1. Introduction
Elbow dislocation is the second most common major joint dislocation in adults, following the shoulder [
1]. Such injuries frequently involve not only ligament damage but also associated fractures. If these fractures are not accurately diagnosed and managed, they can lead to significant long-term complications. In many cases, loose bone fragments within the joint make simple closed reduction unfeasible. Elbow dislocations that remain unreduced for longer than three to six weeks are referred to as neglected elbow dislocations [
2].
In the specialized literature, neglected elbow dislocations are reported to be followed by severe functional complications, such as joint stiffness, often requiring open surgical procedures to restore function.[
2,
3,
8,
24].
Treatment can be particularly difficult due to factors such as severe soft tissue contractures, ligament instability, fibrosis, potential nerve involvement, myositis ossificans, non-compliant patients, and the requirement for prolonged postoperative physiotherapy. The primary aim of surgical intervention is to restore a pain-free, stable, and mobile elbow with proper joint congruency.
In the present case, the patient presented with a complex injury: a Terrible Triad, consisting of a severe elbow dislocation associated with fractures of the radial head and coronoid process. The patient experienced pain and elbow deformity in extension, accompanied by a severely restricted range of motion that significantly affected daily activities. Repeated attempts to mobilize the dislocated elbow led to joint stiffness and heterotopic ossification. Management of such cases is challenging due to the high risk of complications, including neurovascular injury, and the unpredictable course of functional recovery.
Elbow dislocations are categorized according to the direction in which the ulna is displaced relative to the humerus. The main types include posterior dislocations, (further divided into posterolateral and posteromedial subtypes), as well as anterior, medial, and lateral dislocations. Among these, posterior dislocations are by far the most common, accounting for approximately 90% of all cases[
4]. This type of injury typically occurs following a fall onto an outstretched hand which generates a posteriorly directed force. They can be simple, or complex if associate concomitant fractures (of radial, or coronoid process), or ligaments ruptures. This mechanism of injury was consistent with the case of the patient presented here.
When such a fall occurs, the valgus stress on the elbow joint causes initial damage to the medial collateral ligament, which is usually the first structure to fail under the load [
5]. As the injury progresses, the lateral collateral ligament complex may also be compromised, further destabilizing the joint. The combination of valgus stress and hyperextension leads to a progressive displacement of the proximal radius and ulna in a lateral and posterior direction.
During this process, a hyperextension force acts on the elbow, which causes the coronoid process of the ulna to become dislodged from its articulation with the humerus. This often occurs in conjunction with an avulsion of a bone fragment from the coronoid. (this case is described as terrible triad: elbow dislocation, radial head fracture and coronoid fracture). Additionally, the anterior soft tissue structures, such as the joint capsule and associated musculature, undergo tearing or disruption, further contributing to the instability. As a result of these combined forces and injuries, the elbow typically dislocates posteriorly or posterolaterally, depending on the specific direction and magnitude of the applied forces [
5].
During the traumatic event, the radial head frequently impacts the capitulum of the humerus, leading to a fracture of the radial head. In many cases, this fracture results in intra-articular displacement of bone fragments [
6]. The presence of these loose fragments within the joint space often obstructs attempts at closed reduction, making realignment of the dislocation impossible without surgical intervention. In the case presented, the dislocation was not surgically addressed in the acute phase, and the joint was not opened for fragment removal or anatomical reduction.
As a result, the surrounding soft tissues, particularly the joint capsule, ligaments, and periarticular muscles, underwent progressive contracture over time, contributing significantly to joint stiffness [
2,
3]. This was further exacerbated by prolonged immobilization in a cast, which limited joint mobility and promoted fibrotic changes in periarticular structures.
When the patient eventually began rehabilitation, the elbow was still dislocated and already compromised by soft tissue contracture. At this stage, residual bone and cartilage fragments inside the joint, along with ongoing local inflammation, acted as key pathological stimuli for the development of heterotopic ossification and myositis ossificans. These abnormal bone formations within soft tissues led to additional limitations in range of motion and increased pain, making subsequent management more challenging.
2. Patient Information
The patient was a 67-year-old right-handed male with no significant medical or surgical history, except for mild, well-controlled hypertension. He had not undergone any previous surgical interventions. His main concerns at presentation were persistent pain, elbow deformity, and severe stiffness that had progressively developed over six months following the initial trauma. These symptoms caused major functional limitations in daily activities, particularly in flexion-extension and pronation-supination of the forearm. No relevant family or genetic history was identified.
