1. Introduction
Peripheral artery disease assessment typically focuses on symptoms and physical findings in the lower extremities. However, few practitioners recognize the significance of upper extremity arterial disease, which, besides causing hand and arm symptoms, can be linked to serious neurologic and cardiac complications.
Subclavian artery stenosis can cause significant morbidity by leading to symptomatic ischemic issues affecting the upper extremities, brain, and sometimes the heart.
While atherosclerosis is the most common cause, other causes include arteritis, radiation-induced inflammation, compression syndromes, fibromuscular dysplasia, and neurofibromatosis. The incidence of subclavian stenosis in the general population ranges from 3% to 4%, [
1] and can be as high as 11–18% in patients with documented peripheral artery disease [
2]. Among patients with subclavian or innominate lesions, 50% also have coronary artery disease, 27% have lower extremity artery involvement, and 29% have carotid obstructive disease [
3,
4]. Consequently, these patients face an increased risk of developing symptomatic coronary artery disease and cerebrovascular events [
5,
6].
Subclavian steal syndrome (SSS) is a vascular condition characterized by reverse blood flow through the vertebral artery, typically resulting from critical stenosis or occlusion of the subclavian artery proximal to its origin. This phenomenon is often worsened by age-related vascular changes and atherosclerosis, especially in older adults.
Patients with significant subclavian artery stenosis may experience cerebrovascular ischemia, leading to various neurological symptoms mainly due to reduced blood flow to the posterior circulation [
7]. In aging populations, risk factors for subclavian steal syndrome include atherosclerosis, hypertension, and lifestyle factors such as tobacco use and dyslipidaemia, all of which increase the risk of arterial stenosis [8, 9]. Additionally, aging can lead to vascular remodelling, predisposing individuals to this condition. Patients may present with symptoms of vertebrobasilar insufficiency, such as light-headedness, syncope, dizziness, and even transient ischemic attacks or strokes, underscoring the importance of prompt diagnosis and treatment [10, 11].
Effective management of comorbid cardiovascular conditions is crucial for slowing the progression of atherosclerosis and its effects in the vulnerable older population [12, 13]. Given the complex nature of subclavian steal syndrome and its interaction with aging, attention to vascular health and timely intervention are vital for improving outcomes in patients with this condition.
Overshadowed omarthrosis and subclavian steal syndrome are two distinct yet potentially related conditions that warrant careful attention, especially in older adults. Both can significantly impair quality of life and functional ability, highlighting the importance of accurate diagnosis and comprehensive management strategies.
Glenohumeral arthritis, often caused by degenerative changes related to age, trauma, or repetitive use, leads to deterioration of the shoulder joint. This condition typically presents with pain, stiffness, and impaired shoulder function, which can severely hinder daily activities. The underlying pathology involves changes in articular cartilage, subchondral bone, and synovial inflammation, which are often exacerbated by systemic inflammatory responses common in older adults.
Omarthrosis—shoulder osteoarthritis—is increasingly recognized among the aging population due to various factors, including aging, occupational exposures, and continuous use of the shoulder joint. As people age, degenerative changes in the shoulder joint are common, with conditions such as adhesive capsulitis, rotator cuff disease, and generalized osteoarthritis being prevalent among older individuals, leading to significant morbidity and functional limitations [
14]. Occupational factors play a key role in worsening shoulder disorders, research shows that repetitive tasks, awkward arm positions, and prolonged mechanical stress can increase the risk of shoulder pain and dysfunction [15, 16].
The interaction between age and occupational factors is vital to understanding the risk of shoulder disorders. Older adults previously involved in physically demanding work face higher risks of shoulder pain and related functional impairments. Moreover, the cumulative impact of occupational exposures over a person's work life can lead to the early onset of degenerative joint conditions.
The interaction between omarthrosis and subclavian artery occlusion, especially in older adults, is a significant clinical issue. Age-related factors contribute to both conditions, which may have overlapping symptoms, making accurate diagnosis and treatment challenging. This overlap can cause orthostatic hypotension to mask the symptoms of subclavian artery occlusion, potentially delaying recognition of associated vascular problems.
Symptoms of SSS may include dizziness, vertigo, or other signs of vertebrobasilar insufficiency, which can be mistaken for musculoskeletal issues related to shoulder osteoarthritis. For example, a patient experiencing dizziness might interpret this as due to pain and limited mobility from omarthrosis, rather than a sign of possible cerebrovascular insufficiency.
The diagnostic challenges caused by this overlap require careful assessment. Clinicians should take a detailed history and perform a thorough physical exam to distinguish between different causes of symptoms. Imaging tests, such as Doppler ultrasound or angiography, may be necessary to identify vascular problems, especially when SSS symptoms are suspected in conjunction with shoulder conditions.
In conclusion, having both omarthrosis and subclavian artery occlusion can complicate clinical signs in older adults, where mobility issues from shoulder arthritis may hide severe vascular symptoms. An interdisciplinary approach to evaluation and treatment is crucial for preventing future cerebrovascular events and ensuring the effective management of both musculoskeletal and vascular issues.
2. Case Presentation
An 87-year-old woman with a significant medical history, including dementia, hypertension, and coronary artery disease, was brought to the emergency department by ambulance. Her nephew, who was out of town, contacted the police after not hearing from her for two days. The police assisted in accessing her apartment, where she lived alone.
2.1. Emergency Department Admission
Upon admission, the patient was immobile, had limited rational contact, and reported lower back pain. Initial laboratory diagnostics revealed moderate hyponatremia (127.3 mmol/l), hypokalaemia (2.65 mmol/l), and elevated inflammatory parameters (CRP 32.0 mg/l).
