The successful implementation of thoracoscopic surgery highly depends on effective lung isolation techniques [
1]. An ideal lung isolation technique must meet the following key requirements: (1) ensuring the ventilation function of the healthy lung, (2) preventing the spread of blood, secretions, and necrotic tumor tissue from the diseased lung to the healthy lung, and (3) achieving complete collapse of the diseased lung to optimize the surgical view [
2]. The two most commonly used lung isolation techniques in clinical practice are the double-lumen tube (DLT) and the bronchial blocker (BO) [
3].
DLT, as a traditional lung isolation tool, has advantages such as independent ventilation of both lungs and thorough separation of secretions, making it particularly suitable for patients with wet lungs and empyema [
4]. However, its larger outer diameter and rigid structure often lead to difficulties in intubation and may cause complications such as airway injury, hypoxemia, and elevated peak airway pressure [
5]. In contrast, BO achieves lung isolation by blocking one side of the bronchus, with its smaller diameter and flexible positioning significantly reducing the difficulty of intubation and the risk of airway injury. As a result, its clinical application has been increasingly widespread in recent years [
6].
With the development of visualization technology, video-assisted intubation systems have provided a new solution for lung isolation techniques. This system integrates a high-definition camera at the tip of the catheter to achieve real-time visualization during intubation, allowing for precise positioning without the need for a laryngoscope. Existing studies show that video-assisted intubation significantly improves the success rate of intubation and reduces airway injury [
7,
8]. While some studies have explored the application of visualization technology in lung isolation, systematic research on the combination of video-assisted intubation and bronchial blockers (BO) is still lacking.
Therefore, this study aims to compare the clinical effects of video-assisted double-lumen tube (VDLT), BO, and their combined use in thoracic surgery through a prospective randomized controlled trial. The focus will be on evaluating the impact on peak airway pressure, lung ventilation time, hemodynamic parameters, and postoperative recovery, with the aim of providing evidence for the optimal selection of lung isolation techniques in clinical practice.
Methods
Sample Source
This study is a prospective randomized controlled trial aimed at evaluating the impact of different lung ventilation methods on airway management during anesthesia in thoracic surgery patients. A total of 135 patients who underwent thoracic surgery under anesthesia and required lung ventilation between May 2020 and May 2024 at our hospital were included. The patients were randomly divided into three groups: Video-Assisted Double-Lumen Tube (VDLT) group (n=45), Bronchial Blocker (BO) group (n=45), and VDLT+BO combined use group (n=45) using a random number table. Informed consent was obtained from all patients prior to surgery, and the study was approved by the ethics committee of our hospital. The inclusion criteria were: age 18 to 80 years, requirement for thoracic surgery, normal lung function or mild ventilation dysfunction, and American Society of Anesthesiologists (ASA) physical status classification of I-IV [
9]. The exclusion criteria were: thoracic deformities or trauma, abnormal cardiopulmonary function, bronchial anomalies with anatomical variations, suspected difficult airway (e.g., thyromental distance <6 cm, mouth opening <3 fingers, Mallampati airway classification III-IV), malignant arrhythmias, severe liver or kidney dysfunction, psychiatric disorders, or severe cognitive impairments [
10]. The research funds are supported by the Huaibei Science and Technology Bureau Fund(rj201806).
Anesthesia Process
After admission, all patients were brought to the operating room where an intravenous access was routinely established and Lactated Ringer’s solution was infused. During the surgery, physiological parameters including heart rate (HR), non-invasive blood pressure (NIBP), oxygen saturation (SpO2), electrocardiogram (ECG), partial pressure of carbon dioxide (PaCO2), and anesthetic depth were monitored. The anesthesia induction regimen included intravenous injections of midazolam 0.05-0.07 mg/kg, fentanyl 1-4 μg/kg, propofol 2 mg/kg, and cisatracurium 0.2 mg/kg. After induction, mask ventilation was performed for 3 minutes to ensure complete muscle relaxation, with the anesthetic trend index maintained within the range of 37-64 and SpO2 stabilized at 100%, before proceeding to intubation.
Intubation Protocol
In the VDLT group, intubation was performed by selecting one side of the main bronchus and inflating the cuff. Visualization technology was used to confirm the position of the cuff, primary carina, and other major bronchial edges to ensure proper placement of the catheter. After insertion, the catheter position was confirmed by auscultation and secured. In the BO group, a fiberoptic bronchoscope was used to guide the precise placement of the bronchial blocker into the required main bronchus. In the VDLT+BO group, the bronchial blocker was advanced into the target main bronchus under guidance from the camera integrated with the video-assisted double-lumen tube, with continuous adjustments made based on bilateral auscultation and real-time monitoring of the blocker position. Once the correct position of the bronchial blocker was confirmed, the patient entered a one-lung ventilation state, and ventilation parameters were adjusted accordingly with a mechanical ventilator. Throughout the process, the positions of the catheter and blocker were continuously monitored and adjusted as needed based on changes in the patient’s surgical position.
