Submitted:
09 September 2025
Posted:
10 September 2025
You are already at the latest version
Abstract
Background: As a noble and extremely sensitive organ, particularly during in utero development, the brain has intrinsic systems to reduce the risk of cerebral damage in cases of insult, such as energy deprivation, due to a mechanism of positive balance in cerebral oxygen–energy substrate demand and supply. This mechanism is called cerebral autoregulation and is present in both the fetal and adult brain. The inaccessibility of the fetal brain to currently available measurement techniques limits its knowledge. Physiological and pathological alterations of fetal cerebral blood flow (CBF) can be assessed during the latter half of pregnancy using sonographic Doppler studies. The limited studies on this subject suggest a potential role for Doppler assessment of the fetal internal carotid artery. Objective: This article reviews the concept of CBF autoregulation and the role of fetal Doppler studies in various brain vascular territories in clinical practice. Methods: A PubMed search was performed, and 156 English articles were used as references in this bibliographic review, published between January 1996 and December 2021. Results: The study of fetal CBF involves indirect observation; the fetal brain constantly changes its characteristics towards complete maturation, which will be fully accomplished only after birth; and the maternal environment influences this process. Conclusion: Doppler study of the internal cerebral artery might be useful in clinical practice. However, technical issues for its study are not established, there are no reference curves, and studies on its clinical value have limited applicability.
