1. Introduction
Artificial intelligence (AI) has emerged as one of the most transformative technologies of the 21st century, profoundly influencing diverse scientific domains, including that of medicine (1). Broadly, AI operates under three major paradigms: symbolic, statistical, and domain-specific (2). Its rapid evolution—from the first AI program in 1951 to the seminal Dartmouth Conference in 1956— laid the foundation for modern applications across numerous fields of healthcare and clinical practice(3).
In medicine, the uneven global distribution of healthcare resources and persistent challenges of subjective diagnosis and medical errors highlight the urgent need for advanced computational technologies(4). AI encompasses a wide spectrum of techniques, including machine learning (ML), deep learning (DL), natural language processing (NLP), and large language models (LLMs), each of which can enhance clinical decision-making and healthcare delivery (5).
AI is increasingly being applied in medical research to analyze large datasets, detect subtle patterns often missed by human interpretation, and accelerate advances in areas such as genomics, biomedical imaging, and drug discovery(6). In clinical settings, AI contributes to diagnostic accuracy, patient-specific treatment planning, prognosis prediction, medical education, and robot-assisted surgery, all of which promise to improve healthcare quality and outcomes(7). Furthermore, AI supports the early detection of chronic diseases, alleviates the economic and societal burden of illness, and facilitates patient engagement in disease management (8).
Key applications of AI in healthcare include machine learning–based algorithms for big data analytics, natural language processing (NLP) for interpreting electronic medical records, image recognition systems for diagnostic support, automation of routine tasks, predictive analytics for individualized treatment strategies, and clinical decision support systems promoting personalized medicine(7, 9, 10). The potential benefits include improved diagnostic speed and precision, reduced human error, wider availability of expertise, and lower costs of care(11). However, challenges exist, such as dependence on large volumes of training data, technical limitations, risks of exclusive reliance on algorithmic decisions, and data privacy concerns (12).
Documenting and sharing evidence-based insights on AI’s integration of AI into healthcare is vital for empowering clinicians and policymakers with the knowledge needed to guide successful implementation. This review aims to provide a comprehensive evaluation of AI in medicine, highlighting its current applications, strengths, limitations, and future opportunities to facilitate its meaningful incorporation into clinical workflows and enhance patient care outcomes(13).
2. Materials and Methods
This study was designed as a narrative review aiming to provide a comprehensive overview of the current landscape of artificial intelligence (AI) and its applications in healthcare. Relevant literature was identified through systematic searches in multiple electronic databases, including PubMed, Web of Science, Scopus, ResearchGate, and Google Scholar, to capture both peer-reviewed and pre-printed materials (12).
The search strategy combined general and domain-specific terms such as artificial intelligence, machine learning, deep learning, natural language processing, large language models, medical imaging, radiology, pathology, endoscopy, laboratory medicine, clinical decision support, drug discovery, precision medicine, rare diseases, paramedicine, and medical education. Priority was given to recent comprehensive reviews and seminal studies that reported validated clinical performance or clear translational potential (14).
After the initial retrieval, all references were deduplicated and curated manually to ensure coverage across the breadth of AI-driven applications in medicine. The inclusion approach was intentionally broad to balance technical, clinical, and educational perspectives, thereby providing a narrative synthesis that reflects both state-of-the-art innovations and practical challenges in their implementation.
3. Artificial Intelligence in Healthcare: Key Applications and Impact
Artificial intelligence (AI) has become a cornerstone of modern medical innovation, fundamentally transforming the landscape of healthcare delivery, research, and clinical decision-making (4). The applications of AI span a broad spectrum—from diagnostic support and treatment planning, to laboratory automation, medical imaging, remote monitoring, and the optimization of administrative tasks. Recent advances have led to the deployment of sophisticated machine learning, deep learning, and natural language processing systems for the early detection of diseases, individualized therapeutic strategies, and evidence-based prognosis prediction(10). As AI integration accelerates, new domains such as rare disease management, genomics, drug discovery, and robotic surgery benefit from enhanced accuracy, efficiency, and personalization (15).
The adoption of AI was further catalyzed during the COVID-19 pandemic, driving innovations in telemedicine, remote patient care, diagnostic automation, and vaccine development (16). Simultaneously, advances in clinical laboratory medicine, endoscopy, pathology, and nursing practice have reshaped traditional workflows and educational paradigms through AI-enabled tools and automation (17). However, the success and long-term impact of these technologies are inextricably linked to the careful handling of challenges related to data privacy, bias, transparency, and regulatory compliance (18).
This review provides a comprehensive synthesis and categorization of AI’s contemporary applications across all major domains of medical science, including, diagnosis and clinical decision support (radiology, pathology, endoscopy, laboratory medicine), personalized medicine (predictive modeling, genomics, rare diseases) therapeutic interventions (surgery, robotic assistance, drug discovery), patient monitoring and remote care (wearable devices, edge computing), administrative and operational optimization, medical education and training (chatbots, large language models), ethical, legal, and regulatory considerations (privacy, bias, accountability).
3.1. Applications of Artificial Intelligence in Healthcare
Artificial intelligence (AI) is increasingly being integrated across diverse domains of healthcare, ranging from diagnosis and treatment planning to patient monitoring and administrative work (19). By leveraging computational approaches, such as machine learning, natural language processing, and computer vision, AI systems can process complex clinical data, enable early disease detection, and provide decision support for healthcare professionals in routine and critical settings (20).
One of the most impactful contributions of AI lies in its capacity to drive personalized medicine, wherein treatment strategies are tailored to individual patient profiles by combining predictive algorithms with real-world clinical data(21). In parallel, AI-enabled solutions help reduce the burden of repetitive administrative tasks through automation, and predictive analytics enhance the forecasting of patient trajectories and clinical outcomes (22).
The COVID-19 pandemic accelerated the adoption of AI technologies in health systems worldwide. During this period, AI was effectively deployed for rapid diagnostic testing, telemedicine and remote patient management, drug repurposing, and even guiding vaccine development pipelines (23, 24).
While these applications highlight the transformative potential of AI in improving healthcare delivery and patient outcomes, their success is closely tied to careful implementation and consideration of ethical and regulatory frameworks. Addressing issues of transparency, data privacy, bias, and accountability remains essential to maximize the safe and equitable integration of AI into routine clinical practice (25, 26). An overview of the representative applications of AI across healthcare domains is illustrated in
Figure 1.
Artificial intelligence (AI) has emerged as a powerful tool for the diagnosis and management of rare diseases, where early and accurate detection is often a critical challenge. In conditions such as Pompe disease, AI-driven algorithms that analyze electronic health records (EHRs) have markedly enhanced the identification of affected individuals, reducing delays in diagnosis and offering greater accuracy in treatment planning (27). Recent advances in machine learning (ML) and deep learning (DL) have enabled the prediction of disease progression and supported the development of optimized treatment strategies for patients with rare and complex conditions. Moreover, advanced architectures, such as recurrent neural networks and graph-based models, demonstrate strong potential for estimating disease probabilities and supporting clinical decision-making based on patient-specific symptom profiles(28, 29).
Beyond diagnosis, AI is accelerating progress in genomics and drug discovery. In areas such as gene editing and precision therapeutics, AI systems improve accuracy and efficiency by screening vast molecular data sets. Machine learning–based approaches have significantly reduced the time and cost of identifying novel drug candidates, thereby streamlining the transition from discovery to clinical trials (30). Although these tools show promise, concerns remain regarding data quality, reproducibility of results, and transparency of algorithms, which must be addressed to maximize their impact in pharmaceutical sciences (31).
AI is also reshaping personalized healthcare by supporting tailored treatment strategies, real-time health monitoring, and predictive systems that anticipate the trajectory of diseases. These applications extend to robotics-assisted surgery, in which AI contributes to surgical planning, intraoperative precision, and enhanced patient safety (32). In continuous monitoring, AI, particularly through edge computing devices, has enabled real-time decision support, structural health monitoring, and adaptive care delivery with ongoing model performance updates (33)
Furthermore, AI has notable implications for nursing practice and education. Chatbots and conversational agents can reduce patient waiting times by delivering timely and individualized health information, whereas large language models, such as ChatGPT, are being piloted for nursing education and clinical training. While promising, these tools raise challenges regarding patient privacy, ethical use, and academic integrity, which require robust governance frameworks (34).