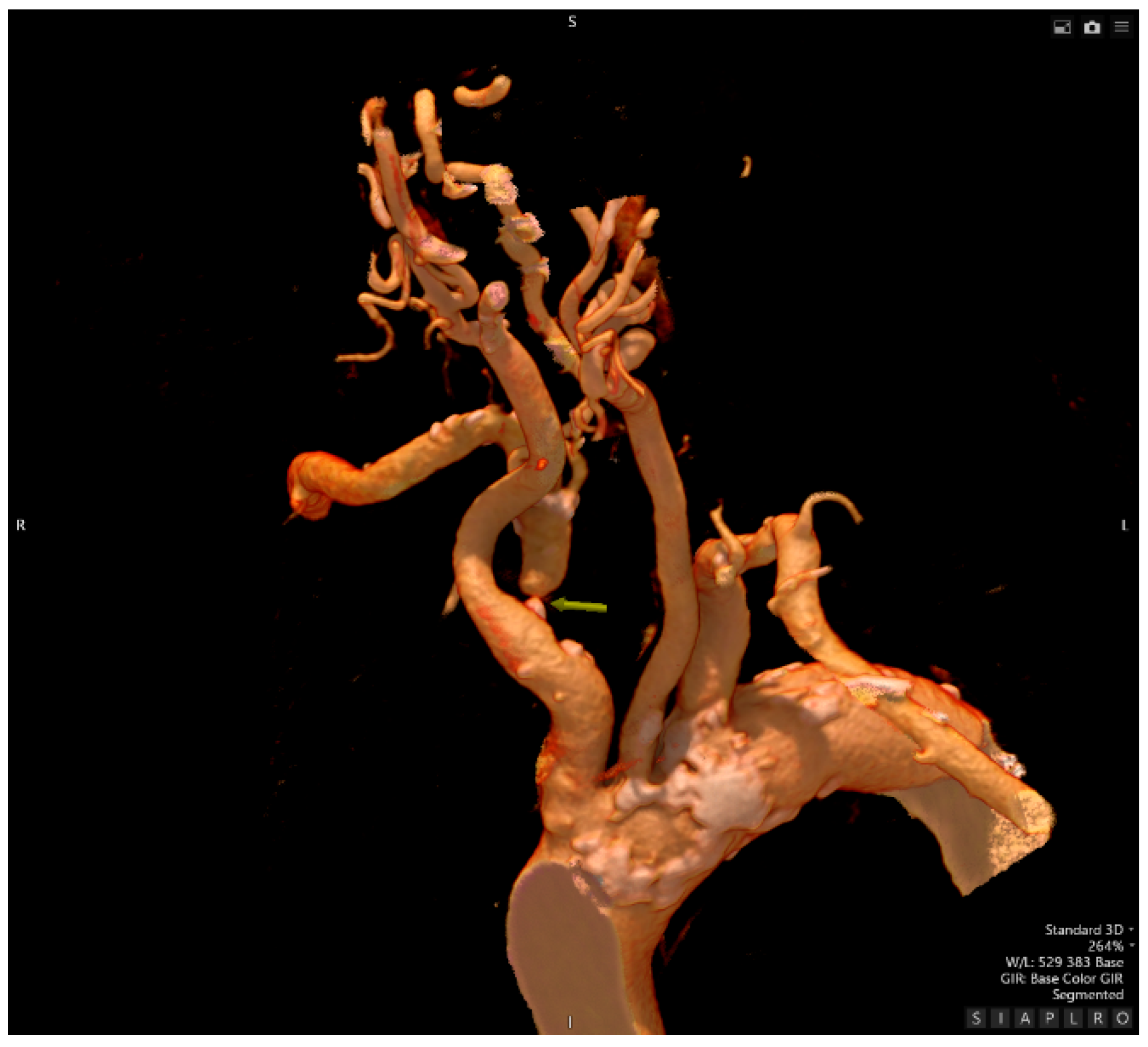
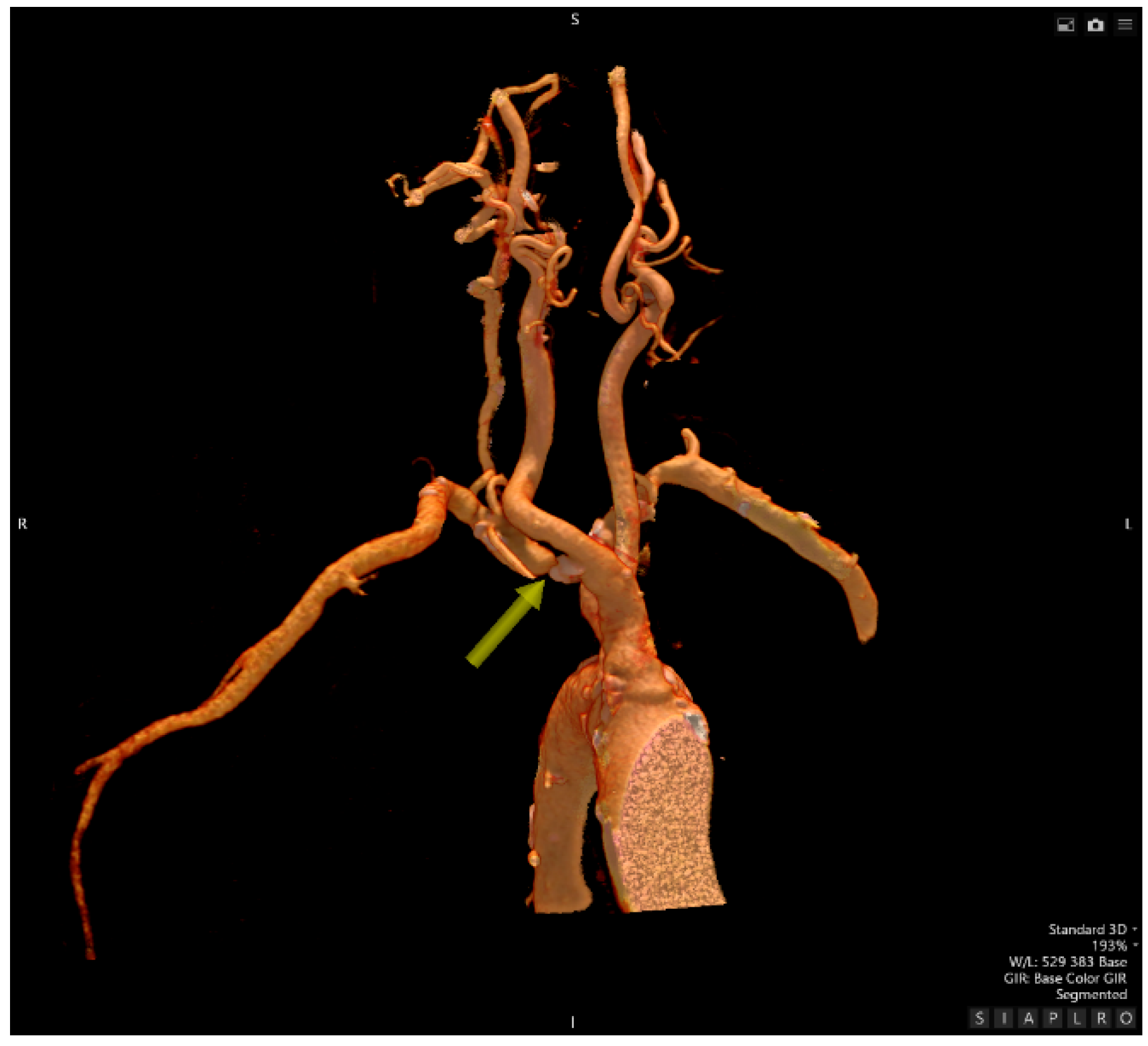
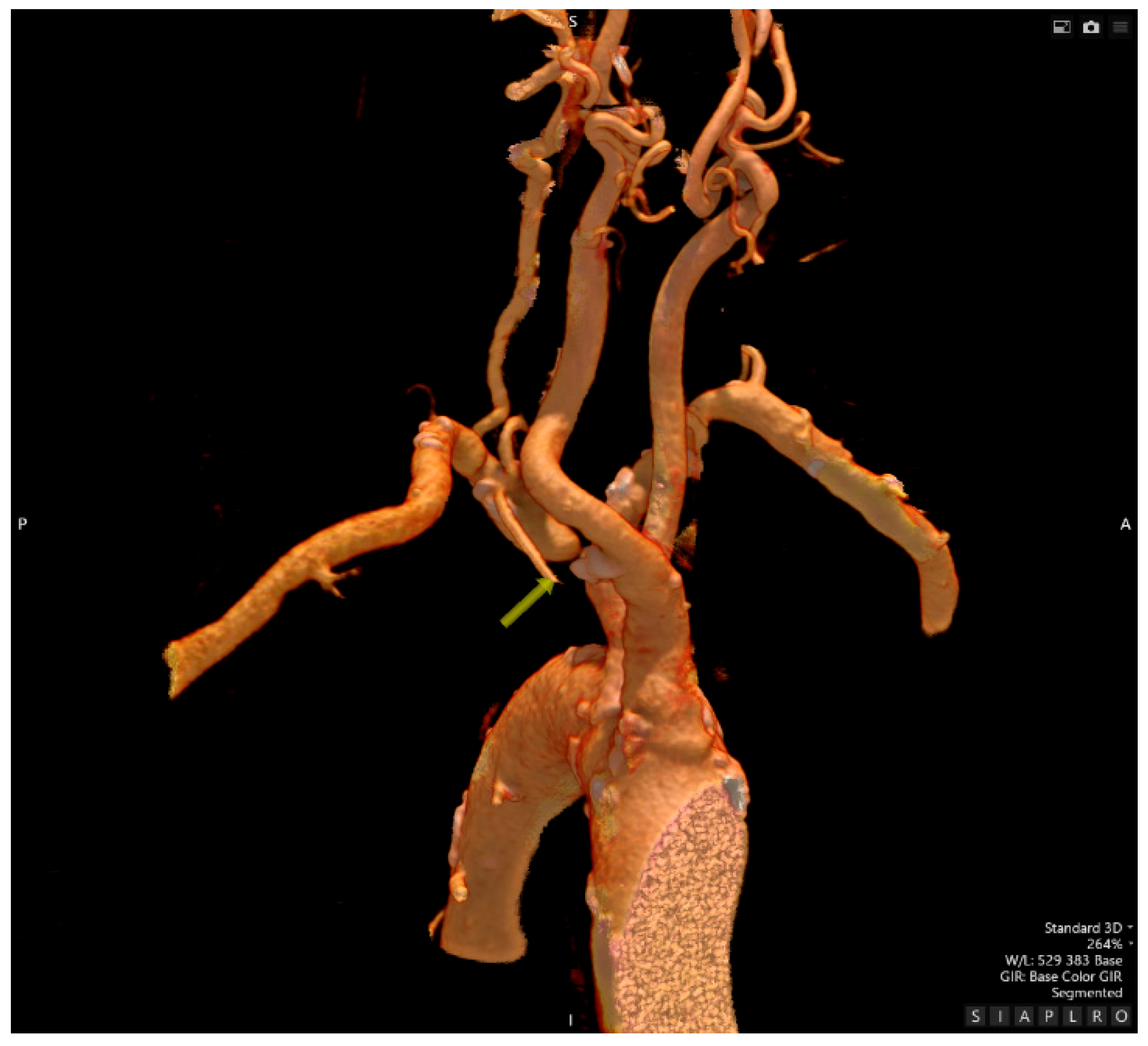
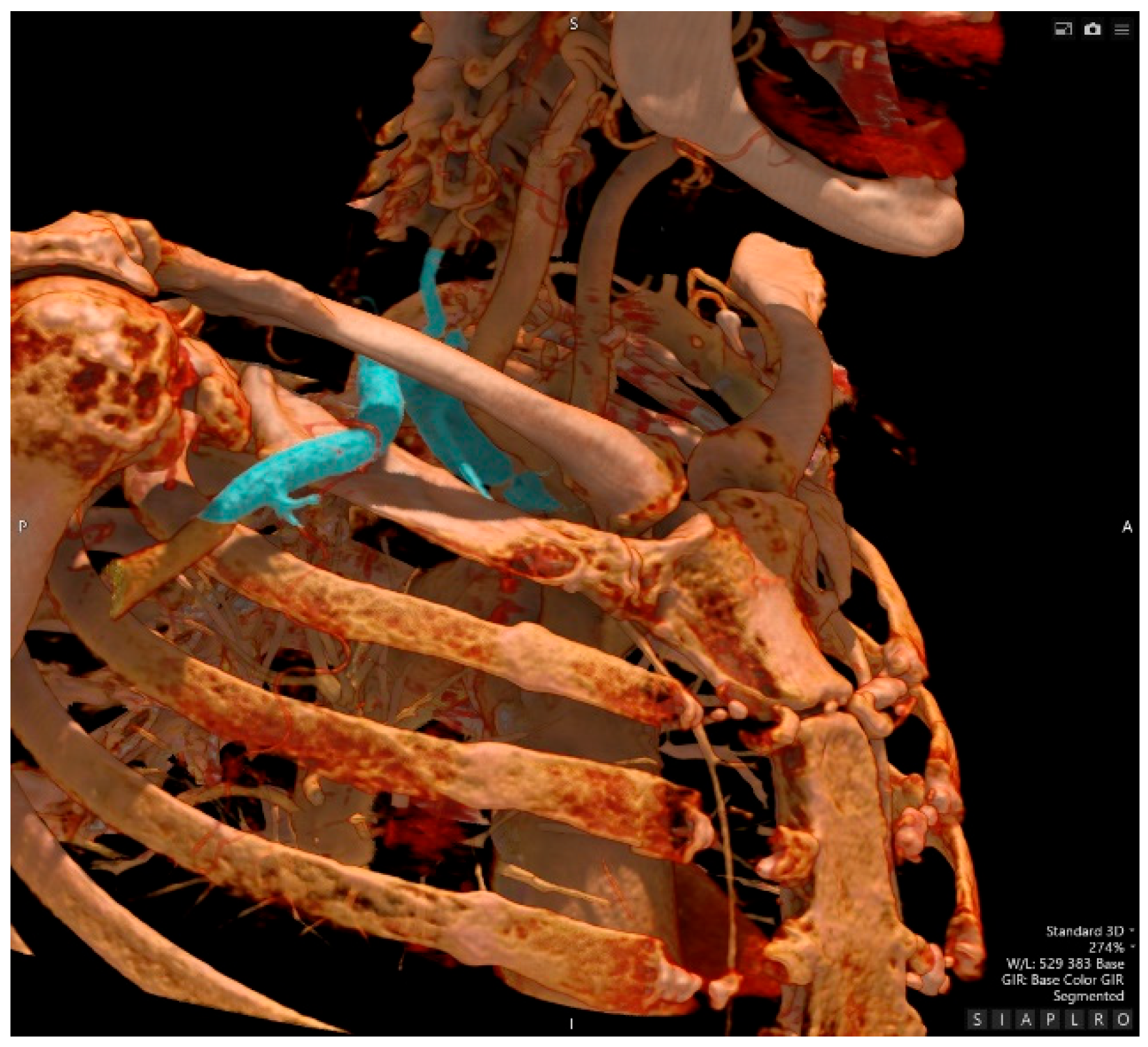
Known medical history (from electronic records) upon admission includes 13 pack-years, arterial hypertension/labile hypertension, ischemic heart disease, unstable angina pectoris, left anterior fascicular block, occasional supraventricular extrasystoles, calcification changes in the aortic and mitral valves, mitral insufficiency grade II, widespread atherosclerosis (aorta, heart, central nervous system), right-sided glenohumeral arthritis (Fig. 1 & Fig. 5), hypercholesterolemia, subclinical hypothyroidism, polytopic vertebrogenic algic syndrome, early lower limb dystrophy, bilateral grade II coxarthrosis, dementia—probably of vascular origin—with calcifications of the basal ganglia on the right, leukoaraiosis, diffuse brain atrophy, hypoacusis, chronic kidney disease (KDIGO 2) due to nephrosclerosis, hyperuricemia, and pulmonary emphysema secondary to ex-nicotinism. The patient worked as a hairdresser for most of her life. She is the mother of two children—both her son and daughter are deceased. Her mother died at age 80 and was treated for type 2 diabetes and hypertension.
2.2. Geriatrics Department
After correcting the mineral imbalance, discontinuing hydrochlorothiazide from the antihypertensive treatment, starting parenteral analgesic therapy, and inserting a urinary catheter, X-rays of the pelvis and lower spine were performed (showing no traumatic changes).
A subsequent magnetic resonance imaging confirmed central lumbar spinal stenosis with multi-level disc bulging; neurosurgical intervention was not advised. In addition to local therapy, the neurologist prescribed pregabalin and recommended physiotherapy. Laboratory tests revealed normocytic normochromic anaemia with iron and cobalamin deficiency. Elevated inflammatory markers were attributed to a urinary tract infection, and a suspected fall was likely responsible for the isolated increase in D-dimers (9.0 mg/l).
