism (Loomes et al., 2017), suggesting a need for differentiated scheduling or monitoring.
Such a framework supports a precision public health approach, integrating epidemiological data, developmental science, and international best practices for public health. It encourages policymakers to move beyond rigid schedules and adopt flexible, evidence-based strategies that prioritize both infectious disease prevention and neurodevelopmental safety. Hence, this study lays the groundwork for a global rethinking of vaccine administration in infancy—one that balances efficacy with developmental sensitivity, and promotes long-term health outcomes across diverse populations.
5.2. Health Policy Implications of This Study
These findings have significant implications for basic public health policy:
Reevaluating Vaccine Schedules: While vaccines are essential for preventing infectious diseases (Nath, 2023), the timing and intensity of early-life immunizations may need reconsideration. Personalized schedules that account for individual risk factors—such as prematurity or family history of neurodevelopmental disorders—could mitigate potential adverse effects (Pichichero, 2014; Sadeck and Kfouri, 2023, Shattock et al., 2024).
International Benchmarking: Countries with a protective policy in figure 1 (e.g., Norway, Denmark, Finland) may serve as models for balancing effective immunization with lower autism prevalence. Policymakers can learn from these systems to optimize vaccine delivery.
Targeted Monitoring: Countries in transitional area of figure 1, like Italy and the UK, should be closely observed for trends in autism incidence. Early intervention and policy adjustments may prevent convergence toward higher-risk profiles.
Overall, then, the findings of this study have important implications for health policy, particularly in the context of vaccine scheduling and neurodevelopmental safety. The statistically significant association between early-life vaccine intensity and national autism rates suggests that current immunization schedules—especially those concentrated in the first year of life—may benefit from reassessment. Countries like the United States, Australia and Japan, which administer a high number of vaccines to infants under one year, also report elevated autism rates. In contrast, countries such as Norway and Finland, which follow more gradual vaccine schedules, show lower autism prevalence, indicating a potential protective effect. These results support a policy shift toward developmentally sensitive vaccine scheduling, including delaying non-critical vaccines until after 4–6 months and reducing the number of vaccines administered in the first year. Such adjustments could help mitigate potential neurodevelopmental risks while maintaining high immunization coverage. Nath (2023) calls for coordinated global action involving manufacturers, healthcare agencies, scientists, and legislators to investigate vaccine-related neurological adverse events and develop preventive and therapeutic strategies. This study reinforces Nath’s (2023) call by providing empirical evidence that could guide such collaborative efforts. Health policymakers should consider integrating these findings into national immunization programs, promoting flexible, evidence-based schedules that prioritize both infectious disease prevention and neurodevelopmental health. Enhanced surveillance, transparent communication, and international cooperation will be essential to ensure vaccine safety and public trust.
5.3. Limitations and Future Prospects
While this study provides compelling evidence of a statistically significant association between early-life vaccine intensity and national autism rates, some limitations must be acknowledged.
First, the study relies on aggregate national data, which may obscure important individual-level variations. Autism diagnosis rates can be influenced by differences in healthcare access, diagnostic criteria, cultural attitudes, and reporting practices across countries. These factors may confound the observed associations and limit the generalizability of the findings. Second, the study does not establish causality. Although strong correlations were found between vaccine dose intensity and autism rates, these do not confirm a direct causal relationship. Autism is a multifactorial condition influenced by genetic, environmental, and developmental factors (Talantseva et al., 2023; Grosvenor et al., 2024), and vaccine exposure may be one of many interacting variables. Third, the study does not include longitudinal data, which would be necessary to track developmental outcomes over time and assess delayed effects of early-life vaccine exposure.
Future studies should focus on Controlled studies that examine vaccine timing, dose concentration, and composition in relation to neurodevelopmental markers; Sex-specific analyses, given known differences in autism prevalence (Loomes et al., 2017); Integration with surveillance systems, as Nath (2023) recommends, to investigate vaccine-related neurological events and guide safer immunization practices. Such research would strengthen the evidence base and support more personalized, developmentally sensitive vaccine policies worldwide.
