1. Introduction
The popularity of the otoendoscope has been increasing in recent years and the benefits are well documented. Enhanced visibility of key areas in complex middle ear surgery, lack of post auricular incision and manoeuvrability are key advantages when comparing to the classic microscopic technique. As surgeons become more au fait with the strengths and limitations of the endoscope, the boundaries of same are being explored and what was once thought to be technically challenging has become the norm for some. One such important operative step is that of ossicular chain reconstruction (OCR) or ossiculoplasty, a challenging task when operating single handedly.
The middle ear ossicles transmit sound from the tympanic membrane to the oval window and cochlea via the stapes. The malleus has an additional function of mechanical support of the tympanic membrane; the incus lies between the malleus and the stapes. The three ossicles are held together by delicate joints: the incudo-mallear joint and the incudo-stapedial joint. A number of muscles and ligaments support and move the chain. The transmission of sound and impedance of this transmission is highly dependent on a number of factors including
1) Integrity of the tympanic membrane - perforated, sclerotic or atelectatic
2) Integrity of the ossicular chain - fixed or discontinuous
3) Dynamics of ossicular chain
When sound is not adequately transmitted through the ossicular mechanism, a conductive hearing loss can ensue. When considering OCR, the type of graft material used may vary with ear status: titanium, hydroxyapatite, autologous etc [
1]. A long list of environmental, surgical and patient factors has been shown to affect the audiological outcomes in OCR, with active infection/frequent infection, middle ear mucosal disease, mastoidectomy, revision surgery and patient age amongst others showing an effect on outcomes [
2].
The reporting of outcomes in otological surgery remains somewhat ill-defined and comprises an extremely heterogeneous group of patients, procedure types and variations in not only surgeons approaches and preferences.
2. Materials and Methods