Overall, healthcare organizations worldwide are rapidly embracing AI because of its ability to improve diagnostic accuracy, treatment planning, and patient outcomes (35). The integration of ML, DL, natural language processing (NLP), and predictive analytics into daily practice is reshaping healthcare delivery through automation, personalization, and improved efficiency (36). Particular emphasis is placed on early disease detection, novel drug discovery, and remote patient care, illustrating AI’s transformative role of AI. However, sustainable adoption depends on addressing ethical constraints, regulatory requirements, and implementation standards, ensuring responsible deployment for the long-term benefit of patients and healthcare systems (37).
3.2. Applications of Artificial Intelligence in Medical Science
Artificial intelligence (AI) has emerged as a crucial tool in medical science, offering innovative solutions for diagnostics, treatment planning, and clinical outcome prediction (38). By leveraging computational methodologies, AI systems can identify clinically significant correlations within large and complex datasets, thereby supporting physicians in evidence-based decision-making (39). One of the key enablers in this domain is the application of AI-driven data annotation and labeling services, which streamline clinical workflows and enhance efficiency in both medical research and practice settings (40).
Medical imaging is one of the most widely adopted areas of AI integration. Advanced algorithms are now used to analyze computed tomography (CT), magnetic resonance imaging (MRI), X-rays, and retinal fundus photographs, allowing for the early identification of abnormalities that may signal diseases such as cancer, cardiovascular diseases, and ocular pathologies. Importantly, AI technologies can recognize subtle radiological features often overlooked by the human eye, thereby improving early detection and diagnostic accuracy (41-43).
Beyond medical imaging, AI is extending into predictive modeling through the analysis of electronic health records (EHRs), patient history, laboratory investigations, and clinical symptoms(44). Through such applications, AI algorithms can identify patterns indicative of an elevated disease risk, enabling proactive screening and timely intervention (45). In parallel, the capacity of AI to process large-scale biological datasets, including genomic sequences, proteomic networks, and metabolomic profiles, has accelerated progress in personalized medicine by uncovering molecular signatures associated with disease susceptibility and progression (46). Furthermore, AI integration with remote patient monitoring systems, such as wearable and edge computing devices, enables the continuous assessment of vital signs and activity levels, thereby facilitating the early recognition of disease onset and real-time decision support (47). AI also contributes significantly to medical research by enhancing clinical trial design, surgical procedure optimization, and drug discovery pipelines (48). The integration of AI within the framework of the 4P medicine model (Predictive, Preventive, Personalized, and Participatory) has been particularly impactful, offering tailored diagnostics and individualized therapeutic strategies for complex clinical conditions (4). However, ethical and regulatory considerations remain critical challenges. Issues such as data privacy, algorithmic bias, transparency, and accountability raise concerns regarding the responsible implementation of AI in medical practices(49). Addressing these challenges requires the continuous development of robust guidelines and governance frameworks (50). Some Applications of Artificial Intelligence in Medical Science have been shown in
Figure 2.
3.3. AI Applications in Treatment
Artificial intelligence (AI) technologies have demonstrated wide-ranging benefits in medical treatment, including the advancement of personalized medicine, enhancement of clinical decision-making, and acceleration of drug discovery. Several studies have demonstrated AI's capacity of AI to improve diagnostic precision and efficiency, particularly in identifying diseases such as breast and skin cancers (51). AI enables the development of highly individualized therapeutic regimens by leveraging predictive analytics to identify impending critical health events—such as cardiovascular episodes, acute kidney injury, and sepsis—thereby facilitating early, targeted clinical interventions and significantly enhancing patient outcomes through data-driven precision (52). In clinical decision-making, AI systems serve as valuable tools by providing evidence-based recommendations that assist healthcare professionals in making informed and timely treatment choices. These AI-driven decision support systems analyze comprehensive patient data, enabling a tailored approach to therapy that aligns with the individual health profiles (53). Furthermore, in medical research, machine learning algorithms are used to process large-scale patient information and medical records. This allows the identification of hidden correlations and patterns, aiding the development of personalized treatment plans that are both effective and adaptive to patient-specific needs (54). The integration of AI in treatment and diagnostic approaches continues to expand, as illustrated in
Figure 3.
3.4. Current Applications of AI in Medicine
Recent advances in Artificial Intelligence (AI), especially through deep learning, a powerful subset of machine learning algorithms, have ignited renewed interest in AI’s transformative potential of AI in medicine (55). Early pioneering AI systems, such as Internist-1, MYCIN, and CASNET, laid the groundwork for modern intelligent decision-support tools and databases used in clinical settings. AI has permeated numerous medical fields, ushering in a paradigm shift often described as "AI plus medicine"the synergistic integration of AI technologies with clinical practice, heralding revolutionary changes in healthcare delivery (56).
In paramedicine, AI-driven systems that combine voice and text data processing have shown promise in augmenting the emergency medical services. By utilizing advanced deep learning architectures, such as Long Short-Term Memory (LSTM) networks and convolutional neural networks (CNNs), these systems can classify complex patient information, including medical histories, treatment regimens, and medication alerts. This enables the timely delivery of medication notifications and improves paramedic responsiveness, ultimately prioritizing patient care and reducing errors. The integration of AI into paramedic workflows holds significant potential for streamlining emergency response and optimizing patient outcomes in critical settings (57, 58).
3.4.1. AI in Radiology
Radiology is a cornerstone of medical diagnostics, with a strong scientific foundation essential for the evaluation of numerous diseases. As the demand for diagnostic radiology services steadily increases alongside the growing expertise of radiologists, the rising workload and risk of human error highlight the urgent need for innovative solutions, such as artificial intelligence (AI), to enhance diagnostic accuracy and efficiency (59).
Recent advances in deep learning have led to the development of high-sensitivity algorithms for early disease detection. Francesco et al. introduced a novel algorithm capable of rapid diagnosis and classification of retinal disorders, findings that are supported by other contemporary studies demonstrating AI’s capacity to detect subtle imaging features overlooked by human observers (60). Similarly, Gong et al. developed a computer-aided diagnosis (CADx) system utilizing AI to discriminate between benign and malignant pulmonary nodules based on clinical CT data from 243 patients. By further integrating quantitative imaging features with serum biomarker profiles in 173 patients, their model achieved enhanced accuracy in nodule classification, underscoring AI’s role of AI in multimodal diagnostic approaches (61). Rodriguez-Ruiz et al. compared AI system performance with that of radiologists in breast cancer detection from mammographic images, revealing that AI integration not only surpassed radiologists in accuracy but also reduced workload by 88%. Automated preselection functions implemented in breast cancer screening have substantially alleviated clinical burdens, fostering faster and more reliable diagnosis (62).
In magnetic resonance imaging (MRI) analysis, AI algorithms have demonstrated superior sensitivity to human experts in detecting early inflammatory changes indicative of rheumatoid arthritis, enabling earlier treatment initiation and better patient management (63).
