Submitted:
19 January 2026
Posted:
21 January 2026
You are already at the latest version
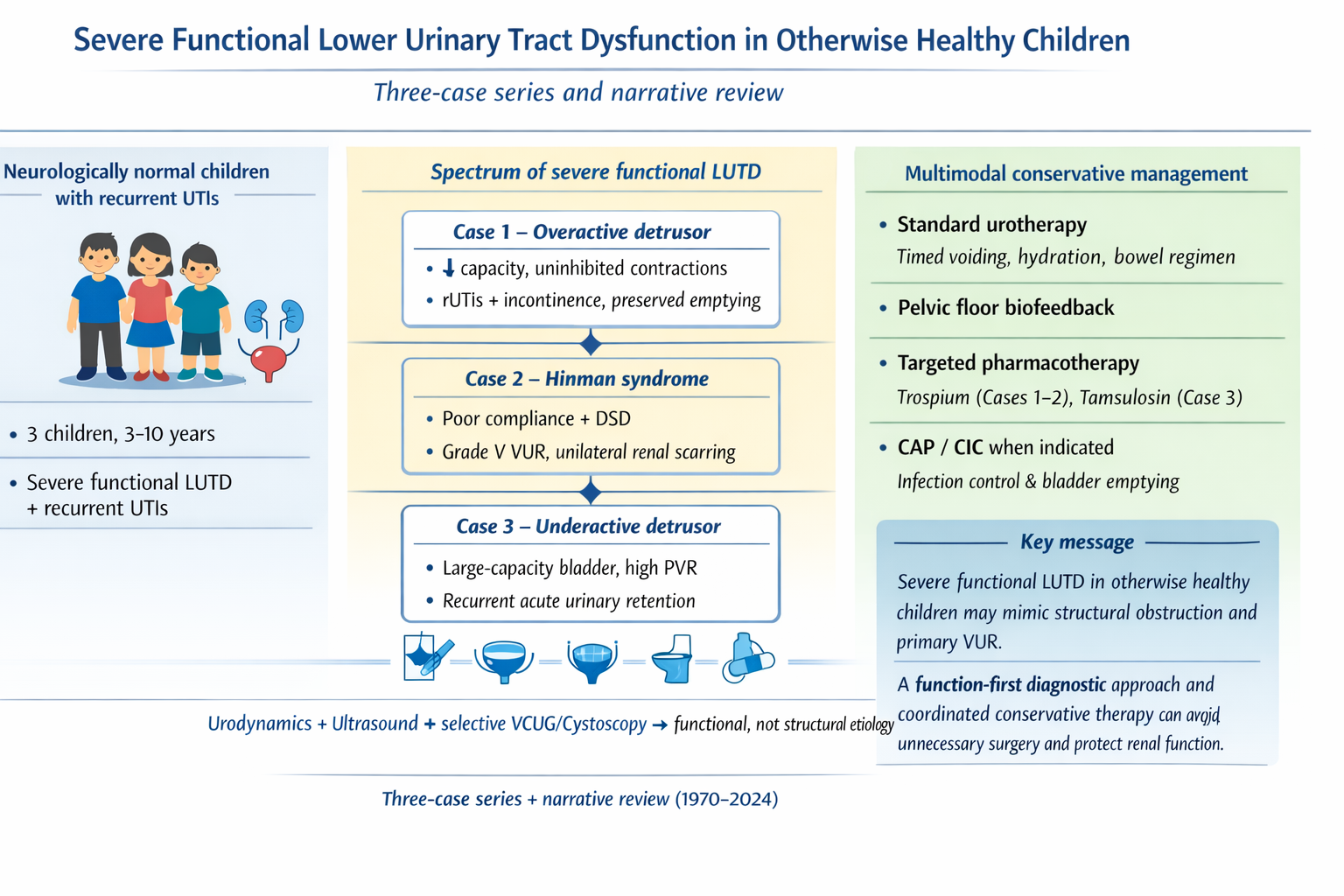
Abstract
Keywords:
1. Introduction
2. Case Series
2.1. Methods
2.2. Case Presentations
4. Discussion
Suggested Diagnostic Approach to Severe LUTD in Neurologically Intact Children
Pathophysiologic Considerations
Clinical and Diagnostic Correlation
Management Implications
Combination Therapy with Trospium Chloride and Biofeedback
Outcomes and Comparison with Literature
Misdiagnosis and Iatrogenic Management Pitfalls
| Common Misstep | Underlying Issue / Reason | Typical Consequence | Evidence-Based Alternative (ICCS & Current Guidelines) |
|---|---|---|---|
| Performing cystoscopic bulking injections for presumed VUR without functional assessment | Misinterpretation of rUTIs or hydronephrosis as anatomical reflux | Persistence or recurrence of UTIs and incontinence; unresolved high bladder pressures; possible upper tract deterioration | Comprehensive LUTD work-up first: uroflowmetry, post-void residual (PVR), and urodynamics; initiate urotherapy ± pharmacotherapy before considering anti-reflux surgery |
| Ureteral reimplantation in children with unrecognized dysfunctional voiding | Reflux secondary to bladder outlet dysfunction misdiagnosed as primary anatomical VUR | Postoperative persistence of reflux/incontinence; recurrent infections despite technically successful surgery | Treat functional outlet dysfunction (biofeedback, timed voiding, bowel management, antimuscarinics/α-blockers); reassess reflux after functional correction |
| Labeling incontinence or retention as behavioral without urodynamic confirmation | Lack of objective testing; underestimation of detrusor overactivity or underactivity | Delayed diagnosis; progression to hydronephrosis or renal scarring | Early non-invasive uroflow/PVR; cystometry when indicated; phenotype-guided therapy |
| Neglecting constipation or bowel dysfunction in LUTD management | Overlooking bladder–bowel interaction | Treatment failure; recurrent UTIs and incontinence | Integrated bowel regimen as part of standard urotherapy; dietary fiber, laxatives, timed toileting |
| Prolonged antibiotic prophylaxis without addressing voiding dysfunction | Treating infection consequence rather than the cause | Persistent bacteriuria and antimicrobial resistance | Functional evaluation and correction; prophylaxis only as temporary adjunct during therapy initiation |
| Proceeding to invasive or surgical intervention before multidisciplinary review | Fragmented care, absence of urodynamic input | Iatrogenic morbidity, continued symptoms | Multidisciplinary team evaluation (urology, nephrology, physiotherapy, psychology); individualized stepwise management |
Limitations
Clinical Takeaways
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LUTD | Lower Urinary Tract Dysfunction |
| UTI | Urinary Tract Infection |
| VCUG | Voiding Cystourethrography |
| ED | Emergency Department |
References
