1. Introduction
Ultrasonography is the most widespread diagnostic imaging modality. Ultrasound examinations are performed by physicians as well as representatives of other medical professions, both for diagnostic purposes and during interventional procedures. The versatility and safety of ultrasonography contribute to the growing number of ultrasound examinations performed worldwide [
1]. This may cause work overload and the development of work-related musculoskeletal diseases (WMSDs) in sonographers. According to our previous study 65,6% of sonographers experience pain during or shortly after performing ultrasound examinations, most commonly reported in the cervical and lumbosacral spine, shoulder and the wrist [
2,
3,
4,
5,
6,
7]. Discomfort caused by poor working conditions may affect the course and accuracy of the examination as well as its result. To counteract WMSDs, associations related to healthcare and medical ultrasonography had proposed standards and recommendations regarding work ergonomics for ultrasound specialists [
8,
9,
10,
11]. These preventive principles are mostly based on observational studies of forced body positions and subjective opinions regarding discomfort accompanying sonographic examinations, and incorporate recommendations developed for similar workstations, including computer work [
12,
13]. To date, there are only a few studies that quantitatively measured joint loads, and even fewer that had used dedicated equipment for measurements of the body kinematics in sonographers [
14,
15,
16,
17,
18]. Various validated measurement methods are used to identify incorrect postures and points of physical overload as well as to assess the risk of WMSDs, including the Rapid Upper Limb Assessment (RULA), the Rapid Entire Body Assessment (REBA), the Ovako Working Posture Analysis System (OWAS) or the National Institute for Occupational Safety and Health (NIOSH) regulations [
19,
20,
21,
22,
23]. Both RULA and REBA methods implement a point converter for the position angles of the arm, forearm and the wrist, as well as the neck, trunk and legs. Measurements are taken in the sagittal plane separately for each of the upper limbs. The final score includes additional points for coronal parameters such as raised shoulder, abducted arm, moving the forearm and the wrist sideways from the midline, making RULA/REBA methods highly suitable for the analysis of sonographers’ position.
The purpose of this study was to measure, analyze and quantify the typical musculoskeletal loads in sonographers performing breast and abdominal ultrasound examinations with dedicated biomechanic methodology.
2. Materials and Methods
2.1. Participants
This investigative study initially included 5 radiologists, three women and two men aged 29 to 39, who were substantially trained in breast and abdominal ultrasonography. The experience of the study participants ranged from 12 months (in this case, if at least 20 ultrasound examinations were performed per week) to 12 years.
The exclusion criteria for study participants, apart from the lack of required experience, included:
• previous musculoskeletal surgeries,
• history of serious injuries,
• the presence of endoprostheses or skeletal stabilizing implants,
• chronic and symptomatic diseases of the musculoskeletal system,
• acute pain or exacerbation of chronic pain during the study period,
• chronic or occasional (within 7 days preceding the study) use of painkillers, anti-inflammatory drugs, and antiepileptic drugs.
Ultrasound examinations were performed during routine patients’ follow-up in the Department of Diagnostic Imaging and Interventional Radiology of the University Clinical Center, Katowice, Poland. Sonographers performed examinations in the same setting, using the same equipment, and were sitting on a stool without lumbar support (indicated as the most common type of seat in our previous survey). All participants were right-handed. Each participant performed complete breast and abdominal ultrasound twice, amounting to 10 sets of breast and abdominal ultrasound examinations. A single set consisted of abdominal and breast examinations performed on one patient in continuity. A total of 10 patients were involved.
Both doctors and patients gave informed written consent to participate in the study. The study protocol has been approved by the bioethics committee of the Medical University of Silesia in Katowice, Poland (BNW/NWN/0052/KBI/2/24).
As a result of the data quality verification process, all incomplete recordings and those containing any registration errors were excluded. Ultimately, 4 out of the 10 recorded sessions from 4 radiologists (ID1-ID4) i.e., three women and one man, were qualified for the analysis.
2.2. Kinematic Analysis
Sonographer kinematics were monitored using Noraxon Ultium Motion system (Noraxon, Scottsdale, Arizona, USA). Sixteen sensors were attached to the participants according to the previously described protocol (
Figure 1) [
24]. Sensor data was recorded in real time and analyzed with Noraxon MR3.18 software.