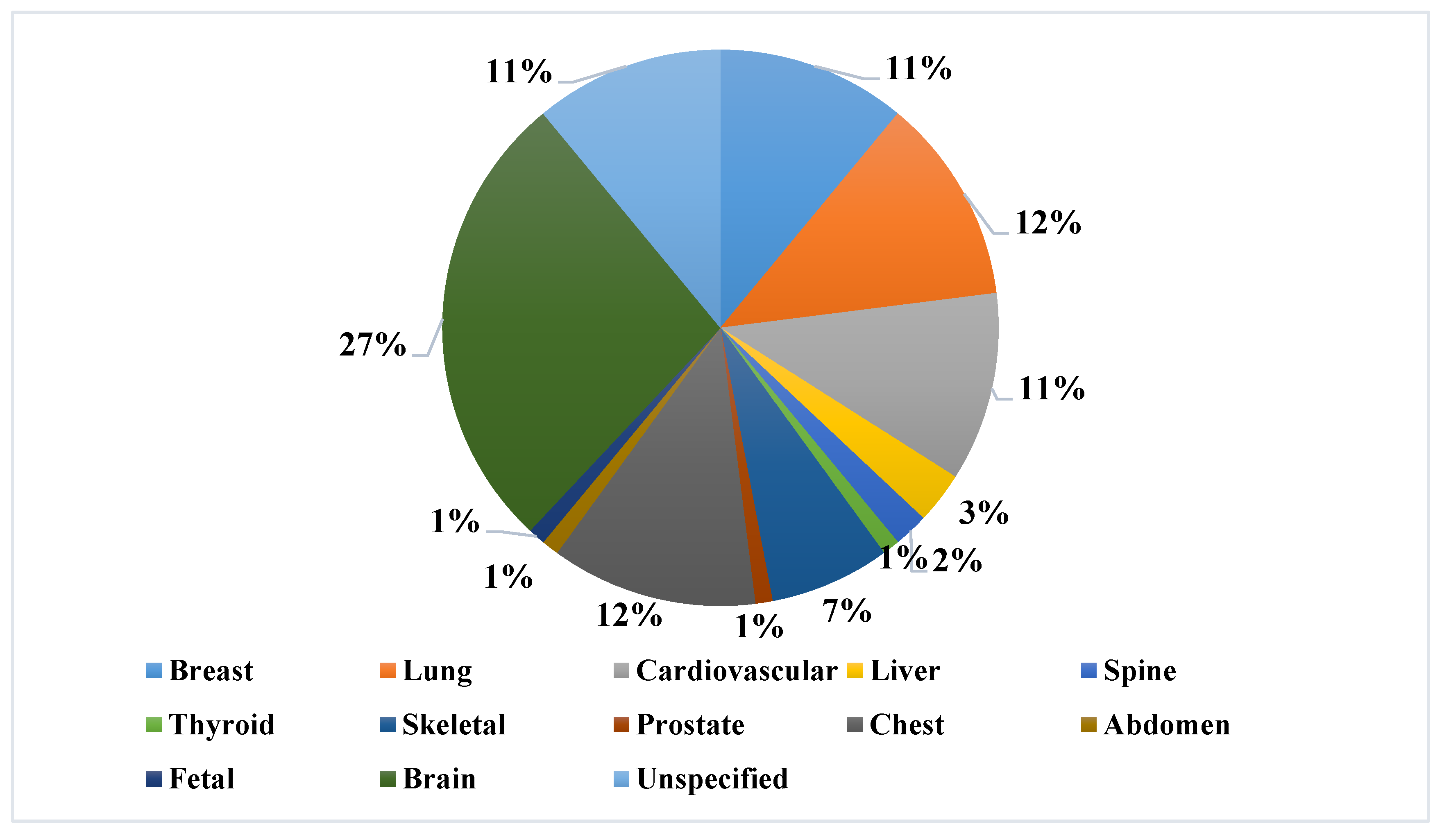
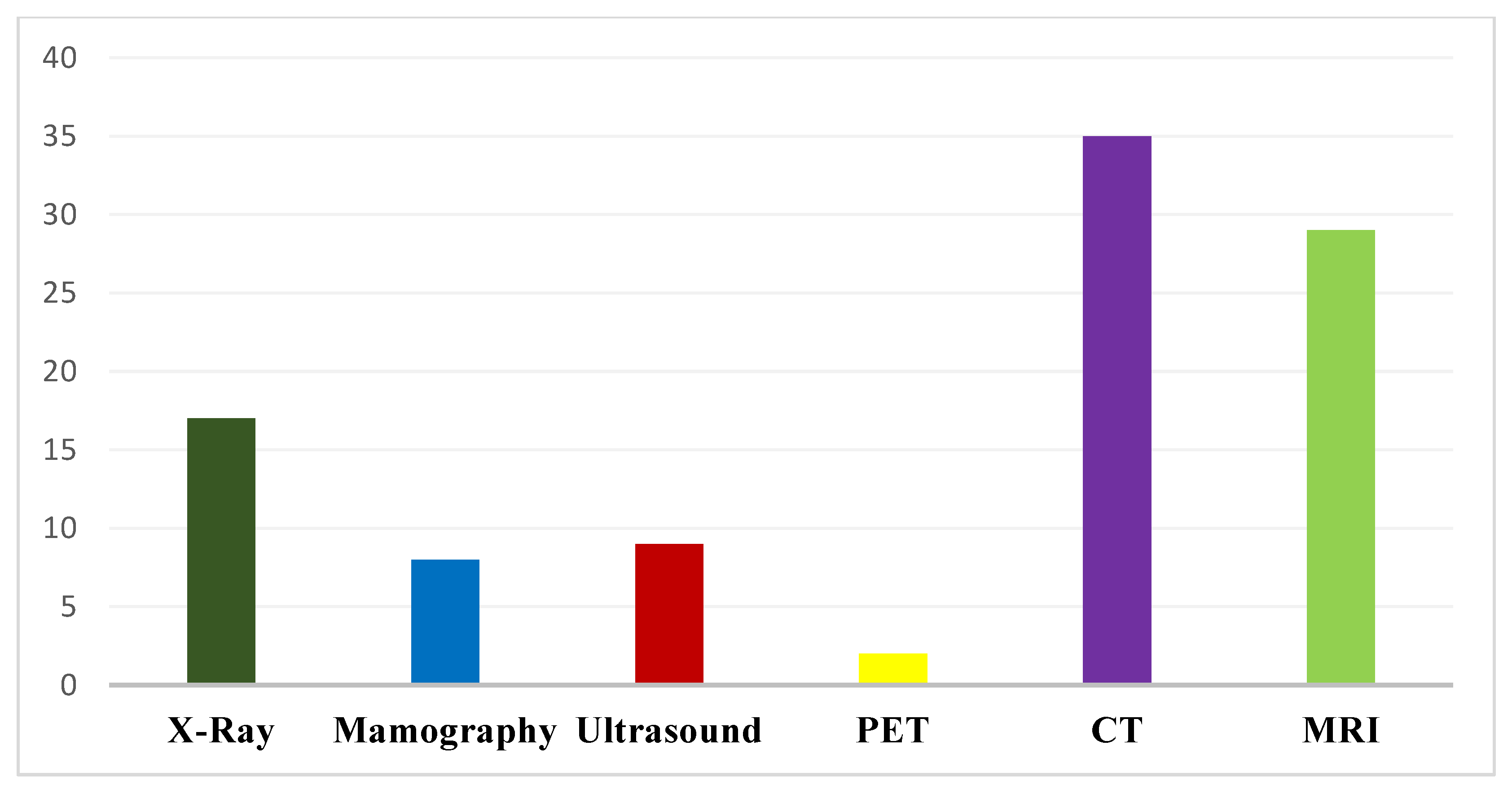
Chart 1 and
Chart 2 illustrate AI applications focusing on specific anatomical regions and diverse radiology modalities, highlighting the accelerating integration of AI into radiologic practices.
