1. Introduction
Chronic kidney disease (CKD) currently affects more than 10% of the global population, and its prevalence is continuously rising. Several chronic illnesses and conditions can result in end-stage kidney disease (ESKD). Hemodialysis (HD) is the most widespread renal replacement therapy for this condition. As kidney function declines, patients often experience numerous complications, resulting in burdensome symptoms [
1]. Patients with progressive, chronic, non-malignant illnesses, such as ESKD, experience a similar symptom burden to those with advanced cancer who are receiving palliative care (PC) [
2,
3].
Kidney supportive care (KSC) must be applied to all individuals with advanced kidney disease. Like PC in oncology, its primary goal is to reduce suffering throughout the disease, including at the end of life with hospice care. KSC is most effectively delivered through a collaborative approach that involves nephrologists applying “primary PC” skills for the routine assessment and management of symptoms. For complex cases that present a significant and challenging symptom burden, such as severe pain, consultation with PC specialists is recommended. Randomized prospective trials have demonstrated significant improvements in symptom burden, quality of life (QoL), functional status, and reductions in depression and anxiety for individuals receiving PC, compared to those who only receive standard specialty care [
3,
4,
5,
6]. PC programs are most effective in Canada, the United Kingdom, Australia, New Zealand, and Hong Kong [
3]. However, surveys conducted in Australia, New Zealand, and the United Kingdom indicate that more than a third of nephrology units lack dedicated KSC services [
7]. In Australia, 72% of HD patients who could have potentially benefited from PC don’t receive it [
8]. In Hungary, as in several other countries [
9,
10,
11,
12,
13,
14], specialized PC for patients with ESKD is not available.
Research shows that 50% of patients with ESKD who are undergoing HD experience pain [
2,
3,
15]. In December 2023, we conducted a study to evaluate the symptom burden of 168 patients undergoing chronic HD using the Integrated Palliative Care Outcome Scale Renal (IPOS-Renal) questionnaire. The average age of the participants was 65 (±12) years, and the average duration of dialysis treatment was 64 (±55) months. The underlying diseases that caused ESKD were diabetes (DM) (24%), polycystic kidney disease (22%), hypertension (HT) (20%), glomerulonephritis (20%), and other or unknown causes (14%). The Charlson Comorbidity Index, which assesses severe comorbid conditions, had a mean score of 6 (±2), indicating a high level of comorbidity and a 98% ten-year mortality rate. Additionally, responses to the “surprise question” stated a 27% one-year mortality rate. In this patient population, the most significant physical symptom reported was pain, with 52% of patients indicating this issue [
9].
Based on these findings, we initiated a cross-sectional study to explore the incidence and characteristics of pain and the pharmacological treatments utilized by our HD patients. To improve our understanding of the potential factors that trigger pain, we conducted a comparison of clinical data and routine laboratory parameters with the intensity of pain experienced, similar to previous studies [
16,
17,
18,
19,
20,
21,
22]. We aimed to evaluate the potential benefits of providing specialized PC for patients undergoing HD in our country. To achieve this, we studied recent literature on PC for ESKD patients [
10,
11,
12,
13,
14,
23,
24].
2. Materials and Methods
In our study at the National Dialysis Center of Pécs in 2024, we included 159 adult chronic HD patients who had been part of the dialysis program for at least 3 months. Patients who were unable to complete the questionnaire due to their mental state were excluded from the study.
To evaluate patients’ pain experiences, we employ the “PQRST” approach for symptom assessment. „PQRST” stands for Provokes and Palliates, Quality, Region and Radiation, Severity (using the Numeric Rating Scale/NRS/), and Time [
25], along with the negative impact of pain. To better understand the possible factors triggering pain, we compared clinical data and routine laboratory parameters with the intensity of the pain experienced. We compared our results with literature data on patients with ESKD who received palliative care [
8,
13].