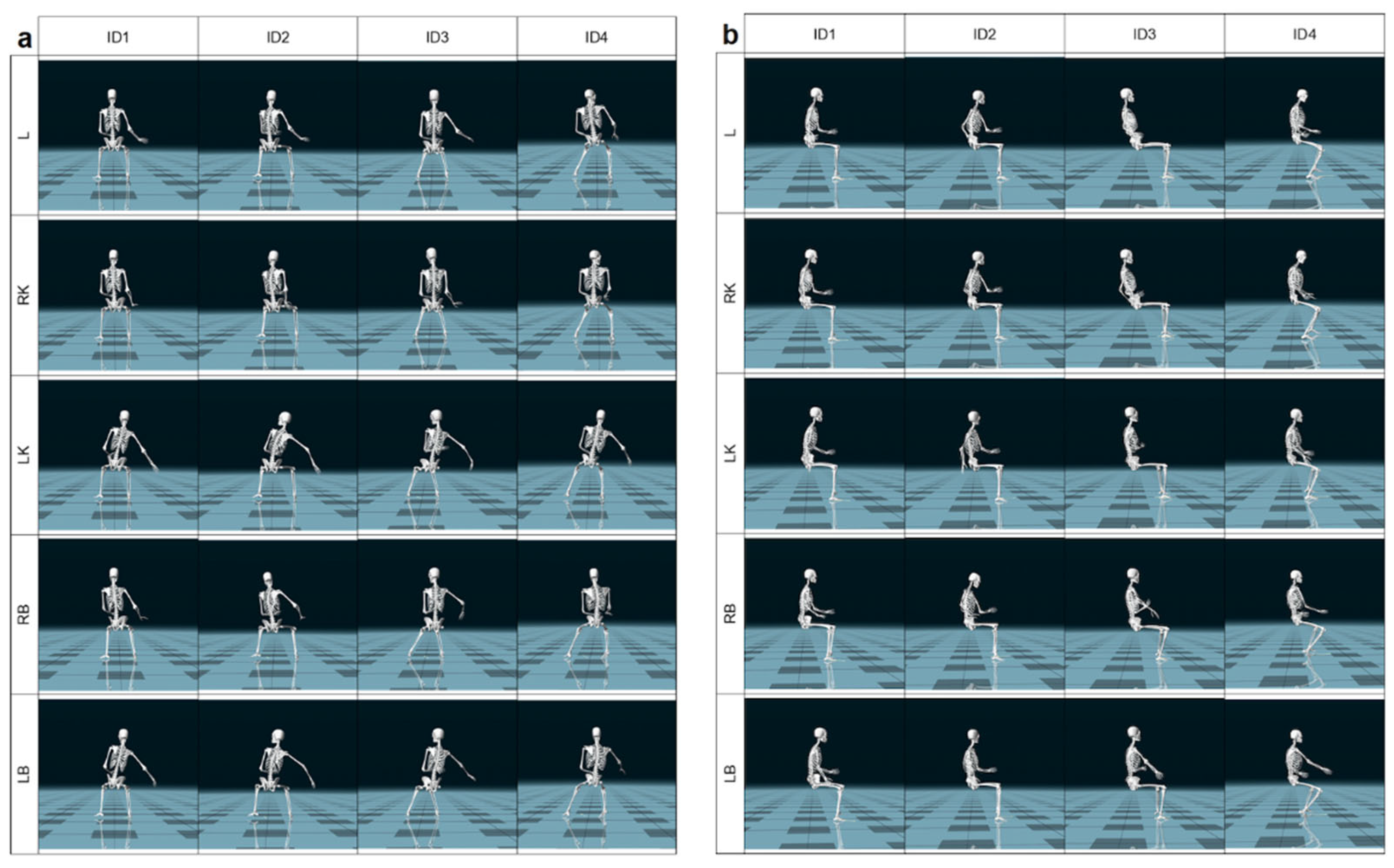
Based on the analysis of the kinematic recordings five critical positions of the transducer were identified and located over the right breast (RB), left breast (LB), liver (L), right kidney (RK) and left kidney (LK) (
Figure 2). These examination segments were determined objectively by detecting the most demanding body positions, including trunk tilt and limb flexion, as well as based on the subjective reports of discomfort. The analysis included shoulder joint abduction, elbow joint flexion, dorsal/palmar wrist flexion, head flexion in the sagittal plane, and trunk flexion in the sagittal plane. Hip and knee joint flexions were additionally considered for the REBA method.
2.3. Biomechanical Analysis
The obtained angle measurements were analyzed according to the RULA and REBA methods using the official assessment sheets, which allowed for a comparison of results and a more detailed identification of ergonomic risk factors [
19,
20]. To perform the analysis data recorded with the Noraxon Ultium Motion system were segmented according to a previously described framework. This approach allowed for the identification of anatomical structures most burdened within the musculoskeletal system. Additionally, complete recordings of abdominal and breast examinations were analyzed to assess the overall ergonomic risk and the potential for occupational diseases resulting from tasks performed by sonographers. The ergonomic assessment in both methods is conducted using images or video recordings captured in the sagittal plane [
25,
26,
27].
2.3.1. RULA Method
The first step in RULA method involves evaluating flexion at the shoulder joint, followed by flexion at the elbow joint, wrist dorsiflexion/palmar flexion, and wrist twist. Based on these measurements, Group Score A is determined, which pertains to the upper body. Two additional indicators are then incorporated: Muscle Use Score (non-static posture—frequent changes in position more than 4 per minute) and Force/Load Score (less than 4.4 lb—holding only the ultrasound transducer). Next, Group B is assessed—this includes the posture of the head, trunk, and legs. As the clinician was seated without backrest and the legs were in contact with the ground, the legs were considered as providing support. Similarly to Group A, indicators of Muscle Use Score (non-static posture) and Force/Load Score (again below 4.4 lb) were added.