A case report to highlight successful outcome in a with adverse patient and disease factors and a narrative review of the literature.
3. Results
3.1. Case Report
A 36 year old lady presented to the Otology Outpatients with a history of left sided hearing loss and infrequent bouts of otorrhea. There was a preceding history of 2 previous tympanoplasties, one 10 years ago and the second 6 years ago both of which had failed (residual perforation). The operation notes for these procedures were unobtainable.
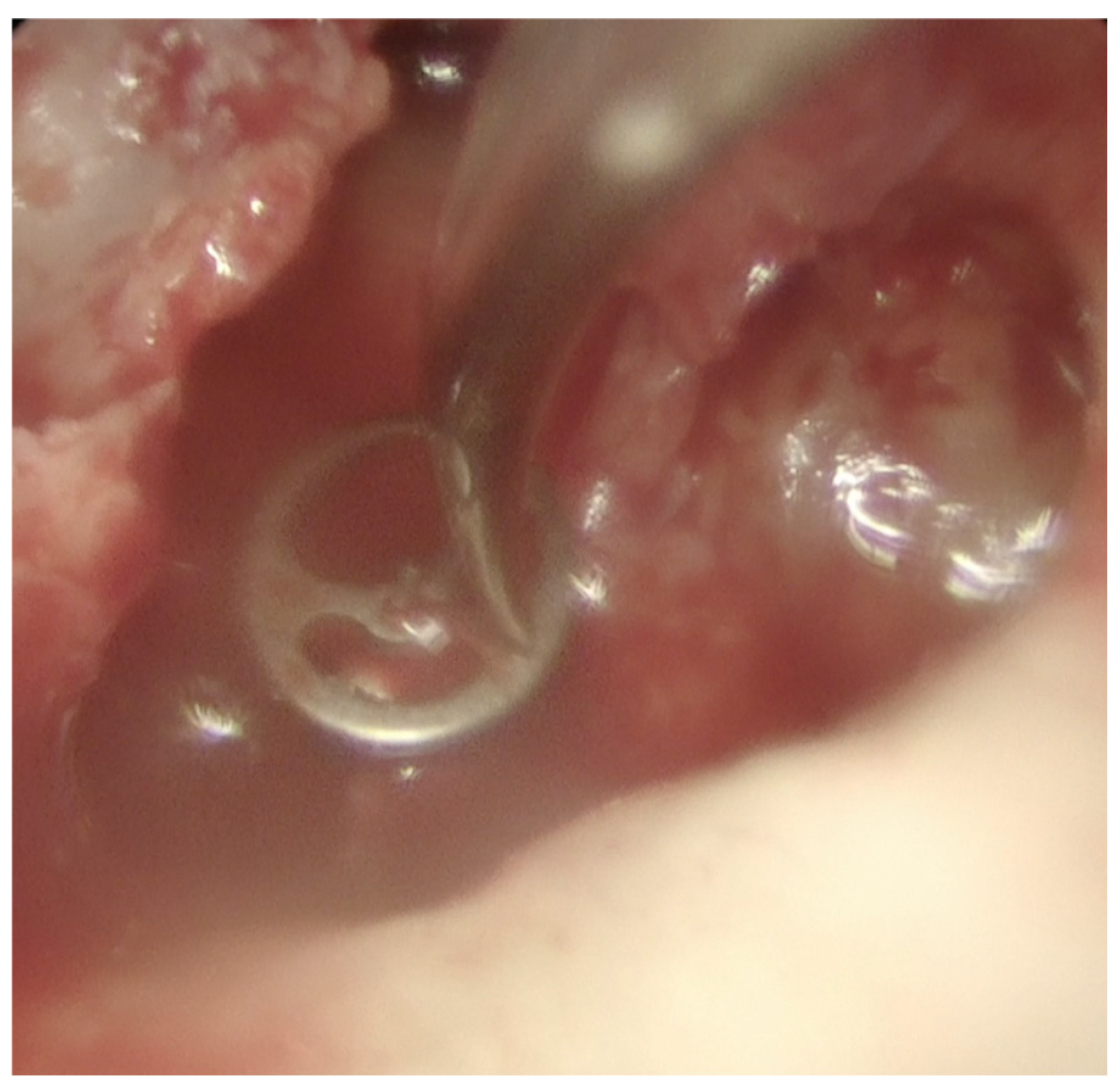
Examination revealed a superior perforation with keratin within (
Figure 1a). The remaining drum was opacified consistent with previous graft reconstruction and/or tympanosclerosis.
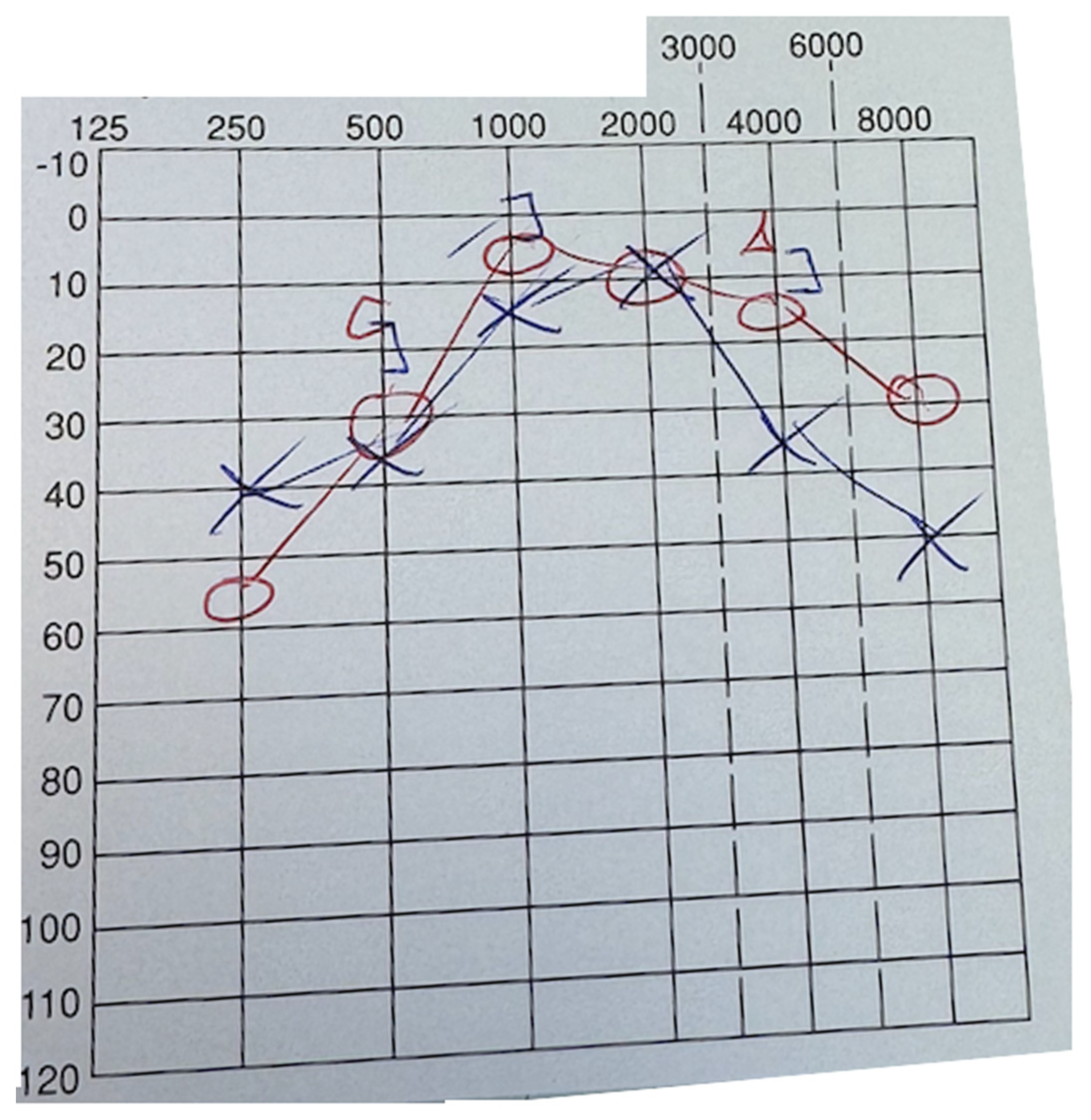
Pure tone audiogram confirmed a severe conductive hearing loss with an air-bone gap of up to 40dbHL (
Figure 2a).
A CT temporal bone scan showed erosion of all middle ear ossicles with some surrounding mesotympanic opacification, clear mastoid air cells and minimal epitympanic disease.
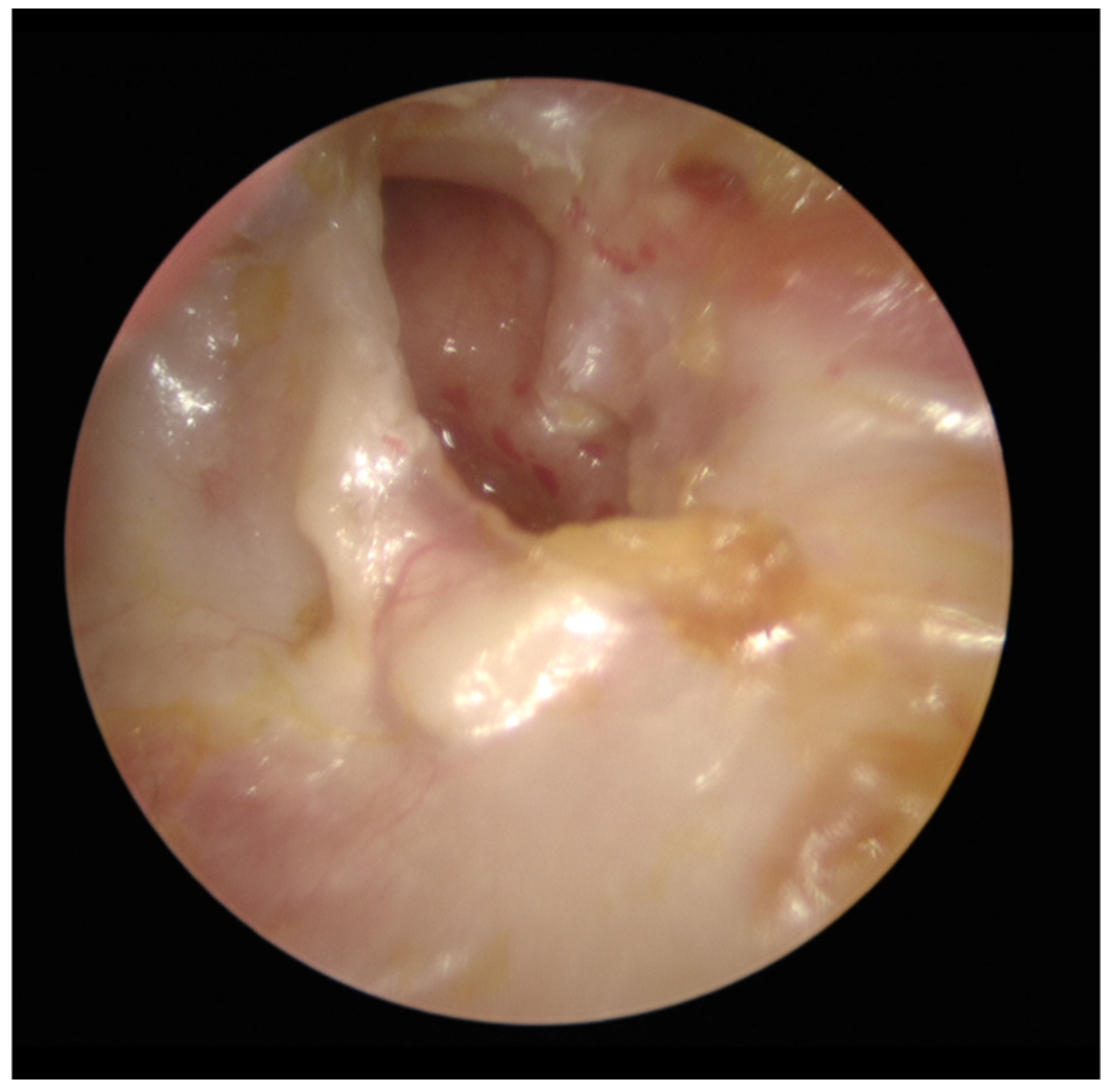
The patient was placed on the waiting list for left endoscopic tympanoplasty and ossicular chain reconstruction. At the time of the surgery, examination remained unchanged and a tympanomeatal flap was raised. There was a tiny incus remnant superiorly which was removed and no discernible malleus remnant. Stapes was within the oval window niche, not fixed and fully intact (Figure 1b). Disease extent was reasonably confined to the mesotympanum and consistent with cross sectional imaging. Keratin was fully cleared from the stapes. Curettage of the scutum and inspection of all key areas ensured all macroscopic disease had been removed. A Kurz partial ossicular chain prosthesis (PORP) was placed. The Variac system was used, and the “dummy” showed the optimal length to be 2.5mm.
Figure 1b.
Endoscopic view of left tympanic membrane, tympanomeatal flap has been raised showing absent malleus and incus with stapes intact.
Figure 1b.
Endoscopic view of left tympanic membrane, tympanomeatal flap has been raised showing absent malleus and incus with stapes intact.