Statistical analyses were conducted using SPSS software version 21.0 (SPSS, Inc., Chicago, IL, USA). The data are presented as means with standard deviations (SD) and as percentages. We utilized Student’s t-test and ANOVA, as needed, to compare clinical and laboratory parameters. The average standard deviation was utilized to represent information from a Gaussian distribution. The factors that influence the pain intensity were investigated using univariate and multivariate linear regression analysis. Values of p < 0.05 were considered statistically significant.
3. Results
Table 1 summarizes the baseline clinical data and pain presence in 159 patients with ESKD on HD.
The mean age of the patients was 65 ± 12 years, with 80 (50%) being men. A total of 91 patients (57%) reported experiencing pain.
We conducted a detailed examination of the pain characteristics in these 91 patients. In 36 cases (40%), patients reported pain in several different regions. The characteristics of the pain varied across these areas, which explains why the total percentage of different characteristics can exceed 100%.
Table 2 summarizes the severity of pain in various areas, categorized by the NRS.
The results show that 15 patients (16%) experienced mild pain (NRS 1-3), 39 patients (43%) had moderate pain (NRS 4-6), and 41 patients (45%) reported severe pain (NRS 7-10).
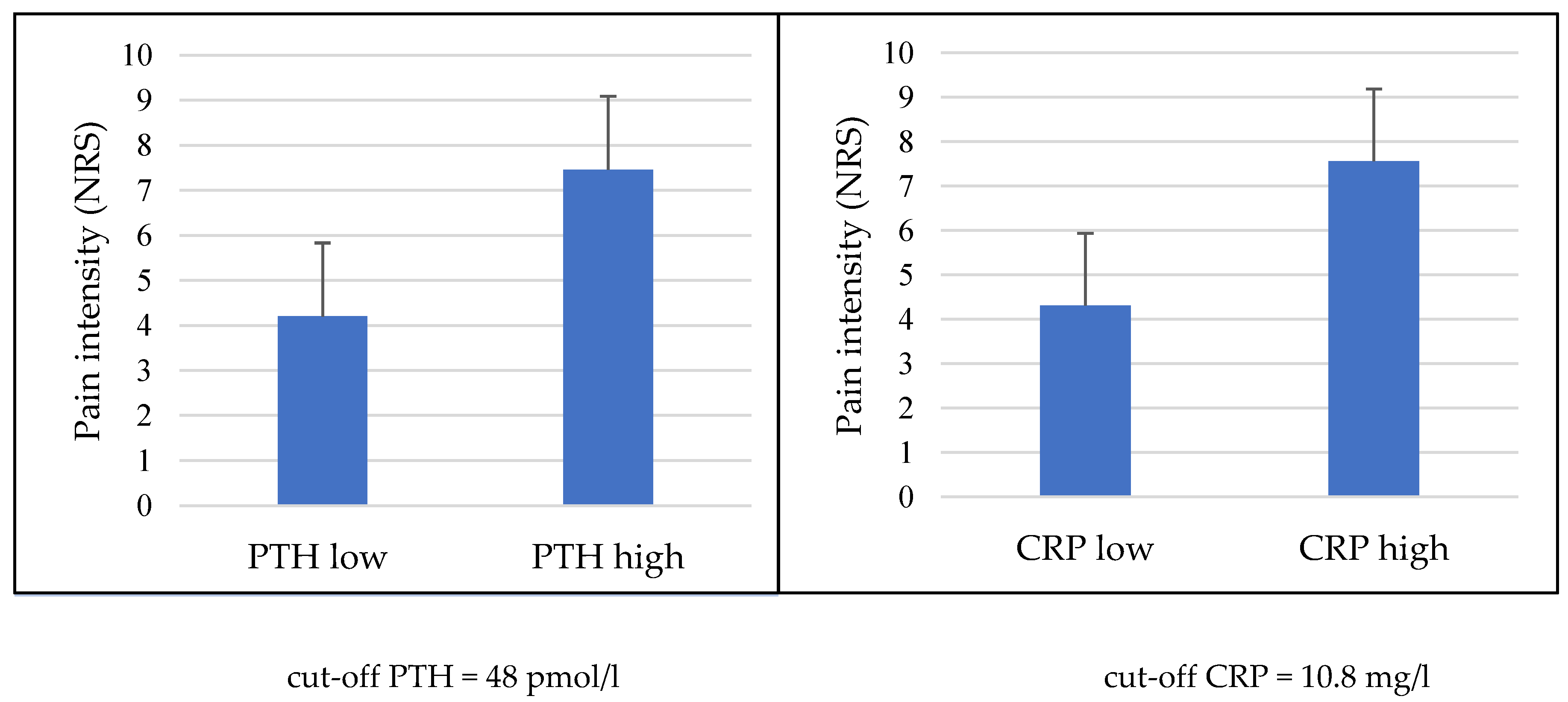
To enhance our understanding of the factors that trigger pain, we compared clinical data and routine laboratory parameters with the intensity of pain experienced. Patients were divided into two groups based on median parathyroid hormone (PTH) and C-reactive protein (CRP), showing a significant difference in pain intensity between individuals with low and high values (cut-off values PTH = 48 pmol/l, CRP = 10.8 mg/l, p < 0.01) (
Figure 1).
The significant confounding factors of intensity of pain were body mass index (BMI) (OR = 2.296, 95% CI: 1.019-2.981, p = 0.012), HT (OR: 7.93; 95% CI: 1.207-14.658, p < 0.05), DM (OR = 7.375; 95% CI: 1.917-13.833, p = 0.013), and PTH (OR = 1.578, 95% CI: 1.089-2.236, p = 0.027) (
Table 3).
The details regarding the location and characteristics of the pain are summarized in
Table 4.
