1. Introduction
Burnout, a syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment, is a well-documented issue among healthcare workers, with profound implications for both patient outcomes and workforce retention [
1,
2]. Chronic workplace stress, exacerbated by factors such as long hours, high workloads, and insufficient support, contributes significantly to burnout, which in turn has been linked to decreased quality of care, increased medical errors, and organizational inefficiencies [
2,
3,
4]. Even before the COVID-19 pandemic, burnout among health care providers was a growing concern [
3,
5].
The onset of the COVID-19 pandemic intensified these challenges, placing unprecedented demands on health care systems worldwide. In response to surging patient volumes, hospitals implemented strategies such as redeployment of staff and increased nursing-to-patient ratios to address workforce shortages [
6,
7]. Redeployment, while necessary during crises, often involves shifting staff to unfamiliar roles with minimal notice and limited training, increasing stress and the likelihood of burnout [
8,
9,
10,
11]. Research has shown that redeployment during the COVID-19 pandemic was associated with heightened emotional exhaustion, anxiety, and depressive symptoms among health care workers [
8,
12,
13,
14,
15].
Monitoring the true prevalence and impact of burnout can be challenging. Innovative tools, such as real-time ecological momentary assessments (EMA), have emerged as potential solutions. EMA is a real-time data collection survey tool that captures people’s experiences and emotions as they occur in their natural environment, providing a more accurate and detailed understanding than traditional surveys. Such a tool minimizes recall bias and provides detailed insights into the fluctuations of emotional states and stress levels, making it particularly valuable in dynamic, high-pressure environments like those encountered during public health emergencies [
16,
17]. Further, EMA utilizes real-time measures to identify at-risk individuals and generates actionable data to inform timely and targeted interventions [
18,
19,
20,
21].
The use of EMA and automated platforms like Qualtrics or REDCap remains underutilized in health care workforce studies, despite their ability to efficiently and repeatedly distribute questionnaires to participants. Most existing research on burnout has relied on cross-sectional or short-term longitudinal designs, which fail to capture the nuanced and evolving interplay of factors like redeployment, workload, and support systems over extended periods [
4,
18,
22]. Additionally, many studies focus on the immediate impacts of crises, neglecting the sustained effects of stress and burnout. This creates critical gaps in understanding burnout trajectories both during and after public health emergencies, knowledge essential for designing targeted interventions for high-risk groups.
Our study leverages EMA to examine burnout trajectories among health care workers, focusing on the roles of redeployment and caseload. Conducted during the first year of the COVID-19 pandemic, this intensive longitudinal study uniquely evaluates how burnout evolves over time and how specific factors exacerbate or mitigate its effects. By combining frequent, real-time data collection with a robust analysis of workforce dynamics, this research aims to demonstrate the value of EMA in enhancing disaster preparedness and workforce resilience strategies.
2. Materials and Methods
2.1. Design
This observational study employed an ecological momentary assessment in an intensive longitudinal survey design to examine the effects of redeployment on burnout among health care workers during the first year of the COVID-19 pandemic. Extending previous analyses, this study assessed variations in burnout when participants worked in their usual roles versus when they were redeployed. Redeployment was defined as assignment to a role or location outside the participant’s typical scope of work [
12,
13]. Details of our data collection methodology and full Frontline Well-being survey are published in Pan et al [
18]. Eligible participants included physicians, physician assistants, nurses, and trainees, with no specific exclusion criteria.
2.2. Data Collection
A 12-item EMA survey instrument, designed to be brief and simple, measured key dimensions of burnout, including emotional exhaustion and workload perceptions, and took approximately one minute to complete. Surveys were administered every five days from April 14, 2020–March 31, 2021, resulting in 70 assessments of redeployment status and burnout. The Qualtrics platform was used to email surveys to clinical staff hospital-wide. Participants received daily reminders to complete the initial survey and two reminders for each additional survey.
