Capsule
The evidence for a correlation between HBOT use and female infertility is present but weak. More studies are needed for comparing the different protocols more precisely.
1. Introduction
1.1. Rationale
Infertility is a real problem and the scientific world is constantly looking for possible solutions that can increase the chances of a pregnancy. The WHO (World Health Organization) reports that between 48 million couples and 186 million individuals live with infertility globally.
It is now known that sirtuins positively affect fertility. Sirtuins, whose family includes seven types, are a family of proteins with enzymatic activity belonging to class III histone deacetylases (HDACs) and which differ in sequence and length in their N- or C-terminal domains. They share a NAD+ binding catalytic domain and can act specifically on different substrates depending on the biological processes in which they are involved [
1]. SIRT1-SIRT7 sirtuins are involved in many and varied cellular functions ranging from gene silencing to cell cycle control, apoptosis and energy homeostasis [
2]. SIRT3-5 are in the mitochondrion and, in particular, SIRT3 seems to be involved in the process related to female fertility. As reported in an interesting and recent study published in 2021 in
Antioxidants [
3], it seems to be involved in the mechanism of female reproduction, improving the competence of oocytes in the human species and animal models. Furthermore, SIRT3 protects oocytes and early embryos against stress. However, still little is known about the functions of sirtuins 4 and 5 on the reproductive system.
1.1.1. Focus on SIRT 1
Another study published in the journal ‘Human Reproduction Update’ in 2018 [
4] states that there are numerous studies that associate SIRT1 with the physiological or pathological reduction of ovarian reserve.
It is hypothesized that increasing SIRT1 activity may have potential effects on improving fertility in PCOS, diabetes, endometriosis, xenobiotic stress, and ageing. Since the effects and the innumerable processes in which sirtuins are involved are broadly known, one wonders at this point how they can be regulated.
It has also been shown how it regulates proliferation and apoptosis in granulosa cells. SIRT1 plays a key role in fertility. Its down-regulation is associated with reduced ovarian reserve. In general, sirtuins affect female reproductive physiology by acting as antioxidants against ROS and SIRT1 is a principal and precise pharmacological focus against ROS-destroying oocytes [
5]. SIRT1 activity can enhance fertility by conserving ovarian reserve, regulating granulosa cell (GCs) proliferation and apoptosis, and protecting against oxidative stress. The decreased expression of SIRT1 affects infertility. It causes
mitochondrial dysfunction with an increase in ROS, lipid peroxidation and DNA damage in both male and female gametes [
5].
1.1.2. Relationship Between Sirtuins and HBOT