The most common sites of pain were the hip and lower limb, affecting 50 patients (55%), followed by the back, reported by 20 patients (22%), and the shoulder and arm, also reported by 20 patients (22%). Pain localized to the head and neck was experienced by 18 patients (20%). Additionally, 16 patients (18%) reported distal foot pain, 15 patients (16%) reported waist pain, and 10 patients (11%) experienced pain in the gluteal region. Pain in the abdominal area was reported by nine patients (10%), distal hand pain by seven patients (8%), and chest pain by six patients (7%).
In terms of pain characteristics, 28 patients (31%) reported experiencing sharp pain, while 22 patients (24%) reported cramping pain, and another 22 (24%) described aching pain. Additionally, 16 patients (18%) experienced dull pain, 15 patients (16%) reported numbness, 12 patients (13%) experienced stabbing pain, 8 patients (9%) described throbbing pain, and 6 patients (7%) reported burning sensations.
Furthermore, 38 patients (42%) noted that their pain was constant, and 27 patients (30%) described their pain as radiating.
Although our primary objective was not to categorize the pain types, the nature of the reports indicated that nociceptive pain (sharp, cramping, aching, dull, throbbing) was the most prevalent. However, neuropathic pain (numbness, stabbing, burning) also occurred frequently, affecting 36% of the patients.
Seventy-three patients (80%) suffered from chronic pain lasting more than three months, while 63 patients (69%) had experienced pain for over a year. Twelve men and 21 women reported experiencing severe pain for more than a year.
Factors that influence pain and its impact on quality of life are summarized in
Table 5.
Pain increased with movement in 46 cases (51%), while it intensified with rest in 12 patients (13%). Three patients (3%) noted a connection between their pain and HD treatment, three patients (3%) linked it to weather changes, and two patients (2%) associated it with food. Rest reduced pain for 33 patients (36%), and movement alleviated it in 16 patients (18%).
Specifically, 57 patients (63%) reported difficulties with physical activity, 44 patients (48%) had disturbed sleep, worsening their nutritional, physical, and psychological conditions. Fourteen patients (15%) reported loss of appetite, 13 patients (14%) faced emotional challenges, 10 patients (11%) mentioned difficulties with attention, and five patients (5%) experienced relationship issues.
The medications used for pain management and their effectiveness are listed in
Table 6.