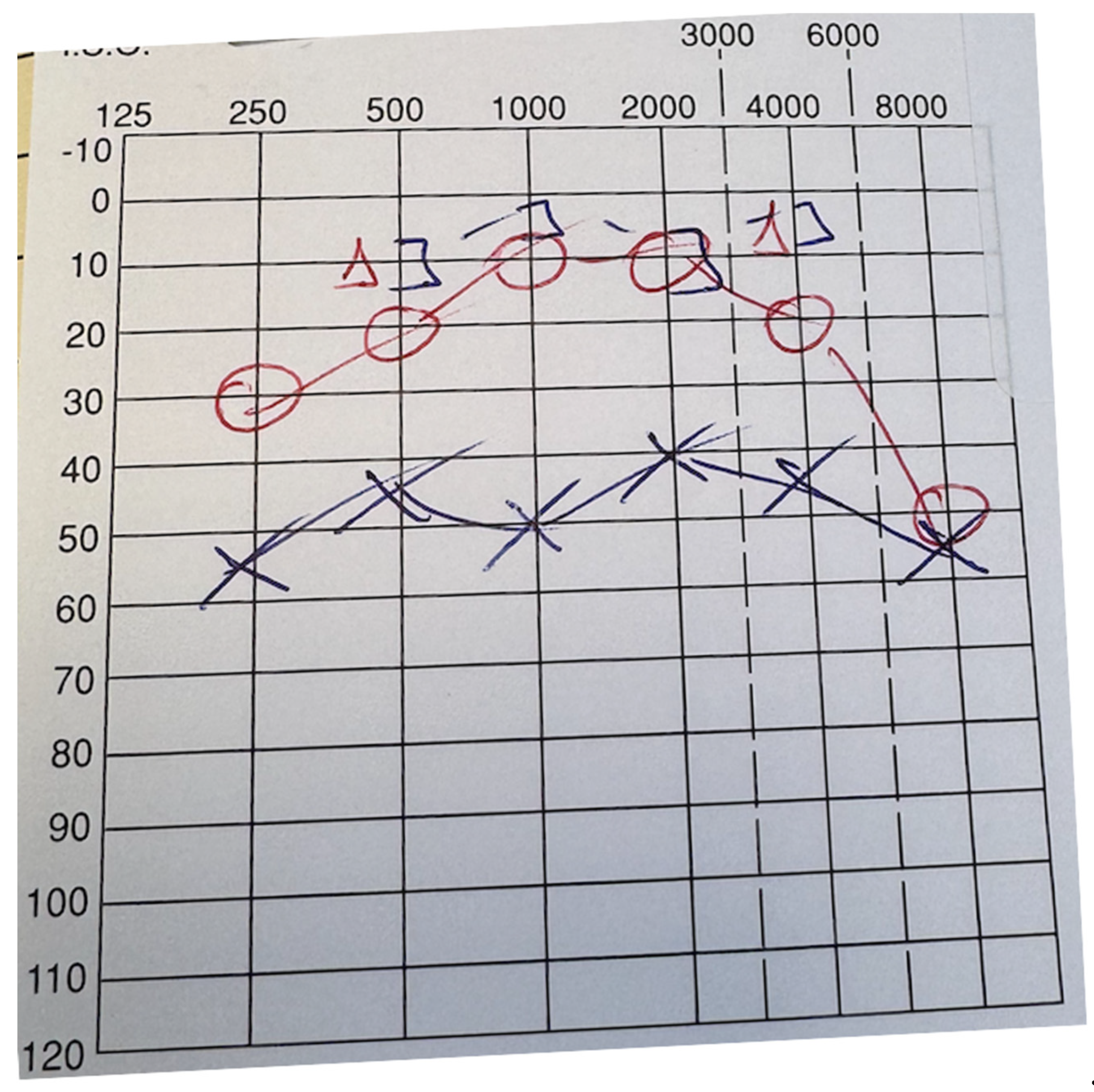
The prosthesis was measured and then gently clipped onto the stapes head and position confirmed and optimised (Figure 1c). Tragal cartilage was placed onto the head of the prosthesis as recommended to prevent extrusion. The drum was reconstructed with the remaining uncut tragal cartilage. Post operatively there were no immediate or long term complications the drum remained fully intact 1 year post operatively without any bouts of otorrhea. Post operative pure tone audiogram at (PTA) at one year revealed complete closure of the air-bone gap (ABG)and patient has had a significant subjective improvement (Figure 2b). A 2 year DWI MRI IAM is awaited to assess for any cholesteatoma recurrence as per surgeon’s follow up protocol.