The ergonomic risk levels, as defined by the RULA method, are defined as follows: 1-2—acceptable posture; 3-4—further investigation, change may be needed; 5-6—further investigation, change soon; ≥7—investigate and implement change.
2.3.2. REBA Method
In the REBA method, Group A refers to the posture of the head, trunk, and legs. The legs were assigned the maximum score, as the physician was in a seated position. Subsequently, the Force/Load Score was assessed—here, the lowest value (<11 lb) was assigned, as the physician was only holding the ultrasound probe. Next, Group B was evaluated, corresponding to the upper extremities. An additional component, the Hand Coupling Score, was also assessed. In this case, a value corresponding to Well-Fitting Handle and Mid-Range Power Grip was selected, as the ultrasound probe was ergonomically shaped and fit well in the hand. In the final stage of the analysis, the Activity Score was determined, with point added for repeated small range actions (more than 4 per minute).
The levels of ergonomic risk according to the REBA method are defined as follows: 1—negligible risk; 2-3—low risk, change may be needed; 4-7—medium risk, further investigate, change soon; 8-10—high risk, investigate and implement change; ≥11—very high risk, implement change.
2.4. Statistical Analysis
The RULA and REBA scores were analyzed using MATLAB R2023a (MathWorks, Natick, MA, USA). For each specified anatomical location (L, RK, LK, RB, LB) and group (Group A, Group B, Total Score) the median and interquartile range (IQR; 25th–75th percentile) were calculated using the MATLAB functions median() and prctile(). The results are presented in the standard format: median (Q1–Q3).
3. Results
The evaluation was conducted using two ergonomic assessment methods, namely RULA and REBA. The results are presented separately according to the method used.
3.1. RULA Analysis
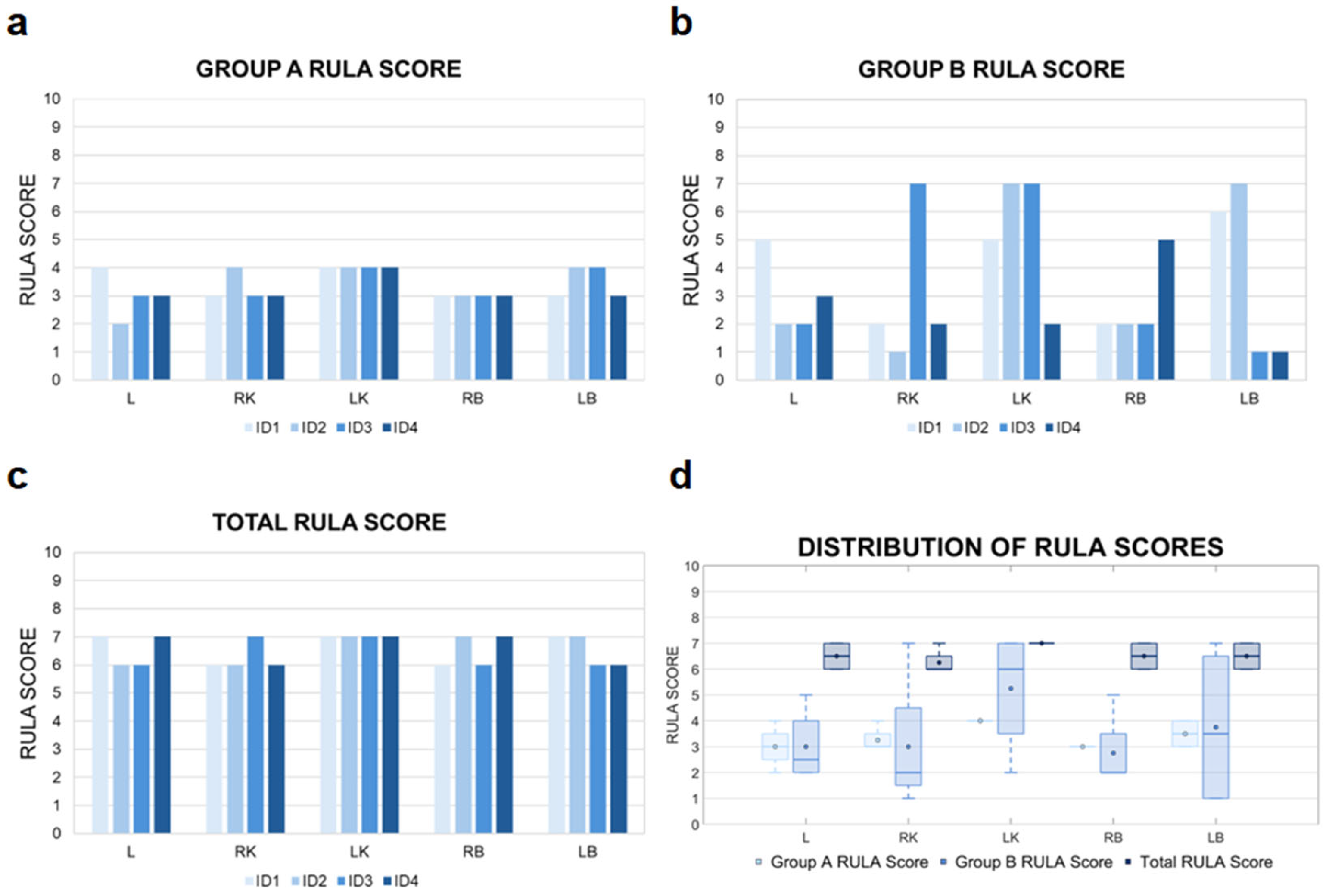
The results obtained using the RULA method are presented collectively in
Figure 3.