A total of fifty-eight patients, representing 64% of those experiencing pain, were using regular medication to manage their pain, sometimes in combination. However, none reported using non-pharmacological methods. Among these 58 patients, 31 (53% of those using medication) were taking non-steroidal anti-inflammatory drugs (NSAIDs), 22 (38%) were using metamizole, three patients (5%) were on paracetamol, and 13 (22%) were using weak opioids such as tramadol. No patients used strong opiates or adjuvant medications.
Of the patients receiving treatment, pain was successfully eliminated for 17 patients, which represents 29%.
4. Discussion
Pain is a common symptom among patients with ESKD. Research shows that 50% of patients undergoing HD experience pain, with over 80% of those reporting moderate to severe pain [
2,
3,
15,
26]. In comparison, the prevalence of pain in patients with advanced metastatic cancer is 55%, but these patients may receive PC [
2,
3,
27].
Our study indicated that 57% of patients reported experiencing pain, and among those, 88% indicated that the severity of their pain was moderate to severe. This aligns with previously published data [
2,
3,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26].
Numerous studies have examined the relationship between pain intensity and both clinical data and laboratory results in patients undergoing HD. Several factors have been associated with the experience of pain in these patients, including: older age [
19], female gender, high comorbidity index, numerous painful sites, dialysis duration exceeding 24 months [
17], increased BMI [
21], presence of diabetic retinopathy and neuropathy, as well as elevated levels of intact PTH [
16,
22], calcium [
16], and CRP [
20], decreased levels of calcitriol [
16], hemoglobin [
18] and serum albumin concentration [
20].
Our study found a significant difference in pain intensity between individuals with low and high levels of PTH and CRP. We also observed a strong correlation between pain intensity and factors such as DM, HT, BMI, and PTH levels.
DM and HT can cause pain through various mechanisms, including nerve damage (neuropathy) and reduced blood flow (ischemic changes) [
28]. Higher BMI may worsen chronic pain by lowering the pain threshold and increasing sensitivity. Additionally, various endocrine changes associated with obesity can affect pain modulation [
21]. CRP serves as an objective measure of inflammatory activity in ESKD, accurately reflecting the production of pro-inflammatory cytokines [
21]. Moreover, increased PTH levels may lead to skeletal pain due to renal osteodystrophy [
22].
The most common source of pain among HD patients is musculoskeletal issues [
26], which are often linked to a high incidence of bone disease, bone fragility, and the progressive loss of muscle mass [
29]. A survey, conducted by Fleishman and colleagues, identified the most common locations of pain as the lower limb and lower back pain. Headaches are a common issue for HD patients [
17], while abdominal pain is prevalent, though its cause remains unclear [
29].
Our study, consistent with existing literature, found that musculoskeletal pain was the most common issue, particularly in the hip and lower limbs. Headaches and abdominal pain were also frequently reported among the patients.
Research indicates that the assessment and treatment of chronic pain in HD patients are often inadequate [
3,
30]. Nephrologists may not be trained to identify and manage pain effectively [
3,
11]. A study by Davison involving patients on HD who experience pain revealed that 35% were not receiving any analgesics. Furthermore, only 6% reported effective pain management [
26].
In our study, consistent with previous research, 36% of patients did not take medication for their pain. Drug treatment successfully eliminated pain in only 29% of patients.
Preliminary studies suggest that therapies targeting pain in the dialyzed population could improve their QoL [
30,
31]. Non-pharmacological analgesic therapies, such as massage, yoga, heat therapy, posture correction, music therapy, acupuncture, breathing exercises, and spiritual coping, can be effective either on their own or in combination with pharmacological treatments [
29,
31,
32,
33,
34,
35,
36]. In patients undergoing HD, complex pain syndromes require a comprehensive analgesic approach that includes a combination of non-opioid medications, opioids, and adjuvant therapies [
37]. According to the World Health Organization (WHO) analgesic ladder [
15], non-opioid medications such as metamizole sodium, paracetamol, and nonsteroidal anti-inflammatory drug (NSAID) should be the primary choice for drug treatments [
38]. Opioids, whether weak or strong, should only be used in dialysis patients for moderate to severe pain that cannot be effectively managed with non-opioid analgesics [
39]. Non-opioid and opioid analgesics effectively treat nociceptive pain. A poor response to paracetamol, NSAIDs, and most opioids characterizes neuropathic pain. According to treatment guidelines for neuropathic pain, the initial approach should involve adjuvant medications [
1].