Data Collection
During surgery, we compared the peak airway pressure, correct positioning time, and lung ventilation time among the three groups. In addition, hemodynamic parameters were monitored and recorded, including mean arterial pressure (MAP), heart rate (HR), oxygen saturation (SpO2), arterial carbon dioxide partial pressure (PaCO2), arterial oxygen partial pressure (PaO2), forced expiratory volume in 1 second (FEV1), and forced vital capacity (FVC). Postoperatively, we evaluated airway management outcomes, including intubation success rate, postoperative pain score (out of 10), white blood cell count, pneumonia incidence, length of hospital stay, and hospitalization costs.
Statistical Analysis
Statistical analysis was performed using SPSS 22.0 (IBM Corp., USA). Continuous data that met normal distribution (Shapiro-Wilk test, P > 0.05) were expressed as mean ± standard deviation (Mean ± SD), while non-normally distributed data were presented as median (interquartile range) [M (Q1, Q3)]. Categorical data were presented as count (percentage) [n (%)] and analyzed using the chi-squared test (χ²) or Fisher’s exact test (when expected frequencies were <5). Comparisons between groups for continuous variables were conducted using independent samples t-test (with Levene’s test for homogeneity of variances) or one-way analysis of variance (ANOVA), followed by Bonferroni post-hoc test if there were significant differences (P < 0.05). Multivariate analysis included: (1) multiple linear regression to analyze the impact of peak airway pressure, lung ventilation time, and other variables on arterial oxygen partial pressure (PaO2), with validation of linearity assumptions and multicollinearity (VIF < 5) before model construction. Stepwise regression was used to select variables, reporting standardized coefficients (β) and 95% confidence intervals (CI); (2) multinomial logistic regression to analyze postoperative pneumonia as the dependent variable, with intubation method and baseline patient characteristics as independent variables, calculating odds ratios (OR) and 95% CI. For ordered categorical variables, the parallel regression assumption was tested (P > 0.05). The goodness of fit of the models was evaluated using adjusted R² and ANOVA F-test for linear regression, and Hosmer-Lemeshow test (P > 0.05) and Nagelkerke pseudo-R² for logistic regression. A two-tailed P value of <0.05 was considered statistically significant.
