1. Introduction
According to the World Health Organization (WHO), children and adolescents are defined as individuals aged 5 to 19 years, which is a key stage of physical and cognitive development that shapes their future wellbeing [
1,
2]. As of 2022, an estimated 390 million children and adolescents worldwide were overweight, and around 190 million suffered from undernutrition [
3,
4]. The double burden of malnutrition (DBM) is characterized by the coexistence of both undernutrition and overnutrition within the same population, within a mother -child pair in the same household or even within the single individual [
5,
6,
7,
8]. DBM is highly prevalent and affecting about one-third of Low- and Middle-Income Countries (LMICs) [
6].
According to The Lancet Commission on DBM, the South Asian region has experienced a persistent burden of undernutrition, while undergoing a simultaneous rise in childhood overweight and obesity[
9]. The coexistence of under- and overnutrition amongst children has become more prevalent in urban areas than the rural areas in this region [
10,
11]. Rapid urbanization in LMICs across South Asia has influenced unhealthy diets, such as processed food and sedentary lifestyle amongst children leading to overnutrition, while low household income limits access to adequate and diverse diet leading to undernutrition in children [
12,
13].
Bangladesh is a LMIC in South Asia undergoing substantial socio-demographic transitions through a rapid urbanization and changes in socio-economic status [
14,
15]. Low parental education and socio-economic inequalities also influence the nutritional landscape among children in urban settings in Bangladesh [
16]. Evidence suggests that undernutrition remains prevalent among poorer households, while overweight and obesity are increasingly observed in wealthier families [
17,
18]. Currently, the prevalence of DBM is 15.8% in urban households, in which mothers with overweight are paired with under-5 children with stunting [
19]. A study conducted in urban Dhaka reported that 16% of children and adolescents were underweight, while 28% were overweight [
20]. However, data on DBM are limited to school-aged children and women of reproductive age in urban settings [
20,
21]. Although prevalence of DBM has been reported to vary across different socio-economic status in South Asia, these estimates are not known for population or household levels [
22,
23]. Further, factors attributing to the high burden of DBM is unknown, although this evidence would be crucial for identifying the most vulnerable groups in a setting with a high burden of undernutrition, such as Bangladesh for designing targeted interventions [
19,
20,
21,
22].
The National Nutrition Services (NNS) in Bangladesh coordinates nutrition policy and integrates services into primary health care through training, capacity-building, supervision, and routine monitoring under the Health, Population and Nutrition Sector Program [
24]. For children, core services include growth monitoring and promotion, infant and young child feeding counseling, vitamin A supplementation, deworming, and management of acute malnutrition. For women, services focus on antenatal nutrition counseling and breastfeeding support alongside iron–folic acid supplementation to prevent and treat anemia delivered through ANC contacts and community health workers [
25]. It is unknown if the current nutrition policies recognize the burden of DBM in Bangladesh and what directions are available for addressing the emerging threat of DBM in Bangladesh. This study presents a secondary analysis of data obtained from the national survey among school age children (5-19 year) in the urban areas in Bangladesh to report the regional variations of DBM and factors contributing to DBM in Bangladesh. Alongside this we present a rapid review of the policy landscape of the current nutrition services in Bangladesh to identify the gaps in national policy targeting DBM.
2. Materials and Methods
2.1. Study Design and Participants
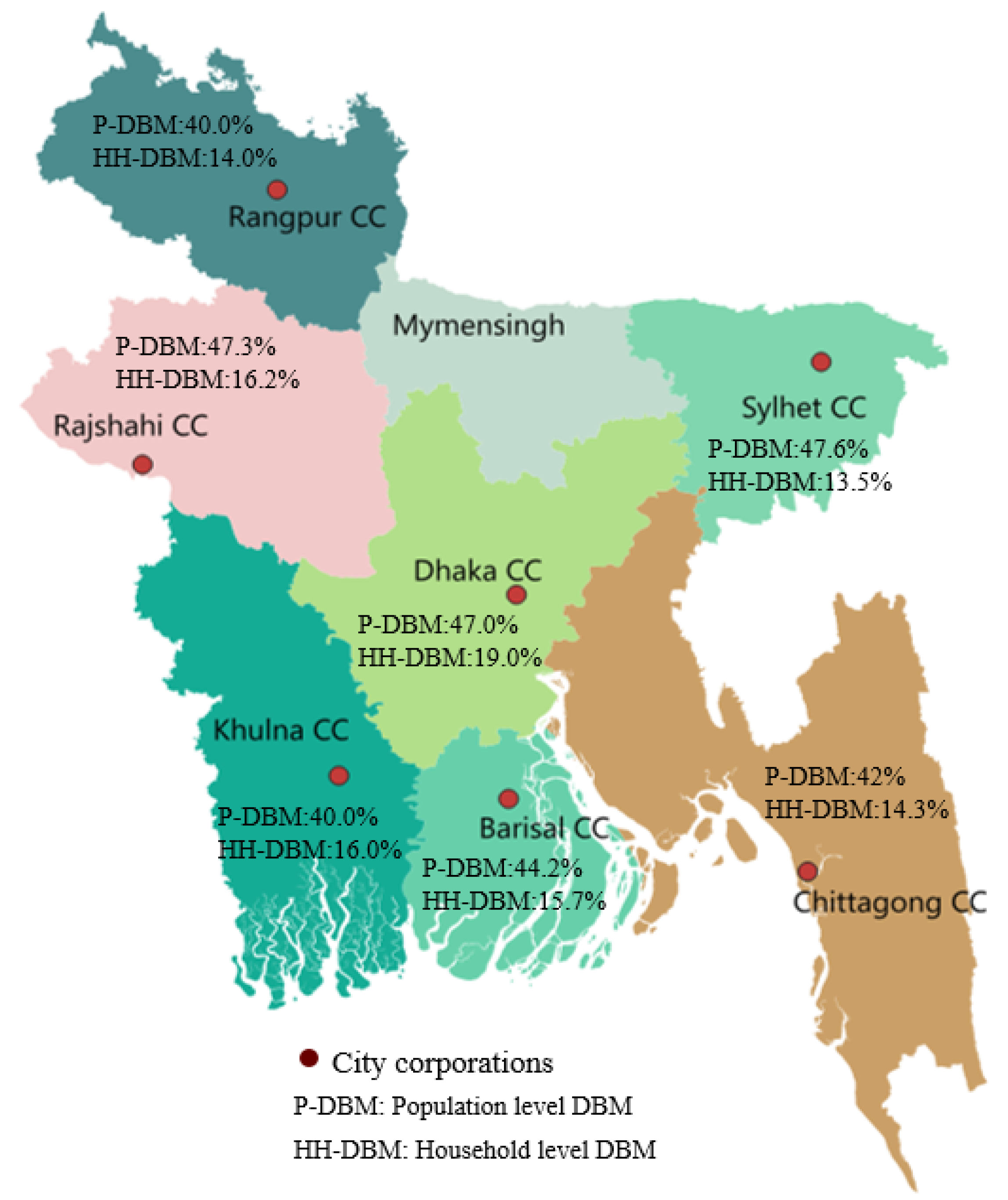