Figure 1b.
Endoscopic view of left middle ear, PORP clip has been placed single handedly using a curved needle.
Figure 1b.
Endoscopic view of left middle ear, PORP clip has been placed single handedly using a curved needle.
Figure 2B.
Preoperative PTA showing closure of air-bone gap.
Figure 2B.
Preoperative PTA showing closure of air-bone gap.
4. Discussion
The overall success (closure of ABG) of ‘ossiculoplasty’ is quoted as anywhere between 53% and 84% [
3] [
4] [
5]
, and doesn’t differ significantly with the use of the endoscope.
When compared to the classic microscopic technique, the endoscope has similar audiological outcomes in OCR. A systematic review is suggestive of shorter operating times and reduced morbidity, but the heterogeneity of the data limits the significance of these findings [
6]. When specifically comparing endoscopic partial ossicular reconstruction prosthesis (PORP) with microscopic, short term results (1 month) were slightly better. Longer term follow up proved them to be equivocal (3 and 6 months). Endoscopic total ossicular reconstruction prosthesis (TORP) rendered a statistically significant mean postoperative air-bone gap and air-bone gap closure at 1 month when compared to that of microscopic PORP ossiculoplasty. In total ossicular reconstruction prosthesis (TORP) there was no statistically significant difference in the two techniques. Anecdotally, better visualization was described in this study[
7]. The lack of post auricular incision may also confer less pain and morbidity [
8].
The patient in this case report had a number of documented poor prognostic factors in ossiculoplasty surgery such as:
Multiple previous middle ear surgeries
Presence of cholesteatoma
Erosion of ossicular chain/absence of malleus
and these will be discussed in turn.
Multiple previous middle ear surgeries
There is a paucity of high level data regarding the outcome of OCR relating to multiple previous ear surgeries. In the setting of revision OCR, the outcomes are generally inferior [
2]. And this is thought to be relating to the detrimental effect of repeated manipulation of the middle ear such as adhesion formation and fibrosis[
7] In a small cohort study (n=26), e
ndoscopic revision ossiculoplasty emerges as a reliable and effective approach [
10]
.
Presence of cholesteatoma
Endoscopic middle ear surgery in ossiculoplasty has been shown to be successful in monitoring and removal of disease and helpful in reconstruction [
6]. It can be challenging to describe the intraoperative findings across studies, but preservation of the canal wall can be a positive influence in outcomes[
11]. In a larger study of 101 patients, presence of tympanic membrane perforation, ossicular chain erosion and facial nerve dehiscence/perifacial disease were negatively associated with improved hearing postoperatively[
12]. Cholesteatoma limited to the attic was association with better outcomes. Few of these findings failed to achieve statistical significance, and staging of cholesteatoma remains challenging[
13,
14].
Erosion of ossicular chain/absence of malleus
The malleus has an important role to play in terms of middle ear biodynamics and transmission of sound, and a number of theories as to how it actually does this have been proposed[
15]
. However, studies vary in the overall importance of the presence of an intact malleus in the outcomes of OCR, with most of the effect being seen on longer term follow up. Slight audiological improvements are seen with an intact malleus in the short term (mean follow up time nine months)[
16]
.
Other studies suggest that planned malleus removal during ossicular chain reconstruction, allows for simpler reconstruction and comparable results to its preservation and could be considered during surgical planning[
17].
Conversely, absent malleus along with otorrhea has also been shown to be an important unfavourable factor for short-term outcomes in OCR, (6 months), and in the longer term (5 years) absent malleus can be the sole unfavourable factor for long term outcome in OCR. [
18].
In both PORP and TORP, the presence of malleus handle has a statistically significantly positive effect on hearing outcome [
9]. The Senior Author would encourage preservation of the malleus where possible, and to approach with caution in order to achieve long term success.