2.2.1. Demographic and Professional Information
Items inquired about demographics (i.e., age, sex, race/ethnicity, and marital status) and professional information (i.e., professional role, department, and years of practice). One item asked if participants had worked in a clinical capacity within the past 24 hours.
2.2.2. Redeployment
To assess redeployment status, a single item asked if participants were currently working outside their usual professional role and coded as “Redeployment Status”. We created two additional variables. On an observation level, we created a new variable labeled “Pre vs Post Redeployment”, which permitted us to identify before and after redeployment periods. At a person level, a variable “Redeployment Group” was coded if participants were ever redeployed over the course of the study period.
2.2.3. Burnout
Burnout was assessed with the Dolan et al. (2015) single item validated measure of burnout in health care workers.23 Participants chose from 5 answers with responses ranging from no burnout to potentially debilitating burnout [
24].
2.2.4. Caseload and Case Severity
Hospital administration provided information about the daily Department of Medicine census, COVID-19-related caseload, and the number of COVID-19 patients receiving critical care. Caseloads were calculated using the average number of COVID-19 cases over a rolling period of five days (PROC EXPAND, SAS 9.4).
2.2.5. Participant Comments
In addition to the quantitative survey, the participants were asked if they had any additional comments and given the option to provide a written text response. These comments were analyzed for common themes to help provide a richer context around the interplay between the COVID-19 pandemic, redeployment, professional roles, and resultant burnout.
2.3. Data Analysis-Survey
We conducted a multilevel mixed regression analysis (MMLM) (PROC GLIMMIX, SAS 9.4) to examine how professional role, caseload, and redeployment were associated with burnout. Additional details about the analytic approach, including model specifications and transformations, are available in the
Supplementary Materials. Predictors in the model included redeployment status, caseload, and professional role, along with their interactions. The final model included significant effects only.
2.4. Data Analysis-Comments
A total of 479 comments from 143 distinct participants were collected over the course of the study. We did not obtain permission to publish the comments verbatim, so all references to comments in this paper will not include direct quotations. Each comment underwent content analysis and was categorized by its main topics. To ensure the accuracy of our analysis, two team members separately reviewed all comments. This approach follows methodologies used in previously published research [
25].
3. Results
3.1. Characteristics of the Sample
As previously reported, a total of 398 participants completed the initial survey. Almost 81% (n = 322) completed the survey multiple times.18 On average, participants completed 12 surveys (median = 5), yielding a total of 5,070 surveys over one year. Of the 398 participants, 94% (n = 372) provided data on burnout. There were no significant associations between the number of surveys a participant completed and their burnout scores. Participants completing the survey more than once did not significantly differ from those who completed the survey only once on any demographic or professional role variables.
3.2. Demographic Data
Nursing and nurse practitioners comprised the largest group in the sample (55.6%, n = 221), followed by attending physicians (22%, n = 87), trainees (residents and fellows) (15%, n = 60), and physician assistants (11%, n = 44). The study population was primarily self-identified women (70%, n = 277), with 79% (n = 306) under the age of fifty. Demographically, the study population mirrored the institute’s workforce diversity. The majority identified as Asian (44.3%, n = 171), followed by White (37.5%, n = 145), Black (10.4%, n = 40), and Latino (7.8%, n = 30). Most participants had less than five years of experience (41.2%, n = 164).
3.3. Redeployment
Of the 398 participants, 58.52% were redeployed during at least one of their survey responses (n = 230) and 41.48% were never redeployed (n = 163) and 5 were missing redeployment data. About 10% of participants were redeployed during all survey responses (n = 37). There were no statistically significant differences in age (P = .86), gender (P = .59), professional role (P = .17) or hospital department (P = .62) between those who were ever redeployed and those who were never redeployed.
Redeployment and Burnout
Our prior analyses (see Pan et al, 2023) indicated that age, gender, professional role, and caseload served as significant predictors of burnout.18 Therefore, in the current analyses, we included these variables as initial covariates. The final model obtained from multilevel mixed semi-linear regression analyses estimating the relationship between redeployment and burnout is shown in
Appendix A. Effects not found to be significant in prior analyses were removed from the final model.