We analyzed the data from the nationwide survey on childhood obesity which was conducted between January and June 2013 by the International Centre for Diarrhoeal Disease Research, Bangladesh (PR#13024) sponsored by the NNS. The survey was conducted in seven city corporation (CC) areas including Dhaka, Chattogram, Rajshahi, Sylhet, Khulna, Barisal and Rangpur divisions (
Table 1 &
Figure 1). Dhaka represents the oldest city corporation established in 1864 and Rangpur is the newest city corporation established in 2012[
26]. Thirty wards (the lowest administrative unit in a CC) out of the total were randomly selected from each CC and all households with a child aged 5–19 years and their biological mothers were listed in order to develop the sampling frame. From each ward, twenty children were randomly selected using the improved WHO Expanded Programme on Immunization (EPI) cluster-sampling approach[
27,
28]. Written consent was obtained from parents or guardians of all participants, and assent obtained from children aged 10–19 years. Any child who lived in a study area for less than six months or did not have a biological mother or had a mother who was too sick to provide consent was excluded from the survey.
Trained research staff used a structured questionnaire to collect data from children on age, sex, school grade completed, parents’ information including education and socio economic status (ownership of durable assets, materials used for the roof, walls, and floor, access to electricity, type of toilet facilities, drinking water sources and types of cooking fuels). In the national survey, height of children and mothers was measured using a wooden stadiometer, and their weight was measured using a Tanita HD-351 digital scale [
29]. Data quality was checked with 5% of the respondents within 24 hours of data collection. All data forms were transported to the designated data management team in icddr,b every week for data entry.
BMI of children was estimated following the International Obesity Task Force (IOTF) reference curves using the standard formula: weight (kg) / height (m²) applying the age and sex specific BMI cut-off values to classify children and adolescents (aged 5–18 years) into underweight (<5th percentile), normal weight (5th–84th percentile), overweight (85th–94th percentile), and obese (≥95th percentile)[
30]. BMI of mothers was classified into underweight (<18.5 kg/m²), normal weight (≥18.5 and <23.0 kg/m²), overweight (≥23.0 and <27.5 kg/m²), and obese (≥27.5 kg/m²) using the WHO recommended Asian BMI cut-off values [
31].
2.2. Data Acquisition and Data Management for Secondary Analyses
The full database was obtained from icddr,b and data were managed by a qualified group of data managers. Age of children was categorized in to two groups (i) 5 to 9 years of age and (ii)10 to 19 years for adolescents following WHO guidelines [
32]. Educational status was categorized into four groups: (1) never attended a school, (2) below primary (completed 1 to 4 grades or attended a pre-school), (3) completed primary (completed 5 to 9 grades), (4) completed secondary (completed 10th to 12th grade) and (5) completed higher secondary (completed 13th grade or above). Low education was defined for those who never attended a school or had an education below primary. Father’s occupation was categorized as service, business and manual workers (rickshaw/van puller/transport worker/migrant worker/agriculture). Mother’s occupation was categorized as housewife and employed (service, business and manual labor). Wealth index (WI) was calculated using principal component analysis (PCA) following the standard guidelines of the Demographic and Health Survey [
33]. The WI variable was then divided into five quintiles to define socioeconomic status: lower quintile (1st 20% of WI), lower-middle quintile (2nd 20% of WI), middle quintile (3rd 20% of WI), upper-middle quintile (4th 20% of WI), and upper quintile (5th 20% of WI).
2.3. Data Analysis
DBM at the population level was defined as the presence of underweight and overweight/obesity among children and adolescents within the same population [
34]. DBM at the household level was defined as the coexistence of maternal overweight/obesity and child undernutrition within the same household [
35,
36]. A binary variable was created with DBM coded as 1 if either population level or a household level DBM was present and 0 otherwise.