The doses of the ACE inhibitor were increased due to ongoing hypertension. Previously elevated creatine kinase and myoglobin levels decreased, ruling out statin myopathy.
Due to the patient’s immobility and the placement of a permanent urinary catheter, she was transferred to the long-term care ward on the seventh day of hospitalization.
2.3. Long-term Care Department
On admission, the patient was hemodynamically stable, with no signs of infection, and was oriented to time, place, and person. A systolic murmur 2/6 was auscultated over the precordium. BMI was 27.5; SpO2 was 96% on room air; pulse rate ranged from 57 to 61 beats per minute; blood pressure in the left upper limb was 187-194/72-76 mmHg; and in the right upper limb, it was 136/91 mmHg.
The clinical picture is characterized by pain in the right shoulder at rest and during minimal exertion. The right upper limb shows no signs of ischemia, nor are there noticeable differences in skin temperature between the limbs. Objectively, the temperature of the right shoulder was 35°C, while the left shoulder measured 36.2°C.
Pulsations of the radial and ulnar arteries on the right arm were minimally palpable. Continuous Wave Doppler and Colour Duplex Doppler Ultrasonography: The right shoulder showed a 120 mmHg monophasic waveform, and the left shoulder showed a 160 mmHg triphasic waveform.
Findings indicate severe stenosis of the right subclavian artery—a calcified atherosclerotic plaque, approximately 1.5 cm long, with an estimated 70% stenosis in the prescalene segment.