3. Clinical Findings
On clinical examination, the patient’s elbow appeared visibly deformed and stiff. The anterior aspect of the distal humerus was prominently palpable, and the olecranon was abnormally projected posteriorly. A significant retraction and shortening of the biceps muscle was also noted, likely secondary to prolonged disuse and altered joint biomechanics. The elbow was fixed in a semi-flexed position between 45 and 50 degrees, with only minimal passive movement possible (5 degrees). Active range of motion was almost entirely absent, and any attempt to move the joint elicited pain. Importantly, both forearm rotation movements, pronation and supination, were completely absent. Despite the functional impairment, there were no clinical signs of distal neurovascular deficit; peripheral pulses were intact, capillary refill was normal, and motor and sensory testing of the radial, median, and ulnar nerves revealed no abnormalities (
Figure 1).
4. Timeline
The timeline below outlines the sequence of clinical events, diagnostic assessments, surgical interventions, and follow-up milestones for this case (
Table 1).
5. Diagnostic Assesment
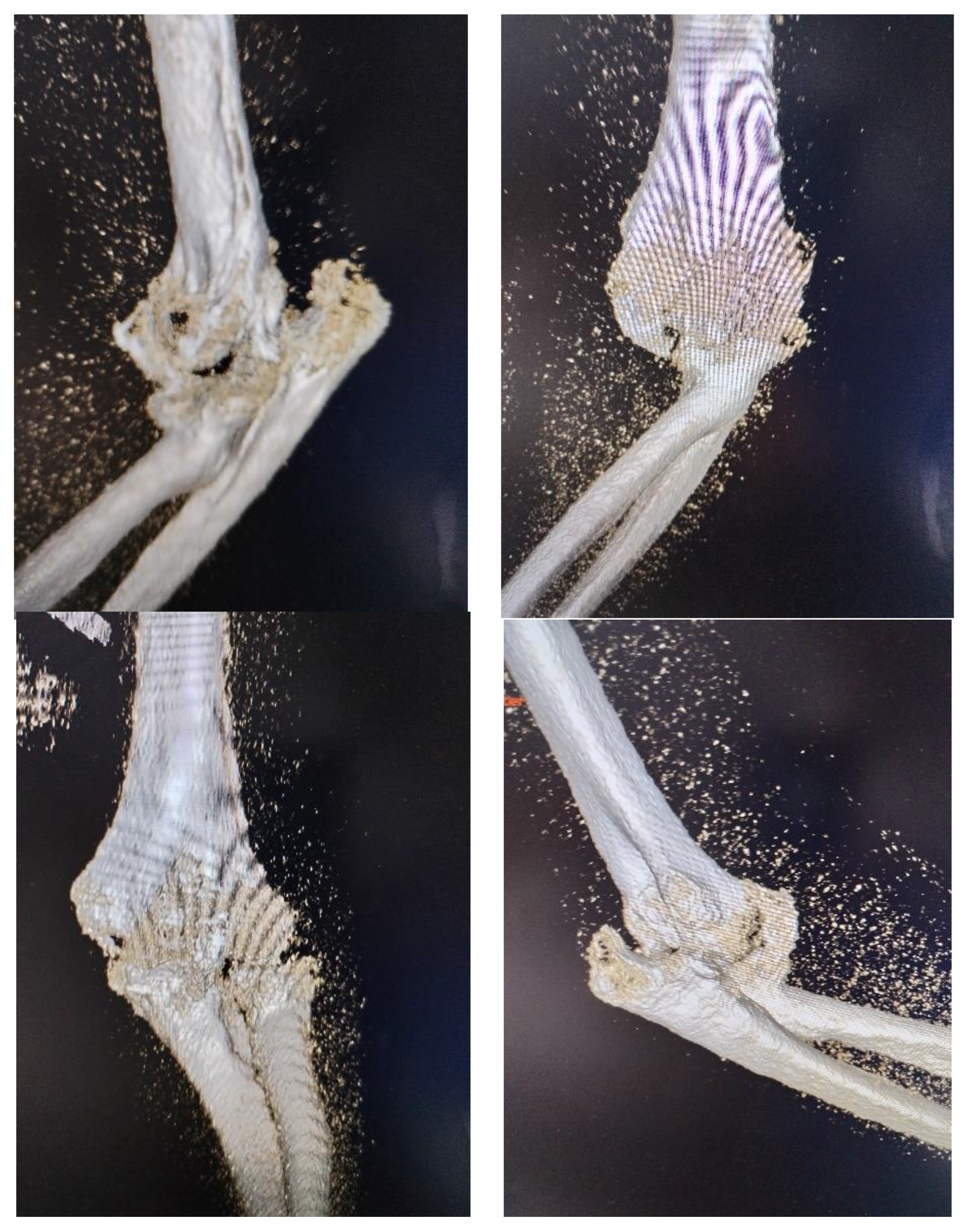
At the time of injury, the diagnosis of posterior elbow dislocation with associated fractures was not fully recognized. The patient underwent closed reduction and cast immobilization, but we did not have access to the initial radiographs taken immediately after the trauma and following the first reduction. The radiographs presented at the time of admission to our clinic were inconclusive due to heterotopic ossification, so a 3D computed tomography (CT) scan was requested to provide a more accurate depiction of the bony anatomy and the relative position of the joint structures (
Figure 2). The CT scan revealed a chronic posterior dislocation of the elbow, accompanied by a large heterotopic bony mass within the joint space. The coronoid process of the ulna was no longer identifiable, suggesting it had been either resorbed or fragmented at the time of injury. Additionally, the radial head was found to be severely deformed (Masson 3), impeding normal articulation with the capitulum and rendering the proximal radioulnar joint functionally blocked.