Keywords:
1. Introduction
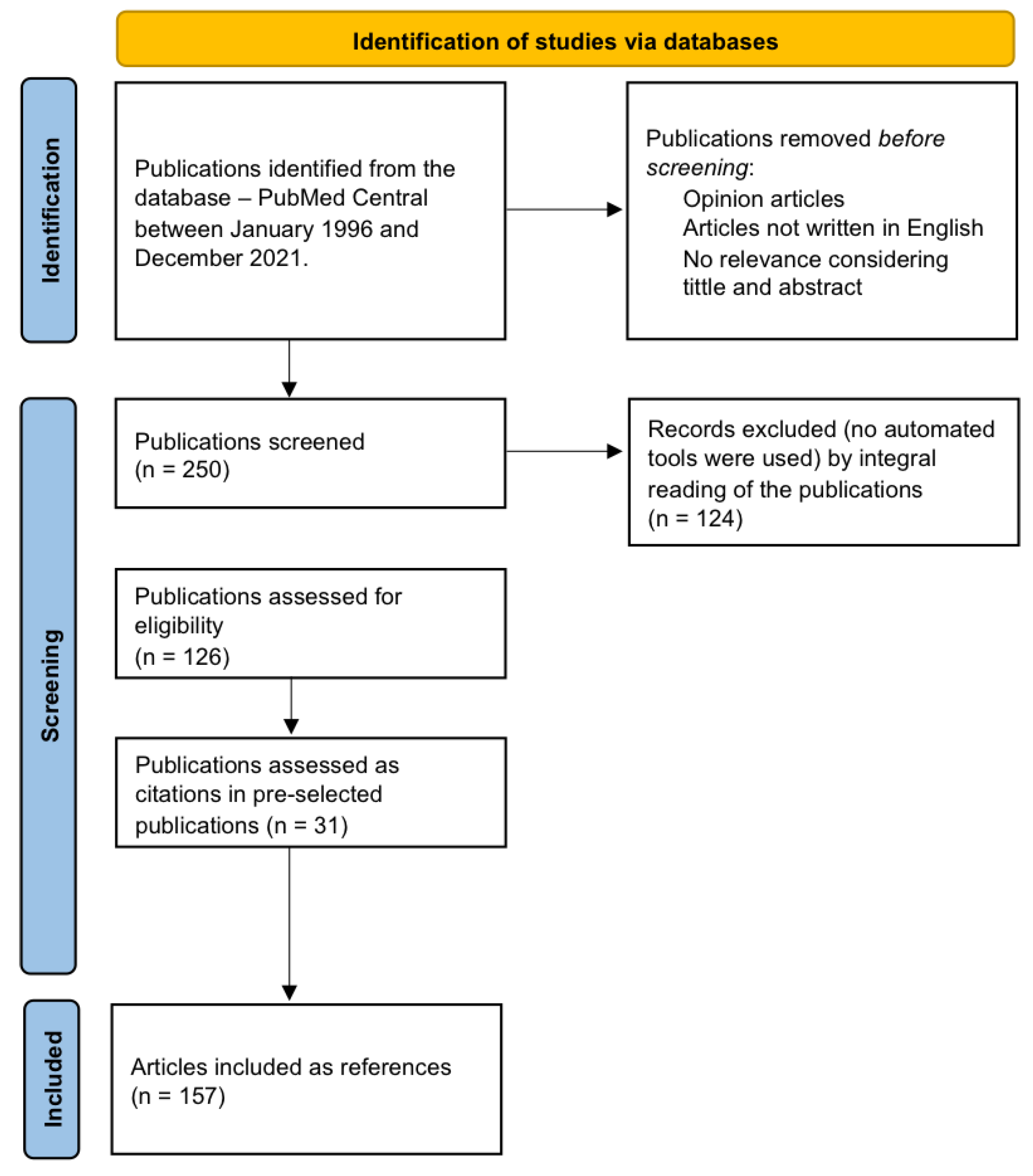
2. Materials and Methods
3. The Fetal Cerebral Circulation
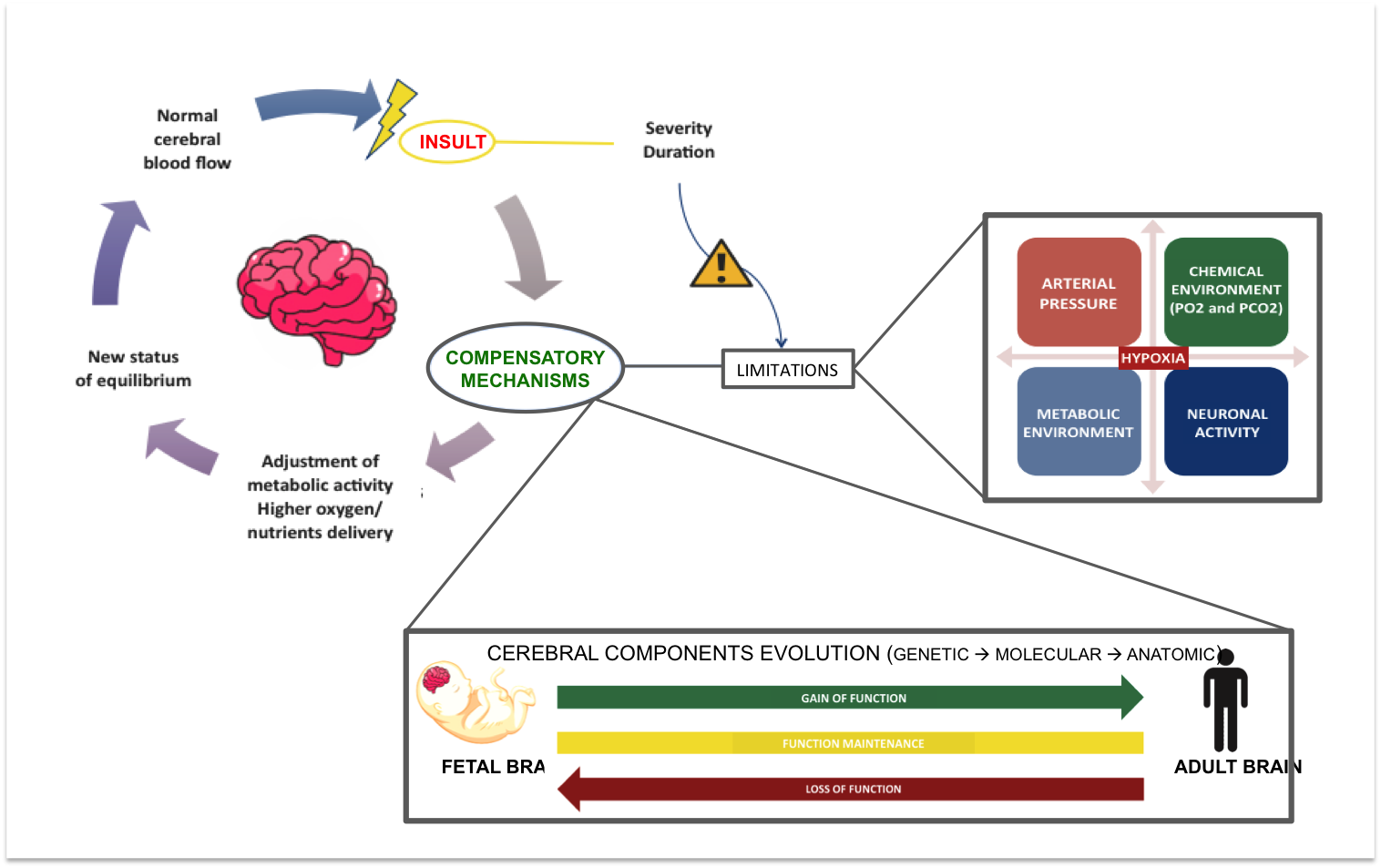
3.1. Fetal Cerebral Autoregulation
3.2. The Effects of Hypoxia on Fetal Cerebral Structure and Function
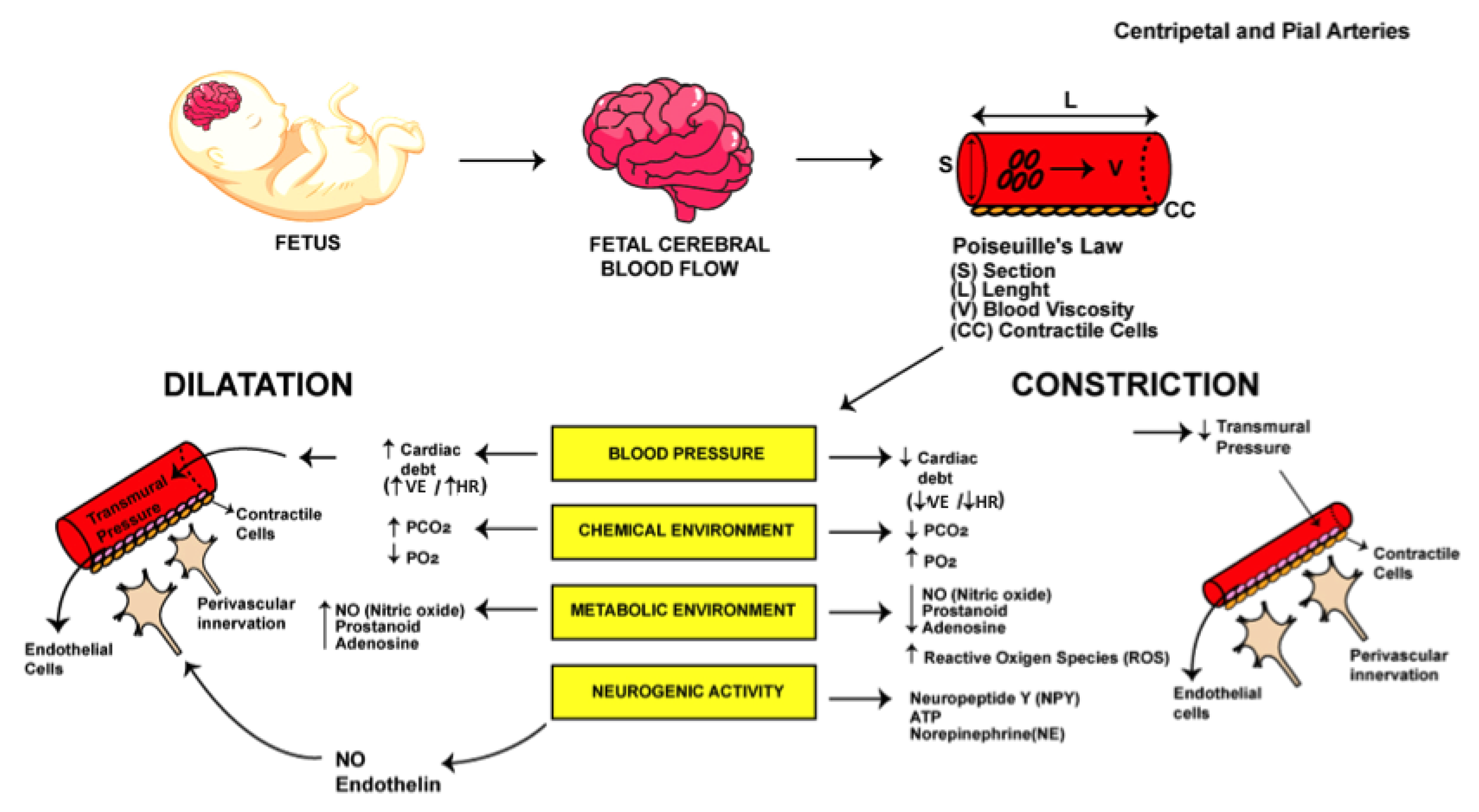
3.3. Contractile Characteristics of Fetal Cerebrovasculature
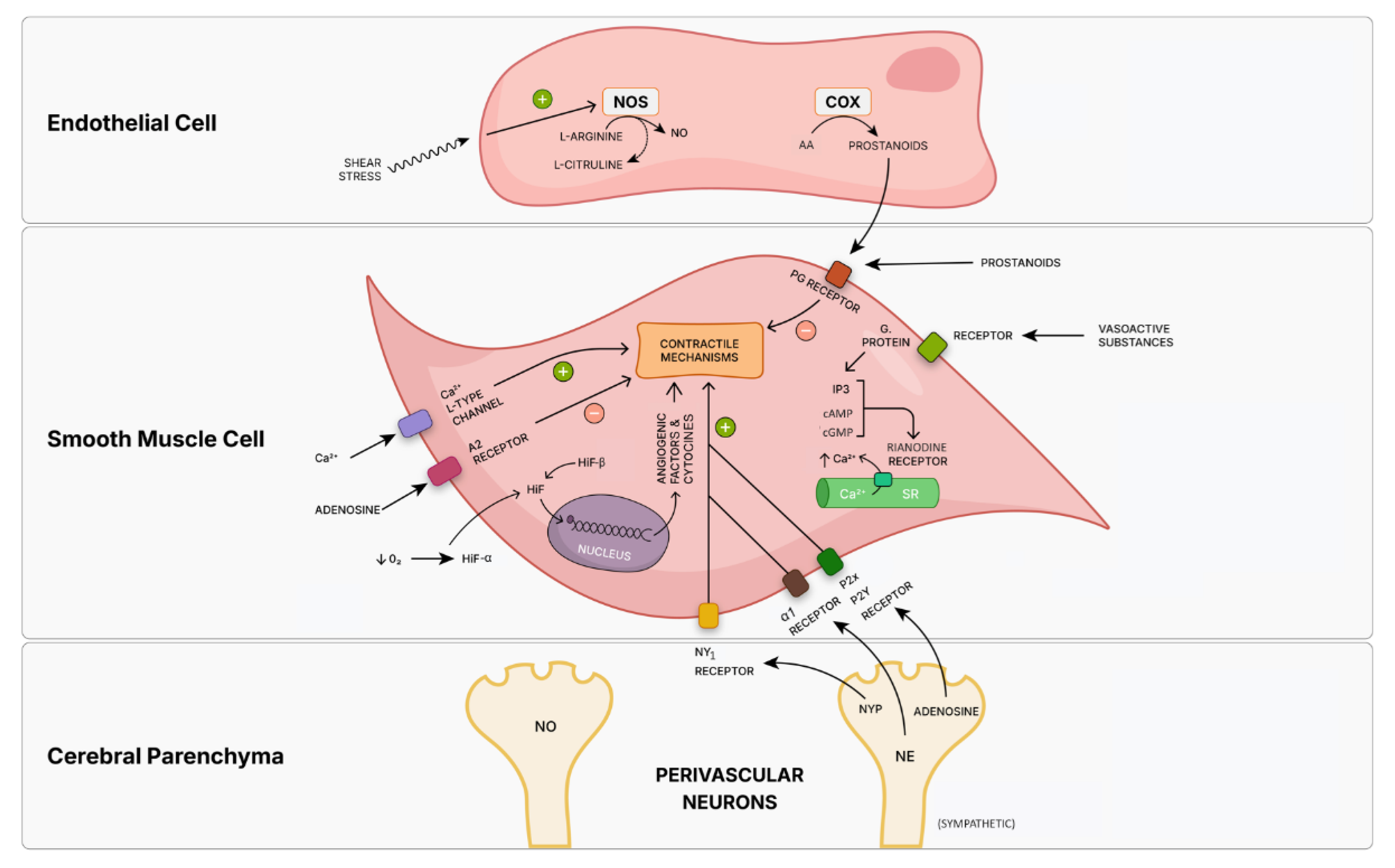
3.4. Fetal Cerebrovascular Signal Transduction
3.4.1. Calcium
3.4.2. Nitric Oxide and Prostaglandins
3.4.3. Adenosine
3.4.4. Reactive Oxygen Species
3.4.5. Hypoxic Inducible Factor-1
3.4.6. Neurovascular Unit and Its Effectors
3.5. Fetal Carotid Arteries Maturation
3.6. The Concept of Fetal Cerebral Blood Flow Redistribution
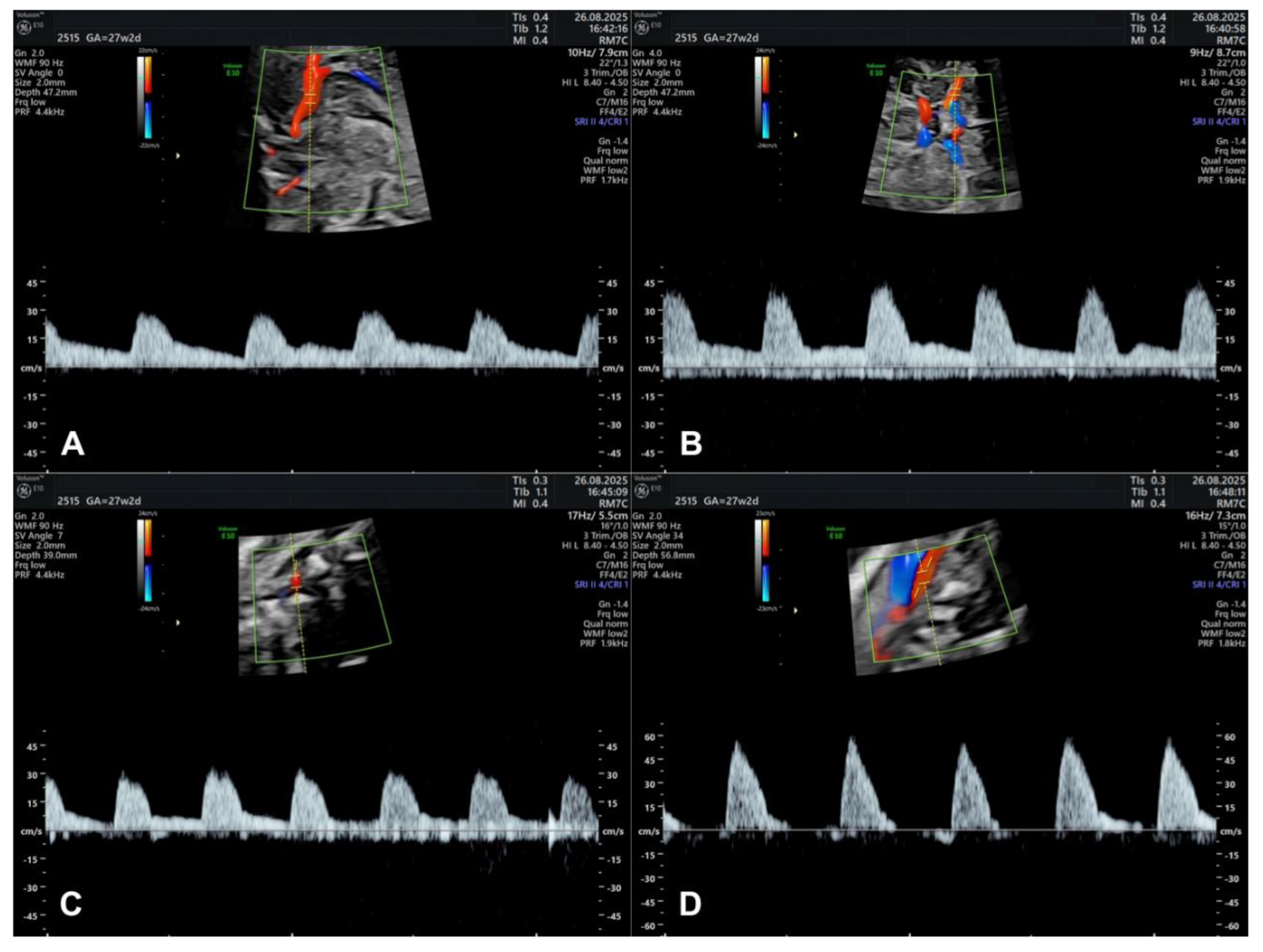
3.7. Doppler Studies of Foetal Cerebral Blood Flow
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 5-HT | Serotonin |
| AA | Arachinoid acid |
| ANGII | Angiotensin II |
| ATP | Adenosine triphosphate |
| Ca2+ | Calcium |
| cAMP | Cyclic adenosine monophosphate |
| CBF | Cerebral blood flow |
| CC | Contractile cells |
| cGMP | Cyclic guanosine monophosphate |
| CO2 | Carbon dioxide |
| COX | Cyclo-oxygenase |
| EEG | Electroencephalogram |
| EPO | Erythropoietin |
| EV | Ejection volume |
| FGF | Fibroblast growth factor |
| FLNA | Filamin isoform A |
| FLNB | Filamin isoform B |
| FBP1 | Formin binding protein 1 |
| HIF | Hypoxia inducible factor |
| HIF-1α | Hypoxia inducible factor 1-alfa |
| HIF-1β | Hypoxia inducible factor 1-beta |
| HR | Heart rate |
| ICA | Internal carotid artery |
| ICAs | Internal carotid arteries |
| ISUOG | International Society of Ultrasound in Obstetric and Gynecology Guidelines |