In contrast to previous research [
32,
34,
35,
36,
38], our study found that patients on HD did not receive any non-pharmacological treatment, effective adjuvant medications for neuropathic pain, or strong opioids for severe nociceptive pain that was resistant to treatment.
Numerous studies highlight the importance of integrated palliative care for patients undergoing HD. They emphasize a holistic approach to palliative care, which recognizes that “total pain” includes physical, psychosocial, and spiritual components. Accurate assessment is crucial for effective pain management, as pain is often underdiagnosed and inadequately treated [
40], as demonstrated by our study. A comprehensive patient history, thorough examination, and assessment tools are essential skills in palliative care pain management [
25]. Palliative care facilitates the multidisciplinary use of non-pharmacological methods, which can help reduce the side effects associated with drug treatments in frail patients with advanced kidney disease [
23], as would have been necessary for our patients. In cases of severe and treatment-resistant pain, a palliative consultation is essential to determine the appropriate medications, as demonstrated by the complete absence of adjuvant agents and strong opioids in our study. For all patients with serious illnesses, including those with advanced kidney disease, it is essential to carefully consider the potential risks and benefits of therapy in the context of each individual’s situation. Close monitoring for adverse effects and careful dose adjustments are standard practices in specialty palliative care [
3]. Despite the importance of palliative care, research shows that its regular availability for patients with ESKD is severely limited in most countries, including Hungary [
7,
9,
14,
41].
5. Conclusions
Pain is a common issue for patients undergoing HD, and the level of pain they experience is comparable to that faced by patients with advanced cancer who may receive PC. In our investigation of factors influencing this symptom burden, we found a significant difference in pain intensity between individuals with low and high levels of PTH and CRP. Additionally, we observed a strong correlation between pain intensity and factors such as DM, HT, BMI, and PTH levels. Palliative care plays a crucial role in alleviating symptoms for patients through comprehensive pain assessments and a multidisciplinary treatment approach. Pain management should be initiated by nephrologists, as their training in PC is crucial. However, in cases of severe and treatment-resistant pain, a palliative consultation is necessary. It highlights the necessity for patients with ESKD to have access to PC.
Author Contributions
All authors (N.Sz., B.Cs., Á.Cs. and B.S.) have made a substantial contribution to the information or material submitted for publication. Specifically, the author contributions are as follows: N.Sz.: writing—original draft preparation, Á. Cs.: writing—review and editing, B.Cs.: methodology, B.S.: validation, data curation. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of the Medical School of Pécs (Reference No. 8825-PTE2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Not applicable.
Acknowledgments
We want to thank Edit Fejes, for her exceptional work on the multivariate statistical analysis.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
BMI, body mass index; CKD, chronic kidney disease; CRP, C-reactive protein; DM, diabetes mellitus; ESKD, end-stage kidney disease; HD, hemodialysis; HT, hypertension; KSC, kidney supportive care; NRS, Numeric Rating Scale; NSAID, non-steroidal anti-inflammatory drug; PC, palliative care; PTH, parathyroid hormone; QoL, quality of life; SD, standard deviation; WHO, World Health Organization.