To exclude any potential nerve entrapment or structural lesion, magnetic resonance imaging (MRI) was performed. The MRI confirmed the absence of nerve damage, further supporting the clinical finding of intact neurovascular status. No additional imaging or laboratory investigations were deemed necessary at this stage, as the diagnosis and surgical planning could proceed based on the existing radiologic and clinical findings.
To objectively quantify the patient’s baseline functional status and to facilitate postoperative outcome monitoring, the Mayo Elbow Performance Index (MEPI) was applied (
Table 2). This scoring system assesses four key parameters: pain, range of motion, stability, and daily function. The patient’s preoperative Mayo Elbow Performance Index (MEPI) score was 25, which is considered very poor and indicative of severe functional impairment. This low score reflected intense pain, a minimal range of motion, joint instability, and significant limitations in performing activities of daily living. The MEPI evaluation confirmed the need for surgical intervention aimed at restoring joint alignment, relieving pain, and improving overall elbow function.
6. Therapeutic Intervention
The treatment of neglected posterior dislocation of elbow is quite challenging especially in this case, due to the significant soft tissue contractures, heterotopic ossification, ligamentous insufficiencies and fibrosis, bone fractures, capsular lesion, and the need for long-term postoperative physiotherapy [
7]. All associated with frustration of patient who had pain. The goal of surgical treatment was to achieve a painless, stable and mobile elbow with a congruent joint space.
Closed reduction was impossible from the beginning because bone mass formation and deformation of radial head. Besides that, were capsular retraction with elbow dislocated. Open reduction was normally required to treat this condition.
Many authors described variants of elbow approaches, like single posterior approach [
8,
9], or two incision approach [
10]. Every aproach has his advantages and disadvantages. Posterior aproach offeres a very excellent exposure of the joint and contracted soft tissues allowing joint manipulation and reduction under direct vision. If it is necessary, an ostheosynthesis of radial head, or artroplasty of radial head is performed. It is advised to maintain reduction by transfixing the olecranon to the humerus with one or two small smooth pins with the elbow at 90° of flexion for approximately 14 days, to allow soft tissue healing followed by vigorous but protected physical therapy [
11]. When is avalable, a hinged external fixator is a better option [
12].
In old neglected dislocation, triceps contracture can make surgical intervention very dificult [
11,
13]. Tricepsplasty should be performed when contracture of the muscle makes reduction of the elbow impossible. It should be carried out by midline posterior incision with medial and lateral approach in the deeper planes [
14]. Disadvantage of this procedure is potential instability of the joint.
The two incision approach protect the triceps insertion with better functional results as compared to posterior approach [
15]. Lateral approach provides better exposure of the humeroradial joint and the anterior coronoid fossa. Medial approach provides exposure of the posteromedial capsule for extraperiosteal dissection. The major disadvantages is the difficulty to do tricepsplasty without a midline posterior incision. The advantages of retaining the triceps muscle integrity are less postoperative pain, improved joint stability, improved range of motion and early successful rehabilitation [
16].
For our case we chose the two incision approach. The reason was to provide as much joint stability as possible. The patient had general anesthesia and were positioned in dorsal decubitus with the affected arm placed on the chest. This position allows exposure to the both side of elbow, medial and lateral. Tourniquet was applied on the proximal arm. On medial side was identified the ulnar nerve, who was then protected throughout surgical intervention. Its separation from the fibrous and bony tissue mass was difficult, requiring extra care to avoid intraoperative injury. Combined lateral and medial approach offered access to remove the big anterior ossification (
Figure 3) and to clean posterior compartment. At the same time, the triceps insertion was preserved, which provided greater postoperative joint stability.