To conclude, this study provides statistically significant evidence of a positive association between early-life vaccine intensity and national autism rates, suggesting that vaccine scheduling may play a role in neurodevelopmental outcomes. While causality is not established, the findings support a reconsideration of current immunization practices, especially in countries with high autism prevalence and intensive early-life vaccine schedules. As Miravalle and Schreiner (2014) emphasize, distinguishing between temporal associations and causal links is essential to address public misperceptions and guide responsible health policy. In this context, this research contributes to that effort by offering data-driven insights that can inform safer, developmentally sensitive vaccine strategies for public health policies in nations and worldwide.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table 1A. Descriptive statistics, Log scale, N=12 Countries.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could influence the work reported in this paper. No funding was received for this study.
References
- American Psychiatric Association, 2022. Diagnostic and statistical manual of mental disorders: DSM-5-TR (5th edition, text revision). Washington, DC: American Psychiatric Association Publishing, 2022.
- Australia (2025) Australian Government, Department of Health, Disability and Ageing, National Immunization Program for children, https://www.health.gov.au/topics/immunisation/when-to-get-vaccinated/national-immunisation-program-schedule. https://www.health.gov.au/sites/default/files/2025-09/national-immunisation-program-schedule_0.
- Benati, I. ,Coccia M. 2022. Global analysis of timely COVID-19 vaccinations: improving governance to reinforce response policies for pandemic crises. International Journal of Health Governance, vol. 27, No. 3, pp. 240-253. [CrossRef]
- Canada (2025), Government of Canada, Recommended immunization schedules: Canadian Immunization Guide. https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-1-key-immunization-information/page-13-recommended-immunization-schedules.
- Çatlı, Nermin Eylül, Özyurt, Gonca 2025. The relationship between autism and autism spectrum disorders and vaccination: review of the current literature, Trends in Pediatrics. Review. [CrossRef]
- CDC 2025. Data and Statistics on Autism Spectrum Disorder, May 27. https://www.cdc.gov/autism/data-research/index.html#cdc_data_surveillance_section_3-cdcs-addm-network.
- Chaufan, C. , Natalie Hemsing. 2024. Is resistance to Covid-19 vaccination a “problem”? A critical policy inquiry of vaccine mandates for healthcare workers[J]. AIMS Public Health, 2024, 11(3): 688-714. [CrossRef]
- Coccia, M. 2016. Problem-driven innovations in drug discovery: co-evolution of the patterns of radical innovation with the evolution of problems, Health Policy and Technology, vol. 5, n. 2, pp. 143-155. [CrossRef]
- Coccia, M. 2021. Effects of human progress driven by technological change on physical and mental health, STUDI DI SOCIOLOGIA, 2021, N. 2, pp. [CrossRef]
- Coccia, M. 2022. Optimal levels of vaccination to reduce COVID-19 infected individuals and deaths: A global analysis. Environmental Research, vol. 204, Part C, number 112314. [CrossRef]
- Coccia, M. 2023. COVID-19 Vaccination is not a Sufficient Public Policy to face Crisis Management of next Pandemic Threats. Public Organiz Rev 23, 1353–1367. [CrossRef]
- Coccia, M. , Bellitto M. 2018. Human progress and its socioeconomic effects in society, Journal of Economic and Social Thought, vol. 5, n. 2, pp. [CrossRef]
- Denmark (2025). Statens Serum Institut. Childhood vaccination programme. https://en.ssi.dk/vaccination/the-danish-childhood-vaccination-programme.
- Doja A, Roberts W. 2006. Immunizations and autism: a review of the literature. Can J Neurol Sci. 2006 Nov;33(4):341-6. [CrossRef] [PubMed]
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. 2015. Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. J Am Acad Child Adolescent Psych 2015; 54: 580–87.
- Finland (2025). Finnish Institute for Health and Welfare. Vaccination programme for children and adults. https://thl.fi/en/topics/infectious-diseases-and-vaccinations/information-about-vaccinations/vaccination-programme-for-children-and-adults.