The CTA showed segmental occlusion of the right subclavian artery at its origin from the brachiocephalic trunk, approximately 7 mm in length, caused by mixed atherosclerotic plaques, located more distally than the right subclavian artery (Fig. 2, 3, 4, 5). It also involved the peripheral vessels of the right upper limb, mainly supplied through the right vertebral artery and several other muscular arterial connections, along with connections from the right external carotid artery. A small aneurysm with a wider neck in the C7 segment of the ACI on the left, measuring approximately 3 x 2 mm, was found in the captured part of the intracranial region, extending laterally.
Cortical brain atrophy and vascular leukoencephalopathy were observed. An incidental finding included the retropharyngeal course of the ACI on the right and kinking of the ACI behind bilateral branches.
Otherwise, there was age-appropriate opacification of the remaining epiaortal branches of the aortic arch, which supply the arteries of the circle of Willis.
Verified compression deconfiguration of the L1-L2 vertebrae, recommended a custom-made lumbar support belt, and suggested physiotherapy, considering the patient's comorbidities and current condition.
The patient reports long-term weakness in her right arm, mainly noticed when washing her hair, with an inability to raise her upper limb properly. Recently, the weakness has worsened, and over the past 1-2 months, she has experienced vertigo, which she described as difficult to explain, especially when turning her head to the sides. This vertigo was relieved when lying on a flat surface. She denied diplopia, although she has had eye surgery and has not been able to see clearly for a long time. She had no difficulty swallowing or speech disorders. She also reported no paraesthesia in her upper or lower limbs.