3.4. Analyses
3.4.1. Role-Specific Burnout Trends
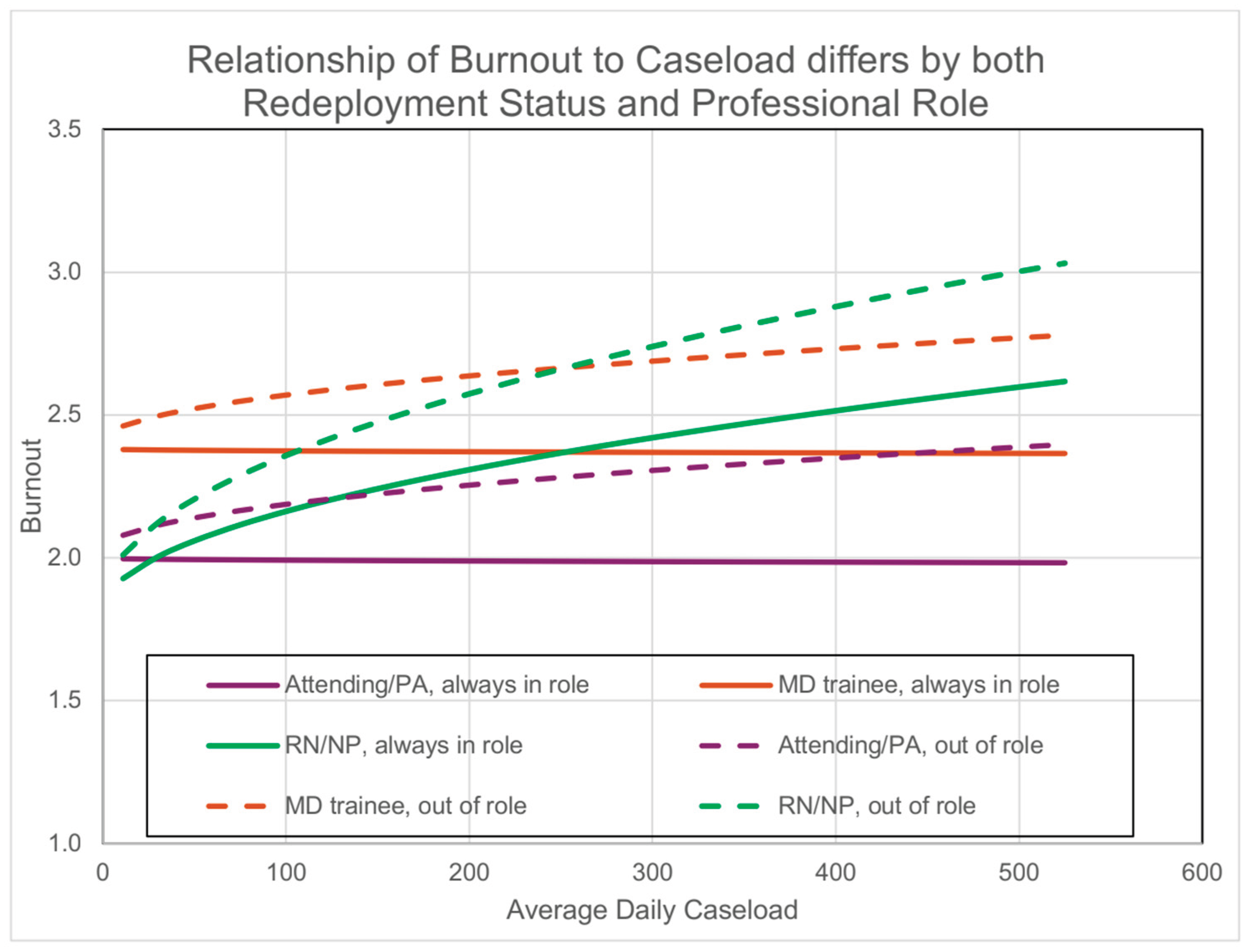
As shown in
Figure 1, the relationship between burnout and caseload differed significantly by both redeployment status and professional role. Nurses experienced a significant increase in burnout as caseloads rose (b = 0.3591; SE = 0.0746; P < .0001), an effect not observed in other professional roles.