After all soft tissue was released from the bone (with exception of triceps insertion) and articular surface was free of any adhesions, anterior capsule was attached to the coracoid bone with two anchors, preventing posterior dislocation. The common extensors of the forearm were detached from the distal humerus, as they were retracted and obstructing both the visualization and removal of the intra-articular ossification.
The collateral ligaments were detached because of the degree of contracture and this aided joint motion. The detached ligaments were not reconstructed at the end of procedure, but reattached to the adjoining fibrous tissues to avoid excessive tension. The damaged radial head was removed and for supplementary stabilization an arthroplasty of radial head was performed. Usually we prefer osteosynthesis, but in this chronic case, the radial head was damaged and block the movement. After arthroplasty, pronation and supination was verified.
During manipulation of elbow, a small fragment of olecranon was displaced being stabilized with a screw. The elbow range of motion was about 100-120 degrees. The full extension could not be gained because of the contracture of biceps and brahial muscles. Pronation and supination were assessed with the elbow flexed at 90 degrees. They were complete.
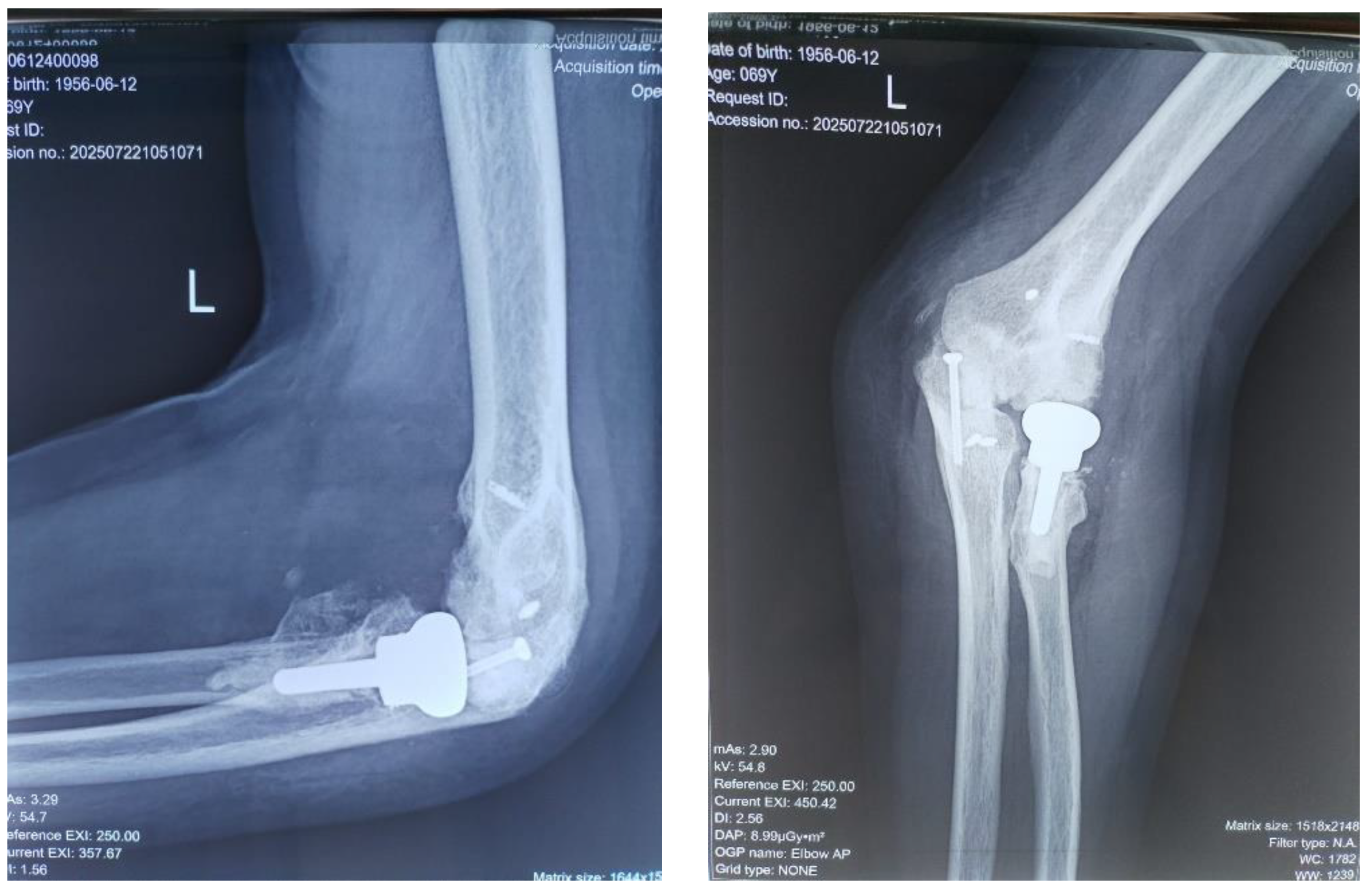
The common extensors were attached with anchors and ulnar nerve anterior transposition was made at the end of procedure. Soft tissue was sutured with elbow at 90 degrees and with radius in pronation to use as stabilizer prosthetical head. Then postoperative X-ray was taken to evaluate the elbow joint alignment (
Figure 4). The wound was closed in a standard manner over a suction drain to prevent the accumulation of a subcutaneous hematoma.