| IP3 | Inositol-1,4,5-trisphosphate |
| K+ | Potassium |
| L | Length |
| MCA | Middle cerebral artery |
| MLC | Myosin Light chain |
| MLCK | Myosin light chain kinase |
| mRNA | Messenger riboucleic-acid |
| Na/K-ATPase | Sodium-potassium adenosine triphosphate desidrogenase |
| NE | Norepinephrine |
| NO | Nitric oxide |
| NOS | Nitric oxide synthase |
| NPY | Neuropeptide |
| pCO2 | Carbone dioxide arterial partial pressure |
| PDGF | Platelet derived growth factor |
| PI | Pulsatility index |
| pO2 | Oxygen arterial partial pressure |
| PG | Prostaglandin |
| ROS | Reactive oxygen species |
| S | Section |
| SR | Sarcoplasmic reticulum |
| US | Ultrasound |
| V | Blood viscosity |
| VEGF | Vascular endothelial growth factor |
References
- Bueno, D.; Parvas, M.; Garcia-Fernàndez, J. The embryonic bloodcerebrospinal fluid barrier function before the formation of the fetal choroid plexus: Role in cerebrospinal fluid formation and homeostasis. Croat Med J 2014, 55, 306–316. [Google Scholar] [CrossRef]
- Bueno, D.; Parvas, M.; Nabiuni, M.; Miyan, J. Embryonic cerebrospinal fluid formation and regulation. Semin Cell Dev Biol 2020, 102, 3–12. [Google Scholar] [CrossRef]
- Vasung, L.; Abaci Turk, E.; Ferradal, S.L.; Sutin, J.; Stout, J.N.; Ahtam, B.; et al. Exploring early human brain development with structural and physiological neuroimaging. Neuroimage 2019, 187, 226–254. [Google Scholar] [CrossRef]
- du Plessis, A.J. Cerebral Blood Flow and Metabolism in the Developing Fetus. Clin Perinatol 2009, 36, 531–548. [Google Scholar] [CrossRef]
- Lemire, R.J.; Loeser, J.D.L.R. Cerebral vasculature. In: Normal and Abnormal Development of The Human Nervous System. 1975. p. 1–42.