3.4.2. AI in Pathology
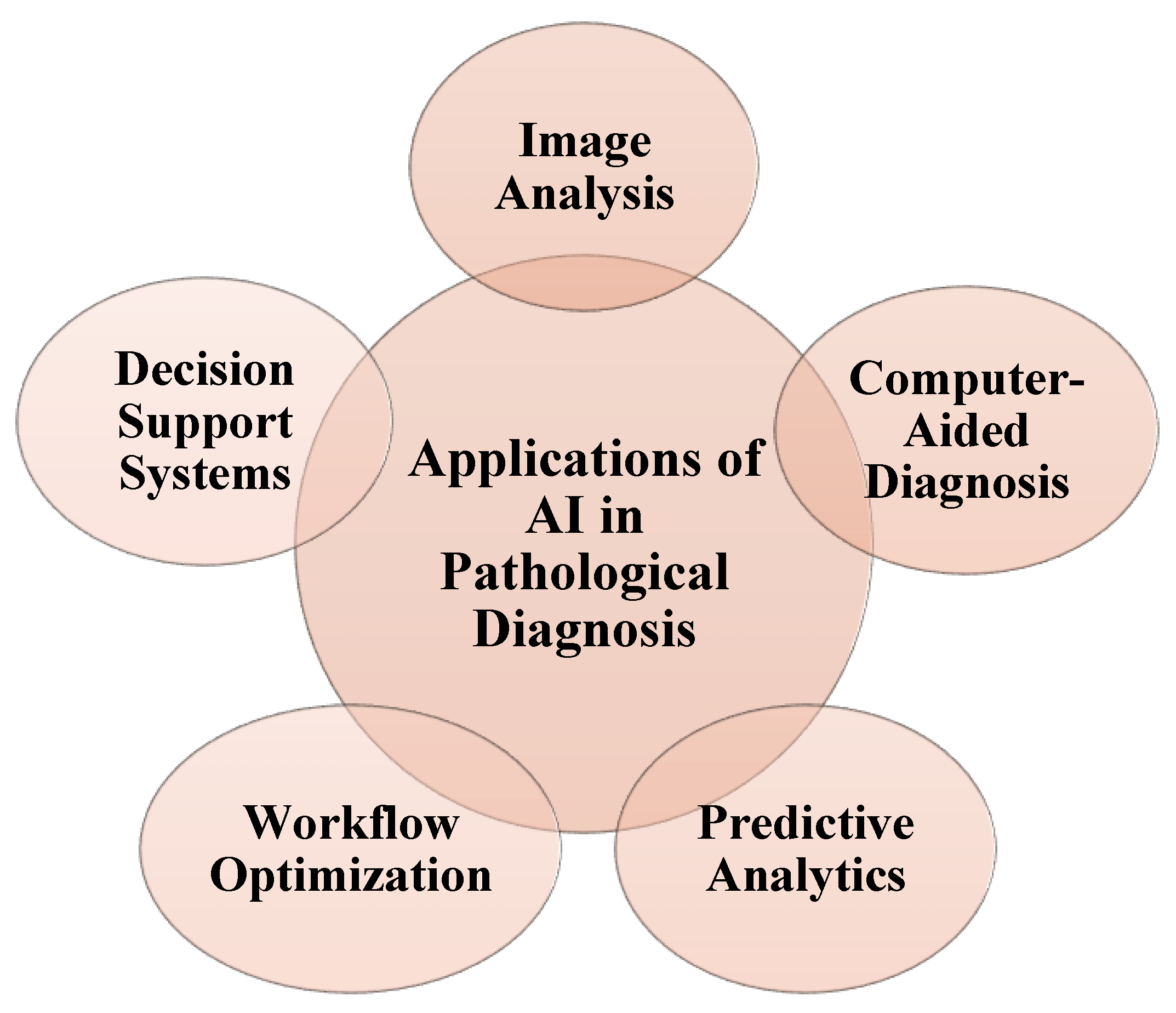
Pathology is a cornerstone of medical diagnosis, particularly in the early detection and classification of cancer. Advances in digital slide scanning and associated software technologies have markedly improved the accuracy of tumor recognition and lesion characterization. In this context, artificial intelligence (AI) has emerged as a transformative force and is increasingly regarded as the next frontier in precision pathology (64).
Significant progress has been achieved in image segmentation, tumor detection, and metastasis evaluation by refining machine learning and deep learning algorithms, ultimately enhancing the quality and efficiency of diagnostic workflows (65). In certain scenarios, AI systems have been shown to outperform human experts in terms of diagnostic accuracy (66).
For instance, AI-based models have demonstrated high precision in distinguishing Spitz lesions from normal melanocytic networks. Furthermore, researchers have introduced multitasking deep learning models that can analyze pathological images across multiple scales simultaneously. When applied to gastric cancer specimens with varying degrees of differentiation, these models outperformed other state-of-the-art AI approaches, offering higher diagnostic efficiency and accuracy. Notably, the system could predict six clinically relevant cancer-associated genetic mutations with an accuracy exceeding 97%, thereby facilitating subtype classification and genomic profiling (67).
These applications are not limited to gastric cancers. AI has been successfully employed in the diagnosis of epithelial tumors, lung cancer, basal cell carcinoma, and glomerulosclerosis, underscoring its growing relevance across a wide spectrum of pathological conditions. Collectively, these developments illustrate how the integration of AI in pathology accelerates diagnostic workflows and fosters a shift towards personalized, data-driven clinical decision-making (68). The applications of artificial intelligence in pathological diagnosis are shown in
Figure 4.
3.4.3. AI in Endoscopy
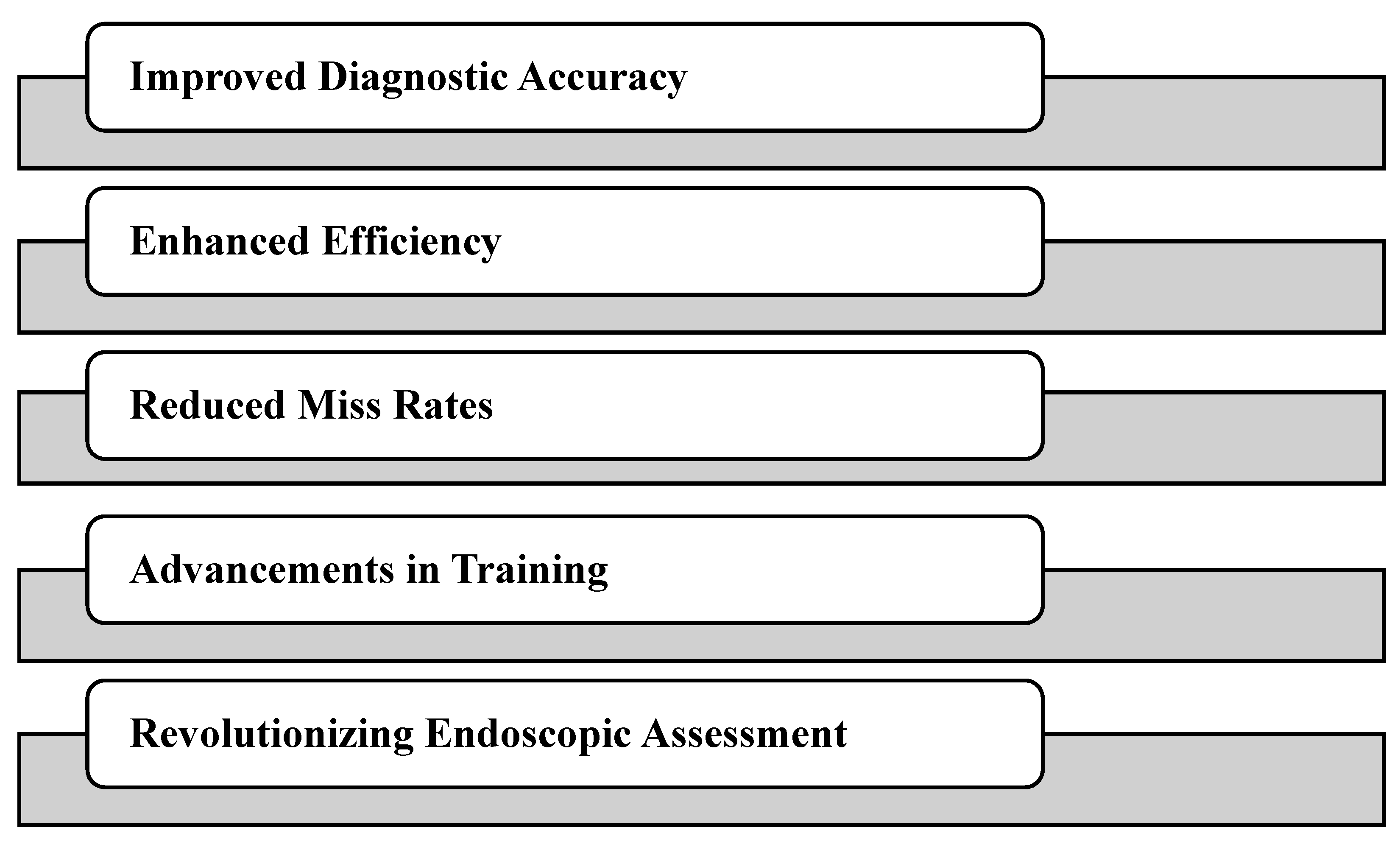
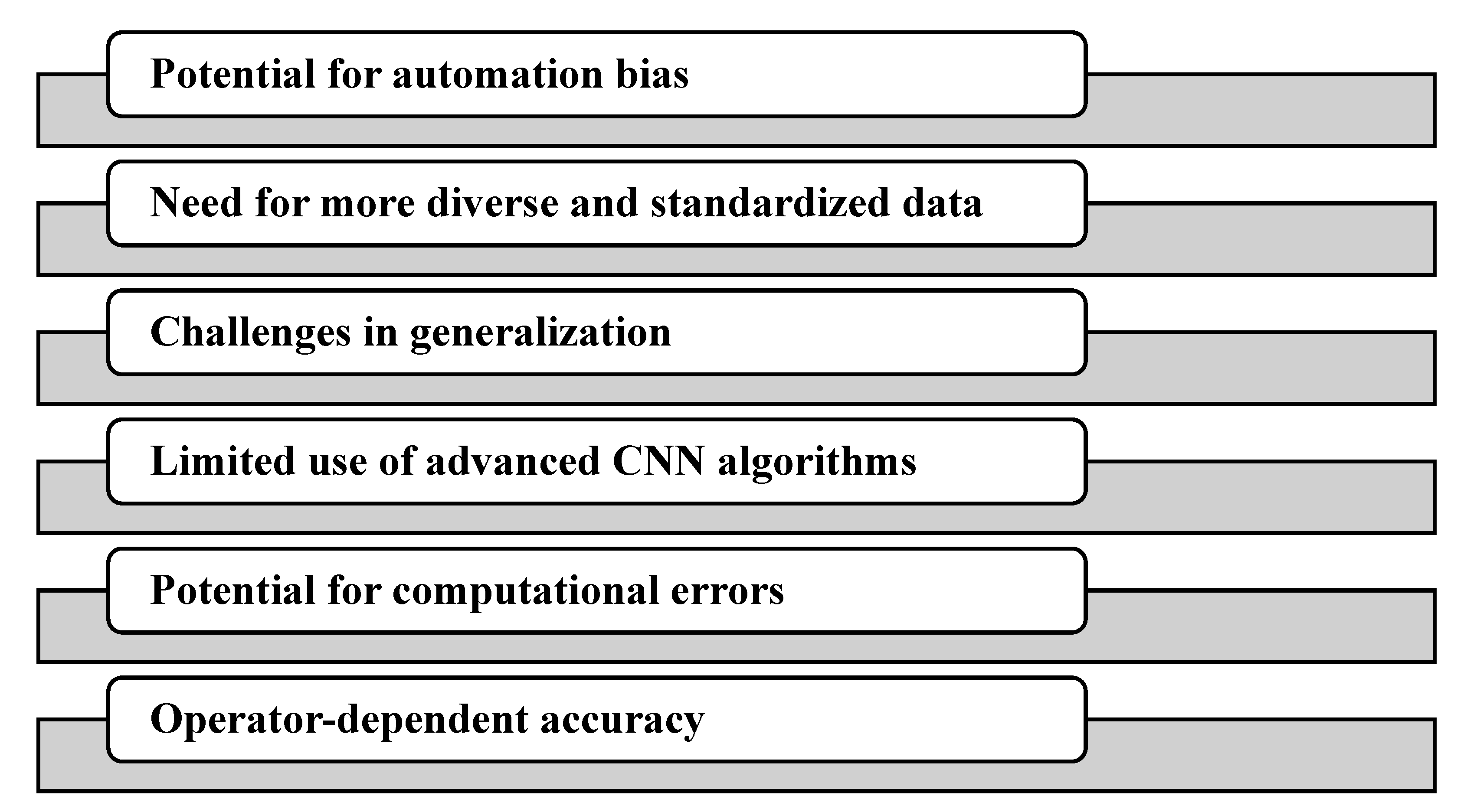
Artificial intelligence (AI) is increasingly transforming endoscopy by enhancing diagnostic accuracy, improving patient outcomes, and streamlining clinical workflows. Among AI approaches, convolutional neural networks (CNNs) have demonstrated particular value in endoscopic ultrasound (EUS) and video capsule endoscopy (VCE), where they aid in the detection and characterization of lesions, thereby reducing the need for repeated procedures (69). A growing body of evidence indicates that integrating AI into endoscopic practice significantly improves the diagnostic performance of a wide spectrum of gastrointestinal (GI) diseases, including Barrett’s esophagus, colorectal polyps, gastric cancer, adenomas, and gastrointestinal bleeding (70-72). By enabling the identification of subtle pathological features that may be overlooked during real-time examination, AI enhances the timeliness and precision of clinical decision-making. In gastrointestinal endoscopy, AI is advancing applications across multiple procedural domains, such as esophagogastroduodenoscopy (EGD), capsule endoscopy (CE), and colonoscopy (73).