3.4.2. Combined Impact of Caseload and Redeployment
Caseload moderated the effect of redeployment on burnout. As caseloads increased, the positive relation between redeployment and burnout increased (b = 0.1691; SE = 0.0491; P = .001). The combination of high caseloads and redeployment was associated with the most pronounced burnout levels across all participants. This effect did not vary by professional role.
3.4.3. Long-Term Burnout Effects of Redeployment
Burnout levels were significantly higher after participants' initial redeployment compared to the period before redeployment (b = 0.1251; SE = 0.0488; P = .010). This effect persisted regardless of whether participants returned to their usual roles and was consistent across all professional roles.
3.5. Analysis of Comments
During the data collection period, approximately one-third of participants (35.9%, n = 143) provided at least one comment, resulting in a total of 479 comments. The most prevalent themes are outlined in
Table 1, with 17.75% (n = 85) of all comments directly addressing redeployment-related concerns.
Analysis of redeployment-related comments highlighted several critical challenges that clinicians experienced during redeployment. These included:
Being reassigned to unfamiliar roles with minimal notice.
Insufficient training for redeployed responsibilities.
Lack of guidance regarding policies and procedures on new units.
Concerns about personal safety in less familiar environments.
These comments provide qualitative evidence of the stressors captured by the EMA tool, offering deeper insights into the lived experiences driving burnout. For example, participants described feeling “uncomfortable” and “horrible” when thrust into unfamiliar roles without notice. Regarding the lack of training and guidance, participants expressed feeling “outside our comfort zone” and called for “some sort of in-service and/or training” to familiarize them with “equipment, policies, and protocols.”
4. Discussion
This study demonstrates the utility of ecological momentary assessment (EMA) as an innovative and scalable tool for real-time monitoring of burnout among health care workers during crises. It offers a practical and user-friendly solution for real-time monitoring, requiring minimal time investment from participants while delivering more nuanced and actionable insights compared to traditional retrospective surveys. Our use of EMA enabled a capturing of dynamic, temporal variations in burnout in frontline health care workers during the first year of the COVID-19 pandemic. The longitudinal design allowed for the identification of critical patterns, such as the persistent effects of redeployment and the amplifying role of increased caseloads on burnout levels. These findings highlight the power of EMA to deliver actionable data that can guide organizational decision-making.
Participants who experienced redeployment reported higher burnout levels than those who remained in their usual roles, with these effects persisting over time and intensifying when caseloads increased. Redeployment-related burnout often did not resolve even after individuals returned to their original roles, suggesting that redeployment represents a significant stressor with potential long-term impacts [
26,
27]. EMA’s ability to capture these patterns in near real-time offers organizations a critical advantage, enabling early identification of at-risk staff and the implementation of targeted interventions before burnout becomes entrenched, as supported by existing literature [
28].
In addition to burnout trends, EMA allowed the collection of qualitative feedback from participants, which provided deeper context for the observed quantitative findings. Comments highlighted recurring themes, such as the stress of transitioning to new roles with minimal preparation, the lack of formal guidance on new policies and procedures, and concerns for personal safety in unfamiliar environments. These lived experiences underscore the importance of integrating real-time qualitative insights into burnout monitoring efforts, as they can reveal actionable gaps in organizational processes and staff support systems.
This study has several limitations. The initial response rate of approximately 20%, while consistent with similar studies involving voluntary clinician participation, was accompanied by participant attrition over the study period [
3]. This declining response rate could affect the reliability of longitudinal findings. Despite its strengths, the use of EMA is not without challenges, including the potential for survey fatigue among participants due to frequent data collection. Further, the complex nature of EMA results creates large datasets that require advanced statistical methods and specialized expertise to analyze effectively.