- Degani, S. Fetal cerebrovascular circulation: A review of prenatal ultrasound assessment. Gynecol Obstet Invest 2008, 66, 184–196. [Google Scholar] [CrossRef]
- Rudolph, A.M. Impaired cerebral development in fetuses with congenital cardiovascular malformations: Is it the result of inadequate glucose supply? Pediatr Res 2016, 80, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Nagaraj, U.D.; Evangelou, I.E.; Donofrio, M.T.; Vezina, L.G.; McCarter, R.; Du Plessis, A.J.; et al. Impaired global and regional cerebral perfusion in newborns with complex congenital heart disease. J Pediatr 2015, 167, 1018–1024. [Google Scholar] [CrossRef]
- Sam, C.; Li, F.F.; Liu, S.L. Inherited neurovascular diseases affecting cerebral blood vessels and smooth muscle. Metab Brain Dis 2015, 30, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- McQuillen, P.S.; Miller, S.P. Congenital heart disease and brain development. Ann N Y Acad Sci 2010, 1184, 68–86. [Google Scholar] [CrossRef] [PubMed]
- Dupin, E.; Le Douarin, N.M. The neural crest, A multifaceted structure of the vertebrates. Birth Defects Res Part C - Embryo Today Rev 2014, 102, 187–209. [Google Scholar] [CrossRef]
- Wu, H.M.; Chuang, Y.M. The clinical relevance of fetal variant of the circle of willis and its influence on the cerebral collateral circulation. Acta Neurol Taiwan 2011, 20, 232–242. [Google Scholar]
- Rees, S.; Harding, R.; Inder, T. The developmental environment and the origins of neurological disorders. Dev Orig Heal Dis 2006, 379–391. [Google Scholar]
- Rasmussen, J.M.; Thompson, P.M.; Entringer, S.; Buss, C.; Wadhwa, P.D. Fetal programming of human energy homeostasis brain networks: Issues and considerations. Obes Rev 2022, 23, 1–27. [Google Scholar] [CrossRef]
- Limperopoulos, C. Disorders of the Fetal Circulation and the Fetal Brain. Clin Perinatol 2009, 36, 561–577. [Google Scholar] [CrossRef]
- Tweed, W.A.; Cote, J.; Wade, J.G.; Gregory, G.; Mills, A. Preservation of fetal brain blood flow relative to other organs during hypovolemic hypotension. Pediatr Res 1982, 16, 137–140. [Google Scholar] [CrossRef]
- Löhle, M.; Müller, T.; Wicher, C.; Roedel, M.; Schubert, H.; Witte, O.W.; et al. Betamethasone effects on fetal sheep cerebral blood flow are not dependent on maturation of cerebrovascular system and pituitary-adrenal axis. J Physiol 2005, 564, 575–588. [Google Scholar] [CrossRef]
- Hernandez-Andrade, E.; Benavides Serralde, J.A.; Cruz-Martinez, R. Can anomalies of fetal brain circulation be useful in the management of growth restricted fetuses? Prenat Diagn 2012, 32, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Andrade, E.; Stampalija, T.; Figueras, F. Cerebral blood flow studies in the diagnosis and management of intrauterine growth restriction. Curr Opin Obstet Gynecol 2013, 25, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Bukiya, A.N.; Dopico, A.M. Fetal cerebral circulation as target of maternal alcohol consumption. 2019, 42, 1006–1018. [Google Scholar] [CrossRef]
- Bar, J.; Weiner, E.; Levy, M.; Gilboa, Y. The thrifty phenotype hypothesis: The association between ultrasound and Doppler studies in fetal growth restriction and the development of adult disease. Am J Obstet Gynecol MFM 2021, 3, 100473. [Google Scholar] [CrossRef]
- Mihu, D.; Diculescu, D.; Costin, N.; Mihu, C.M.; Blaga, L.; Ciortea, R.; et al. Applications of Doppler ultrasound during labor. Med Ultrason 2011, 13, 141–149. [Google Scholar]
- Kawakita, T.; Sasaki, H.; Hirabuki, S.; Asamoto, A. Fetal growth restriction and reversed middle cerebral artery end-diastolic flow with subchorionic placental lake. J Obstet Gynaecol Res 2013, 39, 578–582. [Google Scholar] [CrossRef] [PubMed]
- Nassr, A.A.; Abdelmagied, A.M.; Shazly, S.A.M. Fetal cerebro-placental ratio and adverse perinatal outcome: Systematic review and meta-analysis of the association and diagnostic performance. J Perinat Med 2016, 44, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Hershkovitz, R.; Kingdom, J.C.P.; Geary, M.; Rodeck, C.H. Fetal cerebral blood flow redistribution in late gestation: Identification of compromise in small fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol 2000, 15, 209–212. [Google Scholar] [CrossRef]
- Wolf, H.; Stampalija, T.; Lees, C.C.; Arabin, B.; Berger, A.; Bergman, E.; et al. Fetal cerebral blood-flow redistribution: analysis of Doppler reference charts and association of different thresholds with adverse perinatal outcome. Ultrasound Obstet Gynecol 2021, 58, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Back, S.A.; Riddle, A.; Dean, J.; Hohimer, A.R. The Instrumented Fetal Sheep as a Model of Cerebral White Matter Injury in the Premature Infant. Neurotherapeutics 2012, 9, 359–370. [Google Scholar] [CrossRef]
- Sinha, A.K.; Cane, C.; Kempley, S.T. Blood flow in the common carotid artery in term and preterm infants: Reproducibility and relation to cardiac output. Arch Dis Child Fetal Neonatal Ed 2006, 91, 31–35. [Google Scholar] [CrossRef]
- van den Wijngaard, J.A.G.W.; Reuss, A.; Wladimiroff, J.W. The blood flow velocity waveform in the fetal internal carotid artery in the presence of hydrocephaly. Early Hum Dev 1988, 18, 95–99. [Google Scholar] [CrossRef]
- Cohen, E.; Baerts, W.; Van Bel, F. Brain-Sparing in Intrauterine Growth Restriction: Considerations for the Neonatologist. Neonatology 2015, 108, 269–276. [Google Scholar] [CrossRef]
- Robinson, R.; Iida, H.; O’Brien, T.P.; Pane, M.A.; Traystman, R.J.; Gleason, C.A. Comparison of cerebrovascular effects of intravenous cocaine injection in fetal, newborn, and adult sheep. Am J Physiol - Hear Circ Physiol 2000, 279, 1–6. [Google Scholar] [CrossRef]
- Tarzamni, M.K.; Nezami, N.; Gatreh-Samani, F.; Vahedinia, S.; Tarzamni, M. Doppler waveform indices of fetal middle cerebral artery in normal 20 to 40 weeks pregnancies. Arch Iran Med 2009, 12, 29–34. [Google Scholar] [PubMed]
- Silverman, A.; Petersen, N.H. Physiology, Cerebral Autoregulation. StatPearls [Internet] 2020, 1–8. [Google Scholar] [PubMed]
- Greisen, G. Autoregulation of cerebral blood flow in newborn babies. Early Hum Dev 2005, 81, 423–428. [Google Scholar] [CrossRef]
- Wu, T.W.; Azhibekov, T.; Seri, I. Transitional hemodynamics in preterm neonates: Clinical relevance. Pediatr Neonatol [Internet] 2016, 57, 7–18. [Google Scholar] [CrossRef] [PubMed]
- De Carli, A.; Andresen, B.; Giovannella, M.; Durduran, T.; Contini, D.; Spinelli, L.; et al. Cerebral oxygenation and blood flow in term infants during postnatal transition: BabyLux project. Arch Dis Child Fetal Neonatal Ed 2019, 104, F648–F653. [Google Scholar] [CrossRef]