- Austin, PF; Bauer, SB; Bower, W; Chase, J; Franco, I; Hoebeke, P. The standardization of terminology of lower urinary tract function in children and adolescents. Neurourol Urodyn 2016, 35, 471–81. [Google Scholar] [CrossRef]
- Chase, J; Austin, PF; Hoebeke, P; McKenna, P. The management of dysfunctional voiding in children: A report from the International Children’s Continence Society. Journal of Urology 2010, 183, 1296–302. [Google Scholar] [CrossRef]
- Nevéus, T; von Gontard, A; Hoebeke, P; Hjälmås, K; Bauer, S; Bower, W; et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children’s Continence Society. J Urol 2006, 176, 314–24. [Google Scholar] [CrossRef]
- Kopač, M; Lusuardi, L; Sillen, U. Pediatric lower urinary tract dysfunction. Biomedicines 2024, 12, 547. [Google Scholar] [CrossRef]
- Fuentes, M; Figueroa, V; Burbano, J. Diagnosis and management of bladder dysfunction in children. Front Pediatr 2019, 7, 298. [Google Scholar] [CrossRef]
- Wang, J; Ren, L; Liu, X; Liu, J; Ling, Q. Underactive Bladder and Detrusor Underactivity: New Advances and Prospectives. International Journal of Molecular Sciences 2023, Vol 24 24, 15517. [Google Scholar] [CrossRef] [PubMed]
- Franco, I. Functional bladder problems in children: Pathophysiology, diagnosis, and treatment. Pediatr Clin North Am 2012, 59, 783–817. [Google Scholar] [CrossRef] [PubMed]
- Keren, R; Shaikh, N; Pohl, HG. Risk factors for recurrent urinary tract infection and renal scarring in children. Pediatrics 2015, 169, 913–21. [Google Scholar] [CrossRef]
- Shaikh, N; Morone, NE; Lopez, J. Recurrent urinary tract infections in children with bladder and bowel dysfunction. Pediatrics 2016, 136, e13–21. [Google Scholar] [CrossRef]
- Veauthier, B; Cabrera, J. Urinary tract infections in young children and infants: Common questions and answers. Am Fam Physician 2020, 102, 278–85. [Google Scholar]
- Nieuwhof-Leppink, AJ; Hussong, J; Chase, J; Larsson, J; Renson, C; Hoebeke, P; et al. Definitions, indications and practice of urotherapy in children and adolescents: - A standardization document of the International Children’s Continence Society (ICCS). J Pediatr Urol 2021, 17, 172–81. [Google Scholar] [CrossRef]
- Gampala, S; Alkukhun, L; Khan, Z. Hinman Syndrome: A Rare Entity with Neurogenic Bladder-Like Symptoms. Cureus 2024, 16, e55684. [Google Scholar] [CrossRef]
- Hinman, F. Nonneurogenic neurogenic bladder (the Hinman syndrome)—15-year follow-up of 14 cases. Journal of Urology 1986, 136, 769–77. [Google Scholar] [CrossRef]
- Hinman, F; Baskin, LS. Hinman’s Atlas of Pediatric Urologic Surgery; Elsevier Health Sciences, 2009. [Google Scholar]
- Nevéus, T; von Gontard, A; Hoebeke, P. The standardization of terminology of lower urinary tract function in children and adolescents. Neurourol Urodyn 2016, 35, 471–81. [Google Scholar] [CrossRef]
- Hoebeke, P; Van Laecke, E; Raes, A; Renson, C; Theunis, M; Vande Walle, J. Bladder function and non-neurogenic dysfunction in children: classification and terminology. Acta Urol Belg 1995, 63(2), 93–8. Available online: https://pubmed.ncbi.nlm.nih.gov/7785550/ (accessed on 15 November 2025). [PubMed]