Upon examination, the patient was conscious and oriented, with no signs of meningeal irritation. Speech was everyday without dysarthria or fatigue, eyeballs were in the midline, pupils were equal and reactive to light, with no oculomotor abnormalities or nystagmus. No other cranial nerve deficits were observed. The tongue was midline. There was mild monoparesis of the right upper limb, with no weakness in the left upper limb. Slightly increased muscle tone was noted in the elbow joints, possibly influenced by patient effort. No signs of irritation or sensory deficits were present. Posture and gait could not be assessed due to the current condition.
A multidisciplinary team recommended that the patient attempt recanalization of the subclavian artery due to subclavian steal syndrome, right shoulder pain, and labile hypertension.
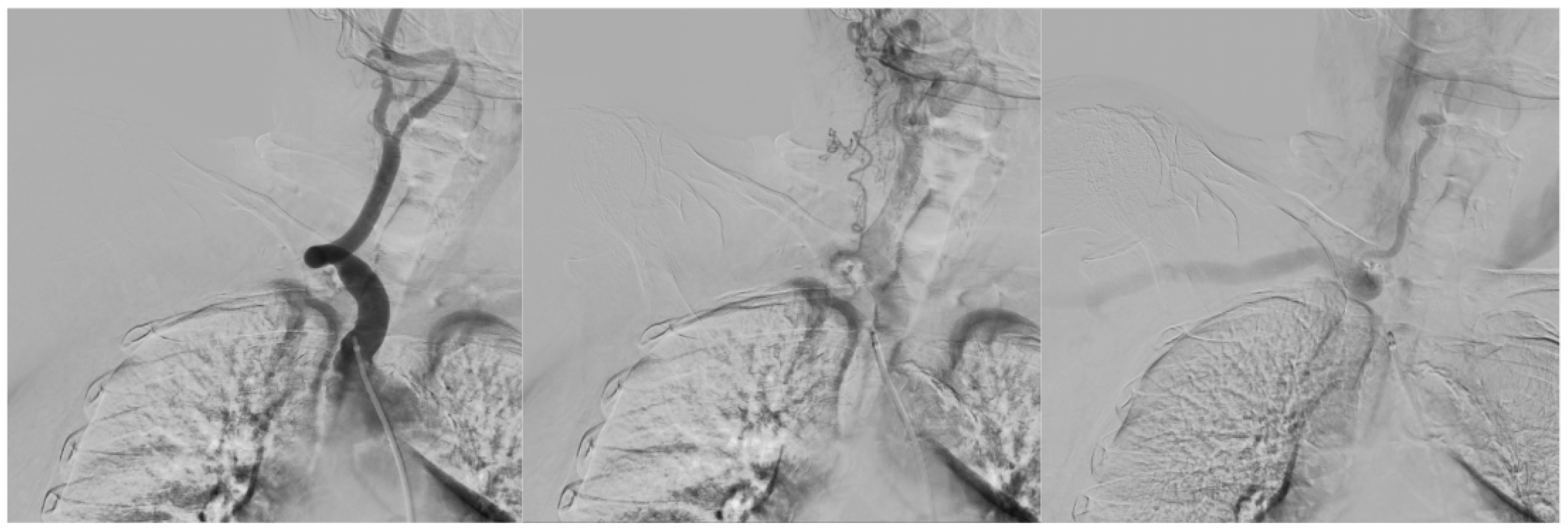
Under local anaesthesia, a 90 cm, 6F sheath was inserted via a right transfemoral approach. The brachiocephalic trunk was catheterized to verify occlusion of the right subclavian artery caused by a thick, calcified lesion using DSA (Fig. 6). Multiple types of catheters and guides were used in attempts at antegrade recanalization, which was unsuccessful. Therefore, retrograde puncture of the right brachial artery using micro instruments was performed, gradually advancing the 4F sheath to the occlusion of the subclavian artery from the distal side. Using 0.035" and low-profile instruments (0.018", 0.014"), recanalization was attempted, but only a subintimal technique was possible, with re-entry in the aortic arch area. Because of the need to maintain direct flow in the right common carotid artery, this approach was not feasible. Passage through the rigid occlusion intraluminally was not possible.
At the final DSA check, no complications were present.
An incidental small aneurysm with a wider neck was found in the C7 segment of the left internal carotid artery, measuring approximately 3x2mm and deviating laterally.
During the assessment, the patient was conscious, alert, and showed no signs of headache or meningeal irritation, with preserved and symmetrical limb mobility. UIATs 4/12 in favour of conservative treatment.
Upon admission to the Long-term Care Department, the patient scored 25 points. At the time of discharge, the patient reached 50 points.
During admission to the long-term care ward, we thoroughly reviewed all available medical records. Documentation from the primary care physician, outpatient clinics, and all hospitalizations over the past 13 years mentions only one instance of absent pulsation in the right radial artery, which occurred in May 2012 (Tab. 1 & Tab. 2).
Table 1.
Patients’ hospitalisations over the past years.
Table 1.
Patients’ hospitalisations over the past years.
| 05/2012 |
Department of Geriatrics - unstable angina |
| 08/2012 |
National Institute for Cardiovascular Diseases - coronarography |
| 10/2012 |
Oncological Institute - postmenopausal metrorrhagia |
| 12/2012 |
Oncological Institute - uterine adenocarcinoma |
| 09/2015 |
Department of Geriatrics - ISMN-related collapse |
| 2017 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
| 2018 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
| 2019 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
| 2020 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
| 2021 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
| 2023 |
Brought to the ER due to the ISMN-related collapse/short-term hospitalisation |
Table 2.
Patients’ outpatient visits with different specialists over the past years.
Table 2.
Patients’ outpatient visits with different specialists over the past years.
| 06/2012 |
Internal medicine outpatient |
| 07/2012 |
Internal medicine outpatient |
| 07/2012 |
Preoperative evaluation (Internal medicine) |
| 10/2012 |
Preoperative evaluation (Internal medicine) |
| 11/2012 |
Preoperative evaluation (Dept. of Anaesthesiology and Intensive Care) |
| 01/2013 |
Geriatrics outpatient |
| 02/2013 |
Geriatrics outpatient |
| 06/2013 |
Geriatrics outpatient |
| 12/2013 |
Geriatrics outpatient |
| 06/2014 |
Geriatrics outpatient |
| 12/2014 |
Geriatrics outpatient |
| 06/2015 |
Geriatrics outpatient |
| 01/2016 |
Cardiology outpatient |
| 01/2017 |
Cardiology outpatient |
| 09/2017 |
Cardiology outpatient |
| 03/2018 |
Cardiology outpatient |
| 10/2018 |
Cardiology outpatient |
| 05/2019 |
Cardiology outpatient |
| 01/2020 |
Cardiology outpatient |
| 10/2020 |
Cardiology outpatient |
| 07/2021 |
Cardiology outpatient |
| 03/2023 |
Cardiology outpatient |
We also observed that during most hospitalizations, an intravenous access was inserted on the right side, which means blood pressure was mainly measured on the left arm, as the patient has better and more prominent vascular patterns on the right arm.