- Altman, D.I.; Perlman, J.M.; Volpe, J.J.; Powers, W.J. Cerebral oxygen metabolism in newborns. Pediatrics 1993, 92, 99–104. [Google Scholar] [CrossRef]
- Altman, D.I.; Powers, W.J.; Perlman, J.M.; Herscovitch, P.; Volpe, S.L.; Volpe, J.J. Cerebral blood flow requirement for brain viability in newborn infants is lower than in adults. Ann Neurol 1988, 24, 218–226. [Google Scholar] [CrossRef]
- Giussani, D.A.; Niu, Y.; Herrera, E.A.; Richter, H.G.; Camm, E.J.; Thakor, A.S.; et al. The Fetal Cerebral Circulation: Three Decades of Exploration by the LLU Center for Perinatal Biology. Adv Exp Med Biol [Internet] 2014, 814, 77–87. [Google Scholar] [CrossRef]
- Bishai, J.M.; Blood, A.B.; Hunter, C.J.; Longo, L.D.; Power, G.G. Fetal lamb cerebral blood flow (CBF) and oxygen tensions during hypoxia: A comparison of laser Doppler and microsphere measurements of CBF. J Physiol 2003, 546, 869–878. [Google Scholar] [CrossRef]
- RCVannucci, M.J.H. Perinatal cerebral blood flow. Mead Johnson Symp Perinat Dev Med [Internet] 1980, 17, 17–29. [Google Scholar]
- Tweed, W.A.; Pash, M.; Doig, G. Cerebrovascular mechanisms in perinatal asphyxia: The role of vasogenic brain edema. Pediatr Res 1981, 15, 44–46. [Google Scholar] [CrossRef]
- Jones, M.D.; Travstman, R.J. Cerebral oxygenation of the fetus, newborn, and adult. Semin Perinatol [Internet] 1984, 8, 205–216. [Google Scholar]
- Greisen, G. Autoregulation of Cerebral Blood Flow in the Preterm Fetal Lamb. Early Hum Dev 2005, 81, 423–428. [Google Scholar] [CrossRef]
- Jaiswal, P.; Upadhyay, A.; Gothwal, S.; Chaudhary, H.; Tandon, A. Comparison of Umbilical Cord Milking and Delayed Cord Clamping on Cerebral Blood Flow in Term Neonates. Indian J Pediatr 2015, 82, 890–895. [Google Scholar] [CrossRef] [PubMed]
- Katheria, A.C.; Szychowski, J.M.; Essers, J.; Mendler, M.R.; Dempsey, E.M.; Schmölzer, G.M.; et al. Early Cardiac and Cerebral Hemodynamics with Umbilical Cord Milking Compared with Delayed Cord Clamping in Infants Born Preterm. J Pediatr 2020, 223, 51–56.e1. [Google Scholar] [CrossRef] [PubMed]
- Kooi, E.M.W.; Richter, A.E. Cerebral Autoregulation in Sick Infants: Current Insights. Clin Perinatol [Internet] 2020, 47, 449–467. [Google Scholar] [CrossRef] [PubMed]
- Peyvandi, S.; Donofrio, M.T. Circulatory Changes and Cerebral Blood Flow and Oxygenation During Transition in Newborns With Congenital Heart Disease. Semin Pediatr Neurol [Internet] 2018, 28, 38–47. [Google Scholar] [CrossRef]
- Hahn, G.H.; Maroun, L.L.; Larsen, N.; Hougaard, D.M.; Sorensen, L.C.; Lou, H.C.; et al. Cerebral autoregulation in the first day after preterm birth: No evidence of association with systemic inflammation. Pediatr Res 2012, 71, 253–260. [Google Scholar] [CrossRef]
- Noori, S.; Seri, I. Hemodynamic antecedents of peri/intraventricular hemorrhage in very preterm neonates. Semin Fetal Neonatal Med [Internet] 2015, 20, 232–237. [Google Scholar] [CrossRef]
- Wu, T.W.; Tamrazi, B.; Soleymani, S.; Seri, I.; Noori, S. Hemodynamic Changes During Rewarming Phase of Whole-Body Hypothermia Therapy in Neonates with Hypoxic-Ischemic Encephalopathy. J Pediatr [Internet] 2018, 197, 68–74.e2. [Google Scholar] [CrossRef]
- Binder-Heschl, C.; Urlesberger, B.; Schwaberger, B.; Koestenberger, M.; Pichler, G. Borderline hypotension: How does it influence cerebral regional tissue oxygenation in preterm infants? J Matern Neonatal Med 2016, 29, 2341–2346. [Google Scholar] [CrossRef]
- Noori, S.; Anderson, M.; Soleymani, S.; Seri, I. Effect of carbon dioxide on cerebral blood flow velocity in preterm infants during postnatal transition. Acta Paediatr Int J Paediatr 2014, 103, 334–339. [Google Scholar] [CrossRef]
- Wyatt, J. Cerebral oxygenation and haemodynamics in the foetus and newborn infant. Philos Trans R Soc B Biol Sci 1997, 352, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Tortora, D.; Severino, M.; Rossi, A. Arterial spin labeling perfusion in neonates. Semin Fetal Neonatal Med [Internet] 2020, 25, 101130. [Google Scholar] [CrossRef]
- Richardson, B.S.; Carmichael, L.; Homan, J.; Patrick, J.E. Electrocortical activity, electroocular activity, and breathing movements in fetal sheep with prolonged and graded hypoxemia. American Journal of Obstetrics and Gynecology 1992, 167, 553–558. [Google Scholar] [CrossRef]
- Ashwal, S.; Majcher, J.S.; Longo, L.D. Patterns of fetal lamb regional cerebral blood flow during and after prolonged hypoxia: Studies during the posthypoxic recovery period. Am J Obstet Gynecol 1981, 139, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Park, M.K.; Kuehl, T.J. Relaxant and contractile responses to prostaglandins in premature, newborn and adult baboon cerebral arteries. J Pharmacol Exp Ther 1985, 233, 628–635. [Google Scholar] [CrossRef]
- Pearce, W.J.; Ashwal, S. Developmental changes in thickness, contractility, and hypoxic sensitivity of newborn lamb cerebral arteries. Pediatr Res 1987, 22, 192–196. [Google Scholar] [CrossRef]
- Scher, M.S. Normal and abnormal cerebrovascular development: Gene-environment interactions during early life with later life consequences [Internet]. 1st ed. Vol. 112, Handbook of Clinical Neurology. Elsevier B.V.; 2013. 1021–1042. [CrossRef]
- Xing, C.Y.; Tarumi, T.; Liu, J.; Zhang, Y.; Turner, M.; Riley, J.; et al. Distribution of cardiac output to the brain across the adult lifespan. J Cereb Blood Flow Metab 2017, 37, 2848–2856. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.R.; Leggett, R.W. Reference values for resting blood flow to organs of man. Clin Phys Physiol Meas 1989, 10, 187–217. [Google Scholar] [CrossRef]
- Northington, F.J.; Tobin, J.R.; Harris, A.P.; Traystman, R.J.; Koehler, R.C. Developmental and regional differences in nitric oxide synthase activity and blood flow in the sheep brain. J Cereb Blood Flow Metab 1997, 17, 109–115. [Google Scholar] [CrossRef]
- El-Dib, M.; Soul, J.S. Monitoring and management of brain hemodynamics and oxygenation [Internet]. 1st ed. Vol. 162, Handbook of Clinical Neurology. Elsevier B.V.; 2019, 295–314. [CrossRef]
- Akundi, R.S.; Rivkees, S.A. Hypoxia alters cell cycle regulatory protein expression and induces premature maturation of oligodendrocyte precursor cells. PLoS One 2009, 4. [Google Scholar] [CrossRef] [PubMed]
- Low, J.A. Intrapartum fetal asphyxia: Definition, diagnosis, and classification. Am J Obstet Gynecol 1997, 176, 957–959. [Google Scholar] [CrossRef] [PubMed]