Results
Baseline Characteristics
Table 1 presents the baseline characteristics of the study population divided into three groups (N=45 per group). In terms of age distribution, the VDLT group was 47.58±8.20 years, the BO group was 43.23±9.99 years, and the VDLT+BO group was 44.93±9.74 years. The median BMI in each group was comparable: 23.60 (23.12-23.97), 23.02 (21.75-24.29), and 23.31 (22.50-24.70) kg/m². There were slight differences in systolic blood pressure (93.49±9.29, 96.27±6.44, and 91.97±11.53 mmHg), while diastolic pressure remained similar (147. 18±10.21, 147. 18±8.76, and 148.60±10.25 mmHg). Lung function parameters showed minor intergroup differences: FEV1 (2.57, 2.27, and 2.35 L) and FVC (3.25, 3.27, and 3.28 L). The distribution of ASA physical status classification showed a lower proportion of ASA IV patients in the BO group (2.2%) compared to the VDLT group (8.9%) and the VDLT+BO group (11.1%).
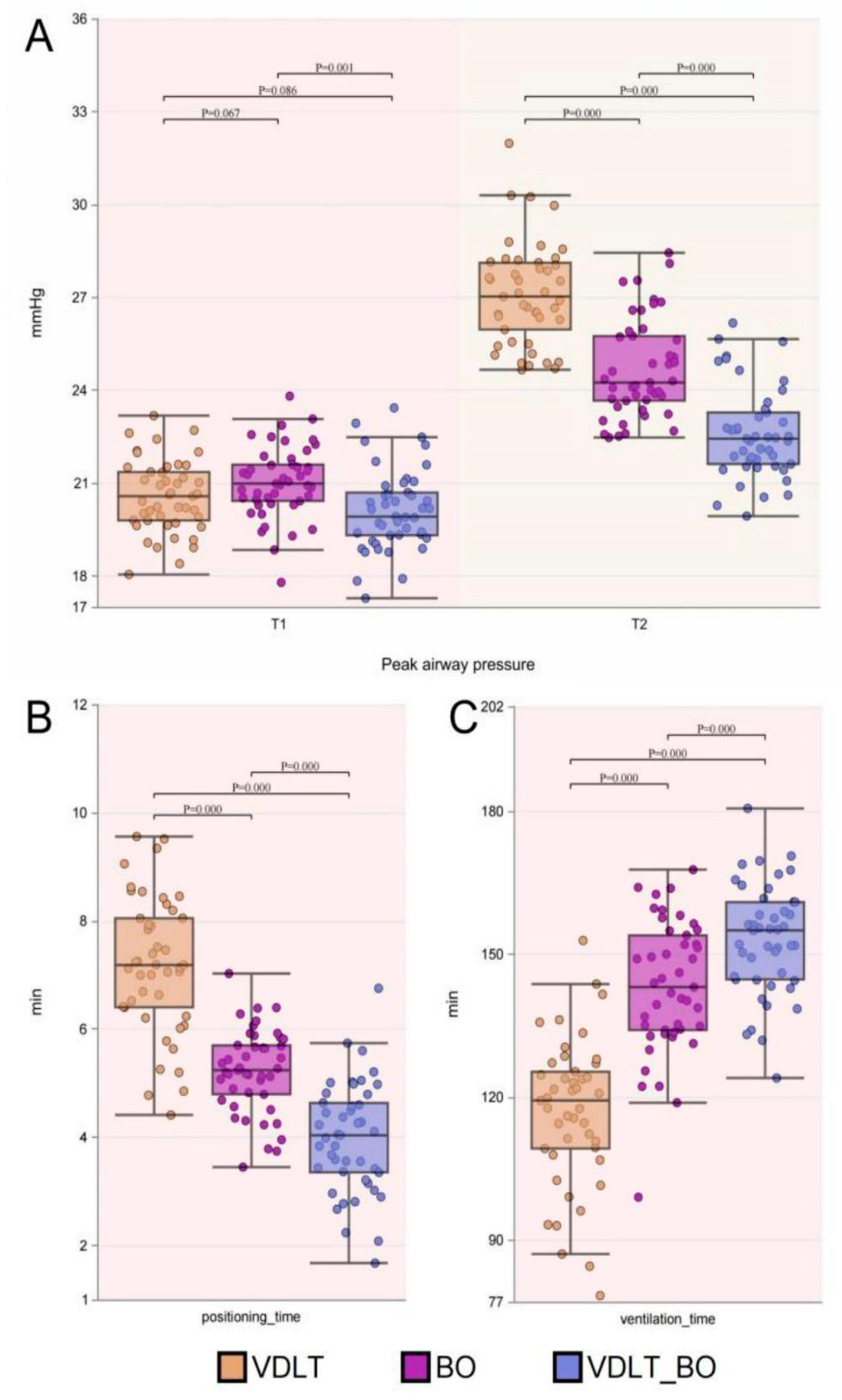
Comparison of Peak Airway Pressure, Correct Positioning Time, and Lung Ventilation Time There was a significant difference in peak airway pressure at time point 1 (peak_pressure_t1) among the three groups (p=0.001), with the BO group, VDLT group, and VDLT+BO group showing mean values of 21.03±1.16, 20.57±1.18, and 20. 12±1.32, respectively. At time point 2 (peak_pressure_t2), the differences were even more pronounced (p<0.001), with mean values of 24.70±1.61 (BO group), 27. 11±1.66 (VDLT group), and 22.61±1.49 (VDLT+BO group). There was also a significant difference in positioning time (p<0.001), with mean values of 5.22±0.77 (BO group), 7. 18±1.27 (VDLT group), and 3.98±1.03 (VDLT+BO group). Ventilation time (p<0.001) was significantly different among the groups, with mean values of 143.03±14.04 (BO group), 116.73±15.70 (VDLT group), and 152.99±11.60 (VDLT+BO group), As shown in
Figure 1.