After surgery, a posterior splint with elbow at 90 degrees in neutral position offered for 2-3 weeks comfort until swelling of soft tissue disappears [
17]. Both intraoperatively and postoperatively, antibiotics were administered to prevent an associated infection. Locally, ice was applied for several days to reduce inflammation.
7. Folow-Up and Outcome
It is known that surgery is only a half of the way in elbow injuries treatment. Active finger movements and limb elevation is started postoperatively. Even the arm was immobilized, the splint was removed every day, beginning with the first day after surgery and guided flexion-extensions and prono-supination were performed to maintain elbow mobility. In many cases, after patient wakes up from anesthesia, because of pain and reflex muscles contracture, some degrees of mobilities are lost. For this reason, early mobilization (gentle, controlled, passive/active range of motion, exercises) is essential to achieve good results.
After 3 weeks the splint was removed definitively being replaced with a sling. At six weeks after the surgery, when soft tissue healing has occurred and a functional range of movements achieved, patient started more aggressive program of rehabilitation.
Theoretically, the posterior splint could be worn at night for 3 months to prevent recurrence of dislocation. Post-operative rehabilitation may need to be continued for long time for optimum results. Our patient, unfortunately, after first two-three months of intense rehabilitation, because some family problems, was obligated to interrupt the rehabilitation program and lost some degrees of the extension.
Heterotrophic ossification is a common postoperative complication which is preventable by Indomethacin prophylaxis (25mgx3/day for 6 weeks with gastric protection), cold packs and monitored physiotherapy [
17]. Other complications such as wound infection, early osteoarthritis and neurological injury are rare on using a sterile, gentle and meticulous surgical technique which includes thorough release of the ulnar nerve [
18].
At two weeks the sutures were removed. The following follow-ups took place at 6 weeks, then three months after surgery, and the last at 18 months later, on which occasion MEPI score was evaluated when patient obtained 95 (
Table 2). At 4-6 weeks after surgery, gradually, the passive motion was replaced by active motion. No wound infection, or ulnar nerve deficit were noted. Follow-up imaging at 18 months postoperatively included plain radiographs, which confirmed maintained reduction, proper positioning of the radial head prosthesis, and no recurrence of heterotopic ossification. (
Figure 5).
Functional elbow motion typically requires a flexion-extension arc of 75–120° and about 50° of pronation-supination, which is generally sufficient for daily activities. [
19].