Descriptive statistics were used to summarize socio demographic characteristics of the study participants and presented as frequencies and percentages (categorical variables), or means with standard deviations (SD) (continuous variables). The prevalence of DBM at both the population and household levels were reported by percentage with 95% confidence intervals (CIs). Comparison between DBM and key socio-demographic factors including age of children, maternal education and socioeconomic status (SES) were assessed using chi-square (χ²) tests. A Spearman’s rank correlation test was performed to assess the relationship between DBM and socioeconomic status.
Multivariable logistic regression models were applied after adjusting for child’s age, sex, father’s occupation and SES. Adjusted odds ratios (AORs) with 95% CIs were reported for modeling DBM with socio-demographic characteristics and socio-economic conditions. Region specific analyses were performed to explore variations of the prevalence of DBM and its socio-demographic characteristics across the administrative divisions. All statistical tests were two-tailed. A P-value <0.1 was considered statistically significant in the bivariate analysis for assessing the association between DBM and participant characteristics, while a P-value <0.05 was considered significant in the multivariable regression model. Model fit was assessed using Hosmer-Lemeshow goodness-of-fit tests. Selection of variables were confirmed in the multivariable model after variance inflation factors were calculated to check for multicollinearity among predictors. All statistical analyses were conducted using IBM SPSS (NY: IBM Corp., USA) and R programming language for cubic spline model.
2.4. Rapid Policy Review
A rapid policy review was conducted to explore the extent to which existing policy documents addressed DBM as major policy changes occurred during the 6th sector programme of Bangladesh in between 2011 and 2016 prioritizing nutrition. The survey was also conducted during this period. We systematically searched ministerial websites including the Ministry of Health and Family Welfare, Ministry of Women and Children Affairs, Ministry of Food, and other relevant ministries to identify policies. Documents were eligible if their titles indicated relevance to health or nutrition of children, adolescents, or women. Eligible documents were then screened for explicit or implicit references to DBM and for policy measures that could address both undernutrition and overnutrition.
2.5. Ethics
The national survey of childhood obesity was originally approved by the Ethical Review Committee of icddr,b. Written consent was obtained from the mothers of children 5 to 17 years and children 18 years or older. Assent was obtained from children 10 -17 years. This study conducted analyses on already collected data from the national survey, hence further ethical approval was not obtained.
2.6. Role of the Funding Source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
3. Results
3.1. Characteristics of the Participants
The national survey included a total of 4,140 children including ~600 children and their mothers from each CC in a division. The mean age of children was 11 years (SD: 4), including 50.3% girls and 66.8% adolescents (10–19 years). Nearly half of the children had an education below primary (47.0%), 34.9% had completed primary, 11.5% completed secondary and 6.6% never attended a school. Among mothers of the children 13.3% never attended a school, 10.4% had an education below primary (23.7%), 39.7% completed primary and 17.4% completed secondary education. Among fathers of the children, 14.1% never attended a school, 23.6% had an education below primary, 32.2% completed primary education and 44.1% had completed secondary education. Occupation of the fathers were business (43.4%), service (33.4%) and manual labor (21.5%), while 91% of the mothers of the children were housewives (
Table 2).
3.2. Prevalence of Population Level DBM and Variations Across Divisions
The overall prevalence of population level DBM was 44.0% (95% CI: 42.5–45.5%), including underweight in 29.6% children and overweight/obesity in 14.4% children. The prevalence of DBM was significantly higher in children than adolescents (51.3% vs. 40.3%; P < 0.001). Children of mothers with a low education had a higher prevalence of DBM than children of mothers who had completed secondary education (48.3% vs. 43.1%; P=0.007). Similarly, children whose fathers had a low education had a higher prevalence of DBM than children whose father had completed secondary education (47.7% vs. 41.8%; P=0.011). The highest prevalence of DBM was observed in Sylhet division (47.5%) followed by Rajshahi (47.3%), Dhaka (47.0%), Barisal (44.2%), Chattogram (42.0%), Khulna (40.0%) and Rangpur (40.0%). No significant variations in DBM were observed by sex, , and parents’ occupation (
Table 3 and
Figure 1).
3.3. Factors Attributing to Population Level DBM and Variations Across Divisions
Table 4 presents the adjusted odds ratios (ORs) of the relationship between the DBM among children and adolescents (5–19 years) at the population level across divisions in Bangladesh. Overall, children aged 5–9 years had significantly higher odds of DBM than those aged 10–19 years (OR = 1.56; 95% CI: 1.37–1.78). At the regional level, the relationship between age and DBM was significant in Barisal (OR = 1.83; 95% CI: 1.29–2.60), Khulna (OR = 1.57; 95% CI: 1.09–2.27), Rajshahi (OR = 2.28; 95% CI: 1.60–3.25), and Rangpur (OR = 1.77; 95% CI: 1.22–2.56), which was not observed in other divisions. (
Table 4)
Overall, no significant relationship was observed between DBM and socio-economic status. However, in Sylhet division, the odds of DBM was three times higher in lower SES (OR = 3.21; 95% CI: 1.16–8.90), two times higher in lower-middle SES (OR = 2.06; 95% CI: 1.12–3.80), and 74% higher in middle SES (OR = 1.74; 95% CI: 1.07–2.82) compared to upper SES. In Dhaka, by contrast, children from upper-middle SES had lower odds of DBM than upper SES (OR = 0.59; 95% CI: 0.37–0.93) (
Table 4)
.