- Pearce, W. Hypoxic regulation of the fetal cerebral circulation. J Appl Physiol 2006, 100, 731–738. [Google Scholar] [CrossRef]
- Fahey, J.; King, T.L. Intrauterine asphyxia: Clinical implications for providers of intrapartum care. J Midwifery Women’s Heal 2005, 50, 498–506. [Google Scholar] [CrossRef]
- Rudolph, A.M. Circulatory changes during gestational development of the sheep and human fetus. Pediatr Res 2018, 84, 348–351. [Google Scholar] [CrossRef]
- Rudolph, A.M. Cerebral glucose deficiency versus oxygen deficiency in neonatal encephalopathy. J Neonatal Perinatal Med 2018, 11, 115–120. [Google Scholar] [CrossRef]
- Hüppi, P.S.; Warfield, S.; Kikinis, R.; Barnes, P.D.; Zientara, G.P.; Jolesz, F.A.; et al. Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann Neurol 1998, 43, 224–235. [Google Scholar] [CrossRef]
- Yadav, B.K.; Hernandez-Andrade, E.; Krishnamurthy, U.; Buch, S.; Jella, P.; Trifan, A.; et al. Dual-Imaging Modality Approach to Evaluate Cerebral Hemodynamics in Growth-Restricted Fetuses: Oxygenation and Perfusion. Fetal Diagn Ther 2020, 47, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Wolfberg, A.J.; du Plessis, A.J. Near-Infrared Spectroscopy in the Fetus and Neonate. Clin Perinatol 2006, 33, 707–728. [Google Scholar] [CrossRef]
- Segovia, K.N.; Mcclure, M.; Moravec, M.; Luo, N.L.; Wan, Y.; Gong, X.; et al. Arrested Oligodendrocyte Lineage Maturation in. Ann Neurol 2008, 63, 520–530. [Google Scholar] [CrossRef]
- Fan, X.; Heijnen, C.J.; van der Kooij, M.A.; Groenendaal, F.; van Bel, F. The role and regulation of hypoxia-inducible factor-1α expression in brain development and neonatal hypoxic-ischemic brain injury. Brain Res Rev [Internet] 2009, 62, 99–108. [Google Scholar] [CrossRef]
- Alonso-Spilsbury, M.; Mota-Rojas, D.; Villanueva-García, D.; Martínez-Burnes, J.; Orozco, H.; Ramírez-Necoechea, R.; et al. Perinatal asphyxia pathophysiology in pig and human: A review. Anim Reprod Sci 2005, 90, 1–30. [Google Scholar] [CrossRef]
- Tomimatsu, T.; Kakigano, A.; Mimura, K.; Kanayama, T.; Koyama, S.; Fujita, S.; et al. Maternal carbon dioxide level during labor and its possible effect on fetal cerebral oxygenation: Mini review. J Obstet Gynaecol Res 2013, 39, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, A.M. Maternal hyperoxygenation for the human fetus: should studies be curtailed? Pediatr Res [Internet] 2020, 87, 630–633. [Google Scholar] [CrossRef]
- Tomimatsu, T.; Pereyra Peňa, J.; Hatran, D.P.; Longo, L.D. Maternal oxygen administration and fetal cerebral oxygenation: Studies on near-term fetal lambs at both low and high altitude. Am J Obstet Gynecol 2006, 195, 535–541. [Google Scholar] [CrossRef]
- Müller, J.J.; Antonow-Schlorke, I.; Kroegel, N.; Rupprecht, S.; Rakers, F.; Witte, O.W.; et al. Cardiovascular effects of prenatal stress—Are there implications for cerebrovascular, cognitive and mental health outcome? Neurosci Biobehav Rev [Internet] 2020, 117, 78–97. [Google Scholar] [CrossRef] [PubMed]
- Nathaniel, T.I. Brain-regulated metabolic suppression during hibernation: A neuroprotective mechanism for perinatal hypoxia-ischemia. Int J Stroke 2008, 3, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Pourcyrous, M. Cerebral hemodynamic measurements in acute versus chronic asphyxia. Clinics in Perinatology 1999, 26, 811–28. [Google Scholar] [CrossRef]
- Longo, L.D.; Pearce, W.J. High altitude, hypoxic-induced modulation of noradrenergic-mediated responses in fetal and adult cerebral arteries. Comp Biochem Physiol A Mol Integr Physiol 1998, 119, 683–694. [Google Scholar] [CrossRef]
- Rakers, F.; Rupprecht, S.; Dreiling, M.; Bergmeier, C.; Witte, O.W.; Schwab, M. Transfer of maternal psychosocial stress to the fetus. Neurosci Biobehav Rev 2020, 117, 185–197. [Google Scholar] [CrossRef]
- McMillen, I.C.; Robinson, J.S. Developmental origins of the metabolic syndrome: Prediction, plasticity, and programming. Physiol Rev 2005, 85, 571–633. [Google Scholar] [CrossRef] [PubMed]
- Weinstock, M. Gender differences in the effects of prenatal stress on brain development and behaviour. Neurochem Res 2007, 32, 1730–1740. [Google Scholar] [CrossRef] [PubMed]
- Anwar, M.A.; Schwab, M.; Poston, L.; Nathanielsz, P.W. Betamethasone-mediated vascular dysfunction and changes in hematological profile in the ovine fetus. Am J Physiol - Hear Circ Physiol 1999, 276, 1137–1143. [Google Scholar] [CrossRef]
- Malhotra, A.; Ditchfield, M.; Fahey, M.C.; Castillo-Melendez, M.; Allison, B.J.; Polglase, G.R.; et al. Detection and assessment of brain injury in the growth-restricted fetus and neonate. Pediatr Res 2017, 82, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Dabertrand, F.; Nelson, M.T.; Brayden, J.E. Acidosis dilates brain parenchymal arterioles by conversion of calcium waves to sparks to activate BK channels. Circ Res 2012, 110, 285–294. [Google Scholar] [CrossRef]
- Niño Cruz, G.I.; Ramirez Varela, A.; da Silva, I.C.M.; Hallal, P.C.; Santos, I.S. Physical activity during pregnancy and offspring neurodevelopment: A systematic review. Paediatr Perinat Epidemiol 2018, 32, 369–379. [Google Scholar] [CrossRef]
- Antonow-Schlorke, I.; Schwab, M.; Cox, L.A.; Li, C.; Stuchlik, K.; Witte, O.W.; et al. Vulnerability of the fetal primate brain to moderate reduction in maternal global nutrient availability. Proc Natl Acad Sci USA 2011, 108, 3011–3016. [Google Scholar] [CrossRef]
- Colberg, C.; Antonow-Schlorke, I.; Müller, T.; Schubert, H.; Witte, O.W.; Schwab, M. Recovery of glucocorticoid-related loss of synaptic density in the fetal sheep brain at 0.75 of gestation. Neurosci Lett 2004, 364, 130–134. [Google Scholar] [CrossRef]
- Schwab, M.; Schmidt, K.; Roedel, M.; Mueller, T.; Schubert, H.; Akthar Anwar, M.; et al. Non-linear changes of electrocortical activity after antenatal betamethasone treatment in fetal sheep. J Physiol 2001, 531, 535–543. [Google Scholar] [CrossRef]
- Salihagić-Kadić, A.; Medić, M.; Jugović, D.; Kos, M.; Latin, V.; Jukić, M.K.; et al. Fetal cerebrovascular response to chronic hypoxia - Implications for the prevention of brain damage. J Matern Neonatal Med 2006, 19, 387–396. [Google Scholar] [CrossRef]
- Korček, P.; Širc, J.; Straňák, Z. Cerebral oxygenation reflects fetal development in preterm monochorionic and dichorionic twins. Early Hum Dev [Internet] 2020, 144, 105025. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.L.; Huppi, P.S.; Mallard, C. The consequences of fetal growth restriction on brain structure and neurodevelopmental outcome. J Physiol 2016, 594, 807–823. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Fu, W.; Liu, J. Neurodevelopment in children with intrauterine growth restriction: Adverse effects and interventions. J Matern Neonatal Med 2016, 29, 660–668. [Google Scholar] [CrossRef]