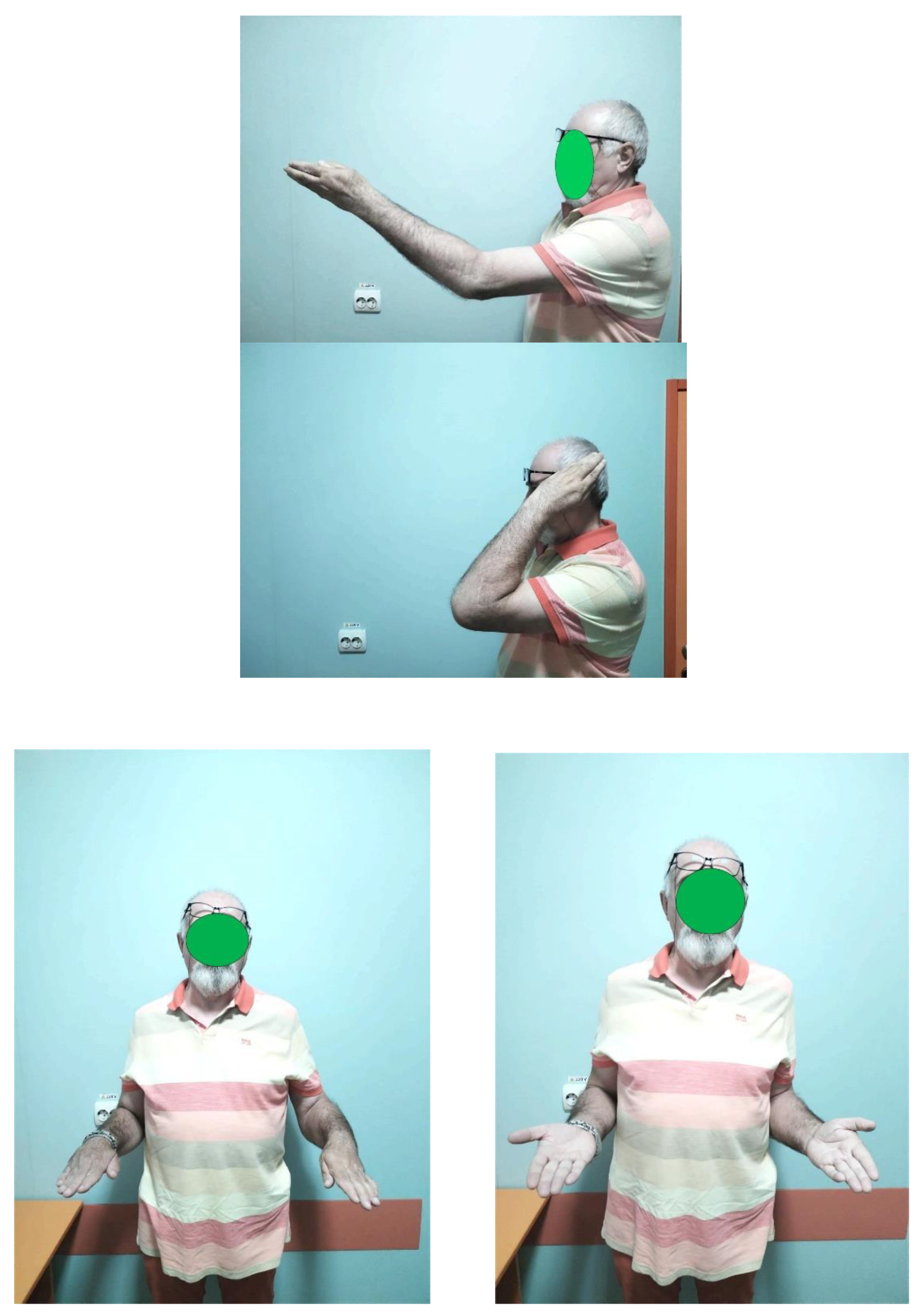
Our patient presented stable, nonpainful joint with an range of motion (flexion-extension) of 75° in the morning, with an increases of up to the 80° during the day. It is known that after wake up from anesthesia, because of pain and muscular contracture, some of degrees of motion are lost, for this reason, rehabilitation must begin early, most recovery happening between 6 weeks and 3 months after surgery [
20]. Although the patient was unable to follow the full prescribed rehabilitation plan due to family reasons, at 18 months post-surgery he has pain-free joint, a flexion-extension arc of 80°, and pronation and supination are nearly normal, allowing him to carry out daily activities and work (pronation was 80
° and supination 75°). This mobility and stability of the joint allows him to do current activities as washing of the face, shaving, dressing, combing hair, working. The strength of fore arm was quite good, patient being able to carry a few kg without problems (maximum was 12 kg) (
Figure 6). No adverse or unanticipated events occurred during the follow-up period. The patient did not experience infection, neurovascular complications, prosthesis loosening, or additional fractures.
8. Discussion
This case illustrates the complexity of managing neglected posterior elbow dislocations with associated fractures and heterotopic ossification. A key strength of our approach was the use of a two-incision surgical technique combined with radial head arthroplasty and meticulous excision of heterotopic bone, which allowed us to restore joint stability and function. Limitations included the lack of initial radiographs and delayed presentation, which increased the technical difficulty and limited the achievable range of motion.
The literature confirms that neglected elbow dislocations are challenging due to soft tissue contractures, ossification, and joint instability[
21,
22]. Early diagnosis and intervention are crucial to prevent irreversible stiffness and functional impairment. Previous studies have highlighted that open reduction, removal of ossifications, and, when necessary, radial head arthroplasty can provide acceptable outcomes even in chronic cases [
23,
24,
25,
26,
27,
28,
29,
30]. Our management was guided by these principles, prioritizing preservation of joint stability and early postoperative mobilization.
The rationale for our conclusions is based on the observed postoperative results: at 18 months follow-up, the patient achieved a stable, pain-free elbow with functional motion, confirming that timely, carefully planned surgical intervention can restore function even in complex neglected dislocations.
A key take-away from this case is that early recognition and referral of complex elbow dislocations to specialized centers can prevent severe functional complications.