It has been demonstrated by Nofar Schottlender et al. in 2021 how short-term treatments cause deleterious effects on both mitochondrial activity and ROS production, while long-term treatments increase mitochondrial activity and decrease ROS levels, partially due to the effects of hyperbaric oxygen therapy which increases the antioxidant defence mechanisms [
6].
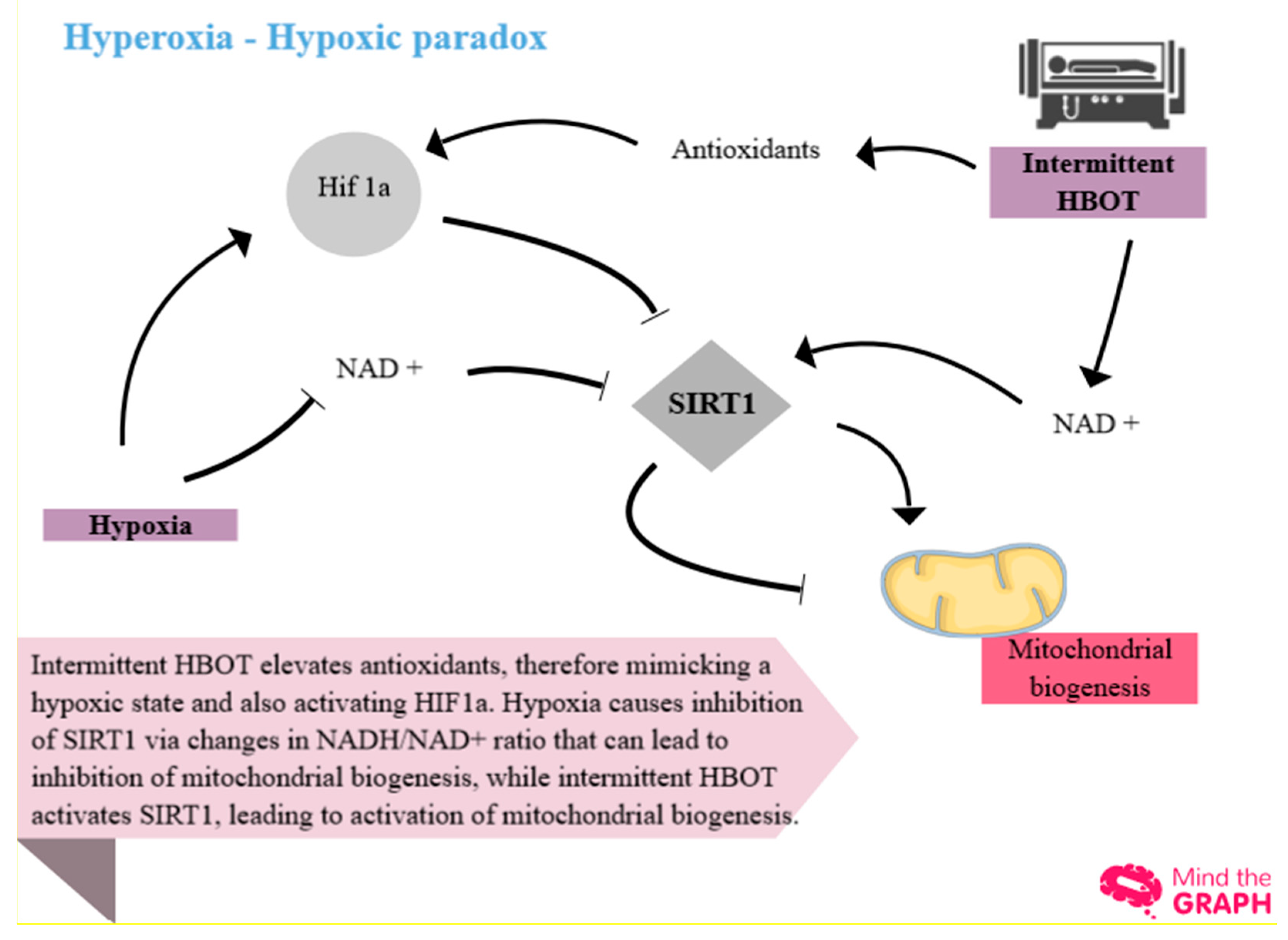
Figure 1.
shows the concept of the ‘hyperoxic-hypoxic paradox’ or ‘normobaric oxygen paradox’. In the same study [
6], it is explained how this consists of the fluctuation, not only at the end of the session but also during the HB treatment itself, between 100% oxygen and 21% oxygen. This fluctuation is perceived by the body as a sort of relative hypoxia and hyperoxia and recruits important factors, HIF1a (hypoxia-induced factor) and SIRT1 which can be inhibited or activated depending on the activated pathway.
Figure 1.
shows the concept of the ‘hyperoxic-hypoxic paradox’ or ‘normobaric oxygen paradox’. In the same study [
6], it is explained how this consists of the fluctuation, not only at the end of the session but also during the HB treatment itself, between 100% oxygen and 21% oxygen. This fluctuation is perceived by the body as a sort of relative hypoxia and hyperoxia and recruits important factors, HIF1a (hypoxia-induced factor) and SIRT1 which can be inhibited or activated depending on the activated pathway.
At present, the method of applying hyperbaric oxygen therapy in the field of female infertility is unclear. There are many protocols used, but none of these is validated or internationally accepted for this type of pathology.
1.1.3. Description of the Methods Being Investigated
The use of HBOT in the context of female infertility is infrequent. In this review, all possible treatments on the topic that include hyperbaric oxygen therapy are mentioned.
1.1.4. How These Methods Might Work
The methods of the studies summarized in this review have an important social impact. The protocols examined and summarized here will be commented on in their heterogeneity.
1.1.5. Why It Is Important to Do This Review
Until 8 December 2022, this review is the only one to address the topic of the possible correlation between hyperbaric oxygen therapy and female infertility. It plays an essential role, in being female infertility a social problem. Understanding the correct methodology for using HBOT in the field of female infertility would be useful for understanding the possible correlations in more detail, as well as finding a possible further therapy for this pathology.
1.2. Objectives
The primary objective of this review is to analyze with a precise methodology the relationship, little studied in the scientific panorama, between HBOT and female infertility and clarify its possible correlation and methods of use. This is proposed by reviewing the studies on the effect that oxygen therapy has on the studies present in this field and by studying the methodology of the intervention. Another objective is to try to understand, based on what has been seen here, if there are reasons that can justify the use of this therapy in this important and disabling pathology.