References
- Kitala-Tańska, K.; Kania-Zimnicka, E; Tański, D; Kwella, N; Stompór, T; Stompór, M. Prevalence and Management of Chronic Pain, Including Neuropathic Pain, in Dialysis Patients with End-Stage Renal Disease. Med. Sci. Monit. 2024, 30, e943808. [Google Scholar] [CrossRef]
- Davison, S.N; Jhangri, G.S. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J. Pain Symptom Manage. 2010, 39, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Gelfand, S.L.; Scherer, J.S.; Koncicki, H.M. Kidney Supportive Care: Core Curriculum 2020. Am. J. Kidney Dis. 2020, 75, 793–806. [Google Scholar] [CrossRef]
- Litjens, E.J.R.; Dani, M.; Verberne, W.R.; Van Den Noortgate, N.J.; Joosten, H.M.H.; Brys, A.D.H. Geriatric Assessment in Older Patients with Advanced Kidney Disease: A Key to Personalized Care and Shared Decision-Making—A Narrative Review. J. Clin. Med. 2025, 14, 1749. [Google Scholar] [CrossRef]
- Martino, F.K.; Novara, G.; Nalesso, F.; Calò, L.A. Conservative Management in End-Stage Kidney Disease between the Dialysis Myth and Neglected Evidence-Based Medicine. J. Clin. Med. 2024, 13, 41. [Google Scholar] [CrossRef]
- Lanini, I.; Samoni, S.; Husain-Syed, F.; Fabbri, S.; Canzani, F.; Messeri, A.; Mediati, R.D.; Ricci, Z.; Romagnoli, S.; Villa, G. Palliative Care for Patients with Kidney Disease. J. Clin. Med. 2022, 11, 3923. [Google Scholar] [CrossRef]
- Marsh, S.; Varghese, A.; Snead, C.M.; Hole, B.D.; O’Hara, D.V.; Agarwal, N.; Stallworthy, E.; Caskey, F.J.; Smyth, B.J.; Ducharlet, K. A Multinational, Multicenter Study Mapping Models of Kidney Supportive Care Practice. Kidney Int. Rep. 2024, 9, 2198–2208. [Google Scholar] [CrossRef]
- Cooper, A.L.; Panizza, N.; Bartlett, R.; Martin-Robins, D.; Brown, J.A. A period prevalence study of palliative care need and provision in adult patients attending hospital-based dialysis units. J. Nephrol. 2025, 38, 687–695. [Google Scholar] [CrossRef]
- Szigeti, N.; Tóth, S.; Kun, Sz.; Ladányi, E.; Csiky, B.; Wittmann, I. A dializált betegek palliatív ellátása = Palliative care of patients treated by dialysis. HYPERTONIA ÉS NEPHROLOGIA 2024, 28, 187–189. [Google Scholar]
- ALHosni, F.; Al Qadire, M.; Omari, O.A.; Al Raqaishi, H.; Khalaf, A. Symptom prevalence, severity, distress and management among patients with chronic diseases. BMC Nurs. 2023, 22, 155. [Google Scholar] [CrossRef]
- Bursic, A.E.; Schell, J.O. Hospice Care in Conservative Kidney Management. Semin. Nephrol. 2023, 43, 151398. [Google Scholar] [CrossRef]
- Vahlkamp, A.; Schneider, J.; Markossian, T.; Balbale, S.; Ray, C.; Stroupe, K.; Limaye, S. Nephrology-Palliative Care Collaboration to Promote Outpatient Hemodialysis Goals of Care Conversations. Fed. Pract. 2023, 40, 349–351a. [Google Scholar] [CrossRef]
- Darawad, M.W.; Reink, L.F.; Khalil, A.; Melhem, G.B.; Alnajar, M. Palliative Care for Patients With End-Stage Renal Disease: An Examination of Unmet Needs and Experiencing Problems. J. Hosp. Palliat. Nurs. 2025, 27, E107–E117. [Google Scholar] [CrossRef] [PubMed]