- Global Burden of Disease Study 2021 Autism Spectrum Collaborators. The global epidemiology and health burden of the autism spectrum: findings from the Global Burden of Disease Study 2021. Lancet Psychiatry. 2025 Feb;12(2):111-121. [CrossRef]
- Grosvenor LP, Croen LA, Lynch FL, Marafino BJ, Maye M, Penfold RB, Simon GE, Ames JL. Autism Diagnosis Among US Children and Adults, 2011-2022. JAMA Netw Open. 2024 Oct 1;7(10):e2442218. [CrossRef]
- Gulati S, Sharawat IK, Panda PK, Kothare SV. The vaccine-autism connection: No link, still debate, and we are failing to learn the lessons. Autism. 2025 Jul;29(7):1639-1645. [CrossRef]
- Howlin P, Magiati I.2017. Autism spectrum disorder: outcomes in adulthood. Curr Opin Psychiatry 2017; 30: 69–76.
- Italy (2025), Regione Lombardia, Calendario Vaccinale, https://www.wikivaccini.regione.lombardia.it/wps/portal/site/wikivaccini/DettaglioRedazionale/vaccinazioni-disponibili/calendario-vaccinale.
- Japan (2025). Changes in the Immunization Schedule Recommended by the Japan Pediatric Society, , 2025, https://www.jpeds.or.jp/uploads/files/20250205_Immunization_Schedule_english.jp/uploads/files/20250205_Immunization_Schedule_english.pdf.
- Kargı, B. , Coccia M., Bekir Cihan Uçkaç 2023. How does the wealth level of nations affect their COVID19 vaccination plans? Economics, Management and Sustainability. 8(2): 6-19. [CrossRef]
- Kargı, B. Coccia M., 2024. Rethinking the Role of Vaccinations in Mitigating COVID-19 Mortality: A Cross-National Analysis. KMÜ Sosyal ve Ekonomik Araştırmalar Dergisi, KMU Journal of Social and Economic Research 26(47), 1173-1192. [CrossRef]
- Lai JKY, Weiss JA. 2017. Priority service needs and receipt across the lifespan for individuals with autism spectrum disorder. Autism Res 2017; 10: 1436–47.
- Loomes, R. , Hull, L., & Mandy, W. P. L. (2017). What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 56(6), 466–474. [CrossRef]
- Lord C, Charman T, Havdahl A, et al. 2022. The Lancet Commission on the future of care and clinical research in autism. Lancet 2022; 399: 271–334.
- Magazzino, C. , Mele M., Coccia M. 2022. A machine learning algorithm to analyze the effects of vaccination on COVID-19 mortality. Epidemiology and infection, 1–24. [CrossRef]
- Miravalle AA, Schreiner T. 2014. Neurologic complications of vaccinations. Handb Clin Neurol. 2014;121:1549-57. [CrossRef] [PubMed]
- Coccia, M. 2023. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency[J]. AIMS Public Health, 2023, 10(1): 145-168. [CrossRef]
- Moye, R. , Antonius Skipper, Tangela Towns, Daniel Rose. 2022. Attitudes toward vaccines during the COVID-19 pandemic: results from HBCU students[J]. AIMS Public Health, 2022, 9(1): 155-172. [CrossRef]
- Nath, A. 2023. Neurologic Complications With Vaccines: What We Know, What We Don't, and What We Should Do. Neurology. 2023 Oct 3;101(14):621-626. [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. 2025. The Comprehensive Autism Care Demonstration: Solutions for Military Families. Washington, DC: The National Academies Press. [CrossRef]
- Norway (2025). Norwegian Institute of Public Health. Vaccination of children in Norway. [Internet]. Oslo: The Norwegian Directorate of Health; updated Thursday, , 2024 [retrieved Friday, October 3, 2025]. Available from: https://www.helsenorge.no/en/information-in-english/vaccination-of-children/ and https://www.fhi.no/en/va/childhood-immunisation-programme/when-will-your-child-be-offered-vaccines/.