While no relationship was observed between DBM and parental education overall. The regional analysis demonstrated that, children whose fathers had low education (OR = 0.48; 95% CI: 0.26–0.86) or completed primary (OR = 0.59; 95% CI: 0.36–0.97) had lower odds of DBM compared with those children whose fathers completed secondary education in Khulna. Conversely, children whose fathers had low education had nearly two times higher odds of DBM (OR = 1.96; 95% CI: 1.11–3.48) compared to children whose fathers completed secondary level in Rangpur division. No significant relationship was observed in the other divisions (
Table 4).
Maternal education demonstrated a protective relationship in Sylhet, where children of mothers who completed primary education had lower odds of DBM than those children whose mothers completed secondary education (OR = 0.60; 95% CI: 0.38–0.97), which was not observed in other divisions (
Table 4).
3.4. Prevalence of DBM Among Mother-Child Pairs at the Household Level
The prevalence of household level DBM was 15.6% (95% CI: 14.5–16.7%) and higher among younger children than adolescents (20.0% vs. 13.4%; P = 0.04). Prevalence varied substantially by region, ranging from 28.1% in Sylhet to 14.7% in Rangpur (P < 0.001). DBM was prevalent among in households where mothers (28.8% vs 18.8%; P = 0.032) or fathers (26.9% vs 19.4%; P = 0.003) had low educational attainment compared with children whose parents had completed secondary education. DBM prevalence was also higher in households where fathers were employed in service (26.3%) or business (25.1%) compared to households where fathers were engaged in manual labor (16.0%; P < 0.001). By SES, DBM was more prevalent in the upper SES than the lower -middle SES (18.0% vs. 12.0%; P < 0.001) (
Table 5 and
Figure 1).
3.5. Factors Attributing to Household Level DBM and Regional Variations
At the national level, households with a child aged 5–9 years had 64% higher odds of DBM than those with a child aged 10–19 years (OR = 1.64; 95% CI: 1.38–1.95). When examined by region, younger children remained at significantly higher odds in Dhaka (OR = 1.83; 95% CI: 1.17–2.86), Barisal (OR = 1.99; 95% CI: 1.22–3.33), and Rajshahi (OR = 1.96; 95% CI: 1.25–3.06) compared to Rangpur, while no relationship was observed in other divisions (
Table 5).
The odds of DBM were higher in children in lower-middle (OR = 1.41; 95% CI: 1.03–1.93) and middle SES households (OR = 1.49; 95% CI: 1.12–2.03) than the upper SES households. Socioeconomic disparities were observed in Sylhet and Chattogram. In Sylhet, the odds of DBM was more than twice among children who belongs to lower-middle (OR = 2.64; 95% CI: 1.13–6.18) and middle socioeconomic groups (OR = 2.62; 95% CI: 1.32–5.19) household compared to children from upper SES. In Chattogram, children from lower SES (OR = 2.75; 95% CI: 1.05–7.20) and lower-middle SES (OR = 2.51; 95% CI: 1.16–5.47) households had significantly higher odds of DBM than those from upper SES. However, no relationship was observed in Barisal, Khulna, Rajshahi, or Rangpur (
Table 5).
In the adjusted models, parental education was not significantly associated with DBM. In Khulna, children whose fathers had low education had significantly 62% lower odds of DBM compared with children whose fathers completed secondary education (OR = 0.38; 95% CI: 0.17–0.82), whereas having a mother with low education was correlated with four times higher odds of DBM (OR = 4.26; 95% CI: 1.81–10.0) compared with children whose mother had completed secondary education. No significant associations with parental education were observed in the other divisions (
Table 6).
3.6. Rapid Policy Review Findings
We identified seven national policy documents (policies and action plans) that prioritized reducing undernutrition and improving nutritional status to specified targets. Out of these 7 documents, 6 also addressed all forms of malnutrition (i.e., undernutrition, overnutrition in the form of overweight, obesity and nutrition related NCDs) at population level and to some extent household levels considering the emergence of overnutrition. None of the documents explicitly mentioned the double burden of malnutrition (DBM), and the term double-duty actions did not appear in any of the policy documents. While most interventions were designed to address a single form of malnutrition, more recent documents included a limited number of measures with potential to address both under- and overnutrition simultaneously. A brief summary of these documents in terms of addressing DBM indirectly is given below.
3.6.1. National Health Policy 2011
Primarily deals with undernutrition at the population level. Considering the physical and mental development of the future generation its main focus was undernutrition within females, pregnant mothers and children. None of the terms overweight, obesity, double burden of malnutrition, and double duty actions, were mentioned in the policy.
3.6.2. National Nutrition Policy 2015
This policy acknowledged nutrition as fundamental right, committed to ensure it for all and put special attention to disadvantaged group including mothers, adolescent girls and children. The policy largely speaks about undernutrition among children, adolescents and pregnant mothers in the context of the vicious cycle of malnutrition that starts with childbearing. It also mentions the emergence of overweight, obesity and different nutrition related NCDs among women.
Along with other interventions that tackles undernutrition and overnutrition separately, single interventions to address both underweight and overweight at the same time include exclusive breastfeeding of newborns till 6 months of age and enabling environment for new mothers to follow breastfeeding; consumption of iron and folic acid and other supplements both for pregnant mothers and children, complementary food provision to infants after 6 months of age along with breastfeeding, consumption of iron and folic acid supplements both for pregnant mothers and children; regulating the marketing of processed food and nutrition education. Although the terms DBM or double duty actions are not mentioned directly, the policy has addressed undernutrition, overweight, obesity and nutrition related NCDs using single intervention mentioned above along with others.