- Chu, W.M.; Tsai, H.B.; Chen, Y.C.; Hung, K.Y.; Cheng, S.Y.; Lin, C.P. Palliative Care for Adult Patients Undergoing Hemodialysis in Asia: Challenges and Opportunities. J. Hosp. Palliat. Care 2024, 27, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.H.; Holley, J.L.; Davison, S.N.; Dart, R.A.; Germain, M.J.; Cohen, L.; Swartz, R.D. Palliative care. Am. J. Kidney Dis. 2004, 43, 172–173. [Google Scholar] [CrossRef] [PubMed]
- Golan, E.; Haggiag, I.; Os, P.; Bernheim, J. Calcium, parathyroid hormone, and vitamin D: major determinants of chronic pain in hemodialysis patients. Clin. J. Am. Soc.Nephrol. 2009, 4, 1374–1380. [Google Scholar] [CrossRef]
- Fleishman, T.T.; Dreiher, J.; Shvartzman, P. Pain in Maintenance Hemodialysis Patients: A Multicenter Study. J. Pain Symptom Manage. 2018, 56, 78–184. [Google Scholar] [CrossRef]
- Plantinga, L.C.; Fink, N.E.; Jaar, B.G.; Huang, I.C.; Wu, A.W.; Meyer, K.B.; Powe, N, R. Relation between level or change of hemoglobin and generic and disease-specific quality of life measures in hemodialysis. Qual. Life Res. 2007, 16, 755–765. [Google Scholar] [CrossRef]
- Bouattar, T.; Skalli, Z.; Rhou, H.; Ezzaitouni, F.; Ouzeddoun, N.; Bayahia, R.; Benamar, L. Evaluation et analyse de la douleur chez les hémodialysés chroniques [The evaluation and analysis of chronic pain in chronic hemodialysis patients]. Nephrol. Ther. 2009, 5, 637–641. [Google Scholar] [CrossRef]
- Mizher, A.; Hammoudi, H.; Hamed, F.; Sholi, A.; AbuTaha, A.; Abdalla, M.A.; Jabe, M.M.; Hassan, M.; Koni, A.A.; Zyoud, S.H. Prevalence of chronic pain in hemodialysis patients and its correlation with C-reactive protein: a cross-sectional study. Sci. Rep. 2023, 13, 5293. [Google Scholar] [CrossRef]
- Marzouq, M.K.; Samoudi, A.F.; Samara, A.; Zyoud, S.H.; Al-Jabi, S.W. Exploring factors associated with pain in hemodialysis patients: a multicenter cross-sectional study from Palestine. BMC Nephrol. 2021, 22, 96. [Google Scholar] [CrossRef]
- Elsurer, R.; Afsar, B.; Mercanoglu, E. Bone pain assessment and relationship with parathyroid hormone and health-related quality of life in hemodialysis. Ren. Fail. 2013, 35, 667–672. [Google Scholar] [CrossRef]
- Raina, R.; Krishnappa, V.; Gupta, M. Management of pain in end-stage renal disease patients: Short review. Hemodial. Int. 2018, 22, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.M.; Mohamed, I.A.; Shahin, M.A.; Abd-El Hady, T.R.M.; Abdelhalim, E.H.N.; Zaghami, D.E.F.; Anwr Akl, D.B.; Ghazy Mohammed, L.Z.; Moustafa Ahmed, F.A. Evaluating palliative care’s role in symptom management for CKD patients in Egypt: A quasi-experimental approach. Palliat. Support. Care. 2025, 23, e33. [Google Scholar] [CrossRef]
- Barnard, A.; Gwyther, E. Pain management in palliative care. South African Family Practice 2006, 48, 30–33. [Google Scholar] [CrossRef]
- Davison, S.N. Pain in hemodialysis patients: prevalence, cause, severity, and management. Am. J. Kidney Dis. 2003, 42, 1239–1247. [Google Scholar] [CrossRef]
- Snijders, R.A.H.; Brom, L.; Theunissen, M.; van den Beuken-van Everdingen, M.H.J. Update on Prevalence of Pain in Patients with Cancer 2022: A Systematic Literature Review and Meta-Analysis. Cancers 2023, 15, 591. [Google Scholar] [CrossRef]
- Santoro, D.; Satta, E.; Messina, S.; Costantino, G.; Savica, V.; Bellinghieri, G. Pain in end-stage renal disease: a frequent and neglected clinical problem. Clin. Nephrol. 2013, 79 (Suppl. S1), S2–S11. [Google Scholar] [PubMed]