- Leclair, MD; Héloury, Y. Non-neurogenic elimination disorders in children. J Pediatr Urol 2010, 6, 338–45. [Google Scholar] [CrossRef]
- Lopez Pereira, P; Miguelez, C; Caffarati, J; Estornell, F; Anguera, A. Trospium Chloride for the Treatment of Detrusor Instability in Children. J Urol 2003, 170, 1978–81. [Google Scholar] [CrossRef]
- Boussetta, A; Jellouli, M; Baati, R; Gargah, T. Neurogenic non-neurogenic bladder in childhood: complications and prognostic factors. Tunis Med 2021, 99, 898. [Google Scholar] [PubMed]
- Pereira, JR. Trospium Chloride for the Treatment of Detrusor Instability in Children. Journal of Urology 2003, 170, 151–5. [Google Scholar] [CrossRef] [PubMed]
- Board, UE. Efficacy and Safety of Trospium Chloride Use in Children With Idiopathic and Neurogenic Detrusor Overactivity: An Overview of Available Data. Urotoday Int J 2011, 4(1), art17. [Google Scholar] [CrossRef]
- Schultz-Lampel, D; Steuber, C; Schultz-Lampel, D; Steuber, C; Hoyer, PF; Bachmann, CJ; Marschall-Kehrel, D; Bachmann, H. Urinary incontinence in children. Dtsch Arztebl Int 2011, 108(37), 613-20. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Danilov, V; Kuznetsov, I. Dynamic Changes of the Residual Urine Symptom During Trospium Chloride Treatment in Children. Russian Journal of Pediatric Urology 2018, 14, 23–8. [Google Scholar] [CrossRef]
- Lee, DH; Kim, YS; Lee, HY; Han, SW. Hinman Syndrome: Long-Term Follow-up of 14 Cases. Korean J Urol 2007, 48, 1058–64. [Google Scholar] [CrossRef]
- Jayanthi, VR; Khoury, AE; McLorie, GA; Agarwal, SK. The Nonneurogenic Neurogenic Bladder of Early Infancy. Journal of Urology 1997, 158, 1282–6. [Google Scholar] [CrossRef]
- Chaichanamongkol, V; Ikeda, M; Ishikura, K. An Infantile Case of Hinman Syndrome with Severe Acute Renal Failure. Clin Exp Nephrol 2008, 12, 145–9. [Google Scholar] [CrossRef]
- Wan, KS; Yang, CC. Psychogenic Urinary Retention in Children: A Case Report. Pediatr Neonatol 2010, 51, 375–8. [Google Scholar] [CrossRef]
- Nerli, R; Pujar, S; Ghagane, S; Hiremath, M; Dixit, N. Persistence and appearance of vesicoureteral reflux/obstruction following open reimplantation for vesicoureteral reflux. Journal of the Scientific Society 2019, 46, 90. [Google Scholar] [CrossRef]
- Capozza, N; Lais, A; Matarazzo, E; Nappo, S; Patricolo, M; Caione, P. Influence of Voiding Dysfunction on the Outcome of Endoscopic Treatment for Vesicoureteral Reflux. J Urol 2002, 168, 1695–8. [Google Scholar] [CrossRef]
- Sillén, U. Bladder Dysfunction and Vesicoureteral Reflux. Adv Urol 2008, 2008, 1–8. [Google Scholar] [CrossRef]
- Noe, HN. The Role of Dysfunctional Voiding in Failure or Complication of Ureteral Reimplantation for Primary Reflux. J Urol 1985, 134, 1172–5. [Google Scholar] [CrossRef]
- Whittam, BM; Thomasch, JR; Makari, JH; Tanaka, ST; Thomas, JC; Pope, IV JC; et al. Febrile Urinary Tract Infection After Ureteroneocystostomy: A Contemporary Assessment at a Single Institution. In Journal of Urology; 2010; Volume 183, pp. 688–93. [Google Scholar] [CrossRef]