The single-site design and convenience sampling method may restrict the generalizability of the results of the survey to other health care systems or disaster scenarios. Additionally, the absence of baseline burnout data collected prior to the pandemic limits our ability to fully attribute observed burnout trends to the pandemic itself. Finally, while the inclusion of participant comments adds depth to the study, a more robust qualitative approach, such as structured interviews or focus groups, could have provided additional context and enhanced understanding of the lived experiences of health care workers.
Future research should explore the application of EMA informed interventions across diverse health care settings and crisis scenarios, assessing its utility in contexts such as natural disasters or prolonged humanitarian emergencies. Additionally, studies should investigate the long-term effectiveness of EMA-informed interventions in reducing burnout and supporting workforce resilience over time. By leveraging the capabilities of EMA, health care systems can build more adaptive, responsive, and sustainable approaches to disaster preparedness and workforce management.
5. Conclusions
This study highlights the critical role of real-time monitoring tools, such as ecological momentary assessment (EMA), in identifying and addressing burnout among health care workers during crises. The findings demonstrate that redeployment, while necessary in emergency scenarios, is associated with persistent increases in burnout, particularly when compounded by high caseloads. Importantly, EMA's ability to capture nuanced, real-time data on burnout provided actionable insights into the temporal and contextual factors exacerbating stress among health care workers. These insights emphasize the need for proactive strategies to mitigate the immediate and long-term effects of redeployment and workload surges.
To enhance workforce resilience and ensure operational readiness during future crises, health care organizations should consider the following actionable recommendations:
Adopt Real-Time Monitoring: Implement EMA or similar tools to continuously track staff well-being and burnout during emergencies. These tools enable the early identification of at-risk individuals and allow for dynamic, data-driven interventions tailored to evolving conditions.
Develop Redeployment Protocols: Establish structured protocols that include preemptive training, clear role-specific guidance, and organized hand-off processes to reduce the stress of sudden redeployment, allowing for dynamic caseload adjustments during surges.
Integrate Mental Health and Peer Support Programs: Provide accessible mental health resources and establish peer support networks to address the emotional challenges associated with redeployment and high workloads. These programs should be sustained beyond crises to support long-term workforce well-being.
Enhance Organizational Communication: Maintain consistent and transparent communication channels to disseminate updates on policies, expectations, and available resources. Clear communication fosters trust and reduces uncertainty during crises.
Expand Professional Development Opportunities: Offer cross-training and professional development programs to prepare staff for redeployment scenarios. Building skills across roles can ease transitions during emergencies and reduce stress by fostering confidence in diverse responsibilities.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, C.P. and E.B.; data curation, A.A., C.P., A.M., and E.B.; formal analysis, A.A., A.N., C.P., R.C., J.E.S., and E.B.; investigation, C.P., P.A., and E.B.; visualization, J.E.S. and A.M.; writing—original draft preparation, A.A., A.N., C.P., R.C., and E.B.; writing—review and editing, P.A., J.E.S., and E.B.; supervision, E.B.; funding acquisition, P.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Theresa and Eugene Lang Center for Research and Education at NewYork-Presbyterian Queens. Dr Norful is supported by the National Institute of Mental Health, Grant number K08MH130652. The APC was funded by the authors.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of NewYork-Presbyterian/Queens, Lang Research Center (IRB File No. 12820320; expedited review under 45 CFR 46.110/21 CFR 56.110; approval date 9 April 2020; approval through 8 April 2021). No animal subjects were involved.
Informed Consent Statement
Patient consent was waived under 45 CFR 46.116(d) because the survey posed minimal risk, involved no procedures for which written consent is normally required, and used de-identified data; a waiver of HIPAA authorization was also granted. No identifiable patient information is presented; written consent for publication was not required.
Data Availability Statement
Data are available on reasonable request from the corresponding author (E.B.) due to privacy and ethical restrictions. De-identified analytic code and variable definitions will be shared upon request. E.B. has full access to all data and takes responsibility for the integrity and accuracy of the analysis.