- Dos Santos, P.R.; Mendonça, C.R.; Hernandes, J.; Borges, C.C.; Barbosa, M.A.; Romeiro, A.M.S.; Alves, P.M.; Dias, N.T.; Porto, C.C. Pain in Patients With Chronic Kidney Disease Undergoing Hemodialysis: A Systematic Review. Pain Manag. Nurs. 2021, 22, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S. Treating pain to improve quality of life in end-stage renal disease. Semin. Dial. 2013, 26, 268–273. [Google Scholar] [CrossRef]
- Belayev, L.Y.; Mor, M.K.; Sevick, M.A.; Shields, A.M.; Rollman, B.L.; Palevsky, P.M.; Arnold, R.M.; Fine, M.J.; Weisbord, S.D. Longitudinal associations of depressive symptoms and pain with quality of life in patients receiving chronic hemodialysis. Hemodial. Int. 2015, 19, 216–224. [Google Scholar] [CrossRef]
- Yan, C.; Liu, H.R.; Kong, Q.; Gan, J.Y.; Liu, K.; Yao, W.G.; Yao, X.M. Effect of Acupuncture Intervention on Chronic Musculoskeletal Pain in Hemodialysis-Dependent Kidney Failure Patients: Study Protocol for a Randomized Controlled Clinical Trial. J. Pain Res. 2024, 17, 4289–4300. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.; Parola, V.; Cardoso, D.; Bravo, M.E.; Apóstolo, J. Use of non-pharmacological interventions for comforting patients in palliative care: a scoping review. JBI Database System. Rev. Implement. Rep. 2017, 15, 1867–1904. [Google Scholar] [CrossRef]
- Klassen, A.; Di Iorio, B.; Guastaferro, P.; Bahner, U.; Heidland, A.; De Santo, N. High-tone external muscle stimulation in end-stage renal disease: effects on symptomatic diabetic and uremic peripheral neuropathy. J. Ren. Nutr. 2008, 18, 46–51. [Google Scholar] [CrossRef]
- Güvener, Y.Ö.; Koç, Z. The effect of breathing exercises on pain, sleep, and symptom management in patients undergoing hemodialysis: a randomized controlled trial. Sleep Breath 2025, 29, 170. [Google Scholar] [CrossRef]
- KauricKlein, Z. Effect of yoga on physical and psychological outcomes in patients on chronic hemodialysis. Complement. Ther. Clin. Pract. 2019, 34, 41–45. [Google Scholar] [CrossRef]
- Raina, R.; Krishnappa, V.; Gupta, M. Management of pain in end-stage renal disease patients: Short review. Hemodial. Int. 2018, 22, 290–296. [Google Scholar] [CrossRef]
- Davison, S.N.; Rathwell, S.; George, C.; Hussain, S.T.; Grundy, K.; Dennett, L. Analgesic Use in Patients With Advanced Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Can. J. Kidney Health Dis. 2020, 7, 2054358120910329. [Google Scholar] [CrossRef] [PubMed]
- Kalim, S.; Lyons, K.S.; Nigwekar, S.U. Opioids in Hemodialysis Patients. Semin. Nephrol. 2021, 41, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Kliuk-Ben Bassat, O.; Brill, S.; Sharon, H. Chronic pain is underestimated and undertreated in dialysis patients: A retrospective case study. Hemodial. Int. 2019, 23, E104–E105. [Google Scholar] [CrossRef]
- Liem, Y.S.; Eidemak, I.; Larsen, S.; Sjøgren, P.; Molsted, S.; Sørensen, J.; Laursen, L.; Kurita., G.P. Identification of palliative care needs in hemodialysis patients: An update. Palliat. Support. Care 2022, 20, 505–511. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).