Comparison of Intubation Success Rates in Different Airway Categories
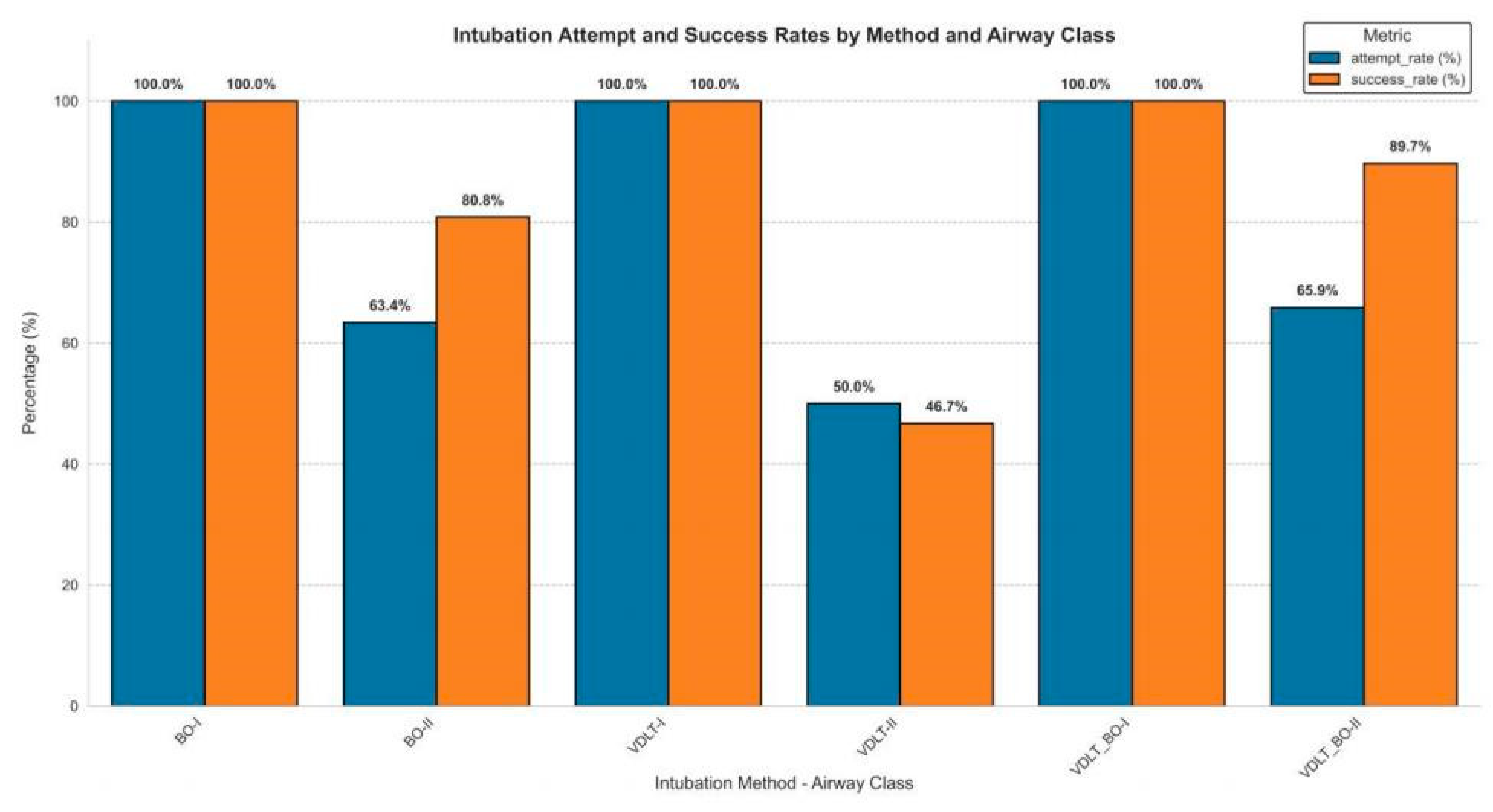
As shown in
Figure 2, The study conducted a stratified analysis of airway management characteristics among the three groups. In patients with Class II airways, the intubation and success rates were slightly higher in the VDLT+BO group compared to the BO group, and significantly higher than in the VDLT group (65.9% vs. 50.2%; 89.7% vs. 46.7%). Notably, in all groups, the intubation failure rate in Class II airway patients was significantly higher than in Class I patients, with the failure rate for Class II patients in the VDLT group as high as 76.7%.
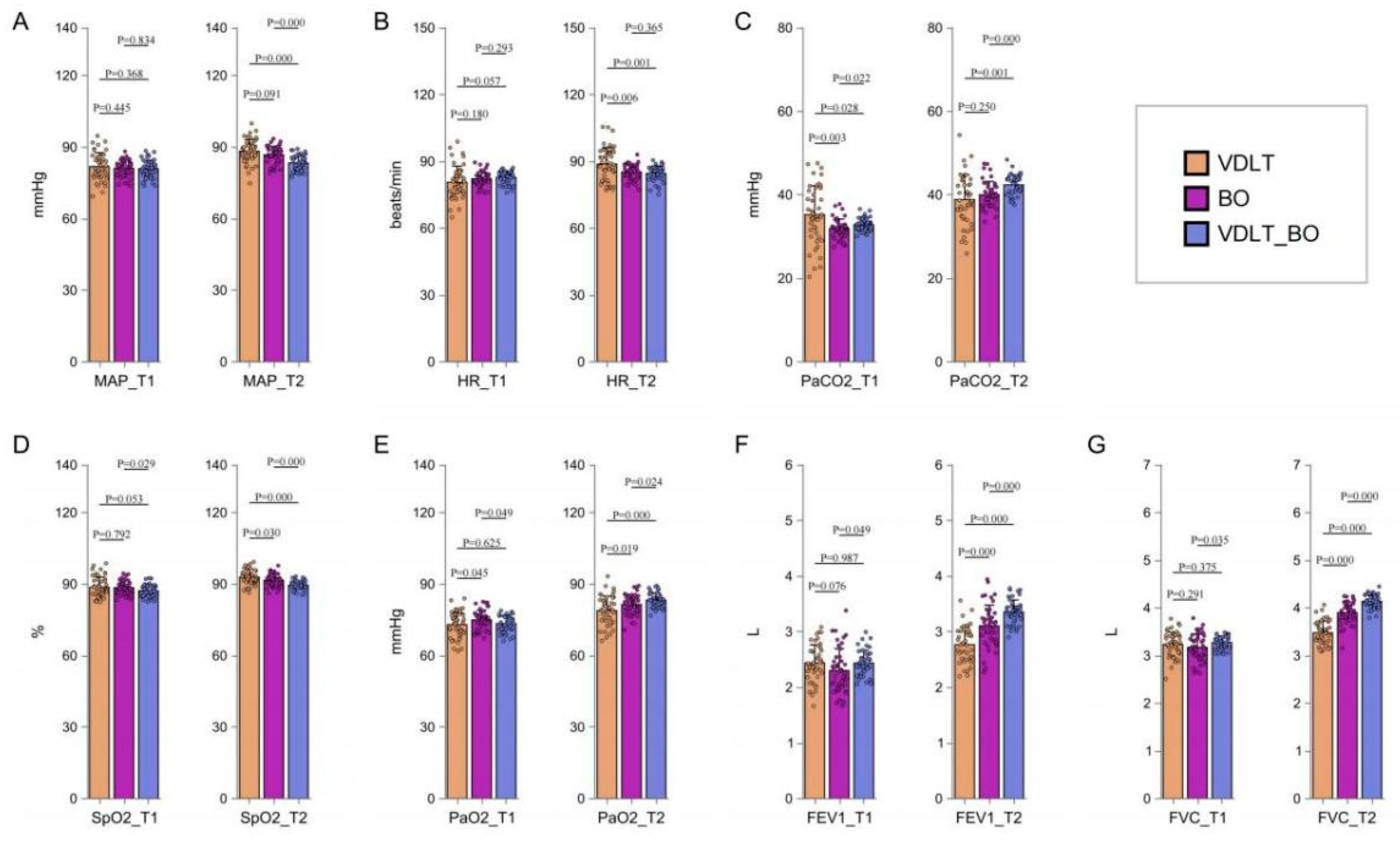
Comparison of Hemodynamic Parameters
Significant differences were observed in multiple hemodynamic parameters among the three groups. At time point 1 (pre-intubation), there was no significant difference in mean arterial pressure (MAP_T1) (p=0.569), while at time point 2 (post-intubation), a significant difference was noted (MAP_T2, p<0.001). Heart rate (HR) at time point 1 (HR_T1) did not show a significant difference (p=0.079), but at time point 2 (HR_T2), the difference was significant (p<0.001). Oxygen saturation (SpO2) showed borderline significant differences at time point 1 (p=0.079), and significant differences at time point 2 (p<0.001). Arterial carbon dioxide partial pressure (PaCO2) showed significant differences at both time points (p<0.001), while arterial oxygen partial pressure (PaO2) only showed significant differences at time point 2 (p<0.001). Lung function parameters showed marginal differences in FEV1 at time point 1 (p=0.073) and significant differences at time point 2 (p<0.001), while FVC showed no significant difference at time point 1 (p=0. 130), but significant differences at time point 2 (p<0.001). These results suggest baseline differences in several physiological parameters, particularly at time point 2 after intervention, Detailed data are presented in
Figure 3.
Comparison of Postoperative Recovery