In the analysis conducted for Group A imaging of the LK was consistently associated with the highest level of musculoskeletal load. It is important to emphasize that due to the fixed position of the ultrasound machine and the operator’s placement on the right side of the patient, accessing the left side of the body necessitated a non-physiological working posture. This included twisting and leaning the torso to the left, along with increased shoulder flexion of the right upper limb.
For anatomical structures located closer to the examiner’s working position—such as the RK or RB—a more neutral and ergonomically favorable posture could be maintained. The individual RULA scores for Group A indicate that LK imaging generates loading levels within the range of 3–4. Other anatomical structures received scores in the 2–3 range.
In Group B the highest levels of individual musculoskeletal load occurred during the imaging of the LK and LB, which were scored the highest by most examiners (up to 7 RULA points). These high scores primarily resulted from torso positioning—significant forward flexion, lateral bending, and rotation. Thus, torso posture was the main factor influencing the final score for this group. An exception was ID4, for whom the highest load was recorded during RB imaging, due to individual differences in scanning technique (
Figure 2a). Combined Total RULA scores indicated a high overall musculoskeletal load, with medians ranging from 6.5 to 7.0 points across all structures.
The analysis of median RULA scores for Group A indicated that the highest upper body load occurred during imaging of LK and LB, due to the need for trunk rotation and leaning toward the examined region. Interquartile ranges were relatively narrow for most structures, indicating low variability between diagnosticians and consistent musculoskeletal strain patterns (
Table 1). For Group B, the highest median RULA score loads were observed for LK (6.0; 3.5–7.0) and LB (3.5; 1.0–6.5). This suggests that imaging structures located further from the operator require more forced postures, increasing lower body strain and resulting in greater inter-individual variability.
The analysis of RULA scores for diagnosticians’ posture throughout the entire duration of the examination revealed that although the average values in Groups A and B may appear relatively low, the overall mean total score was 7 (
Table 2).
3.2. REBA Analysis
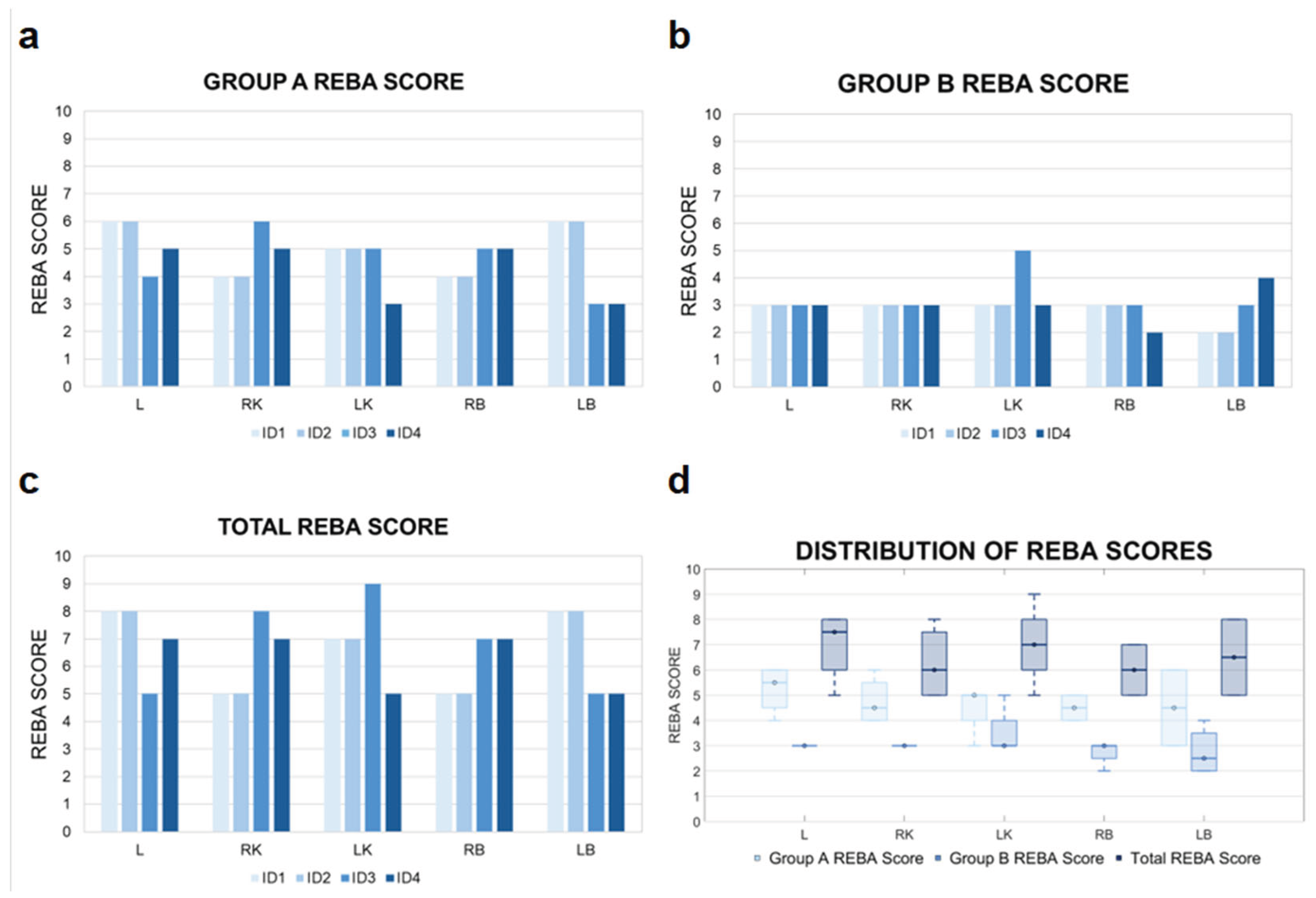
The aggregated results obtained using the REBA method are presented in
Figure 4.