5. Conclusions
Endoscopic ear surgery has become more accepted over the years. There is a learning curve associated with single handed surgery and further fellowship training specifically in this technique is advisable. However, in some institutions, totally endoscopic ear surgery (
TEES) was considered appropriate for OCR immediately after its introduction, even for expert microscopic surgeons[
19]
. A vast range of factors can affect the audiological outcomes in OCR surgery. Although a number of scoring systems have been proposed in order to help surgeons prognosticate and adequately counsel their patients, they are yet to be adapted internationally. These include the
Ear Environment Risk (EER[
20]
. surgical prosthetic infection tissue eustachian tube (SPITE) middle ear grading systems [
21]
. middle ear risk index (MERI) [
22]
and ossiculoplasty outcome scoring parameter (OOPS) [
9]
. These grading systems may be able to assist in future research to Further studies to assess the applicability of these and well-designed randomised controlled trials comparing techniques are warranted.
Informed Consent Statement
No identifying features have been used so consent was not obtained
Conflicts of Interest
“The authors declare no conflicts of interest.”
References
- Kim H, Ha J, Choo OS, Park H, Choung YH. Which is Better for Ossiculoplasty Following Tympanomastoidectomy: Polycel® or Titanium? Ann Otol Rhinol Laryngol. 2023 Nov;132(11):1404-1411. Epub 2023 Mar 23. PMID: 36951055. [CrossRef]
- Gluth MB, Judd RT, Gurgel RK, Dornhoffer JL, Kutz W, Carlson ML, Kuthubutheen J, Anderson RD, Killeen DE, Barnes JH, Fussell WL, Jeganathan C. A Multi-Center Study of Ossiculoplasty Hearing Outcomes and a Grading Scale of Ear Environment Risk. Laryngoscope. 2025 Apr;135 Suppl 2(Suppl 2):S1-S11. Epub 2024 Dec 23. PMID: 39714957; PMCID: PMC11903935. [CrossRef]
- Uzun T, Çaklı H, Kaya E, Pınarbaşlı MÖ, Gürbüz MK, İncesulu A. Long-term outcomes of ossiculoplasty techniques. Acta Otolaryngol. 2025 Jun 26:1-5. Epub ahead of print. PMID: 40567078. [CrossRef]
- Jung DJ, Yoo MH, Lee KY. Comparison of Ossiculoplasty Outcomes Using Different Materials in the Treatment of Chronic Otitis Media. Otol Neurotol. 2021 Jan;42(1):76-81. PMID: 33201076. [CrossRef]
- Singh K, Nagamani YS, Kour A, Mishra AK, Gupta A. A Comparative Prospective Study to Evaluate Outcomes of Ossiculoplasty using Autograft Versus Synthetic Graft. Indian J Otolaryngol Head Neck Surg. 2022 Aug;74(Suppl 1):511-516. Epub 2021 Jan 8. PMID: 36032831; PMCID: PMC9411295. [CrossRef]
- Tsetsos N, Vlachtsis K, Stavrakas M, Fyrmpas G. Endoscopic versus microscopic ossiculoplasty in chronic otitis media: a systematic review of the literature. Eur Arch Otorhinolaryngol. 2021 Apr;278(4):917-923. Epub 2020 Jul 7. PMID: 32632614. [CrossRef]
- Das A, Mitra S, Ghosh D, Sengupta A. Endoscopic ossiculoplasty: Is there any edge over the microscopic technique? Laryngoscope. 2020 Mar;130(3):797-802. Epub 2019 May 23. PMID: 32073145. [CrossRef]
- Coleman H, Tikka T, Curran J, Iyer A. Comparison of endoscopic vs microscopic ossiculoplasty: a study of 157 consecutive cases. Eur Arch Otorhinolaryngol. 2023 Jan;280(1):89-96. Epub 2022 May 22. PMID: 35598229. [CrossRef]
- Dornhoffer JL, Gardner E. Prognostic factors in ossiculoplasty: a statistical staging system. Otol Neurotol. 2001;22(3):299-304.