The three groups showed significant statistical differences in postoperative pain scores (4.66±0.61 vs. 5.34±0.62 vs. 3.73±0.93, F=55.09, p<0.001), length of hospital stay (5.05±0.83 vs. 7.67±1.01 vs. 4.24±1.07, F= 152.00, p<0.001), and hospitalization costs (7694.82±921.31 vs. 9155. 16±1629.53 vs. 6642.53±1248.81, F=42.45, p<0.001). Regarding categorical variables, there was a significant difference in the rate of abnormal white blood cell counts between the groups (χ
2=12.89, p=0.002), with the VDLT group having the highest rate (66.7%) and the VDLT+BO group the lowest rate (28.9%). Pneumonia incidence also differed significantly between the groups (χ
2=6.00, p=0.050), with the VDLT group showing a significantly higher incidence than the other two groups (24.4% vs. 8.9%), See
Table 2 for details. All comparisons were statistically significant (p≤0.05).
Multivariate Analysis
Further analysis using a multiple linear regression model assessed the impact of intubation methods (with the VDLT group as the reference) on post-intubation arterial oxygen partial pressure (PaO2), while controlling for confounding factors such as gender, BMI, and baseline lung function (FEV1%pred). The results showed that the model was statistically significant (F= 10. 12, P<0.001), with an adjusted R2 of 0.22, indicating that the independent variables explained 22% of the variation in PaO2. The estimated intercept was 73.24 (S.E.=2.09, t=35. 1, P<0.001, 95% CI: 69.15—77.33). Compared to the VDLT group, the BO group showed a significant increase in PaO2 by 3. 14 mmHg (β=3. 14, S.E.=0.96, t=3.28, P=0.001, 95% CI: 1.27—5.02), while the VDLT+BO group showed an even more significant increase in PaO2 by 4.70 mmHg (β=4.70, S.E.=0.95, t=4.96, P<0.001, 95% CI: 2.84—6.55), suggesting a potential synergistic effect of the combined approach. Age also had a significant positive effect on PaO2 (β=0. 12, S.E.=0.04, t=2.83, P=0.005, 95% CI: 0.04—0.20), although the effect size was small. In summary, both the intubation method and age were significant positive predictors of post-intubation PaO2, with the VDLT+BO combination showing the most significant improvement, suggesting it may be the optimal choice for optimizing postoperative oxygenation. Detailed data are presented in
Table 3.