3.6.3. Second National Plan of Action for Nutrition (2016-2025)
The term DBM at population level or double duty of actions were not mentioned directly, the plan developed activities that can address undernutrition and overweight, obesity, nutrition related NCDs altogether at the same time at population level and to some extent at household level. In terms of using single interventions to deal with all forms of malnutrition mentioned above, it focused on promoting exclusive breastfeeding including infant and young child feeding (IYCF) during antenatal care (ANC) and postnatal care (PNC) visits aiming to increase the coverage up to 70% of infants below 6 months of age.
3.6.4. National Plan of Action for Adolescent Health Strategy (2017-2030)
DBM or double duty actions were not mentioned explicitly but the strategy designed interventions that targeted both undernutrition, overweight and obesity at the same time. These were: 1) promoting school feeding programme in 80% of the public health school targeting children and adolescents from class 1 to 10; 2) providing health and nutrition education sessions through school to promote healthy food and physical activity with a target to conduct 100 sessions per year; 3) screening for malnutrition and obesity and special nutrition counselling provision to underweight and overweight students targeting 100% coverage.
3.6.5. Bangladesh National Strategy for Maternal Health (2019-2030)
This document focuses on reducing maternal and neonatal mortality along with maternal and neonatal morbidity acknowledging the pivotal role of nutrition to achieve its abovementioned aim. From the context of nutrition, it largely speaks about underweight, lower BMI and severe stunting and food insecurity within ever married women, pregnant women and women in reproductive age and its consequences on newborns in terms of being underweight and undernourished. For this purpose, it emphasizes mainstreaming nutrition at all service delivery points including at health facility and at school. Considering household level DBM among mothers and their children, this document could have had the potential to address the issue along with addressing population level DBM as the strategy focuses on mother and her child. It focuses on improving ANC/PNC visits incorporating nutrition counselling, iron and folic acid supplement distribution.
3.6.6. National School Meal Policy 2019
To tackle undernutrition and overweight among children at population level and to improve nutrition, education and reduce school drop-out among pre-primary and primary school children (age 3-12 years), the national school meal policy 2019 aimed to meet minimum 30% calorie intake through school meals and to meet 50% of the daily micronutrient requirement through school meals for half day school. Neither DBM at population and household level nor double duty of action is mentioned directly.
3.6.7. Bangladesh National Food and Nutrition Security Policy: Plan of Action(2021-2030)
Activities to address both underweight and overweight/obesity/nutrition related NCDs using single intervention includes awareness raising through nutrition education at school to ensure adolescents are consuming at least 400 g of nutritious food (i.e., fruits and vegetables). This activity is also expected to reduce adolescent girl wasting below 15%. Another important activity is to impose regulatory measure to the marketing of processed food to ensure at least half of all food products provide food information and nutrient labelling. Although the document does not directly mention double burden of malnutrition or double duty actions; activities proposed do address population level DBM (Table A1).
4. Discussion
This is the first study to provide a national-level estimates of the prevalence of DBM and regional variations at both population and household levels in urban Bangladesh using a nationally representative data. It highlights three key findings regarding the coexistence of DBM, as well as the complex interplay of socio-demographic characteristics and maternal factors contributing to DBM. First, nearly half of the children and adolescents aged 5 to 19 years in Bangladesh experience the DBM at a population level, which is predominantly higher among younger children whose mother have high education. Second, one-fourth of the mother-child pairs had DBM at the household level and it was higher among mothers with a higher education living in a higher SES group. Third, significant regional variations of DBM were observed at both population level and household levels. Fourth, mothers with a low education belonging to a middle to upper SES represented the key population group that exhibited a higher burden of malnutrition among younger children than adolescents.
The prevalence of DBM is high both at the national and household level in Bangladesh where overnutrition and undernutrition co-exist within the same population or mother-child dyads. This high prevalence has revealed the substantial burden of undernutrition and overnutrition among children and adolescents. The findings are aligned with studies conducted in other low and middle income countries where similar dual burdens have been documented[
37,
38]. In Bangladesh, this finding is further explained by the fact that one-fourth of the mother-child pairs are affected by DBM at the household level. The estimate of DBM is higher compared to what has been reported in Ethiopia [
39] and the burden is rapidly emerging in South and Southeast Asia[
40]. The coexistence of malnutrition at both of the population and the household levels underscores the need to identify vulnerable populations experiencing the highest burden across socio-demographic characteristics and regional factors.
Younger children were more likely to experience DBM compared to adolescents (10 to 18 years). The pattern was consistently observed across all the geographical locations in Bangladesh. The observed higher prevalence of DBM is aligned with existing evidence in India that younger children are in a critical stage of growth and development, which is making them more vulnerable to the adverse effects of malnutrition[
41]. This demographic characteristic can be attributed to younger children being particularly susceptible to micronutrient deficiencies, which can compromise immune function and increase the likelihood of malnutrition[
42]. Furthermore, the findings may be explained by the fact that nearly one in ten mother-child pairs have experienced malnutrition at the household level in which overnutrition in both mother and child has a higher contribution to DBM. Given these complexities, it is essential to explore the role of parental education in improving the nutritional status of children and mitigating the risks associated with DBM.