- Longo, L.; Goyal, R. Cerebral Artery Signal Transduction Mechanisms: Developmental Changes in Dynamics and Ca2+ Sensitivity. Curr Vasc Pharmacol 2013, 11, 655–711. [Google Scholar] [CrossRef] [PubMed]
- Kuban, K.C.; Gilles, F.H. Human telencephalic angiogenis. Ann Neurol 1985, 17, 539–548. [Google Scholar] [CrossRef]
- Nelson, K.B.; Leviton, A. How Much of Neonatal Encephalopathy Is due to Birth Asphyxia? Am J Dis Child 1991, 145, 1325–1331. [Google Scholar] [CrossRef]
- Boegehold, M.A. Endothelium-dependent control of vascular tone during early postnatal and juvenile growth. Microcirculation 2010, 17, 394–406. [Google Scholar] [CrossRef]
- Goyal, R.; Mittal, A.; Chu, N.; Arthur, R.A.; Zhang, L.; Longo, L.D. Maturation and long-term hypoxia-induced acclimatization responses in PKC-mediated signaling pathways in ovine cerebral arterial contractility. Am J Physiol - Regul Integr Comp Physiol 2010, 299. [Google Scholar] [CrossRef]
- Longo, L.D.; Pearce, W.J. Fetal cerebrovascular acclimatization responses to high-altitude, long-term hypoxia: A model for prenatal programming of adult disease? Am J Physiol Regul Integr Comp Physiol 2005, 288, 16–25. [Google Scholar] [CrossRef]
- Nauli, S.M.; Williams, J.M.; Akopov, S.E.; Zhang, L.; Pearce, W.J. Developmental changes in ryanodine- and IP3-sensitive Ca2+ pools in ovine basilar artery. Am J Physiol Cell Physiol 2001, 281. [Google Scholar] [CrossRef] [PubMed]
- Long, W.; Zhang, L.; Longo, L.D. Cerebral artery sarcoplasmic reticulum Ca2+ stores and contractility: Changes with development. Am J Physiol Regul Integr Comp Physiol 2000, 279, 860–873. [Google Scholar] [CrossRef]
- Adeoye, O.O.; Silpanisong, J.; Williams, J.M.; Pearce, W.J. Role of the sympathetic autonomic nervous system in hypoxic remodeling of the fetal cerebral vasculature. J Cardiovasc Pharmacol 2015, 65, 308–316. [Google Scholar] [CrossRef]
- Tao, X.; Lin, M.T.; Thorington, G.U.; Wilson, S.M.; Longo, L.D.; Hessinger, D.A. Long-term hypoxia increases calcium affinity of bk channels in ovine fetal and adult cerebral artery smooth muscle. Am J Physiol Hear Circ Physiol 2015, 308, 707–722. [Google Scholar] [CrossRef]
- Behringer, E.J.; Leite, L.D.; Buchholz, N.E.; Keeney, M.G.; Pearce, W.J.; Vanterpool, C.K.; et al. Maturation and long-term hypoxia alters Ca2+-induced Ca 2+ release in sheep cerebrovascular sympathetic neurons. J Appl Physiol 2009, 107, 1223–1234. [Google Scholar] [CrossRef]
- Geary, G.G.; Osol, G.J.; Longo, L.D. Development affects in vitro vascular tone and calcium sensitivity in ovine cerebral arteries. J Physiol 2004, 558, 883–896. [Google Scholar] [CrossRef]
- Jenkins, D.D.; Wiest, D.B.; Mulvihill, D.M.; Hlavacek, A.M.; Majstoravich, S.J.; Brown, T.R.; et al. Fetal and Neonatal Effects of N-Acetylcysteine When Used for Neuroprotection in Maternal Chorioamnionitis. J Pediatr [Internet] 2016, 168, 67–76.e6. [Google Scholar] [CrossRef]
- Lee HTe Chang, Y.C.; Wang, L.Y.; Wang, S.T.; Huang, C.C.; Ho, C.J. cAMP response element-binding protein activation in ligation preconditioning in neonatal brain. Ann Neurol 2004, 56, 611–623. [Google Scholar]
- Blood, A.B.; Hunter, C.J.; Power, G.G. Adenosine mediates decreased cerebral metabolic rate and increased cerebral flow during acute moderate hypoxia in the near-term fetal sheep. J Physiol 2003, 553, 935–945. [Google Scholar] [CrossRef]
- Koos, B.J. Adenosine A2a receptors and O2 sensing in development. Am J Physiol Regul Integr Comp Physiol 2011, 301. [Google Scholar]
- Masi, S.; Uliana, M.; Virdis, A. Angiotensin II and vascular damage in hypertension: Role of oxidative stress and sympathetic activation. Vascul Pharmacol [Internet] 2019, 115, 13–17. [Google Scholar] [CrossRef]
- Wood, C.E.; Walker, C.D. Fetal and neonatal HPA axis. Compr Physiol 2016, 6, 33–62. [Google Scholar] [CrossRef]
- Power, M.L.; Schulkin, J. Functions of corticotropin-releasing hormone in anthropoid primates: From brain to placenta. Am J Hum Biol 2006, 18, 431–447. [Google Scholar] [CrossRef]
- Reynolds, R.M. Glucocorticoid excess and the developmental origins of disease: Two decades of testing the hypothesis - 2012 Curt Richter Award Winner. Psychoneuroendocrinology [Internet] 2013, 38, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Salceda, S.; Caro, J. Hypoxia-inducible factor 1α (HIF-1α) protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J Biol Chem 1997, 272, 22642–22647. [Google Scholar] [CrossRef]
- Ke, Q.; Costa, M. Hypoxia-Inducible Factor-1 (HIF-1). 2006, 70, 1469–1480. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. Hypoxia-inducible factor 1 (HIF-1) pathway. Sci STKE 2007, 2007, 9–12. [Google Scholar] [CrossRef]
- Buchholz, J.; Edwards-Teunissen, K.; Duckles, S.P. Impact of development and chronic hypoxia on NE release from adrenergic nerves in sheep arteries. Am J Physiol Regul Integr Comp Physiol 1999, 276. [Google Scholar] [CrossRef]
- Teng, G.Q.; Williams, J.; Zhang, L.; Purdy, R.; Pearce, W.J. Effects of maturation, artery size, and chronic hypoxia on 5-HT receptor type in ovine cranial arteries. Am J Physiol - Regul Integr Comp Physiol 1998, 275, 742–753. [Google Scholar] [CrossRef] [PubMed]
- Carstens, M.H. Development of the facial midline. J Craniofac Surg 2002, 13, 129–187. [Google Scholar] [CrossRef]
- Bertulli, L.; Robert, T. Embryological development of the human cranio-facial arterial system: a pictorial review. Surg Radiol Anat [Internet] 2021, 43, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Platt, M.W.; Deshpande, S. Metabolic adaptation at birth. Semin Fetal Neonatal Med 2005, 10, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Booth, L.C.; Tummers, L.; Jensen, E.C.; Barrett, C.J.; Malpas, S.C.; Gunn, A.J.; et al. Differential effects of the adenosine A1 receptor agonist adenosine amine congener on renal, femoral and carotid vascular conductance in preterm fetal sheep. Clin Exp Pharmacol Physiol 2008, 35, 1316–1320. [Google Scholar] [CrossRef] [PubMed]
- Pearce, W.J.; Ph, D. Postnatal Development Alters Functional Compartmentalization Of Myosin Light Chain Kinase In Running Head Functional Compartmentalization of Arterial MLCK Correspondence Center for Perinatal Biology R-00293-2020-R1: Sorensen et al: Functional Compartmen.