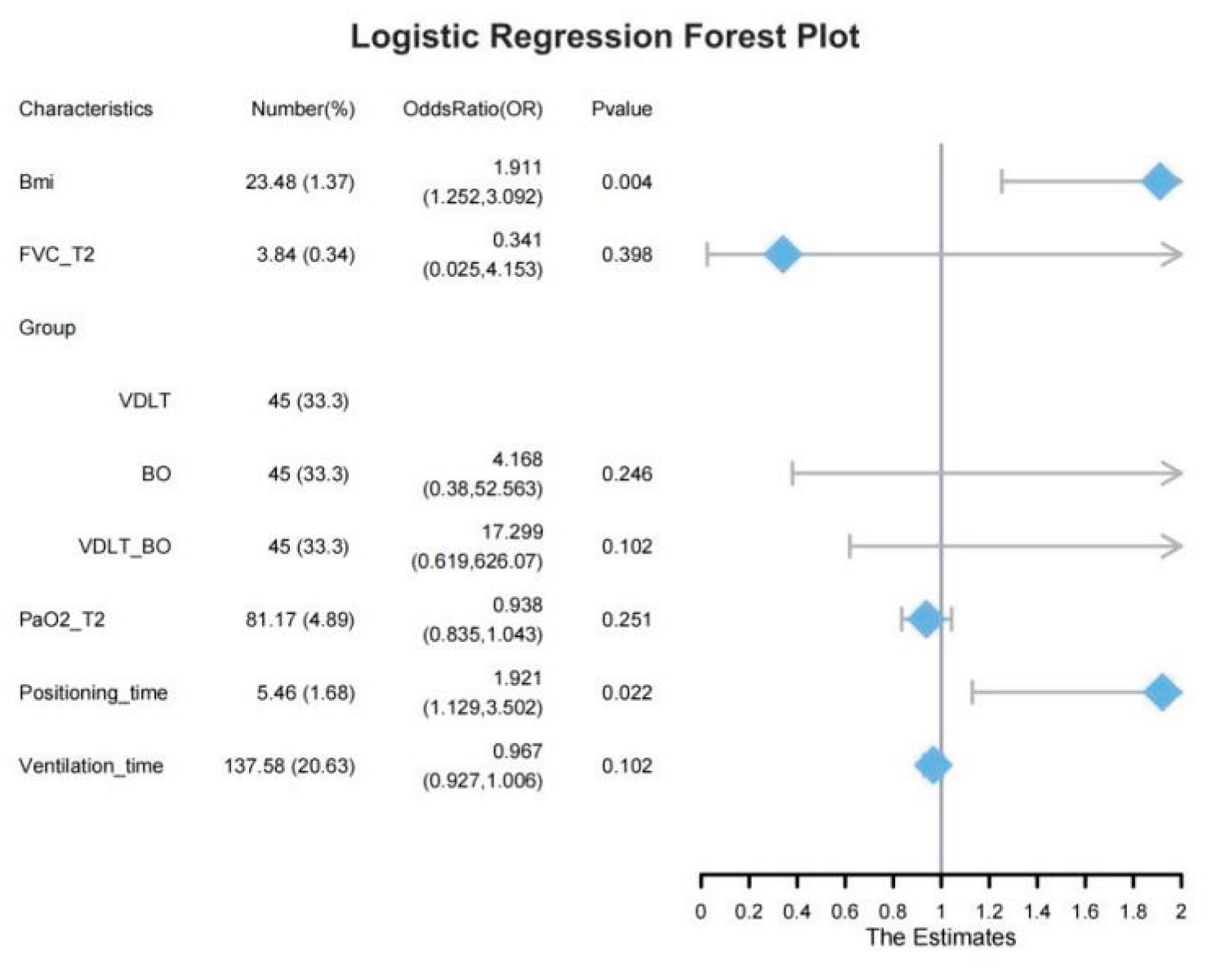
To further investigate the impact of different intubation methods and patient characteristics on postoperative pneumonia, a multivariate logistic regression model was used, with the results presented in a forest plot (
Figure 4). The multivariate logistic regression analysis showed that for each unit increase in BMI (23.48±1.37), the risk of postoperative pneumonia increased significantly (OR= 1.911, 95% CI: 1.252–3.092, P=0.004), suggesting that a higher BMI is an independent risk factor for postoperative pneumonia. Positioning time (mean=5.46±1.88 minutes) also significantly increased the risk with each additional minute (OR= 1.921, 95% CI: 1.129–3.250, P=0.022). Regarding the intubation method (using the VDLT group as the reference), there was no significant difference in pneumonia risk between the BO and VDLT groups (P=0.246), and the risk of postoperative pneumonia was also not significantly different between the VDLT+BO and VDLT groups (P=0.012). Increased BMI and longer positioning time were the primary risk factors for postoperative pneumonia, providing valuable insights for further optimizing perioperative management.
Discussion
This study systematically evaluated the use of video-assisted double-lumen tube (VDLT) combined with a bronchial blocker (BO) in thoracic surgery through a prospective randomized controlled trial, proposing an innovative lung isolation technique combination. The results indicated that the VDLT+BO combined approach demonstrated significant advantages over single-device methods in several areas, including reducing peak airway pressure, shortening positioning time, optimizing hemodynamic stability, and improving postoperative recovery. Specifically, the VDLT+BO combination was effective in reducing peak airway pressure (22.61±1.49 mmHg vs. 27. 11±1.66 mmHg, P<0.001), shortening positioning time (3.98±1.03 minutes vs. 7. 18±1.27 minutes), providing an innovative solution for lung isolation techniques.