9. Patient Perspective
The patient expressed satisfaction with the outcome of the treatment. He reported significant improvement in pain, mobility, and the ability to perform daily activities compared to the preoperative state. Although the rehabilitation process required dedication and regular exercises, he appreciated the gradual recovery of elbow function. The patient also emphasized the importance of being treated in a specialized center with experienced surgeons, which he believes contributed to the positive result.
10. Informe Consent
Written informed consent was obtained from the patient for publication of this case report, including all images and clinical data. The patient was informed about the purpose of the publication, the use of anonymized data, and the possibility of dissemination in scientific literature. A copy of the consent form has already been submitted to the journal.
Author Contributions
Conceptualization, M.T.G. and V.C.; methodology, M.T.G.; validation, .; formal analysis, V.C.; investigation, M.T.G.; resources, M.T.G.; data curation, V.C.; writing— original draft preparation, M.T.G.; writing—review and editing, M.T.G.; visualization, M.T.G..; supervision, C.S, . All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
the data presented in this study are available in references [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30].
Conflicts of Interest
The authors declare no conflicts of interest
References
- Franziska Lioba Breulmann, Sebastian Lappen, Yannick Ehmann, Martin Bischofreiter, Lucca Lacheta & Sebastian Siebenlist, Treatment strategies for simple elbow dislocation - a systematic review, 2024, BMC Musculoskeletal Disorders volume 25, Article number: 148. [CrossRef]
- Kouamé Jean-Eric Kouassi, Koffi Leopold Krah, Loukou Blaise Yao, Bada Justin Leopold Niaoré Sery, Kouamé Innocent Mbra and Michel Kodo, Surgical management of neglected elbow dislocations: A systematic review, 2025, International Journal of Orthopaedics Sciences 2025; 11(1): 219-224. [CrossRef]
- M’Bra Kouamé Innocent, Kouassi Kouamé Jean-Eric, Yao Loukou Blaise, AkobéJean Regis Achie, Sery Bada Justin Léopold, KouassiAya Adélaïde Natacha, Krah Koffi Leopold, Michel Kodo, Treatment of Neglected Elbow Dislocations by Z-Lengthening of the Triceps Brachii, 2022, Open Journal of Orthopedics > Vol.12 No.4. [CrossRef]
- Rokwood and Greeen’s Fractures in Adjults fith Edition, 2001, vol 1.
- O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow, 1991, J Bone Joint Surg; 73A:440-446.
- Jagwant Singh, Michael H. Elvey, Zaid Hamoodi, Adam C. Watts, Current perspectives on elbow dislocation and instability, 2021, AOJ vol 6. [CrossRef]
- Anna E. van der Windt MD, PhD , Joost W. Colaris MD, PhD , Dennis den Hartog MD, PhD , BertramThe MD, PhD , Denise Eygendaal MD, PhD, Persistent elbow dislocation, 2023, JSES International Volume 7, Issue 6, November, Pages 2605-2611.
- Md. Nazrul Islam, Md. Rabiul Islam, Tahmina Begum, Md. Moshabbirul Islam, Surgical Treatment of Neglected Elbow Dislocation by Posterior Approach, 2022, Journal of Current and Advance Medical Research July, Vol. 9, No. 2, pp. 63-68. [CrossRef]
- Alfonso E. Ayala, MD alfonso.ayala1@unlv.edu Kelvin Kim, MD Brandon A. Romero, MD Galen S. Kam, MD, The Boyd approach: a valuable alternative to treating simple to complex elbow fractures and dislocations, 2023, ELBOW Volume 32, Issue 12P2590-2598 December.
- Tito Sumarwoto, Seti Aji Hadinoto, Dina Aprilya, Sigit Bayudono, Totok Siswanto, Functional Outcomesof Neglected Elbow Dislocation Treated with Double Approach Surgery, 2023, Journals, Orthopedic research and Review,Volume 2023:15, Pages 175-181. [CrossRef]
- Midtgaard KS, Ruzbarsky JJ, Hackett TR, Viola RW. Elbow Fractures. Clin Sports Med. 2020; 39(3):623–36.