AI algorithms have been employed in EGD for cancer detection, depth-of-invasion assessment, and prediction of Helicobacter pylori infection. In capsule endoscopy, automated systems have been developed to detect bleeding sites, ulcers, and neoplastic lesions, thereby reducing reading time and inter-observer variability. In colonoscopy, CNN-based models assist in the automated identification, classification, and risk stratification of colorectal polyps, directly contributing to improved adenoma detection (74).
AI also shows promise in the management of inflammatory bowel disease (IBD). By supporting the quantification of mucosal disease activity, AI tools enhance both baseline disease assessment and the longitudinal monitoring of therapeutic interventions. Importantly, these systems not only increase diagnostic efficiency but also reduce inter-observer variation, a longstanding challenge in IBD evaluation (75).
Furthermore, AI models applied to upper GI endoscopy have demonstrated high accuracy in detecting, delineating, and staging esophageal and gastric cancers. Their use has been shown to reduce operator-dependent errors and support reliable real-time interpretation of endoscopic images. Recent clinical trials have also incorporated AI for tasks such as polyp detection and classification, bowel preparation quality scoring, and treatment response assessment, highlighting the growing clinical relevance of these technologies(76, 77). The advantages of using artificial intelligence in endoscopy are shown in
Chart 3. The limitation of using artificial intelligence in endoscopy are illustrated in
Chart 4.
3.4.4. AI in Laboratory Medicine
Artificial intelligence (AI) is reshaping the functioning of clinical laboratories, bringing major improvements in efficiency, accuracy, and delivery of personalized care (78). Integrating artificial intelligence (AI) and machine learning (ML) into laboratory medicine allows for more reliable quality assessment of diagnostic tests. For instance, studies have shown that AI can distinguish between inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) with high sensitivity and specificity, making it easier to identify patients and decide when further testing is needed (79).
One of the most promising areas is computer vision, where AI supports digital pathology by streamlining workflows, reducing human errors, and improving diagnostic consistency. These advances suggest that AI is not just an auxiliary tool but an essential component of modern diagnostic laboratories (80).
AI and ML are also transforming the daily operations of clinical laboratories. Beyond test processing, these technologies assist with interpreting results, suggesting the most appropriate tests, and supporting clinicians in making accurate and data-driven diagnoses. The benefits include improved diagnostic accuracy, enhanced operational efficiency, and better patient service delivery (81).