By combining video-assisted real-time navigation (VDLT) with minimally invasive bronchial blocking technology (BO), VDLT enables precise airway positioning through high-definition imaging, avoiding the airway injury risks associated with traditional blind intubation, especially in patients with Class II airways, where the intubation success rate was significantly higher [
11]. BO, with its smaller diameter and increased ventilation tube area (50% more than DLT), effectively reduces airway resistance [
12]. Combined with VDLT, it significantly optimizes intraoperative ventilation management, improving PaO₂ (4.70 mmHg, P<0.001). This “visual guidance-minimally invasive occlusion” dual mechanism not only improves airway management during surgery but also offers a new technical combination that enhances the clinical feasibility and safety of lung isolation techniques [
13].
Although BO alone has been associated with a potential increase in airway injury risk, particularly displacement issues, as confirmed by meta-analysis13, the combined approach effectively addresses this risk through real-time visual monitoring of the BO’s position, resulting in the lowest peak airway pressure (22.61±1.49 mmHg). This validates the advantage of BO in reducing airway pressure as noted by Xu et al., and through the integration of these techniques, the safety concerns of BO used alone are mitigated, offering a new perspective for clinical application [
1,
14].
The combined approach also showed clear advantages in postoperative recovery and economic benefits. The incidence of pneumonia in the VDLT+BO group was significantly lower than in the VDLT group (8.9% vs. 24.4%, P=0.050), demonstrating that the BO combined with video-assisted technology effectively reduces the risk of postoperative pneumonia. Additionally, the VDLT+BO group had significantly lower pain scores (3.73±0.93), the shortest hospital stay (4.24±1.07 days), and a 27.4% reduction in hospitalization costs (6642.53±1248.81 yuan vs. 9155.16±1629.53 yuan in the VDLT group). These results indicate that the combined approach not only accelerates recovery but also significantly reduces medical costs, carrying important economic significance [
15].
Moreover, multivariate analysis in this study revealed that positioning time (OR= 1.921, P=0.022) and BMI (OR= 1.911, P=0.004) were key factors influencing postoperative pneumonia [
16]. The VDLT+BO combination may indirectly reduce postoperative inflammation by shortening positioning time and optimizing intubation strategies for obese patients. Notably, in Class II difficult airway patients, the intubation success rate in the VDLT+BO group was 43% higher than in the VDLT group (89.7% vs. 46.7%), providing a new management strategy for high-risk patients [
17]. This result highlights the advantages of this combined technique in difficult airway management and provides effective guidance for managing high-risk patients.
The results of this study contribute to a threefold dialogue with existing literature. First, supportive evidence from Xu et al. [
1]. regarding the minimally invasive advantages of BO and from Liang et al. [
18]. regarding the precision of visualization technology shows that the combined application of these advantages creates a significant synergistic effect. Second, the combined approach effectively avoids the airway injury risks of using BO alone, confirming the feasibility of combining the two techniques. Lastly, the mechanism analysis through multivariate regression revealed that the VDLT+BO combination enhances PaO₂ (β=4.70, P<0.001) and stabilizes hemodynamics, making it an independent predictor for improving oxygenation, providing a deeper understanding of the mechanism behind this technique combination.
Limitations and Future Directions
While this study provides strong evidence, there are some limitations. First, the sample size is relatively small (45 patients per group), and the study was limited to thoracic surgery patients, which may restrict the generalizability of the findings. Second, the study lacks long-term follow-up to assess postoperative pulmonary function changes after three months, which needs further exploration in future studies. Multi-center, large-sample cohort studies will help validate the clinical effects of this technique combination and explore its potential application in complex surgeries (such as tracheal reconstruction).
Conclusions
The VDLT+BO combined approach, through the “visual precision navigation” and “minimally invasive occlusion” dual mechanism, significantly optimizes lung isolation during thoracic surgery. It not only reduces airway injury risk, improves oxygenation, but also accelerates postoperative recovery and reduces medical costs. This study provides high-level evidence for lung isolation techniques and recommends further integration of this approach into clinical practice. Future studies should focus on the adaptability of this technique in various surgical procedures and its long-term clinical effects.
What is known
The traditional lung isolation techniques, including the Video-Assisted Double-Lumen Tube (VDLT) and Bronchial Blocker (BO), each have their advantages but also limitations such as airway injury and higher peak airway pressure, especially when used independently.
Studies have shown the effectiveness of video-assisted intubation in improving success rates and reducing airway injury, but systematic research combining VDLT and BO is limited.
What is new
The study introduces a novel combined approach using VDLT and BO for lung isolation during thoracic surgery. This combination significantly reduces peak airway pressure, shortens positioning time, and improves oxygenation, offering a more effective alternative to single-device methods.
The VDLT+BO combination not only enhances clinical outcomes, such as lowering postoperative pneumonia rates and reducing recovery time, but also provides significant economic benefits, reducing hospitalization costs by 27.4%.