The individual analysis of REBA scores for Group A revealed the highest levels of musculoskeletal strain during imaging of L and LB (range of 5–6). The high scores were primarily attributable to torso positioning—including significant forward flexion, rotation, and lateral bending—which contributed most heavily to the overall strain in this parameter. Torso posture proved to be the decisive factor influencing the REBA outcomes in this group.
The REBA score analysis for Group B indicates moderate ergonomic risk levels within the 2–3 point range. An exception was noted in the case of LK imaging by examiner ID3, where the REBA score reached 5, indicating a moderate risk level. This result highlights the necessity for a more detailed analysis and potential adjustments in workstation configuration or scanning technique. Other anatomical structures including L, RK, and both breasts showed no elevated scores, implying more ergonomic examiner postures during those procedures.
The analysis of total REBA scores, reflecting the overall musculoskeletal load showed consistently elevated values across all examined cases. The highest loads were associated with imaging of the LK, with scores up to 9, indicating a very high overload risk. Lower scores were observed during imaging of the RK and RB, denoting moderate strain that still warrants ergonomic attention.
The highest median REBA scores for Group A and relatively narrow IQRs were observed for L and LK, indicating consistently high upper body loads associated with these locations (
Table 3). For Group B, REBA medians were lower for most structures (3.0–3.5), except for LK, which showed an IQR of 3.0–4.0, reflecting moderate variability between diagnosticians.
The analysis of REBA scores for examiner postures throughout the entire examination procedure reveals that, although the average values in Groups A and B fall within the moderate range, the overall mean score reaches 5 (
Table 2).
Table 4.
REBA Scores calculated for the entire duration of both breast and abdominal examinations.
Table 4.
REBA Scores calculated for the entire duration of both breast and abdominal examinations.
| |
ID1 |
ID2 |
ID3 |
ID4 |
MEAN |
SD |
Group A
REBA Score |
4 |
4 |
3 |
4 |
4 |
1 |
Group B
REBA Score |
3 |
3 |
1 |
3 |
3 |
1 |
Total
REBA Score |
5 |
5 |
5 |
5 |
5 |
0 |
4. Discussion
In the analysis conducted for RULA Group A relating to the upper limb the examination of the LK was associated with the highest level of musculoskeletal load, which included twisting and leaning the torso to the left, along with increased shoulder flexion. LK scans also showed the highest loads when analyzing mean RULA values. Other organs received scores in the 2–3 range, suggesting postures that are close to acceptable or require only moderate attention. This classification highlights the need to pay particular attention to the ergonomics of scanning structures located contralaterally to the dominant hand to prevent upper-body musculoskeletal overload. Adequately, the REBA score analysis for Group B indicated moderate ergonomic risk levels suggesting a need only for ongoing monitoring or minor adjustments. Generally low to moderate scores may reflect favorable working conditions for the upper limb. However, even isolated instances of elevated strain emphasize the importance of accounting for individual postural differences and scanning techniques in ergonomic risk evaluation. Regardless of the specific anatomical location, total REBA scoring confirmed a significant and persistent risk of musculoskeletal strain, highlighting the necessity for ergonomic optimization in clinical environments. The particularly high values observed during imaging of left-sided structures likely stem from the need to operate in torso rotation and forward bending.