- Injeti, E.R.; Sandoval, R.J.; Williams, J.M.; Smolensky, A.V.; Ford, L.E.; Pearce, W.J. Maximal stimulation-induced in situ myosin light chain kinase activity is upregulated in fetal compared with adult ovine carotid arteries. Am J Physiol Hear Circ Physiol 2008, 295, 2289–2299. [Google Scholar] [CrossRef]
- Goyal, R.; Longo, L.D. Gene expression in sheep carotid arteries: Major changes with maturational development. Pediatr Res 2012, 72, 137–146. [Google Scholar] [CrossRef]
- Kilavuz, Ö.; Vetter, K. Is the liver of the fetus the 4th preferential organ for arterial blood supply besides brain, heart, and adrenal glands? J Perinat Med 1999, 27, 103–106. [Google Scholar] [CrossRef]
- Giussani, D.A. The fetal brain sparing response to hypoxia: Physiological mechanisms. J Physiol 2016, 594, 1215–1230. [Google Scholar] [CrossRef]
- Benítez-Marín, M.J.; Marín-Clavijo, J.; Blanco-Elena, J.A.; Jiménez-López, J.; González-Mesa, E. Brain sparing effect on neurodevelopment in children with intrauterine growth restriction: A systematic review. Children 2021, 8. [Google Scholar] [CrossRef]
- Meher, S.; Hernandez-Andrade, E.; Basheer, S.N.; Lees, C. Impact of cerebral redistribution on neurodevelopmental outcome in small-for-gestational-age or growth-restricted babies: A systematic review. Ultrasound Obstet Gynecol 2015, 46, 398–404. [Google Scholar] [CrossRef]
- Roza, S.J.; Steegers, E.A.P.; Verburg, B.O.; Jaddoe, V.W.V.; Moll, H.A.; Hofman, A.; et al. What is spared by fetal brain-sparing? Fetal circulatory redistribution and behavioral problems in the general population. Am J Epidemiol 2008, 168, 1145–1152. [Google Scholar] [CrossRef]
- Zhu, M.Y.; Milligan, N.; Keating, S.; Windrim, R.; Keunen, J.; Thakur, V.; et al. The hemodynamics of late-onset intrauterine growth restriction by MRI. Am J Obstet Gynecol [Internet] 2016, 214, e1–e367. [Google Scholar] [CrossRef]
- Laurichesse-Delmas, H.; Grimaud, O.; Moscoso, G.; Ville, Y. Color Doppler study of the venous circulation in the fetal brain and hemodynamic study of the cerebral transverse sinus. Ultrasound Obstet Gynecol 1999, 13, 34–42. [Google Scholar] [CrossRef]
- Morales-Roselló, J.; Khalil, A.; Morlando, M.; Hervás-Marín, D.; Perales-Marín, A. Doppler reference values of the fetal vertebral and middle cerebral arteries, at 19-41 weeks gestation. J Matern Neonatal Med 2015, 28, 338–343. [Google Scholar] [CrossRef]
- Brȩborowicz, A.; Dubiel, M.; Pietryga, M.; Brȩborowicz, G.H.; Gudmundsson, S. Fetal pulmonary and cerebral artery Doppler velocimetry in normal and high risk pregnancy. Ginekol Pol 2014, 85, 26–30. [Google Scholar] [CrossRef]
- Harman, C.R.; Baschat, A.A. Comprehensive assessment of fetal wellbeing: Which Doppler tests should be performed? Curr Opin Obstet Gynecol 2003, 15, 147–157. [Google Scholar] [CrossRef]
- Kiserud, T.; Acharya, G. The fetal circulation. Prenat Diagn 2004, 24, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Bada, H.S.; Hajjar, W.; Chua, C.; Sumner, D.S. Noninvasive diagnosis of neonatal asphyxia and intraventricular hemorrhage by Doppler ultrasound. J Pediatr 1979, 95, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Gudmundsson, S.; Dubiel, M. Doppler velocimetry in the evaluation of fetal hypoxia. J Perinat Med 2001, 29, 399–407. [Google Scholar] [CrossRef]
- Wladimiroff, J.W.; Tonge, H.M.; Stewart, P.A. Doppler ultrasound assessment of cerebral blood flow in the human fetus. BJOG: An International Journal of Obstetrics Gynaecology 1986, 93, 471–475. [Google Scholar] [CrossRef]
- Gailloud, P.; Albayram, S.; Fasel, J.H.D.; Beauchamp, N.J.; Murphy, K.J. Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. Am J Neuroradiol 2002, 23, 585–587. [Google Scholar] [PubMed]
- Bhide, A.; Acharya, G.; Baschat, A.; Bilardo, C.M.; Brezinka, C.; Cafici, D.; et al. ISUOG Practice Guidelines (updated): use of Doppler velocimetry in obstetrics. Ultrasound Obstet Gynecol 2021, 58, 331–339. [Google Scholar] [CrossRef]
- Polavarapu, S.R.; Fitzgerald, G.D.; Contag, S.; Hoffman, S.B. Utility of prenatal Doppler ultrasound to predict neonatal impaired cerebral autoregulation. J Perinatol [Internet] 2018, 38, 474–481. [Google Scholar] [CrossRef]
- Morales-ROSELLOó, J.; Khalil, A.; Morlando, M.; Bhide, A.; Papageorghiou, A.; Thilaganathan, B. Poor neonatal acid-base status in term fetuses with low cerebroplacental ratio. Ultrasound Obstet Gynecol 2015, 45, 156–161. [Google Scholar] [CrossRef]
- Monteith, C.; Flood, K.; Mullers, S.; Unterscheider, J.; Breathnach, F.; Daly, S.; et al. Evaluation of normalization of cerebro-placental ratio as a potential predictor for adverse outcome in SGA fetuses. Am J Obstet Gynecol [Internet] 2017, 216, e1–e285. [Google Scholar] [CrossRef]
- Twickler, D.M.; McIntire, D.D.; Alexander, J.M.; Leveno, K.J. Effects of magnesium sulfate on preterm fetal cerebral blood flow using Doppler analysis: A randomized controlled trial. Obstet Gynecol 2010, 115, 21–25. [Google Scholar] [CrossRef]
- Manaa, E.M.; Romeih, M.S. Fetal responses to epidural analgesia as evidenced by Doppler indices. Middle East J Anesthesiol 2008, 19, 1321–1336. [Google Scholar] [PubMed]
- Aghajanian, P.; Assaf, S.A.; Korst, L.M.; Miller, D.A.; Chmait, R.H. Fetal middle cerebral artery Doppler fluctuations after laser surgery for twin-twin transfusion syndrome. J Perinatol [Internet] 2011, 31, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Oros, D.; Figueras, F.; Cruz-Martinez, R.; Padilla, N.; Meler, E.; Hernandez-Andrade, E.; et al. Middle versus anterior cerebral artery Doppler for the prediction of perinatal outcome and neonatal neurobehavior in term small-for-gestational-age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol 2010, 35, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Benavides-Serralde, J.A.; Hernández-Andrade, E.; Figueroa-Diesel, H.; Oros, D.; Feria, L.A.; Scheier, M.; et al. Reference values for Doppler parameters of the fetal anterior cerebral artery throughout gestation. Gynecol Obstet Invest 2010, 69, 33–39. [Google Scholar] [CrossRef]
- Barbosa, M.M.; Carvalho, F.H.C.; Júnior, E.A.; Nardozza, L.M.M.; Santana, R.M.; Torloni, M.R.; et al. Prediction of acidemia at birth by Doppler assessment of fetal cerebral transverse sinus in pregnancies with placental insufficiency. Ultrasound Obstet Gynecol 2009, 33, 188–192. [Google Scholar] [CrossRef]
- Cruz-Martinez, R.; Figueras, F.; Hernandez-Andrade, E.; Benavides-Serralde, A.; Gratacos, E. Normal reference ranges of fetal regional cerebral blood perfusion as measured by fractional moving blood volume. Ultrasound Obstet Gynecol 2011, 37, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Andrade, E.; Figueroa-Diesel, H.; Jansson, T.; Rangel-Nava, H.; Gratacos, E. Changes in regional fetal cerebral blood flow perfusion in relation to hemodynamic deterioration in severely growth-restricted fetuses. Ultrasound Obstet Gynecol 2008, 32, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.S.K.; Liang, S.T.; Lo, R.L.S.; Chan, F.Y. Middle cerebral arterv Doppler flow velocity waveforms. Obstet Gynecol 1987, 70, 613–616. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