- Johanna Habarta MS, Martin Jordan MD, Rainer Meffert MD, Henner Huflage MD & Jonas Schmalzl MD, Surgical management of a traumatic elbow dislocation with disrupt of brachial artery, 2022, Springer nature link, Volume 17, pages 267-271. [CrossRef]
- Matelenok YM. Treatment of neglected complex dislocations in the elbow joint (clinical case). Orthopaedics, Traumatology & Prosthetics/Ortopediia, Traumatologiia i Protezirovaniie. 2023;(3). [CrossRef]
- Amir Bisadi, Fatemeh Abbasi, Mohammad Abbasalizadeh, Morteza Gholipour, A novel internal fixation technique for chronic elbow dislocations: Technical note and case report 2025, Radiology Case Reports Volume 20, Issue 9, September 2025, Pages 4572-457. [CrossRef]
- Aggarwal S, Paknikar K, Sinha J, Compson J, Reichert I. Comprehensive review of surgical approaches to the elbow. J Clin Orthop Trauma. 2021;20: 101539. [CrossRef]
- Li J, Martin VT, Li DT, et al. Lateral epicondyle osteotomy approach vs. olecranon osteotomy approach: an anatomic study of cadavers. J Shoulder Elbow Surg. 2022;31(11):2339–46. [CrossRef]
- Tangtiphaiboontana J, Agel J, Beingessner D, Hébert-Davies J. Prolonged dislocation and delay to surgery are associated with higher rates of heterotopic ossification in operatively treated terrible triad injuries. JSES international. 2020;4(2):238-41. [CrossRef]
- Mukesh Meena Karmbeer Singh Meena Sanjay Chetan Kumbhare Dushyant Chouhan Lateral Approach Versus Combined Lateral and Anteromedial Approach for Surgical Treatment of Terrible Triad of Elbow: A Meta-Analysis, 2020, Buletin of Emergency and Trauma.
- Hoyt BW, Clark DM, Walsh SA, et al. Surgical elbow dislocation approach to the distal humerus for apparent capitellar and lateral condyle fractures in adults. J Orthop Trauma. 2021;35(3):77–81. [CrossRef]
- Farhan Ahmad BS,Luis Torres-Gonzales BS, Nabil Mehta MD, Mark S Cohen MD, Xavier Simcock MD, Robert W Wysocki MD, range of motion progression patterns following open release for posttraumatic elbow stifness, 2022, JSES International Volume 6, Issue 3, May, Pages 545-549. [CrossRef]
- Nuradeen Altine Aliyu and Ahmad Kamaluddeen Results of Open Reduction and V-Y Triceps Plasty of Old Unreduced Elbow Dislocations in 38 Patients with Severe Extension Deformity Asian Journal of Orthopaedic Research 2024, Volume 7, Issue 2, Page 71-79,; Article no.AJORR.117182.
- Shakti Prasad da, Govid VJ, Preethiv R, Suhav Sondur, Avinash naik, Ankit Gulia, Answesit Mohanty,Outcomes of the Posterior Approach for the Treatment of radial head Fractures and Associated Elbowinjuries: A Retrospective Observational Study, 2023, Cureus journal of Medicine od Science. [CrossRef]
- Salihu MN, Arojuraye SA, Alabi AI, Mustapha IU, Okoh N, Ayeni FB. Old unreduced elbow dislocation: Patients’ perspectives on outcome of open reduction. The Surgeon. 2021;19(2):87-92. [CrossRef]
- M. Wynn, N. Glass, T. Fowler Comparison of direct surgical cost and outcomes for unstable elbow injuries: internal joint stabilizer versus external fixation, 2023 JSES Int, 7 (4) , pp. 692-698. [CrossRef]
- M. Rawal, P.K. Rokaya, D.B. Karki, K.K. Bhandari, A.K. Thakur Outcome of neglected elbow dislocation treated with open reduction at rural tertiary care hospital in Nepal, 2020, J Nepal Health Res CouncNov 14;18(3):525-528. [CrossRef]
- R.A. Agha, T. Franchi, C. Sohrab, G. Mathew, A. Kirwan, A. Thomas, et al. The SCARE 2020 guideline: updating consensus surgical case report (SCARE) guidelines Int. J. Surg., 84 (1) , pp. 226-230.
- W. Sun, X. Jiang, M. Gong, Y. Zha Diagnosis and treatment of chronic elbow dislocation, 2020, Int. J. Surg. , pp. 721-725.
- J. Singh, M.H. Elvey, Z. Hamoodi, A.C. Watts Current perspectives on elbow dislocation and instability 2021 Ann. Joint, 6.
- Eman Faqih, Hasan sawan, Shoog Fahad Alfadhel, Khaled AlAbbasi, Mustafa Alrawi, Chronic Complex elbow fracture dislocation: Restoration of elbow function with ORIF and radial head replacement, a case report with long term follow up, International Journal of Surgery Case Reports Volume 112, November 2023, 108912. [CrossRef]
- Atwan Y, Abdulla I, Grewal R, Faber KJ, King GJ, Athwal GS. 2023, Indomethacin for heterotopic ossification prophylaxis following surgical treatment of elbow trauma: A randomized controlled trial. Journal of Shoulder and Elbow Surgery.;32(6):1242-8. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).