- Pichichero, ME. 2014. Challenges in vaccination of neonates, infants and young children. Vaccine. 2014 Jun 30;32(31):3886-94. [CrossRef]
- Principi N, Esposito S. 2018. Aluminum in vaccines: Does it create a safety problem? Vaccine. 2018 Sep 18;36(39):5825-5831. [CrossRef]
- Coccia, M. 2021. Pandemic Prevention: Lessons from COVID-19. Encyclopedia, vol. 1, n. 2, pp. 433-444. [CrossRef]
- Coccia, M. 2022. Improving preparedness for next pandemics: Max level of COVID-19 vaccinations without social impositions to design effective health policy and avoid flawed democracies. Environmental Research, vol. 213, 22, n. 113566. [CrossRef]
- Ramachandran P, Grose C. 2024. Serious neurological adverse events in immunocompetent children and adolescents caused by viral reactivation in the years following varicella vaccination. Rev Med Virol. 2024 May;34(3):e2538. [CrossRef]
- Rebecchi, K. 2025. Beyond “autism spectrum disorder”: toward a redefinition of the conceptual foundations of autism[J]. AIMS Medical Science, 2025, 12(2): 193-209. [CrossRef]
- Reuters 2025. Autism rates: Why are they on the rise. By Nancy Lapid, . https://www.reuters.com/business/healthcare-pharmaceuticals/why-are-autism-rates-rising-2025-01-14/.
- Sadeck LDSR, Kfouri RÁ. 2023. An update on vaccination in preterm infants. J Pediatr (Rio J). 2023 Mar-Apr;99 Suppl 1(Suppl 1):S81-S86. [CrossRef]
- Sandbank M, Bottema-Beutel K, Crowley LaPoint S, et al. Autism intervention meta-analysis of early childhood studies (Project AIM): updated systematic review and secondary analysis. BMJ 2023; 383: e076733.
- Scientific American 2017. The Real Reasons Autism Rates Are Up in the U.S. By Jessica Wright & Spectrum, , https://www.scientificamerican.com/article/the-real-reasons-autism-rates-are-up-in-the-u-s/#.
- Shattock, Andrew J et al. 2024. Contribution of vaccination to improved survival and health: modelling 50 years of the Expanded Programme on Immunization, The Lancet, Volume 403, Issue 10441, 2307 - 2316.
- Singapour (2025) Government of Singapore, Communicable Diseases Agency, Vaccinations, Table 1: National Childhood Immunisation Schedule, https://www.cda.gov.sg/public/vaccinations and https://isomer-user-content.by.gov.sg/18/00b7fdea-24a1-4c26-b67e-d6618f31d6cb/NCIS_Sept%202025.pdf.
- South Korea (2025). Vaccination for infants, Yangcheon-Gu Office, Seul, https://www.yangcheon.go.kr/english/english/04/10402030000002016110903.jsp and https://www.gunsan.go.kr/_cms/board/eFileDownload/434/1449916/12b2c60c49317fc21ea41eb435a79159.
- Sweden (2025). Vaccination programmes. The Public Health Agency of Sweden, https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/vaccinations/vaccination-programmes/ (Accessed October, 2025).
- Swedish Council on Health Technology Assessment. Vaccines to Children: Protective Effect and Adverse Events: A Systematic Review [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2009 Feb. SBU Yellow Report No. 191. [PubMed]
- Talantseva OI, Romanova RS, Shurdova EM, Dolgorukova TA, Sologub PS, Titova OS, Kleeva DF and Grigorenko EL (2023) The global prevalence of autism spectrum disorder: A three-level meta-analysis. Front. Psychiatry 14:1071181. [CrossRef]
- Tomljenovic L, Shaw CA. 2011. Do aluminum vaccine adjuvants contribute to the rising prevalence of autism? J Inorg Biochem. 2011 Nov;105(11):1489-99. [CrossRef] [PubMed]
- UK (2025). NHS vaccinations and when to have them, https://www.nhs.uk/vaccinations/nhs-vaccinations-and-when-to-have-them/ (Accessed October, 2025).
- USA (2025). CDC, Vaccines & Immunizations, Child and Adolescent Immunization Schedule by Age (Addendum updated , 2025), https://www.cdc.gov/vaccines/hcp/imz-schedules/child-adolescent-catch-up.html; https://www.cdc.gov/vaccines/hcp/imz-schedules/downloads/child/0-18yrs-child-combined-schedule.
- Vazquez JA, Rao ASRS. 2025 Immunizations, Autism, and Statistical Analysis. Am J Med. 2025 Sep;138(9):1175-1176. [CrossRef] [PubMed]
- World Population Review (2025), Autism Rates by Country 2025, https://worldpopulationreview.com/country-rankings/autism-rates-by-country.
- World Population Review (2025a), Vaccination Rates by Country 2025, https://worldpopulationreview.com/country-rankings/vaccination-rates-by-country.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).