Practical applications include automating spectroscopy data analysis, disease detection, and digital image analysis across various pathology specialties. AI can also generate standardized reports, handle repetitive data entry, reduce inappropriate test requests, predict outcomes, and improve quality control by early identification of abnormal results(82).
Some highly specialized use cases are already being implemented. For example, the Mayo Clinic has developed an AI model to automate the spectral analysis of kidney stones, significantly reducing the time and cost. Similarly, AI tools in clinical microbiology are used to identify ova and parasites in stool samples, boosting both accuracy and efficiency (83, 84).
4. Discussion
The use of artificial intelligence (AI) in medical education has notable benefits, ranging from simulating realistic clinical scenarios to strengthening diagnostic reasoning and communication skills, ultimately improving patient care outcomes. Despite these advantages, certain challenges remain to be addressed. AI is not yet capable of producing flawless role-play scripts, students still need to demonstrate genuine understanding during assessments, and ethical considerations around the responsible use of AI must be carefully addressed (85).
Addressing these issues requires ongoing research to evaluate the impact of AI on different areas of medical education. This includes integrating AI tools into coursework, designing curricula that build AI literacy, and encouraging active knowledge exchange between students and faculty. By leveraging AI responsibly, while remaining aware of its current limitations, medical education can be enhanced to prepare future healthcare professionals with stronger skills and deeper knowledge, ultimately leading to improved outcomes for patients (81). The key benefits, challenges, and potential solutions regarding the application of AI in medical education are summarized in
Table 1.
The integration of artificial intelligence (AI) into healthcare is rapidly advancing, bringing clear benefits, such as greater efficiency, streamlined workflows, and enhanced patient care. AI applications in medical devices generally fall into three main categories: data collection, data analysis, and active treatment. Within these domains, AI has become particularly valuable in areas such as clinical imaging, data exchange, large-scale data processing, and the development of machine learning models for disease prediction and classification (82).
A wide range of medical specialties, including oncology, pulmonology, cardiology, orthopedics, hepatology, and neurology, are already leveraging AI to support both clinical practice and research. Common applications include clinical decision support and imaging analysis, which help clinicians generate deeper insights, improve diagnostic accuracy, and strengthen patient experiences and outcomes (83).
Despite these benefits, the adoption of AI in healthcare faces important challenges. Concerns regarding privacy, fairness, equity, and accountability remain central to whether AI systems will gain the trust of both professionals and patients. Therefore, building confidence in AI-powered medical technologies is essential for their global acceptance and effective implementation (84).
When integrated responsibly, AI has the potential to revolutionize healthcare practices. It can accelerate research, assist clinicians in decision-making, and enhance patient safety through various applications, from disease detection and diagnostic support to personalized treatment planning, medical imaging, drug development, and clinical trial optimization. Embedding AI tools directly into clinical workflows adds meaningful context to care decisions, whereas AI-driven decision-support systems can improve error detection and strengthen drug management (85).
5. Conclusions
In summary, artificial intelligence (AI) is rapidly becoming an integral part of modern healthcare, reshaping the approach of clinicians and researchers to clinical problem-solving. AI already plays a vital role in everyday practice, from managing electronic health records and supporting diagnostic decisions to assisting in medication prescriptions, mental health assessments, and medical image analysis.
However, the effective and responsible integration of AI into routine healthcare requires more than technical adoption. This calls for a balanced understanding of both its capabilities and limitations, as well as collaboration across disciplines. Expertise in ethics, philosophy, sociology, psychology, behavioral science, and economics is essential to address the broader implications of machine behavior. Only through this multidisciplinary perspective can AI achieve its full potential to enhance healthcare while safeguarding human values and patient trust.
Acknowledgments
The authors would like to express their profound gratitude to Almighty God for granting them the wisdom, patience, and strength to accomplish this research. The successful completion of this study would not have been possible without His divine guidance and blessings. This work is dedicated to His infinite mercy and grace.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this manuscript.
References
- Rong, G.; Mendez, A.; Assi, E.B.; Zhao, B.; Sawan, M. Artificial intelligence in healthcare: review and prediction case studies. Engineering. 2020, 6, 291–301. [Google Scholar] [CrossRef]
- Hulsen, T. Explainable artificial intelligence (XAI): concepts and challenges in healthcare. Ai. 2023, 4, 652–66. [Google Scholar] [CrossRef]
- Shortliffe, E.H.; Sepúlveda, M.J. Clinical decision support in the era of artificial intelligence. Jama. 2018, 320, 2199–200. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: the convergence of human and artificial intelligence. Nature medicine. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Liu, X.; Faes, L.; Kale, A.U.; Wagner, S.K.; Fu, D.J.; Bruynseels, A.; et al. A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: a systematic review and meta-analysis. The lancet digital health. 2019, 1, e271–e97. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, M.Y. Applications of Artificial Intelligence (AI) in healthcare: A review. ScienceOpen Preprints. 2021. [Google Scholar]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; et al. Artificial intelligence in healthcare: past, present and future. Stroke and vascular neurology. 2017, 2. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Casalino, L.P.; Khullar, D. Deep learning in medicine—promise, progress, and challenges. JAMA internal medicine. 2019, 179, 293–4. [Google Scholar] [CrossRef]
- Gurav, P. Natural language processing in electronic health records: a review. Artificial Intelligence in Health. 2024, 1, 16–31. [Google Scholar] [CrossRef]
- Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; DePristo, M.; Chou, K.; et al. A guide to deep learning in healthcare. Nature medicine. 2019, 25, 24–9. [Google Scholar] [CrossRef] [PubMed]
- Panahi, O. AI in Healthcare Administration: Streamlining Processes for a More Efficient Future. 2025.
- Chustecki, M. Benefits and risks of AI in health care: Narrative review. Interactive Journal of Medical Research. 2024, 13, e53616. [Google Scholar] [CrossRef]
- Jacob, C.; Brasier, N.; Laurenzi, E.; Heuss, S.; Mougiakakou, S.-G.; Cöltekin, A.; Peter, M.K. AI for IMPACTS framework for evaluating the long-term real-world impacts of AI-powered clinician tools: systematic review and narrative synthesis. Journal of medical Internet research. 2025, 27, e67485. [Google Scholar] [CrossRef]
- Nilsen, P.; Sundemo, D.; Heintz, F.; Neher, M.; Nygren, J.; Svedberg, P.; Petersson, L. Towards evidence-based practice 2.0: leveraging artificial intelligence in healthcare. Frontiers in health services 2024, 4, 1368030. [Google Scholar] [CrossRef]
- Chen, J.H.; Asch, S.M. Machine learning and prediction in medicine—beyond the peak of inflated expectations. The New England journal of medicine. 2017, 376, 2507. [Google Scholar] [CrossRef]
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020, 14, 337–9. [Google Scholar]
- Montejo, L.; Fenton, A.; Davis, G. Artificial intelligence (AI) applications in healthcare and considerations for nursing education. Nurse Education in Practice. 2024, 80, 104158. [Google Scholar] [CrossRef] [PubMed]
- Guidance, W. Ethics and governance of artificial intelligence for health. World Health Organization. 2021. [Google Scholar]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; et al. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC medical education. 2023, 23, 689. [Google Scholar] [CrossRef]
- Satapathy, P.; Hermis, A.H.; Rustagi, S.; Pradhan, K.B.; Padhi, B.K.; Sah, R. Artificial intelligence in surgical education and training: opportunities, challenges, and ethical considerations–correspondence. International Journal of Surgery. 2023, 109, 1543–4. [Google Scholar] [CrossRef]
- Shaban-Nejad, A.; Michalowski, M.; Bianco, S. Creative and generative artificial intelligence for personalized medicine and healthcare: Hype, reality, or hyperreality? : SAGE Publications Sage UK: London, England; 2023. p. 2497-9.