- Lipski, BA; Mitchell, ME; Burns, MW. Voiding dysfunction after bilateral extravesical ureteral reimplantation. J Urol. 1998, 159(3), 1019–21. Available online: https://pubmed.ncbi.nlm.nih.gov/9474222/ (accessed on 15 November 2025). [CrossRef] [PubMed]
- MINEVICH, E; ARONOFF, D; WACKSMAN, J; SHELDON, CA. Voiding dysfunction after bilateral extravesical detrusorrhaphy. J Urol 1998, 160, 1004–6. [Google Scholar] [CrossRef] [PubMed]
- Capozza, N; Lais, A; Matarazzo, E; Nappo, S; Patricolo, M; Caione, P. Influence of voiding dysfunction on the outcome of endoscopic treatment for vesicoureteral reflux. J Urol 2002, 168, 1695–8. [Google Scholar] [CrossRef] [PubMed]
- Gnech, M; ’t Hoen, L; Zachou, A; Bogaert, G; Castagnetti, M; O’Kelly, F; et al. Update and Summary of the European Association of Urology/European Society of Paediatric Urology Paediatric Guidelines on Vesicoureteral Reflux in Children. Eur Urol 2024, 85, 433–42. [Google Scholar] [CrossRef]
- Chase, J; Austin, PF; Hoebeke, P; McKenna, P. The management of dysfunctional voiding in children: A report from the International Children’s Continence Society. Journal of Urology 2010, 183, 1296–302. [Google Scholar] [CrossRef] [PubMed]
- Hoberman, A; Keren, R; of Philadel-phia, H; Mathews, R; Kropp, BP; Nelson, CP; et al. Antimicrobial Prophylaxis for Children with Vesicoureteral Reflux. New England Journal of Medicine 2014, 370, 2367–76. [Google Scholar] [CrossRef]

| Characteristic | Description / Rationale |
| Neurologically and anatomically normal | Supports non-neurogenic, non-structural etiology |
| Recurrent UTIs (≥ 2 febrile or ≥ 3 culture-proven within 12 months) | Indicates clinically significant morbidity |
| Urodynamic evidence of detrusor overactivity, dyssynergia, or underactivity | Defines severe functional LUTD phenotype |
| No prior lower urinary tract surgery related to functional obstruction at the time of LUTD evaluation; no systemic disease affecting voiding | Excludes iatrogenic or systemic confounders |
| Characteristic | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age / Sex | 7 years / Male | 3 years / Female | 10 years / Male |
| Presenting Symptoms | Recurrent febrile UTIs, daytime incontinence, urgency, enuresis | Fever, pollakiuria, dysuria, incontinence | Acute urinary retention (recurrent episodes) |
| Prior History | Multiple UTIs over the preceding year | Persistent LUTS after treated UTI | Three prior ED visits for retention |
| Ultrasound Findings | Moderate bladder wall thickening; no residual urine | Left ureterohydronephrosis; crenulated bladder wall | Bladder wall thickened (7–8 mm), irregular contour, heterogeneous content |
| VCUG Findings | Crenulated bladder, no reflux, normal emptying | Grade V left VUR, dilated tortuous ureter, no voiding achieved | Large-capacity bladder, mild crenulation, grade I VUR, incomplete emptying |
| Renal Scintigraphy (DMSA) | – | Left kidney: small, irregular, cortical scarring; function 18.7% | – |
| Cystoscopy Findings | Deep trabeculations, pseudopolypoid mucosa, diverticula, dilated vessels | Marked trabeculation, cell-like and columnar mucosa, difficult ureteric visualization | Trabeculated, pseudodiverticular bladder mucosa, normal urethra |