Acknowledgments
We would like to acknowledge the St. John’s University Collaborative Health Integration Research Program (CHIRP) data management and recruitment teams; Magdelene Barjolo, Heather Zeluff, Brian Vincent, Skylor Loiseau, Kevin Costa, Rebecca Steele, Alexandra Spinelli, Jeavonna Coble and Luke Keating. Their collective efforts were responsible for building and managing the database used in this study. We would also like to thank Teressa Ju, M.D., Miri Kim, M.D., Michael Siu, M.D. and Sabiha Merchant, M.D. for their recruitment assistance.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations
The following abbreviations are used in this manuscript:
| EMA |
Ecological Momentary Assessment |
| MMLM |
Multilevel mixed-effects model |
| REDCap |
Research Electronic Data Capture |
| SAS |
Statistical Analysis System |
Appendix A
Table A1.
Final Mixed Model Examining Effects of Professional, Redeployment Status at Time of Survey, Redeployment Status Overall on Burnout.
Table A1.
Final Mixed Model Examining Effects of Professional, Redeployment Status at Time of Survey, Redeployment Status Overall on Burnout.
| Effect |
Estimate |
Standard
Error |
DF |
t-Value |
Pr > |t| |
Lower |
Upper |
| Intercept |
2.01 |
1.11 |
1253 |
1.81 |
0.07 |
-0.1739 |
4.1986 |
| Caseloads x 100 |
-0.007 |
0.13 |
1539 |
-0.06 |
0.96 |
-0.2526 |
0.2385 |
Trainee (Resident/Fellow) vs Attending
Physicians
|
0.38 |
0.13 |
368.5 |
2.87 |
0.0043* |
0.1205 |
0.6445 |
| Nurse/NP vs Attending Physicians |
-0.19 |
0.14 |
291.9 |
-1.33 |
0.17 |
-0.4676 |
0.09122 |
| Caseloads x 100 * Nurse/NP vs. all others |
0.36 |
0.075 |
228.2 |
4.82 |
<.0001* |
0.2122 |
0.5061 |
| Sex (Women vs Men) |
0.26 |
0.10 |
351.8 |
2.54 |
0.01 |
0.05794 |
0.4564 |
Redeployment Status
(Out of role at the time of survey completion)
|
-0.099 |
0.063 |
3837 |
-1.56 |
0.12 |
-0.2227 |
0.02529 |
| Caseloads x 100 * Redeployment Status |
0.17 |
0.049 |
3317 |
3.45 |
0.0006* |
0.07285 |
0.2653 |
History of redeployment: Pre vs post periods
of redeployment
|
0.13 |
0.049 |
2223 |
2.56 |
0.0104* |
0.02944 |
0.2208 |
References
- Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555-567. [CrossRef]
- Montgomery AP, Azuero A, Baernholdt M, et al. Nurse burnout predicts self-reported medication administration errors in acute care hospitals. J Healthc Qual. 2021;43(1):13-23. [CrossRef]
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. [CrossRef]
- Dionisi T, Sestito L, Tarli C, et al. Risk of burnout and stress in physicians working in a COVID team: a longitudinal survey. Int J Clin Pract. 2021;75(11):e14755. [CrossRef]
- Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-146. [CrossRef]
- Abate SM, Ahmed Ali S, Mantfardo B, Basu B. Rate of intensive care unit admission and outcomes among patients with coronavirus: a systematic review and meta-analysis. PLoS One. 2020;15(7):e0235653. [CrossRef]
- Satomi E, Souza PMR, Thomé BDC, et al. Fair allocation of scarce medical resources during COVID-19 pandemic: ethical considerations. Einstein (Sao Paulo). 2020;18:eAE5775. [CrossRef]
- Singh V, Young JQ, Malhotra P, et al. Evaluating burnout during the COVID-19 pandemic among physicians in a large health system in New York. Arch Environ Occup Health. 2022;77(10):819-827. [CrossRef]
- Coughlan C, Nafde C, Khodatars S, et al. COVID-19: lessons for junior doctors redeployed to critical care. Postgrad Med J. 2021;97(1145):188-191. [CrossRef]
- Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. n Engl J Med. 2020;382(21):2049-2055. [CrossRef]
- Vera San Juan N, Clark SE, Camilleri M, et al. Training and redeployment of healthcare workers to intensive care units during the COVID-19 pandemic: a systematic review. BMJ Open. 2022;12(1):e050038. [CrossRef]
- Denning M, Goh ET, Tan B, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS One. 2021;16(4):e0238666. [CrossRef]
- Ferry AV, Wereski R, Strachan FE, Mills NL. Predictors of UK healthcare worker burnout during the COVID-19 pandemic. QJM. 2021;114(6):374-380. [CrossRef]
- Piercy H, Kelly S, Wills M, Croston M. Psychological impact of caring during the COVID-19 pandemic on HIV nurses. Br J Nurs. 2022;31(1):S10-S15. [CrossRef]
- Kissel KA, Filipek C, Folz E, Jenkins J. The impact of a three-tiered model of nursing redeployment during the COVID-19 pandemic: a cross-sectional study. Intensive Crit Care Nurs. 2023;77:103431. [CrossRef]
- Doherty K, Balaskas A, Doherty G. The design of ecological momentary assessment technologies. Interact Comput. 2020;32(3):257-278. [CrossRef]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1-32. [CrossRef]
- Pan CX, Crupi R, August P, et al. An intensive longitudinal assessment approach to surveilling trajectories of burnout over the first year of the COVID pandemic. Int J Environ Res Public Health. 2023;20(4):2930. [CrossRef]
- Shea JA, Bellini LM, Desai SV, et al. Exploring residents’ well-being and burnout via qualitative ecological momentary assessment. Acad Med. 2022;97(3):414-419. [CrossRef]
- Mengelkoch S, Moriarity DP, Novak AM, Snyder MP, Slavich GM, Lev-Ari S. Using ecological momentary assessments to study how daily fluctuations in psychological states impact stress, well-being, and health. J Clin Med. 2023;13(1):24. [CrossRef]
- Versluis A, Verkuil B, Spinhoven P, van der Ploeg MM, Brosschot JF. Changing mental health and positive psychological well-being using ecological momentary interventions: a systematic review and meta-analysis. J Med Internet Res. 2016;18(6):e152. [CrossRef]
- Luceño-Moreno L, Talavera-Velasco B, Vázquez-Estévez D, Martín-García J. Mental health, burnout, and resilience in healthcare professionals after the first wave of COVID-19 pandemic in Spain: a longitudinal study. J Occup Environ Med. 2022;64(3):e114-e123. [CrossRef]
- Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582-587. [CrossRef]
- Helfrich CD, Simonetti JA, Clinton WL, et al. The association of team-specific workload and staffing with odds of burnout among VA primary care team members. J Gen Intern Med. 2017;32(7):760-766. [CrossRef]
- Boussat B, Kamalanavin K, François P. The contribution of open comments to understanding the results from the Hospital Survey on Patient Safety Culture (HSOPS): a qualitative study. PLoS One. 2018;13(4):e0196089. [CrossRef]
- Schroeder K, Norful AA, Travers J, Aliyu S. Nursing perspectives on care delivery during the early stages of the COVID-19 pandemic: a qualitative study. Int J Nurs Stud Adv. 2020;2:100006. [CrossRef]
- Norful AA, Rosenfeld A, Schroeder K, Travers JL, Aliyu S. Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. Gen Hosp Psychiatry. 2021;69:20-26. [CrossRef]
- Aiken LH, Lasater KB, Sloane DM, et al. Physician and nurse well-being and preferred interventions to address burnout in hospital practice: factors associated with turnover, outcomes, and patient safety. JAMA Health Forum. 2023;4(7):e231809. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).