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Selection Criteria
Studies that match the following criteria were included: [
1] every type of published or ongoing study on specified databases dealing with [a] female infertility of every cause and [b] hyperbaric oxygen therapy or [c] oxygen therapy linked.
PICOs
- Patients: participants included in the review were patients diagnosed with infertility or poor prognosis for pregnancy.
- Intervention: patients included in this review performed hyperbaric oxygen therapy (HBOT) as the main or adjunctive treatment.
- Comparison: standard or other therapy for infertility.
- Outcomes: findings in terms of laboratory values (e.g. AMH levels, endometrial thickness, etc.) directly or indirectly related to infertility were included.
- Study type: every type of published or ongoing study (observational or other) was included.
Studies that match one of the following criteria were excluded: [
1] articles on the Internet not cited; [
2] studies dealing with male infertility. No language restriction was imposed for this review.
2.2. Information Sources
The search was carried out on databases: PubMed/Medline, Scopus, LILACS, and COCHRANE up to December 2022. Relevant articles were also searched on some websites, such as Google Scholar and Google. Duplicated studies and unavailable study data articles were eliminated by human screening. The eligibility of the articles was assessed based on the inclusion and exclusion criteria.
2.3. Search Strategy
The studies were searched on the databases listed below. The last search date was December 8, 2022. In some databases, to obtain a better screening, filters have been placed. The search strategies used to search the various databases are specified in the Appendix of this review ('Database search strategy).
PUBMED
Search: ((((female infertility[MeSH Terms]) OR ((‘endometrial infertility’) OR (((unexplained infertility[MeSH Major Topic]) OR (unexplained infertility)) OR ((female infertility) OR (female infertility[MeSH Major Topic]))))) OR (infertility)) OR (infertility[MeSH Major Topic])) AND (((‘oxygénothérapie hyperbare’) OR ((((hyperbaric oxygen[MeSH Major Topic]) OR (hyperbaric oxygen therapy)) OR (((‘oxygen therapy’) OR (oxygen therapy[MeSH Major Topic])) OR (hbot))) OR (HBO))) OR ((‘intermittent hyperoxia’) OR (‘Hyperoxic-Hypoxic Paradox’)))
SCOPUS
Search: ( ‘hyperbaric oxygen therapy’ OR ‘HBOT’ ) AND ‘female infertility’ [All fields]
LILACS
Search: hyperbaric oxygen therapy AND infertility
COCHRANE
Search: hyperbaric oxygen therapy AND infertility
GOOGLE SCHOLAR
Search: ‘hyperbaric oxygen’ AND ‘female infertility’
filters:2018-2022; scientific articles
GOOGLE
Search: ‘Oxybarotherapy’ AND female infertility; ‘AMH AND hyperbaric’
2.4. Selection Process
2.4.1. Selection of Studies
The studies were selected according to the inclusion criteria. Any studies citing HBOT and female infertility concurrently were included to increase the number of studies to analyze and compare on the topic of this review.
2.4.2. Data Extraction and Management
Also in this phase, a human screening was carried out by the authors. After having obtained the search results using specific terms (see '6.3 – Search Strategy') on the listed databases, the first three authors proceeded to carry out a human screening based on the treated topic according to inclusion and exclusion criteria. No language filter was applied. There were no disagreements between screeners.
2.4.3. Types of Studies
This review included every type of study dealing with the correlation between HBOT and female infertility.
2.4.4. Types of Data
Observational studies, and healthcare trials, including trials of clinical interventions and non-clinical interventions where the effects of HBOT on female infertility outcomes were measured.
2.4.5. Types of Methods
The subject of the review are the methods with which hyperbaric oxygen therapy is administered, the protocol used and above all, if described, the comparison with the current ‘standard’ treatment which does not involve the use of the hyperbaric chamber in female infertility.
2.4.6. Electronic Searches
No linguistic limits have been placed in the databases and on various sites.
2.4.7. Searching Other Resources
A general internet search using Google was also used. Correspondence articles were also included in this review.