Although the attempt to recanalize the subclavian artery was unsuccessful, it was performed without complications. Given the patient's condition and the size of the incidental aneurysm of the left internal carotid artery, a conservative approach—dual antiplatelet therapy—was recommended. Optimization of medication and intensive physiotherapy resulted in the expected improvements. Upon discharge, the patient was able to walk with assistance. Due to her complex health issues, including frequent hospitalizations in recent years (Tab. 1), she was transferred to a nursing home.
3. Discussion
3.1. Impact of SAO and SSS on Cognitive Impairment
Subclavian artery occlusion is increasingly recognized as a factor contributing to cognitive decline, mainly through mechanisms related to cerebral hypoperfusion and vascular dementia. The occlusion cannot only diminish blood flow to the upper limbs but also reduce overall cerebral blood flow, which is vital for maintaining cognitive functions.
This condition is often worsened by various types of cognitive dysfunction caused by impaired brain hemodynamics. One primary way subclavian artery occlusion affects cognition is through cerebral hypoperfusion. A study by Zhao et al. shows that chronic cerebral hypoperfusion, resulting from conditions like stenosis or occlusion of head and neck arteries, leads to executive dysfunction, mainly impacting attention, memory, and cognitive flexibility.
The link between reduced regional cerebral blood flow (rCBF) and cognitive performance shows that moderate decreases in rCBF can significantly impair cognitive abilities, contributing to vascular cognitive impairment [
17]. Furthermore, evidence indicates that large occlusions, including those of the subclavian artery, can cause ischemic strokes, often leading to vascular dementia (VaD).
The SPS3 study emphasizes that lacunar strokes, usually caused by small vessel occlusion, are common causes of executive dysfunction and cognitive decline, indicating that repeated ischemic events can worsen cognitive impairments [
18]. Therefore, managing significant subclavian artery occlusion through procedures like stenting or angioplasty is recommended to help restore cerebral blood flow and improve cognitive function [
19].
Additionally, brain regions, especially vulnerable to hypoperfusion, such as the hippocampus, are crucial for memory and cognitive functions. Animal studies show that chronic hypoperfusion leads to cell damage and cognitive impairments, resembling many features of human vascular dementia [20, 21].
Specifically, Choi et al. found that chronic hypoperfusion can worsen cognitive deficits when combined with other pathological conditions like amyloid toxicity, which is associated with Alzheimer's disease, highlighting the complex nature of cognitive impairment after occlusion [
22]. The anatomical effects of subclavian artery issues extend to how decreased perfusion pressures negatively affect overall brain health. Kalaria explains that vascular risk factors, such as those linked to occlusive disease in the subclavian artery, can lead not only to stable cognitive decline but also to progressive deterioration related to degenerative processes [
23].
Notably, the interconnectedness of cerebrovascular health indicates that subclavian artery occlusion can have both local and systemic effects, ultimately affecting broader cognitive health. In summary, subclavian artery occlusion may lead to cognitive decline through multiple pathways, primarily related to cerebral hypoperfusion and its consequences.
Recognizing these connections highlights the importance of timely interventions to restore blood flow and reduce cognitive impairment, as well as addressing atherosclerosis and its impact on cognitive health.
3.2. Subclavian Steal Syndrome / Subclavian Artery Occlusion and Hypertension
Subclavian artery occlusion and labile hypertension are common conditions that frequently occur together, especially in older adults. Subclavian artery occlusion usually results from atherosclerotic changes that decrease blood flow, which can lead to persistent hypertension with blood pressure fluctuations—known as labile hypertension.
This connection is significant because of its effect on vascular health and overall quality of life in aging patients, who are especially vulnerable to both conditions. Older individuals experience high rates of hypertension mainly due to vascular aging, which involves structural and functional changes in arterial walls, such as thickening and calcification [24, 25].
The high prevalence of hypertension in this group can worsen existing cardiovascular problems by interacting with various pathophysiological processes like impaired kidney function and decreased arterial compliance [
26].
3.3. Methodology of Blood Pressure Monitoring in the Age Group ≥ 65 Years
Monitoring blood pressure in both arms of older individuals is essential for various clinical and diagnostic reasons. Differences in blood pressure readings between arms can reveal underlying vascular issues, such as subclavian artery stenosis.
A difference greater than 15 mmHg in systolic blood pressure between the arms suggests unilateral subclavian stenosis, emphasizing the importance of measuring both arms in patients over 65 years old [
27].
As people age, physiological changes can lead to an increase in blood pressure due to alterations in vascular structure and elasticity. Arteries tend to stiffen with age, resulting in higher systolic blood pressure, while diastolic pressure may stay relatively stable [
28]. Proper blood pressure management is crucial, as older individuals often experience greater blood pressure variability and respond less effectively to antihypertensive medications [
29]. This variability complicates hypertension management and underscores the importance of regular monitoring.
Furthermore, blood pressure patterns over 24 hours in older adults often show a non-dipping pattern, which raises cardiovascular risk. When blood pressure stays high during sleep—that is, it does not decrease—there is an increased risk of cardiovascular events. Recognizing these patterns is important for developing effective hypertension treatment strategies in older adults.
Adding to the importance of thorough monitoring, ambulatory blood pressure measurements provide a more accurate picture of blood pressure fluctuations that might not be detected during a single office visit. Studies have demonstrated that ambulatory monitoring shows a higher prevalence of hypertension compared to traditional clinic measurements, especially in aging populations [30, 31].
3.4. Lesson Learnt - Experience Gained from Case Study
This case highlights the diagnostic challenge of subclavian steal syndrome (SSS) in a patient with advanced age, where advanced osteoarthritis of the right shoulder significantly masked the underlying vascular issue. In this particular case, chronic shoulder pain and limited mobility led clinicians to initially attribute recurrent dizziness and weakness to musculoskeletal problems (Tab. 2), delaying the diagnosis of a critical subclavian stenosis.
The link between subclavian artery occlusion and cognitive decline has been increasingly recognized. In the presented case report, mild cognitive impairment may have been worsened by chronic cerebral hypoperfusion, further highlighting the systemic effects of this condition.