In RULA Group B, which concerns the loads occurring in the torso, the highest levels of musculoskeletal loads occurred during the imaging of the LK and LB. Based on the average RULA scores for the anatomical structures in both groups, it can be concluded that the total musculoskeletal load is high. For almost all evaluated structures—except RK—the total RULA score was 7, indicating a need for immediate intervention. The individual analysis of REBA scores for Group A revealed the highest levels of musculoskeletal strain during imaging of the LB and L. In the case of both RULA and REBA body trunk analyzes, the high scores were primarily attributable to significant forward flexion, rotation, and lateral bending of the torso. Due to the proximity of the right side of the patient to the examiner, a more ergonomic posture was often possible during the imaging of right-sided structures. These cases were associated with lower REBA scores, reflecting improved torso positioning and reduced overall musculoskeletal burden. Although no instances of very high risk levels were observed in this group, the findings clearly underscore the importance of ergonomic consideration—particularly with respect to torso alignment—when planning workstation setups and examination techniques to minimize musculoskeletal overload.
Consistently high total RULA scores (>5) indicate musculoskeletal strain across all anatomical regions, particularly the LK, L, and both breasts. High and comparable RULA scores for nearly all structures suggest that the positioning of sonographers and scanning techniques generate significant muscular tension and postural overload across various body regions, regardless of the specific area being examined. Comparable results were seen in the case of total REBA scores, which showed consistently elevated values across all examined cases ranging from 5 to 9. REBA scores point to a high ergonomic risk particularly during imaging of the LB and L, where scores reached 8.
When evaluating load according to examination-specific regions of interest, the most demanding structures could be identified. For breast ultrasound, the highest medians and ranges were observed for LB. For abdominal ultrasound, LK was the most physically demanding, with ranges reflecting high variability depending on individual technique. Findings indicate that locations opposite the operator’s dominant hand generate the greatest musculoskeletal strain.
Previous research had shown similar conclusions regarding RULA scores. One study examined the musculoskeletal loads according to the RULA method during ultrasound of the thyroid gland, abdominal cavity and venous thrombosis of the lower limbs [
14]. The measurements were performed based on the analysis of the video recording during the examinations and using electrogoniometers. In this study, all scans showed significant Group A scores resulting from awkward upper limb postures, forceful manual exertions, and applied static muscle contraction. Group B scores were consistently found to be higher for left sided organs which required the most immediate attention. In a study by Habes et al. the main ergonomic stress factors observed during abdominal and transvaginal examinations were right shoulder flexion and abduction, sustained static forces, and various types of transducer grips [
15]. Friesen et al. determined detailed values of sonographers joint angles while preforming various ultrasound procedures in which trunk side flexion toward the patient ranged from 5°-10°, shoulder abduction from 10°-60°, shoulder flexion from 30°-40°, and elbow flexion from 30°-110° [
16]. A different video-based study showed sonographers spend 68% of scanning time with >30
o shoulder abduction, 63% time with >30
o shoulder outward rotation, and 37% time with the neck bent forward, laterally or twisted >20
o [
17]. The shoulder was unsupported or static for 73% of scanning time mainly during carotid ultrasound compared with abdominal, obstetrical or lower limbs examinations. For larger patients more wrist flexion and extension were used to reach the closer and further areas of the abdomen [
15]. Sonographers also had to twist the neck to the left to view the monitor, flex and abduct the left shoulder, and extend the elbow to operate the control panel. Based on the EMG analysis of the shoulder and back muscles the static amplitude probability distribution functions exceeded 3% maximum velocity contraction corresponding to a medium risk rating for shoulder and neck disorders [
17]. The same study reported an average probe grip force during scanning of 4 kg with the peak forces reaching over 27 kg [
28]. The minimal applied force of 1 kg provides little or no opportunity to rest and is associated with increased risk of hand/wrist cumulative trauma disorders, including carpal tunnel syndrome. Additional identified factors contributing to the loads experienced by the sonographers were bed width (higher loads observed for wider beds) and the lack of elbow support [
15].
The analysis of scores for sonographers’ postures throughout the entire duration of both breast and abdominal examinations revealed that the average values in Groups A and B were low and moderate for RULA and REBA methods, respectively. Nevertheless, the overall mean total score reached 7 for RULA indicating a high level of musculoskeletal strain, and 5 in case of REBA, corresponding to a notable level of strain. The persistence of such high values underscores the urgent need to optimize working conditions and adapt scanning techniques to effectively reduce musculoskeletal loading among sonographers.
Continuous monitoring and the implementation of ergonomic interventions are essential for improving workplace comfort and occupational safety. The main emphasis is on maintaining a neutral body position during ultrasound examinations, education and training in ergonomics as well as sensible management of the work schedule [
9]. Additional emphasis is placed on equipment and its ergonomic configuration during diagnostic sonography [
29]. Before beginning the examination, it is recommended to adjust the control-panel and monitor as well as the chair and examining bed, utilize footrest and seats with lumbar support. Additional devices include cushions, ergonomic probes, cable braces and forearm/arm/shoulder support systems. The few available reports on prototypes of assistive devices leave considerable room for further biomechanical investigations [
30]. A promising perspective already being dynamically explored is the robot-assisted ultrasound (RAUS) which has the potential to facilitate future ultrasound diagnostics while relieving sonographers of their workload and minimizing the risk of WMSDs [
31].