| Urodynamic Pattern | Detrusor overactivity, reduced capacity, uninhibited contractions | Poor compliance, detrusor–sphincter dyssynergia, high PVR | Hypocontractile detrusor, weak flow (Qmax 4 mL/s), high PVR |
| Diagnosis | Severe functional LUTD | Hinman syndrome (non-neurogenic neurogenic bladder) | Functional LUTD with hypocontractile bladder |
| Treatment | Urotherapy, trospium chloride, CAP, biofeedback | CAP, trospium chloride, CIC, biofeedback | Tamsulosin (Omnic-Tocas), biofeedback |
| Outcome | Initial remission; recurrence after withdrawal, improved with retreatment | Gradual improvement; resolution of UTIs, stable bladder function | Gradual recovery; resolution of acute retention episodes |
| Study / Source | Age / Sex | Neurological Findings | Key Imaging / Cystoscopic Findings | Urodynamic Pattern | Management | Outcome / Remarks |
|---|---|---|---|---|---|---|
| Present Report – Case 1 | 7 y / M | Normal | Crenulated bladder, trabeculated mucosa, pseudopolypoid changes | Detrusor overactivity, small capacity, uninhibited contractions | Trospium chloride, CAP, biofeedback | Resolution of incontinence and UTIs; relapse after withdrawal, improved with retreatment |
| Present Report – Case 2 | 3 y / F | Normal | Grade V VUR, trabeculated pseudopolypoid mucosa, difficult ureteric visualization | Poor compliance, detrusor–sphincter dyssynergia, high PVR | CAP, trospium chloride, CIC, biofeedback | Gradual functional improvement; resolution of UTIs; diagnosed as Hinman syndrome |
| Present Report – Case 3 | 10 y / M | Normal | Large-capacity bladder, mild crenulation, trabeculated trigone | Hypocontractile detrusor, low Qmax (4 mL/s), high PVR | Tamsulosin (Omnic-Tocas), biofeedback | Slow but complete resolution of acute retention |
| Hinman [13] | 6–15 y / Mixed | Normal | Trabeculated, thick-walled bladder; VUR common | Detrusor–sphincter dyssynergia; high pressures | Behavioral retraining, catheterization | Variable; some progressed to renal failure |
| Lee et al. [24] | 5–17 y / 14 pts | Normal | Trabeculation, diverticula, VUR in 50% | Poor compliance; DSD | CIC ± anticholinergics | Improved bladder compliance; preserved renal function in most |
| Chaichanamongkol et al. [26] | 1.5 y / M | Normal | VUR, hydronephrosis | DSD; poor compliance | CIC, CAP | Recovery from renal failure; long-term follow-up stable |
| Gampala et al. [12] | 14 y / M | Normal | Bilateral VUR, trabeculated bladder | DSD; incomplete voiding | Anticholinergic, CIC | Improved voiding and infection control |
| Jayanthi et al. [25] | <2 y / Mixed | Normal | Thickened bladder wall; reflux | DSD, poor compliance | CIC, behavioral therapy | Early infancy presentation; good outcome with early management |
| Wan et al. [27] | 9 y / F | Normal | Normal bladder and urethra | Normal detrusor; voluntary retention | Psychological counseling | Complete recovery; illustrates differential |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.