References
- Xin J, Fan XJ. Effect of visual endotracheal tube combined with bronchial occluder on pulmonary ventilation and arterial blood gas in patients undergoing thoracic surgery. Front Surg. 2023;9:1040224. Published 2023 Jan 6. [CrossRef]
- Purohit A, Bhargava S, Mangal V, Parashar VK. Lung isolation, one-lung ventilation and hypoxaemia during lung isolation. Indian J Anaesth. 2015;59(9):606-617. [CrossRef]
- Palaczynski P, Misiolek H, Szarpak L, et al. Systematic Review and Meta-Analysis of Efficiency and Safety of Double-Lumen Tube and Bronchial Blocker for One-Lung Ventilation. J Clin Med. 2023;12(5):1877. Published 2023 Feb 27. [CrossRef]
- Zhang X, Wang DX, Zhang Q, et al. Effect of intubation in the lateral position under general anesthesia induction on the position of double-lumen tube placement in patients undergoing unilateral video-assisted thoracic surgery: study protocol for a prospective, single-center, parallel group, randomized, controlled trial. Trials. 2023;24(1):67. Published 2023 Jan 29. [CrossRef]
- Ghosh S, Klein AA, Prabhu M, Falter F, Arrowsmith JE. The Papworth BiVent tube: a feasibility study of a novel double-lumen endotracheal tube and bronchial blocker in human cadavers. Br J Anaesth. 2008;101(3):424-428. [CrossRef]
- Knoll H, Ziegeler S, Schreiber JU, et al. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology. 2006;105(3):471-477. [CrossRef]
- Hunter CL, Nguyen L, Papa L. Comparing Air Medical Personnel Intubation Success Rates Using Direct, Channeled Video-Assisted, and Unchanneled Video-Assisted Laryngoscopy. Air Med J. 2024;43(6):523-527. [CrossRef]
- Dean P, Kerrey B. Video screen visualization patterns when using a video laryngoscope for tracheal intubation: A systematic review. J Am Coll Emerg Physicians Open. 2022;3(1):e12630. Published 2022 Jan 6. [CrossRef]
- Chalkias A, Papagiannakis N, Saugel B, et al. Association of Preoperative Basal Inflammatory State, Measured by Plasma suPAR Levels, with Intraoperative Sublingual Microvascular Perfusion in Patients Undergoing Major Non-Cardiac Surgery. J Clin Med. 2022;11(12):3326. Published 2022 Jun 10. [CrossRef]
- Hua Y, Huang Q, Chen G, Zhu T. Comparison of modified anterior and traditional posterior accesses for ultrasound-guided superior laryngeal nerve block in awake endotracheal intubation: study protocol for a randomised non-inferiority clinical trial. BMJ Open. 2023;13(2):e068779. Published 2023 Feb 28. [CrossRef]
- Lee J, Kwak HJ, Lee JY, Chang MY, Lee SY, Kim JY. Comparison of the Pentax AirwayScope and McGrath MAC videolaryngoscope for endotracheal intubation in patients with a normal airway. Medicine (Baltimore). 2017;96(46):e8713. [CrossRef]
- Risse J, Szeder K, Schubert AK, et al. Comparison of left double lumen tube and y-shaped and double-ended bronchial blocker for one lung ventilation in thoracic surgery-a randomised controlled clinical trial. BMC Anesthesiol. 2022;22(1):92. Published 2022 Apr 2. [CrossRef]
- Wu Y, Liu Y, Ruan H, et al. Efficiency and safety of double-lumen bronchial tube and bronchial blocker for one-lung ventilation in patients with thoracic surgery: a meta-analysis. BMC Anesthesiol. 2025;25(1):281. Published 2025. 31 May. [CrossRef]
- Li H, Chu L, Ye H, et al. Lung isolation with a bronchial blocker placed in the lateral position for patients undergoing thoracic surgery: A multicenter, randomized clinical trial. J Clin Anesth. 2025;104:111869. [CrossRef]
- Clayton-Smith A, Bennett K, Alston RP, et al. A Comparison of the Efficacy and Adverse Effects of Double-Lumen Endobronchial Tubes and Bronchial Blockers in Thoracic Surgery: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J Cardiothorac Vasc Anesth. 2015;29(4):955-966. [CrossRef]
- Nowak-Tim J, Gaszynski T, Ratajczyk P. A comparison of face-to-face endotracheal intubation and standard intubation using Airtraq video laryngoscope in morbidly obese patients: A randomized controlled trial. Medicine (Baltimore). 2022;101(48):e32046. [CrossRef]
- Gaszyński T, Gómez-Ríos MÁ, Serrano-Moraza A, Sastre JA, López T, Ratajczyk P. New Devices, Innovative Technologies, and Non-Standard Techniques for Airway Management: A Narrative Review. Healthcare (Basel). 2023;11(18):2468. Published 2023 Sep 5. [CrossRef]
- Liang F, Zheng S, Li J, Xiao XS, Wen LH, Lin JG. Application of visible single-lumen tube combined with bronchial occluder in one-lung ventilation surgery. Guangdong Med J. (2019) 40:1791–4. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).