Study Limitations
One limitation of our study is the small sample size. Only 4 out of 10 sets of examinations from 4 out of 5 sonographers were analyzed due to the presence of incomplete data or incorrect data transfer caused by the sensor’s signal interference. The inclusion criterion for the analysis was a complete recording of both breast and abdominal ultrasound enabling the selection of key moments of the examination for each critical position. An additional limitation of the study which prevents its generalizability is the lack of assessment of the influence of sonographers’ and patients’ anthropometric data on kinematic results. However, a reliable assessment would require examining a large group of individuals with a wide range of body types.
Study Strengths
To the best of our knowledge, this is the first study utilizing motion sensors to assess the kinematics of sonographers. The use of sensors allowed us to obtain the most appropriate and precise measurements and therefore to exclude any measurement errors related to the assessment of body position in a single plane. It is also the first study to analyze biomechanics and postural loads during breast ultrasound examinations.
5. Conclusions
The analyses indicate that LB is the most demanding structure for breast ultrasound, whereas the LK poses the highest load during abdominal ultrasound. Anatomical structures located closer to the examiner’s working position determined a more neutral and ergonomically favorable posture. Adopting a forced body position during ultrasound examinations seems unavoidable, therefore solutions should be sought that will reduce physical strain, including training in work ergonomics and developing supporting devices that relieve the musculoskeletal system.
Author Contributions
Conceptualization, M.W. and R.M.; methodology, M.W., R.M., A.G.-K. and A.M.-B.; software, R.M. and A.G.-K.; validation, R.M., A.G.-K. and M.H.; formal analysis, R.M., A.G.-K., M.W. and M.H.; investigation, M.W., M.H. I.R. and M.C.; resources, M.W., K.S.-R., A.G.-K. A.M.-B. and R.M.; data curation, M.H.; writing—original draft preparation, M.W., M.H.; writing—review and editing, A.G.-K. and A.M.-B. and R.M.; visualization, M.W., M.H.; supervision, K.S.-R., A.G.-K. and R.M.; project administration, M.W.; funding acquisition, M.W. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by the Medical University of Silesia, grant number BNW-2-075/K/5/K.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of the Medical University of Silesia in Katowice, Poland (BNW/NWN/0052/KBI/2/24, 30.01.2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Winder, M.; Owczarek, A.J.; Chudek, J.; Pilch-Kowalczyk, J.; Baron, J. Are We Overdoing It? Changes in Diagnostic Imaging Workload during the Years 2010–2020 including the Impact of the SARS-CoV-2 Pandemic. Healthcare 2021, 9, 1557. [Google Scholar] [CrossRef]
- Ciekalski, M.; Rosół, I.; Filipek, M.; Gruca, M.; Hankus, M.; Hanslik, K.; Pieniążek, W.; Wężowicz, J.; Miller-Banaś, A.; Guzik-Kopyto, A.; Michnik, R.; Winder, M. Work-related musculoskeletal disorders in Polish sonographers-A questionnaire study. Curr Probl Diagn Radiol 2024, 53, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Barros-Gomes, S.; Orme, N.; Nhola, L.F.; Scott, C.; Helfinstine, K.; Pislaru, S.V.; Kane, G.C.; Singh, M.; Pellikka, P.A. Characteristics and Consequences of Work-Related Musculoskeletal Pain among Cardiac Sonographers Compared with Peer Employees: A Multisite Cross-Sectional Study. J Am Soc Echocardiogr 2019, 32, 1138–1146. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.; Roll, S.; Baker, J. Work-Related Musculoskeletal Disorders (WRMSD) Among Registered Diagnostic Medical Sonographers and Vascular Technologists: A Representative Sample. J Diagn Med Sonogr 2009, 25, 287–299. [Google Scholar] [CrossRef]
- Gremark Simonsen, J.; Axmon, A.; Nordander, C.; Arvidsson, I. Neck and upper extremity pain in sonographers - Associations with occupational factors. Appl Ergon 2017, 58, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Hogan, A. Pain Levels and Injuries by Sonographic Specialty: A Research Study. J Diagn Med Sonogr 2021, 38, 53–58. [Google Scholar] [CrossRef]
- Wareluk, P.; Jakubowski, W. Evaluation of musculoskeletal symptoms among physicians performing ultrasound. J Ultrason 2017, 17, 154–159. [Google Scholar] [CrossRef]
- AIUM Practice Principles for Work-Related Musculoskeletal Disorder. J Ultrasound Med 2023, 42, 1139–1157. [CrossRef]
- The Society of Diagnostic Medical Sonography. Available online: https://www.sdms.org/docs/default-source/Resources/work-related-musculoskeletal-disorders-in-sonography-white-paper.pdf (accessed on 31 March 2025).
- The Australasian Sonographers Association. Available online: https://www.sonographers.org/publicassets/e02a231f-e2de-ef11-9137-0050568796d8/SDMS_Industry_Standards_Aug17.pdf (accessed on 31 March 2025).