The findings revealed that the prevalence of DBM was particularly high among mothers and fathers who had a low education. A 15 years long longitudinal study in Bangladesh showed that high maternal education has significantly reduced the burden of malnutrition among children[
43]. In contrast, a community based study in Bangladesh reported that childhood overweight and obesity was highly prevalent among mothers of children who completed secondary education[
44]. A global review conducted across 52 LMICs supports the evidence that more advanced maternal education is associated with a higher risk of overnutrition, while lower maternal education is linked to undernutrition in children[
45]. In urban areas, a lack of space and facilities for physical activity further worsens these nutritional challenges related to malnutrition[
46]. Our findings suggest that the relationship between maternal education and DBM becomes more complex in urban areas due to changes in socioeconomic status. Educated mothers in high-income households may have greater exposure to unhealthy diets and processed foods[
47]. Therefore, maternal education along with the socioeconomic position of the household may contribute to the increasing burden of DBM at both the population and household levels.
Our research further suggests that children whose fathers were engaged in business and service occupations were more likely to have a higher burden of DBM compared to those children whose fathers were manual workers. Similar trends have been reported in other LMICs settings, where households with relatively better income sources often experienced a dual burden of malnutrition due to a nutritional transition[
48]. Increased income may lead to greater consumption of energy-dense, processed foods contributing to overweight and obesity, while underlying child undernutrition persists due to poor dietary diversity or inadequate feeding practices[
6]. In contrast, families dependent on manual labor may have limited resources, but their diets are less likely to include calorie-rich processed foods, potentially reducing the risk of overweight[
49]. This underscores the complexity of socio-economic drivers in the double burden of malnutrition, indicating that higher economic standing alone does not necessarily translate into better nutrition outcomes without concurrent improvements in dietary quality and health behaviors.
We have documented that socioeconomic status had a significant relationship with DBM among mother-child pairs in urban Bangladesh. Our research revealed that DBM was more prevalent in households where mothers had higher education and belonged to the richest SES group. Additionally, the study indicated that as socioeconomic status improved from lower to upper levels, undernutrition decreased while overnutrition increased. This trend reflects the ongoing nutritional transition in urban Bangladesh, where economic growth and lifestyle changes have led to shifts in dietary patterns[
50]. Higher-income households often have greater access to processed and energy-dense foods, contributing to rising obesity rates, while lower-income households continue to struggle with undernutrition due to limited access to diverse and nutritious foods. The interaction analysis further revealed that mothers with at least primary education living in upper SES households were more likely to have DBM. This finding highlights the synergistic effect of education and wealth on nutritional outcomes.
4.1. Policy Implications
Rapid policy review demonstrates that specific actions are in place in the policy documents in Bangladesh that can tackle both undernutrition and all forms of overnutrition. The existing ones are: exclusive breastfeeding to infants at the first 6 months; nutrition counselling during ANC and PNC visits; school feeding programme and market regulation for processed foods. While these are in place, proper governance is required to make sure these interventions are in action to address population level DBM.
Even when the mentioned interventions have the potential to address both mother overnutrition and child undernutrition, the policy documents mostly emphasized capacity to improve nutrition status in favor of children, while these interventions can also improve mother’s nutritional status. For an example: exclusive breastfeeding provides infants essential nutrition but it also helps to regulate mother’s weight gain during post-partum period that can protect mothers from being obese or overweight. More awareness raising is required for the existing interventions that have the potential to act as a double duty action in terms of the benefits both for the child and mothers to address household level DBM.
4.2. Strengths and Limitations
Some limitations must be acknowledged. First, the cross-sectional design prevents us from establishing causality between socio-economic factors and DBM. Second, while BMI is widely used for assessing nutritional status, it does not capture body composition differences, which may affect classifications of undernutrition and overnutrition. Third, the national survey was conducted a decade ago in urban settings only and our findings may not represent the national burden of DBM in rural Bangladesh, or capture any changes that occurred over time, particularly following the global pandemic in 2020-2021[
51]. However, there has not been any baseline data for Bangladesh before COVID-19 pandemic and thus our research represents a strong baseline for the burden of DBM in Bangladesh in urban population in order to monitor the changes following COVID-19 pandemic. Further, our research findings were derived from a population-based samples that has represented the study populations at the divisional level, which has allowed a comprehensive comparative analysis of the regional patterns of DBM in Bangladesh, which is rare to achieve in a low resource setting. Finally, the use of standardized anthropometric measurements and internationally recognized BMI classifications enhanced the reliability of our findings.
5. Conclusions
This study has provided national-level prevalence of DBM among children and adolescents as well as mother-child dyads in urban Bangladesh. The findings highlight that DBM is highly prevalent at both of the population and household levels, particularly among younger children and in households with higher maternal education and socioeconomic status. Maternal education is a key determinant of DBM, with higher education levels associated with both improvements in undernutrition and an increased risk of overnutrition. Additionally, regional disparities in DBM has shown the need for targeted interventions addressing both undernutrition and rising obesity rates. The coexistence of undernutrition and overnutrition varied across division and reflects the ongoing nutritional transition in urban Bangladesh. Further longitudinal research is needed to better understand the long-term effects of maternal education and socioeconomic status on child nutrition and to develop sustainable solutions for reducing DBM in Bangladesh. These patterns underscore an urgent need for double duty policies that curb the rise in childhood overweight while sustaining progress against undernutrition. Priority actions include strengthening school food standards and marketing restrictions, integrating BMI screening and parent counseling into routine child health contacts, and tailoring messages for higher-SES, higher-education households alongside enhanced nutrition support for poorer families. Region-specific programming and longitudinal surveillance are essential to track the nutritional transition and to design scalable, sustainable responses.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
AN conceptualized the study, acquired funding, designed the methodology, supervised project implementation, interpreted data, and contributed to writing, review, and editing. MSI conducted the literature search, curated data, performed formal analysis, interpreted data, and drafted the original manuscript. NNM managed project administration, contributed to data interpretation, and participated in writing, review, and editing. AI and NT contributed to review and editing. AM and AN contributed equally to this work. All authors approved the final version of the manuscript.