Always consider vascular causes in older patients with unexplained dizziness, syncope, or labile hypertension.
Routine bilateral blood pressure measurement should be standard in both primary care and hospital settings for the aging population. This case emphasizes that bilateral blood pressure measurement should be a routine part of assessing older patients with labile hypertension, recurrent dizziness, or collapse episodes. Such a simple step can provide an important clue to subclavian artery occlusion.
Musculoskeletal disorders, such as omarthrosis, can conceal severe vascular conditions, necessitating an interdisciplinary approach to diagnosis. Clinicians should be aware that common issues like degenerative joint disease might coexist with or hide life-threatening vascular problems. An interdisciplinary approach combined with careful physical examination is vital to prevent misdiagnosis.
In frail, older patients with multiple comorbidities, conservative management can be an acceptable treatment option if the diagnosis is accurate and symptoms are well controlled.
Overall, this case emphasizes the importance of combining clinical vigilance with straightforward bedside diagnostic techniques to enhance patient outcomes in geriatrics.
4. Conclusions
The heterogeneity of healthcare needs in the geriatric population requires a comprehensive approach to their care. Healthcare professionals caring for older adults understand that medical issues are not the only factors involved in this “care complexity.” Socioeconomic, cognitive, functional, and organizational factors also play significant roles.
This patient story and case study clearly illustrate the high costs of specific medical errors and missed diagnoses. Healthcare expenses and other indirect socioeconomic impacts can be quantified. However, the impact on health and quality of life, considering the diagnoses and course of events described, cannot be measured.
Science and medicine are constantly advancing, but regarding SAO/SSS, current pharmacological and technological options have not changed much in the past 13 years. The chance for successful recanalization, which could impact the patient's overall health, is no longer feasible. Was it possible 12 years ago? We cannot say for certain.
Still, evidence-based and personalized medicine, case studies, scientific research, and meta-analyses across all areas of medicine, including geriatrics, continue to enhance our knowledge. Despite these advancements, we must remember the importance of basic examinations, clinical skills, judgment, and accuracy in daily practice.
Globally and in Europe, the aging population is growing. There will be more geriatric patients, and their health and social dependence levels are in our hands every day. Many older patients have multiple comorbidities that require diagnosis, making them more vulnerable to misdiagnosis. Misdiagnosis and missed diagnoses not only threaten the health of older patients but also add to broader socioeconomic burdens.
Older populations may be more prone to diagnostic errors due to factors involving both patients and clinicians. Older individuals may dismiss symptoms as a regular part of aging and not report them. Meanwhile, healthcare providers may focus too much on specific clinical signs that point to certain diseases, overlooking conflicting clues or failing to perform comprehensive differential diagnoses.
Diagnostic errors are relatively common and damaging in primary care. Although much remains to be understood, mistakes frequently occur when diagnosing common conditions. These errors in primary care impact all countries, and solutions require involvement from many stakeholders. However, opportunities to address these issues are still limited today.
What we can do is approach our work responsibly every day and remain aware of all the specifics related to different population groups, including the geriatric subpopulation.
Author Contributions
Conceptualization, M.S., S.M.; methodology, M.S.; validation, M.S., L.K., P.P., D.P., and P.M.; formal analysis, L.K., K.G.; investigation, M.S., K.D., and P.M.; data curation, S.M.; writing—original draft preparation, S.M.; writing—review and editing, M.S., L.K.; visualization, M.S., P.M.; supervision, S.M.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Since this is a case study describing only the hospitalization of the subject and standard medical care, without any experimental procedures, and the healthcare provided was not part of any alternative or experimental procedures as defined by Slovak legislation (Act No. 576/2004 Coll. on healthcare and Act No. 362/2011 Coll. on medicines and medical devices), approval from an Ethical Committee, whether from the University, University Hospital, or an Institutional Review Board, is not required. What is required by law in Slovakia is informed consent from the patient or the patient's representative.
Informed Consent Statement
Informed consent was obtained from the subject involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author(s).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ACE |
Angiotensin-Converting Enzyme |
| ACI |
Internal Carotid Artery |
| C7 ACI |
7th Segment of the Internal Carotid Artery |
| CTA |
Computed Tomography Angiography |
| DSA |
Digital Subtraction Angiography |
| ISMN |
Isosorbide mononitrate |
| rCBF |
Regional Cerebral Blood Flow |
| SAO |
Subclavian artery occlusion |
| SPS3 |
Secondary Prevention of Small Subcortical Strokes study |
| SSS |
Subclavian Steal Syndrome |
| UIATS |
The Unruptured Intracranial Aneurysm Treatment Score |
| VaD |
Vascular Dementia |
References
- English, J.L.; Carell, E.S.; Guidera, S.A.; Tripp, H.F. Angiographic prevalence and clinical predictors of left subclavian stenosis in patients undergoing diagnostic cardiac catheterization. Catheter. Cardiovasc. Interv. 2001, 54, 8–11. [CrossRef]
- Gutierrez, G.R.; Mahrer, P.; Aharonian, V.; Mansukhani, P.; Bruss, J. Prevalence of Subclavian Artery Stenosis in Patients with Peripheral Vascular Disease. Angiology 2001, 52, 189–194. [CrossRef]
- Rodriguez-Lopez, J.A.; Werner, A.; Martinez, R.; Torruella, L.J.; Ray, L.I.; Diethrich, E.B. Stenting for Atherosclerotic Occlusive Disease of the Subclavian Artery. Ann. Vasc. Surg. 1999, 13, 254–260. [CrossRef]
- Brountzos, E.N.; Petersen, B.; Binkert, C.; Panagiotou, I.; Kaufman, J.A. Primary Stenting of Subclavian and Innominate Artery Occlusive Disease: A Single Center?s Experience. Cardiovasc. Interv. Radiol. 2004, 27, 616–623. [CrossRef]
- Hennerici, M.; Rautenberg, W.; Mohr, S. STROKE RISK FROM SYMPTOMLESS EXTRACRANIAL ARTERIAL DISEASE. Lancet 1982, 320, 1180–1183. [CrossRef]
- MORAN, K.; ZIDE, R.; PERSSON, A.; JEWELL, E. NATURAL-HISTORY OF SUBCLAVIAN STEAL SYNDROME. 1988, 54, 643–644.