- The Society of Radiographers. Available online: https://www.sor.org/getmedia/d25064fe-ad05-42c0-a777-efaca0d2eb35/sor_industrystandards_prevention_musculoskeletal.pdf_1 (accessed on 31 March 2025).
- Harrison, G.; Harris, A. Work-related musculoskeletal disorders in ultrasound: Can you reduce risk? Ultrasound 2015, 23, 224–230. [Google Scholar] [CrossRef]
- Zangiabadi, Z.; Makki, F.; Marzban, H.; Salehinejad, F.; Sahebi, A.; Tahernejad, S. Musculoskeletal disorders among sonographers: a systematic review and meta-analysis. BMC Health Serv Res 2024, 24, 1233. [Google Scholar] [CrossRef]
- Burnett, D.R.; Campbell-Kyureghyan, N.H. Quantification of scan-specific ergonomic risk-factors in medical sonography. Int J Ind Ergon 2010, 40, 306–314. [Google Scholar] [CrossRef]
- Habes, D.J.; Baron, S. Ergonomic evaluation of antenatal ultrasound testing procedures. Appl Occup Environ Hyg. 2000, 15, 521–528. [Google Scholar] [CrossRef]
- Friesen, M.N.; Friesen, R.; Quanbury, A.; Arpin, S. Musculoskeletal injuries among ultrasound sonographers in rural Manitoba: a study of workplace ergonomics. AAOHN J 2006, 54, 32–37. [Google Scholar] [CrossRef]
- Village, J.; Trask, C. Ergonomic analysis of postural and muscular loads to diagnostic sonographers. Int J Ind Ergon 2007, 37, 781–789. [Google Scholar] [CrossRef]
- Paschoarelli, L.; Oliveira, A.B.; Coury, H. Assessment of the ergonomic design of diagnostic ultrasound transducers through wrist movements and subjective evaluation. Int J Ind Ergon 2008, 38, 999–1006. [Google Scholar] [CrossRef]
- McAtamney, L.; Nigel Corlett, E. RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon 1993, 24, 91–99. [Google Scholar] [CrossRef]
- Hignett, S.; McAtamney, L. Rapid entire body assessment (REBA). Appl Ergon 2000, 31, 201–205. [Google Scholar] [CrossRef]
- Karhu, O.; Kansi, P.; Kuorinka, I. Correcting working postures in industry: A practical method for analysis. Appl Ergon 1977, 8, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Fox, R.R.; Lu, M.L.; Occhipinti, E.; Jaeger, M. Understanding outcome metrics of the revised NIOSH lifting equation. Appl Ergon 2019, 81, 102897. [Google Scholar] [CrossRef] [PubMed]
- Kee, D. Systematic Comparison of OWAS, RULA, and REBA Based on a Literature Review. Int J Environ Res Public Health 2022, 19, 595. [Google Scholar] [CrossRef] [PubMed]
- Piętakiewicz, W.; Sykała, A.; Trybuszkiewicz, P.; Trepiak, R.; Szczyrba, K.; Roszak, M.; Michnik, R.; Molenda, M.; Miller-Banaś, A. Application of the NORAXON myoMotion system in the scope of 5S methodology applications. In TalentDetector2024_Winter: International Students Scientific Conference, 26th January 2024; Bonek, W.M., Ed.; Department of Engineering Materials and Biomaterials, Silesian University of Technology: Zabrze, Poland, 2024; pp. 386–395. [Google Scholar]
- Central Institute for Labour Protection, National Research Institute. Available online: https://www.ciop.pl/CIOPPortalWAR/appmanager/ciop/pl?_nfpb=true&_pageLabel=P620059861340178661073&html_tresc_root_id=300012898&html_tresc_id=300012923&html_klucz=32274 (accessed on 1 June 2025).
- Ergo Plus. Available online: https://ergo-plus.com/wp-content/uploads/rapid-upper-limb-assessment-rula-1.png?x51169 (accessed on 1 June 2025).
- Ergo Plus. Available online: https://ergo‐plus.com/wp‐content/uploads/rapid-entire-body-assessment-reba-1.png?x51169 (accessed on 1 June 2025).
- Silverstein, B.A. (1985). The prevalence of upper extremity cumulative trauma disorders in industry. Ann Arbor: University of Michigan 1985, University Microfilms International.
- Alshuwaer, T.A.; Gilman, F. Prevention of Shoulder Injuries in Sonographers: A Systematic Review. J Diagn Med Sonogr 2019, 35, 392–399. [Google Scholar] [CrossRef]
- Sommerich, C.M.; Lavender, S.A.; Evans, K.; Sanders, E.; Joines, S.; Lamar, S.; Radin Umar, R.Z.; Yen, W.T.; Li, J.; Nagavarapu, S.; Dickerson, J.A. (2016). Collaborating with cardiac sonographers to develop work-related musculoskeletal disorder interventions. Ergonomics 2016, 59, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Hu, Z.; Wang, C.; Cao, S.; Zhang, C. Technological evolution and research frontiers of robot-assisted ultrasound examination: a bibliometric exploration. J Robot Surg 2025, 19, 555. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).