- Wang J, Wang Y, Fang S, Huang L, Cen X, Liang Y, Chen A, Lei W, Xiong G, Wu X, Chen K. Endoscopic revision surgery for ossicular chain reconstruction: intraoperative findings and functional outcomes. Eur Arch Otorhinolaryngol. 2025 Apr;282(4):1809-1814. Epub 2024 Nov 16. PMID: 39549077. [CrossRef]
- Kaffenberger TM, Eichar B, Chi DH. Pediatric ossiculoplasty: optimizing outcomes. Curr Opin Otolaryngol Head Neck Surg. 2019 Dec;27(6):489-494. PMID: 31633493. [CrossRef]
- Kosec A, Zivko J, Kurtic A, Ries M, Tomljenovic D, Ajduk J. Impact of Intraoperative Findings on Hearing in Revision Ear Surgery. Iran J Otorhinolaryngol. 2023 May;35(128):147-155. PMID: 37251298; PMCID: PMC10209817. [CrossRef]
- Tono T, Sakagami M, Kojima H, Yamamoto Y, Matsuda K, Komori M, Hato N, Morita Y, Hashimoto S. Staging and classification criteria for middle ear cholesteatoma proposed by the Japan Otological Society. Auris Nasus Larynx. 2017 Apr;44(2):135-140. Epub 2016 Sep 9. PMID: 27616746. [CrossRef]
- Yung M, Tono T, Olszewska E, Yamamoto Y, Sudhoff H, Sakagami M, Mulder J, Kojima H, İncesulu A, Trabalzini F, Özgirgin N. EAONO/JOS Joint Consensus Statements on the Definitions, Classification and Staging of Middle Ear Cholesteatoma. J Int Adv Otol. 2017 Apr;13(1):1-8. Epub 2017 Jan 6. PMID: 28059056. [CrossRef]
- Page JC, Cox MD, King D, Allsopp T, Dornhoffer JL. Long-term Outcomes of Ossiculoplasty With and Without an Intact Malleus. Otol Neurotol. 2019 Jan;40(1):73-78. PMID: 30540697. [CrossRef]
- Maquet C, Crampon F, Ben Slama N, Charnavel P, Bouchetemble P, Marie JP. Short-term hearing outcome of malleus removal for surgery: An observational cohort study. Eur Ann Otorhinolaryngol Head Neck Dis. 2022 Jan;139(1):17-20. Epub 2021 May 26. PMID: 34052161. [CrossRef]
- Haberman RS 2nd, Salapatas AM. Hearing Outcomes after Ossicular Reconstruction with Removal of the Malleus. Otolaryngol Head Neck Surg. 2018 Jan;158(1):144-150. Epub 2017 Aug 29. PMID: 28849699. [CrossRef]
- Yung M, Vowler SL. Long-Term Results in Ossiculoplasty: An Analysis of Prognostic Factors. Otology & neurotology. 2006;27(6):874–81.
- Fukuda A, Morita S, Hoshino K, Fujiwara K, Nakamaru Y, Homma A. Validity of endoscopic ossiculoplasty immediately after its introduction for ossicular chain disruption. BMC Surg. 2024 May 14;24(1):149. PMID: 38745291; PMCID: PMC11091995. [CrossRef]
- Judd RT, Imbery TE, Gluth MB. The utility of numeric grading scales of middle ear risk in predicting Ossiculoplasty hearing outcomes. Otol Neurotol. 2020;41(10):1369-1378. [CrossRef]
- Black B. Ossiculoplasty prognosis: the spite method of assessment. Am J Otol. 1992;13(6):544-551.
- Becvarovski Z, Kartush JM. Smoking and tympanoplasty: implications for prognosis and the middle ear risk index (MERI). Laryngoscope. 2001;111(10):1806-1811. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).