- Reddy, S.; Fox, J.; Purohit, M.P. Artificial intelligence-enabled healthcare delivery. Journal of the Royal Society of Medicine. 2019, 112, 22–8. [Google Scholar] [CrossRef]
- Huang, J.A.; Hartanti, I.R.; Colin, M.N.; Pitaloka, D.A. Telemedicine and artificial intelligence to support self-isolation of COVID-19 patients: Recent updates and challenges. Digital health. 2022, 8, 20552076221100634. [Google Scholar] [CrossRef]
- Paul, M.M.; Khera, N.; Elugunti, P.R.; Ruff, K.C.; Hommos, M.S.; Thomas, L.F.; et al. The State of Remote Patient Monitoring for Chronic Disease Management in the United States. Journal of Medical Internet Research. 2025, 27, e70422. [Google Scholar] [CrossRef] [PubMed]
- Botes, M.; Lobban, G. Building an artificial intelligence-enabled telehealth future for South Africa: The case for regulatory vision and sectoral strategy. SAMJ: South African Medical Journal. 2025, 115, 6–7. [Google Scholar] [CrossRef]
- Bergquist, R.; Rinaldi, L.; Zhou, X.-N. Artificial intelligence for healthcare: restrained development despite impressive applications. Infectious Diseases of Poverty. 2025, 14, 72. [Google Scholar] [CrossRef]
- Nishat, S.M.H.; Tanweer, A.S.; Alshamsi, B.; Shaheen, M.H.; Tanveer, A.S.; Nishat, A.; et al. Artificial intelligence: A new frontier in rare disease early diagnosis. Cureus. 2025, 17. [Google Scholar] [CrossRef]
- Karako, K. Artificial intelligence applications in rare and intractable diseases: Advances, challenges, and future directions. Intractable & Rare Diseases Research. 2025, 14, 88–92. [Google Scholar]
- Schumacher, E.; Naik, D.; Kannan, A. Rare Disease Differential Diagnosis with Large Language Models at Scale: From Abdominal Actinomycosis to Wilson's Disease. arXiv:250215069. 2025.
- Haapalainen, B. Artificial Intelligence and Patient Centeredness in the Pharmaceutical Industry. 2025.
- Lotter, W.; Hassett, M.J.; Schultz, N.; Kehl, K.L.; Van Allen, E.M.; Cerami, E. Artificial intelligence in oncology: current landscape, challenges, and future directions. Cancer discovery. 2024, 14, 711–26. [Google Scholar] [CrossRef]
- Bhagat, S.V.; Kanyal, D. Navigating the future: the transformative impact of artificial intelligence on hospital management-a comprehensive review. Cureus. 2024, 16. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.-Y.; Hsu, Y.-L.; Chung, C.-L.; Chen, H.-C.; Horng, M.-H.; Lin, C.-H.; et al. Enhancing healthcare AI stability with edge computing and machine learning for extubation prediction. Scientific Reports. 2025, 15, 17858. [Google Scholar] [CrossRef] [PubMed]
- ElArab, R.A.; Abdulaziz, O.; Sagbakken, M.; Ghannam, A.; Abuadas, F.; Somerville, J.G.; Al Mutair, A. Integrative review of artificial intelligence applications in nursing: education, clinical practice, workload management, and professional perceptions. Frontiers in Public Health. 2025, 13, 1619378. [Google Scholar] [CrossRef]
- Tan, L.; Singi, A.; Cross, A. AI-Driven Innovation For A Sustainable Future: Transforming Healthcare. Metallurgical and Materials Engineering. 2025:1432-9.
- Abulata, N.; Salah, A.A.; Adil, M.; Rasmussen, B.S. GLOBAL PERSPECTIVES ON IMPLEMENTING AI:: Real Stories of Strategies, Challenges and Innovations from Healthcare Experts. 2025.
- Khatal, P.A.; Goukonde, R.; Sanap, G. Artificial intelligence in pharmacy: enhancing efficient data processing and healthcare solutions. World J Pharm Res. 2025, 14, 1486–509. [Google Scholar]
- Khalifa, M.; Albadawy, M. Artificial intelligence for clinical prediction: exploring key domains and essential functions. Computer Methods and Programs in Biomedicine Update. 2024, 5, 100148. [Google Scholar] [CrossRef]
- Akinola, S.; Telukdarie, A. Sustainable digital transformation in healthcare: Advancing a digital vascular health innovation solution. Sustainability. 2023, 15, 10417. [Google Scholar] [CrossRef]
- He, J.; Baxter, S.L.; Xu, J.; Xu, J.; Zhou, X.; Zhang, K. The practical implementation of artificial intelligence technologies in medicine. Nature medicine. 2019, 25, 30–6. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D. Revolutionizing Medical Imaging: The Transformative Role of Artificial Intelligence in Diagnostics and Treatment. MDPI; 2025. p. 1557.
- Annoni, A.; Benczur, P.; Bertoldi, P.; Delipetrev, B.; De Prato, G.; Feijoo, C.; et al. Artificial intelligence: A european perspective. 2018.
- COMTEV; BERTOLINIL; CONSOLIS; LEONIG; ZANCAF; QUERCIM; et al. AI-driven Innovation in Medical Imaging. 2025.
- Hunik, L.; Chaabouni, A.; van Laarhoven, T.; Hartman, T.C.O.; Leijenaar, R.T.; Cals, J.W.; et al. Diagnostic Prediction Models for Primary Care, Based on AI and Electronic Health Records: Systematic Review. JMIR Medical Informatics. 2025, 13, e62862. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.L.; Chen, K.F.; Chen, P.C. Harnessing electronic health records and artificial intelligence for enhanced cardiovascular risk prediction: A comprehensive review. Journal of the American Heart Association. 2025, 14, e036946. [Google Scholar] [CrossRef]
- Rehan, H. Enhancing Early Detection and Management of Chronic Diseases With AI-Driven Predictive Analytics on Healthcare Cloud Platforms. Journal of AI-Assisted Scientific Discovery. 2024, 4, 1–38. [Google Scholar]
- Kataria, S.; Ravindran, V. Harnessing of real-world data and real-world evidence using digital tools: utility and potential models in rheumatology practice. Rheumatology. 2022, 61, 502–13. [Google Scholar] [CrossRef]
- Hu, J.-R.; Power, J.R.; Zannad, F.; Lam, C.S. Artificial intelligence and digital tools for design and execution of cardiovascular clinical trials. European Heart Journal. 2025, 46, 814–26. [Google Scholar] [CrossRef]
- Wang, X. Industry Innovation in the Era of Artificial Intelligence: The AI Compass: CRC Press; 2025.