2.5. Data Collection Process
2.5.1. Data Collection and Analysis
The data was collected by searching for the keywords listed above. The analysis was carried out with the ReviewManager 5.4 program. The GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology was applied to assess the certainty of evidence (CoE). The CoE can be rated down by one or two levels under consideration if there are serious or very serious concerns, respectively, in any of the five domains: risk of bias, inconsistency, indirectness, imprecision or publication bias. The level of evidence was finally classified as high, moderate, low and very low. The CoE. GRADE was determined by GRADEpro Guideline Development Tool (McMaster University, 2015 (developed by Evidence Prime, Inc., Hamilton, ON, Canada), accessible from gradepro.org).
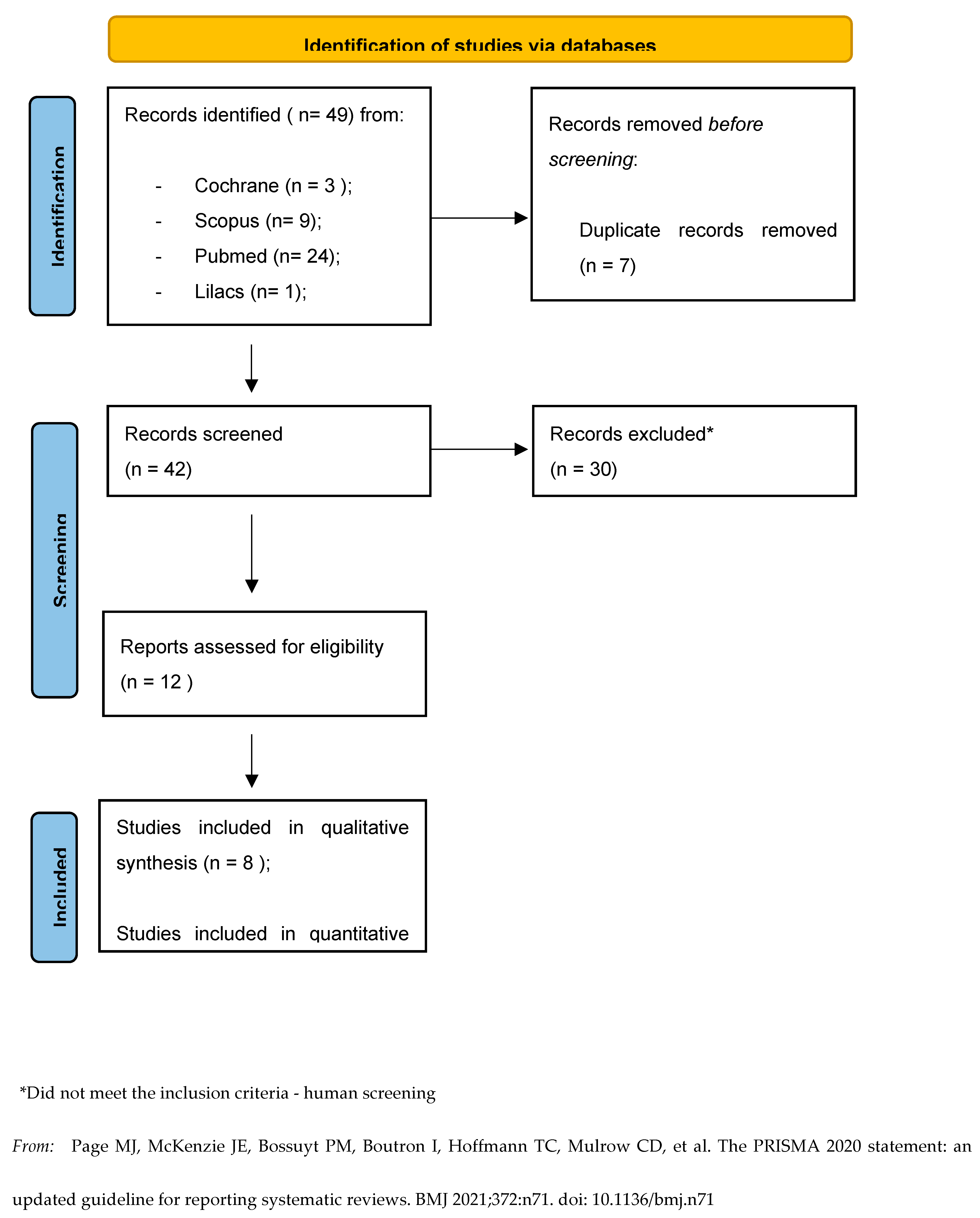
Abstracts of individual studies were viewed first. Subsequently, as reported in the PRISMA flow chart (Figure 2), the duplicates found between one database and another were eliminated. Finally, all studies that did not meet the inclusion criteria were excluded. Data statistical analysis was performed by the first three authors and revisioned by the last one.