Funding
This research was funded by National Nutrition Service, Ministry of Health and Family Welfare, Bangladesh.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethical Review Committee (ERC) of icddr,b (PR-13024) for studies involving humans.
Informed Consent Statement
Written consent was obtained from the mother of children 5 to 17 years of age including an additional assent from children older than 10 -17 years and consent obtained from children 18-19 years of age. The secondary data analyses were conducted with already collected data and no further ethical approval was required prior to the study.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Acknowledgments
This study was funded by the National Nutrition Service (NNS) under the Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh. We extend our sincere gratitude to the Mayors of the City Corporations and the study participants for the support in implementing this study. icddr,b acknowledges with appreciation the dedication of NNS to its research initiatives and is thankful for the core/unrestricted support provided by the Governments of Bangladesh and Canada.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| NNS |
National Nutrition Service |
| DBM |
Double Burden of Malnutrition |
| BMI |
Body Mass Index |
| WHO |
World Health Organization |
| IYCF |
Infant and young child feeding |
| ANC |
Antenatal Care |
| PNC |
Postnatal Care |
References
- Al-Jawaldeh, A. , et al., A new global policy framework for adolescent nutrition? The Lancet, 2022. 399(10320): p. 125-127.
- WHO, Talk about depression, strengthen depression-related services. 2017.
- Organization, W.H. , WHO guideline on the prevention and management of wasting and nutritional oedema (acute malnutrition) in infants and children under 5 years. 2024: World Health Organization.
- Organization, W.H. , Overweight and obesity. 2024.
- Seferidi, P. , et al., Global inequalities in the double burden of malnutrition and associations with globalisation: a multilevel analysis of Demographic and Health Surveys from 55 low-income and middle-income countries, 1992–2018. The Lancet Global Health, 2022. 10(4): p. e482-e490.
- Popkin, B.M., C. Corvalan, and L.M. Grummer-Strawn, Dynamics of the double burden of malnutrition and the changing nutrition reality. The Lancet, 2020. 395(10217): p. 65-74.
- Organization, W.H. , http://apps.who.int/iris/bitstream/10665/255413/1/WHO-NMH-NHD-17.3-eng.pdf. 2016.
- Sahiledengle, B. and L. Mwanri, Unveiling the crisis of the double burden of malnutrition. The Lancet Global Health, 2024. 12(3): p. e348-e349.
- Popkin, B.M., C. Corvalan, and L.M. Grummer-Strawn, Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet, 2020. 395(10217): p. 65-74.
- Anik, A.I. , et al., Double burden of malnutrition at household level: A comparative study among Bangladesh, Nepal, Pakistan, and Myanmar. PloS one, 2019. 14(8): p. e0221274.
- Hossain, M.S. , et al., The double burden of malnutrition—further perspective. The Lancet, 2020. 396(10254): p. 813-814.
- Hossain, M.T., S. K. Luies, and T. Biswas, Prevalence and factors associated with overweight and obesity among primary school children (9–14 years) in a selected area of Dhaka, Bangladesh: A cross-sectional study. Indian Journal of Community Medicine, 2020. 45(4): p. 429-434.
- Anik, A.I. , et al., Urban-rural differences in the associated factors of severe under-5 child undernutrition based on the composite index of severe anthropometric failure (CISAF) in Bangladesh. BMC Public Health, 2021. 21(1): p. 2147.
- Rahaman, M.A., A. Kalam, and M. Al-Mamun, Unplanned urbanization and health risks of Dhaka City in Bangladesh: uncovering the associations between urban environment and public health. Frontiers in public health, 2023. 11: p. 1269362.
- Manik, M.H. , Demographic and socio-economic changes in Bangladesh: evidence from the population census in 2022. FJSR, 2024. 3: p. 29-38.
- Srinivasan, C.S., G. Zanello, and B. Shankar, Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC public health, 2013. 13(1): p. 581.
- Sanghvi, T.G. and E.A. Frongillo, Similarities in socioeconomic disparities and inequalities in women’s nutritional status and health care in Bangladesh, Ethiopia, India, and Nigeria. Global Health Action, 2024. 17(1): p. 2439165.
- http://www.who.int/nmh/countries/bgd_en.pdf.
- Talukder, A. , et al., Influence of Maternal Education and Household Wealth on Double Burden of Malnutrition in South and Southeast Asia. Maternal & Child Nutrition, 2025: p. e70049.
- Tariqujjaman, M. , et al., Determinants of double burden of malnutrition among school children and adolescents in Urban Dhaka: a multi-level analyses. Frontiers in Public Health, 2022. 10: p. 926571.
- Hossain, M.I. , et al., Double burden of malnutrition among women of reproductive age in Bangladesh: A comparative study of classical and Bayesian logistic regression approach. Food Science & Nutrition, 2023. 11(4): p. 1785-1796.