- Pyone, T.; Smith, H.; Van Den Broek, N. Frameworks to assess health systems governance: a systematic review. Health Policy and Planning. 2017, 32, 710–22. [Google Scholar] [CrossRef]
- Morone, G.; De Angelis, L.; Martino Cinnera, A.; Carbonetti, R.; Bisirri, A.; Ciancarelli, I.; et al. Artificial intelligence in clinical medicine: a state-of-the-art overview of systematic reviews with methodological recommendations for improved reporting. Frontiers in Digital Health. 2025, 7, 1550731. [Google Scholar] [CrossRef]
- Veldhuis, L.I.; Woittiez, N.J.; Nanayakkara, P.W.; Ludikhuize, J. Artificial intelligence for the prediction of in-hospital clinical deterioration: a systematic review. Critical care explorations. 2022, 4, e0744. [Google Scholar] [CrossRef] [PubMed]
- Elhaddad, M.; Hamam, S. AI-driven clinical decision support systems: an ongoing pursuit of potential. Cureus. 2024, 16. [Google Scholar] [CrossRef]
- Wang, Y.; Kung, L.; Byrd, T.A. Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological forecasting and social change. 2018, 126, 3–13. [Google Scholar] [CrossRef]
- Miotto, R.; Wang, F.; Wang, S.; Jiang, X.; Dudley, J.T. Deep learning for healthcare: review, opportunities and challenges. Briefings in bioinformatics. 2018, 19, 1236–46. [Google Scholar] [CrossRef] [PubMed]
- Shortliffe, E.H.; Buchanan, B.G. A model of inexact reasoning in medicine. Mathematical biosciences. 1975, 23, 351–79. [Google Scholar] [CrossRef]
- Mendo, I.R.; Marques, G.; de la Torre Díez, I.; López-Coronado, M.; Martín-Rodríguez, F. Machine learning in medical emergencies: a systematic review and analysis. Journal of Medical Systems. 2021, 45, 88. [Google Scholar] [CrossRef]
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in health and medicine. Nature medicine. 2022, 28, 31–8. [Google Scholar] [CrossRef]
- Obuchowicz, R.; Lasek, J.; Wodziński, M.; Piórkowski, A.; Strzelecki, M.; Nurzynska, K. Artificial intelligence-empowered radiology—current status and critical review. Diagnostics. 2025, 15, 282. [Google Scholar] [CrossRef]
- Daich Varela, M.; Sen, S.; De Guimaraes, T.A.C.; Kabiri, N.; Pontikos, N.; Balaskas, K.; Michaelides, M. Artificial intelligence in retinal disease: clinical application, challenges, and future directions. Graefe's Archive for Clinical and Experimental Ophthalmology. 2023, 261, 3283–97. [Google Scholar] [CrossRef]
- Zhan, Y.; Song, F.; Zhang, W.; Gong, T.; Zhao, S.; Lv, F. Prediction of benign and malignant pulmonary nodules using preoperative CT features: Using PNI-GARS as a predictor. Frontiers in Immunology. 2024, 15, 1446511. [Google Scholar] [CrossRef]
- Rodriguez-Ruiz, A.; Lång, K.; Gubern-Merida, A.; Broeders, M.; Gennaro, G.; Clauser, P.; et al. Stand-alone artificial intelligence for breast cancer detection in mammography: comparison with 101 radiologists. JNCI: Journal of the National Cancer Institute. 2019, 111, 916–22. [Google Scholar] [CrossRef]
- Sun, Y.; Lin, J.; Chen, W. Artificial intelligence in rheumatoid arthritis. Rheumatology & Autoimmunity. 2025.
- Quek, S.X.Z.; Lee, J.W.; Feng, Z.; Soh, M.M.; Tokano, M.; Guan, Y.K.; et al. Comparing artificial intelligence to humans for endoscopic diagnosis of gastric neoplasia: an external validation study. Journal of gastroenterology and hepatology. 2023, 38, 1587–91. [Google Scholar] [CrossRef]
- Galvis-García, E.; Vega-González, F.J.; Emura, F.; Teramoto-Matsubara, Ó.; Sánchez-Robles, J.C.; Rodríguez-Vanegas, G.; Sobrino-Cossío, S. Inteligencia artificial en la colonoscopia de tamizaje y la disminución del error. Cirugía y cirujanos. 2023, 91, 411–21. [Google Scholar] [CrossRef]
- Ikeda, A.; Nosato, H. The Digital Transformation (Dx) of Endoscopic Examinations. Gan to Kagaku ryoho Cancer & Chemotherapy. 2023, 50, 681–5. [Google Scholar]
- Khalaf, K.; Terrin, M.; Jovani, M.; Rizkala, T.; Spadaccini, M.; Pawlak, K.M.; et al. A comprehensive guide to artificial intelligence in endoscopic ultrasound. Journal of Clinical Medicine. 2023, 12, 3757. [Google Scholar] [CrossRef]
- Nazarian, S.; Koo, H.; Carrington, E.; Darzi, A.; Patel, N. The future of endoscopy–what are the thoughts on artificial intelligence? Journal of Experimental & Theoretical Artificial Intelligence. 2024, 36, 1875–84. [Google Scholar]
- Okagawa, Y.; Abe, S.; Yamada, M.; Oda, I.; Saito, Y. Artificial intelligence in endoscopy. Digestive Diseases and Sciences. 2022, 67, 1553–72. [Google Scholar] [CrossRef] [PubMed]
- Visaggi, P.; Barberio, B.; Ghisa, M.; Ribolsi, M.; Savarino, V.; Fassan, M.; et al. Modern diagnosis of early esophageal cancer: from blood biomarkers to advanced endoscopy and artificial intelligence. Cancers. 2021, 13, 3162. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Pante, A.; Gross, S.A. Artificial intelligence in endoscopy. Gastrointestinal Endoscopy. 2020, 91, 925–31. [Google Scholar] [CrossRef]
- Huang, W.; Huang, D.; Ding, Y.; Yu, C.; Wang, L.; Lv, N.; et al. Clinical application of intelligent technologies and integration in medical laboratories. iLABMED. 2023, 1, 82–91. [Google Scholar] [CrossRef]
- Lennerz, J.K.; Salgado, R.; Kim, G.E.; Sirintrapun, S.J.; Thierauf, J.C.; Singh, A.; et al. Diagnostic quality model (DQM): an integrated framework for the assessment of diagnostic quality when using AI/ML. Clinical Chemistry and Laboratory Medicine (CCLM). 2023, 61, 544–57. [Google Scholar] [CrossRef] [PubMed]
- Robertson, A.R.; Segui, S.; Wenzek, H.; Koulaouzidis, A. Artificial intelligence for the detection of polyps or cancer with colon capsule endoscopy. Therapeutic Advances in Gastrointestinal Endoscopy. 2021, 14, 26317745211020277. [Google Scholar] [CrossRef]
- Kim, I.; Kang, K.; Song, Y.; Kim, T.-J. Application of artificial intelligence in pathology: trends and challenges. Diagnostics. 2022, 12, 2794. [Google Scholar] [CrossRef]
- Fu, H.-T.; Tu, H.-Z.; Lee, H.-S.; Lin, Y.E.; Lin, C.-W. Evaluation of an AI-based TB AFB smear screening system for laboratory diagnosis on routine practice. Sensors. 2022, 22, 8497. [Google Scholar] [CrossRef]
- Krause, T.; Jolkver, E.; Bruchhaus, S.; Mc Kevitt, P.; Kramer, M.; Hemmje, M. A preliminary evaluation of “gendai”, an ai-assisted laboratory diagnostics solution for genomic applications. BioMedInformatics. 2022, 2, 332–44. [Google Scholar] [CrossRef]
- Wang, B.; Jing, J.; Huang, X.; Hua, C.; Qin, Q.; Jia, Y.; et al. Establishment of a Knowledge-and-Data-Driven Artificial Intelligence System with Robustness and Interpretability in Laboratory Medicine. Advanced Intelligent Systems. 2022, 4, 2100204. [Google Scholar] [CrossRef]
- Undru, T.R.; Utkarsha, U.; Lakshmi, J.T.; Kaliappan, A.; Mallamgunta, S.; Nikhat, S.S.; et al. Integrating artificial intelligence for clinical and laboratory diagnosis–a review. Maedica. 2022, 17, 420. [Google Scholar]
- Boscardin, C.K.; Gin, B.; Golde, P.B.; Hauer, K.E. ChatGPT and generative artificial intelligence for medical education: potential impact and opportunity. Academic Medicine. 2024, 99, 22–7. [Google Scholar] [CrossRef]
- Nagi, F.; Salih, R.; Alzubaidi, M.; Shah, H.; Alam, T.; Shah, Z.; Househ, M. Applications of artificial intelligence (AI) in medical education: a scoping review. Healthcare Transformation with Informatics and Artificial Intelligence. 2023, 648–51. [Google Scholar]
- Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. Journal of family medicine and primary care. 2019, 8, 2328–31. [Google Scholar]
- Karalis, V.D. The integration of artificial intelligence into clinical practice. Applied Biosciences. 2024, 3, 14–44. [Google Scholar] [CrossRef]
- Luchini, C.; Pea, A.; Scarpa, A. Artificial intelligence in oncology: current applications and future perspectives. British Journal of Cancer. 2022, 126, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Shiwlani, A.; Qayyum, M.U.; Sherani, A.M.K.; Hussain, H.K. AI-powered healthcare revolution: an extensive examination of innovative methods in cancer treatment. BULLET: Jurnal Multidisiplin Ilmu. 2024, 3, 87–98. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).