- Khurshid, F.; Khurshid, A. Unraveling the complexity: A comprehensive guide to subclavian steal syndrome.. J. Shifa Tameer-e-Millat Univ. 2023, 6, 100–105. [CrossRef]
- Dieter, R.S.; Darki, A.; Nanjundappa, A.; Lopez, J.J. Subclavian Steal Syndrome Successfully Treated with a Novel Application of Embolic Capture Angioplasty. Int. J. Angiol. 2012, 21, 121–124. [CrossRef]
- Dragičević, D.; Škorić, M.; Kolić, K.; Titlić, M. A case of acquired right-sided subclavian steal syndrome successfully treated with stenting using brachial approach. Case Rep. Clin. Med. 2014, 03, 70–75. [CrossRef]
- Soldo, S.B. Subclavian fusiform aneurysm causing partial subclavian steal syndrome. Case report. Med Ultrason. 2014, 16, 75–77. [CrossRef]
- Smith, M.C.; Pham, R.; Coffey, N.; Kazimuddin, M.; Singh, A. Coronary Subclavian Steal Syndrome With Neurological Symptoms After Coronary Artery Bypass Grafting. Cureus 2021, 13. [CrossRef]
- Amini, R.; Gornik, H.L.; Gilbert, L.; Whitelaw, S.; Shishehbor, M. Bilateral Subclavian Steal Syndrome. Case Rep. Cardiol. 2011, 2011, 1–5. [CrossRef]
- Arı, H., Arı, S., Çamcı, S., Karakuş, A., & Melek, M. (2016). Quantitative assessment of the effect of subclavian steal syndrome on left anterior descending artery flow. Turk Kardiyoloji Dernegi Arsivi-Archives of the Turkish Society of Cardiology.
- Ibounig, T.; Simons, T.; Launonen, A.; Paavola, M. Glenohumeral osteoarthritis: an overview of etiology and diagnostics. Scand. J. Surg. 2020, 110, 441–451. [CrossRef]
- Dickerson, C.R.; Brookham, R.L.; Chopp, J.N. The working shoulder: assessing demands, identifying risks, and promoting healthy occupational performance. Phys. Ther. Rev. 2011, 16, 310–320. [CrossRef]
- Tang, S., Zhang, C., Oo, W.M. et al. Osteoarthritis. Nat Rev Dis Primers 11, 10 (2025).
- Zhao, J.-H.; Tian, X.-J.; Liu, Y.-X.; Yuan, B.; Zhai, K.-H.; Wang, C.-W.; Yue, J.-Y.; Zhang, L.-J.; Li, Q.; Yan, H.-Q.; et al. Executive Dysfunction in Patients With Cerebral Hypoperfusion After Cerebral Angiostenosis/Occlusion. Neurol. medico-chirurgica 2013, 53, 141–147. [CrossRef]
- Benavente, O.R.; White, C.L.; Pearce, L.; Pergola, P.; Roldan, A.; Benavente, M.-F.; Coffey, C.; McClure, L.A.; Szychowski, J.M.; Conwit, R.; et al. The Secondary Prevention of Small Subcortical Strokes (SPS3) Study. Int. J. Stroke 2011, 6, 164–175. [CrossRef]
- Lin, M.-S.; Chiu, M.-J.; Wu, Y.-W.; Huang, C.-C.; Chen, Y.-H.; Li, H.-Y.; Chen, Y.-F.; Lin, L.-C.; Liu, Y.-B.; Chao, C.-L.; et al. Neurocognitive Improvement After Carotid Artery Stenting in Patients With Chronic Internal Carotid Artery Occlusion and Cerebral Ischemia. Stroke 2011, 42, 2850–2854. [CrossRef]
- Srinivasan, V.J.; Yu, E.; Radhakrishnan, H.; Can, A.; Climov, M.; Leahy, C.; Ayata, C.; Eikermann-Haerter, K. Micro-Heterogeneity of Flow in a Mouse Model of Chronic Cerebral Hypoperfusion Revealed by Longitudinal Doppler Optical Coherence Tomography and Angiography. J. Cereb. Blood Flow Metab. 2015, 35, 1552–1560. [CrossRef]
- Mansour, A.; Niizuma, K.; Rashad, S.; Sumiyoshi, A.; Ryoke, R.; Endo, H.; Endo, T.; Sato, K.; Kawashima, R.; Tominaga, T. A refined model of chronic cerebral hypoperfusion resulting in cognitive impairment and a low mortality rate in rats. J. Neurosurg. 2019, 131, 892–902. [CrossRef]
- Choi, B.-R.; Lee, S.R.; Han, J.-S.; Woo, S.-K.; Kim, K.M.; Choi, D.-H.; Kwon, K.J.; Han, S.-H.; Shin, C.Y.; Lee, J.; et al. Synergistic Memory Impairment Through the Interaction of Chronic Cerebral Hypoperfusion and Amlyloid Toxicity in a Rat Model. Stroke 2011, 42, 2595–2604. [CrossRef]
- Kalaria, R.N. Vascular basis for brain degeneration: faltering controls and risk factors for dementia. Nutr. Rev. 2010, 68, S74–S87. [CrossRef]
- Si, Z.; Fan, X. Research Progress on the Relationship between Vascular Aging and Hypertension. Proc. Anticancer. Res. 2021, 5, 91–93. [CrossRef]
- Buford, T. W. (2016). Hypertension and aging. Ageing Research Reviews, 26, 96-111.
- Lionakis, N. (2012). Hypertension in the elderly. World Journal of Cardiology, 4(5), 135.
- Afari, M.E.; Wylie, J.V.; Carrozza, J.P. Refractory Hypotension as an Initial Presentation of Bilateral Subclavian Artery Stenosis. Case Rep. Cardiol. 2016, 2016, 1–3. [CrossRef]
- Fatmawati, S.M.Y.; Watik, K.L.; Abdillah, A. The Reduction of Blood Pressure in Elderly People with Hypertension Through Morning Walk Therapy. J. Nurs. Pr. 2024, 7, 262–269. [CrossRef]
- Salwa, P.; Gorczyca-Michta, I.; Kluk, M.; Dziubek, K.; Wożakowska-Kapłon, B. Variability of circadian blood pressure profile during 24-hour ambulatory blood pressure monitoring in hypertensive patients. Kardiologia Polska 2014, 72, 432–437. [CrossRef]
- García, J., Águila, F., Torres, C., Extremera, B., & Alonso, J. (2012). Ambulatory Blood Pressure Monitoring in the Elderly. International Journal of Hypertension, 2012, 1-8.
- Pimenta, E. and Oparil, S. (2012). Management of hypertension in the elderly. Nature Reviews Cardiology, 9(5), 286-296.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).