- Debnath, S., N. Mondal, and J. Sen, Double burden of malnutrition among adolescents in India. 2019, Human.
- Biswas, T. , et al., Geographical and socioeconomic inequalities in the double burden of malnutrition among women in Southeast Asia: A population-based study. The Lancet Regional Health-Southeast Asia, 2022. 1.
- NNS, D. National Nutrition Service (NNS) Operational Plan 2024; Available from: http://etoolkits.dghs.gov.bd/toolkits/bangladesh-program-managers/national-nutrition-service-nns-operational-plan.
- Billah, S.M. , et al., Quality of nutrition services in primary health care facilities: Implications for integrating nutrition into the health system in Bangladesh. PloS one, 2017. 12(5): p. e0178121.
- List of city corporations in Bangladesh. 2024; Available from: https://en.wikipedia.org/wiki/List_of_city_corporations_in_Bangladesh.
- Organization, W.H. , Training for mid-level managers: The EPI coverage survey, Geneva: WHO expanded programme on immunization, 1991. 2014, WHO/EPI/MLM/91.10.
- Organization, W.H. , Training for mid-level managers (MLM): module 7: the EPI coverage survey, in Training for mid-level managers (MLM): module 7: the EPI coverage survey. 2020.
- Crespi, C.M. , et al., Validity of child anthropometric measurements in the Special Supplemental Nutrition Program for Women, Infants, and Children. Pediatric research, 2012. 71(3): p. 286-292.
- Cole, T.J. , et al., Establishing a standard definition for child overweight and obesity worldwide: international survey. Bmj, 2000. 320(7244): p. 1240.
- Bajaj, S.S., et al., Body Mass Index thresholds for asians: A race correction in need of correction? 2024, American College of Physicians. p. 1127-1129.
- WHO. Adolescent health; https://www.who.int/southeastasia/health-topics/adolescent-health#:~:text=WHO%20defines%20’Adolescents’%20as%20individuals,age%20range%2010%2D24%20years.
- Rutstein, S.O. , DHS comparative reports no. 6. (No Title), 2004.
- Lancet, T. , A future direction for tackling malnutrition. 2020. p. 2.
- Doak, C.M. , et al., The dual burden household and the nutrition transition paradox. International journal of obesity, 2005. 29(1): p. 129-136.
- WHO-SEARO, Mid-term review of the Strategic Action Plan to reduce the double burden of malnutrition in the WHO South-East Asia Region 2016–2025. 2022.
- Balasubramanya, B., A. R. Johnson, and T. Sulekha, Double burden of malnutrition among adolescents: Evidence from a cross-sectional study among school-going adolescents in Bangalore city. Indian Journal of Health Sciences and Biomedical Research kleu, 2024. 17(3): p. 224-229.
- Viana, R.S., K. De Araújo-Moura, and A.C.F. De Moraes, Worldwide prevalence of the double burden of malnutrition in children and adolescents at the individual level: systematic review and meta-regression. Jornal de Pediatria, 2025.
- Belay, M.A. , et al., Double burden of malnutrition among households in Ethiopia: a systematic review and meta-analysis. Frontiers in Public Health, 2025. 12: p. 1417289.
- Talukder, A., et al., Prevalence and Trends of Double Burden of Malnutrition at Household-Level Among Mother-Child Pairs in South and Southeast Asia. Available at SSRN 4938142.
- Amoadu, M. , et al., Risk factors of malnutrition among in-school children and adolescents in developing countries: A scoping review. Children, 2024. 11(4): p. 476.
- Jiang, W. , et al., Cross-country health inequalities of four common nutritional deficiencies among children, 1990 to 2019: data from the Global Burden of Disease Study 2019. BMC Public Health, 2024. 24(1): p. 486.
- Hasan, M.T. , et al., The role of maternal education in the 15--year trajectory of malnutrition in children under 5 years of age in B angladesh. Maternal & child nutrition, 2016. 12(4): p. 929-939.
- Biswas, T. , et al., Overweight and obesity among children and adolescents in Bangladesh: a systematic review and meta-analysis. Public health, 2017. 142: p. 94-101.
- Alem, A.Z. , et al., Double burden of malnutrition and its associated factors among women in low and middle income countries: findings from 52 nationally representative data. BMC Public Health, 2023. 23(1): p. 1479.
- Hasan, A.R. , et al., Challenges of promoting physical activity among school children in urban Bangladesh: a qualitative inquiry. PloS one, 2020. 15(3): p. e0230321.
- Sousa, J.M.d. , et al., Association of Maternal Consumption of Ultra-Processed Foods with Feeding Practices and Malnutrition in Breastfed Infants: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 2025. 22(4): p. 608.
- Tzioumis, E. and L.S. Adair, Childhood dual burden of under-and overnutrition in low-and middle-income countries: a critical review. Food and nutrition bulletin, 2014. 35(2): p. 230-243.
- Tran, B.H. , Relationship between paternal involvement and child malnutrition in a rural area of Vietnam. Food and nutrition bulletin, 2008. 29(1): p. 59-66.
- Zabsyn, S. , A comparative nutritional status and food intake pattern of adolescent girls with emphasis on fish intake (marine & riverine) between selected urban & rural locations. 2025, © University of Dhaka.
- Sarker, A.R., Z. Hossain, and A. Morton, Drivers and distribution of the household-level double burden of malnutrition in Bangladesh: analysis of mother–child dyads from a national household survey. Public Health Nutrition, 2022. 25(11): p. 3158-3171.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).