Figure 1.
PRISMA Statement - Study flow diagram.
Figure 1.
PRISMA Statement - Study flow diagram.
Figure 2.
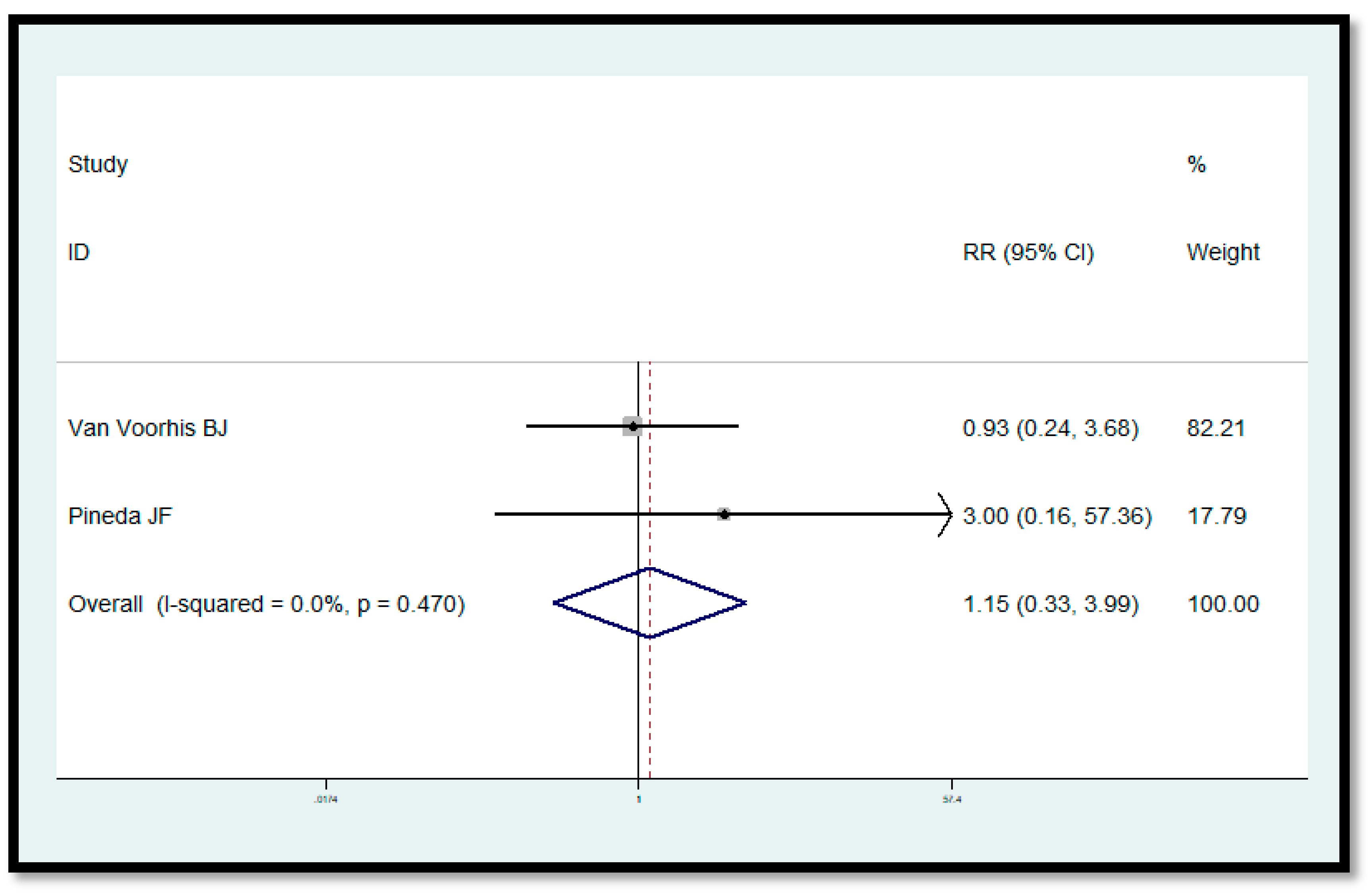
Forest plot showing RR in overall studies. The Forest Plot shows the effect of HBOT in increasing pregnancy probability.
Figure 2.
Forest plot showing RR in overall studies. The Forest Plot shows the effect of HBOT in increasing pregnancy probability.
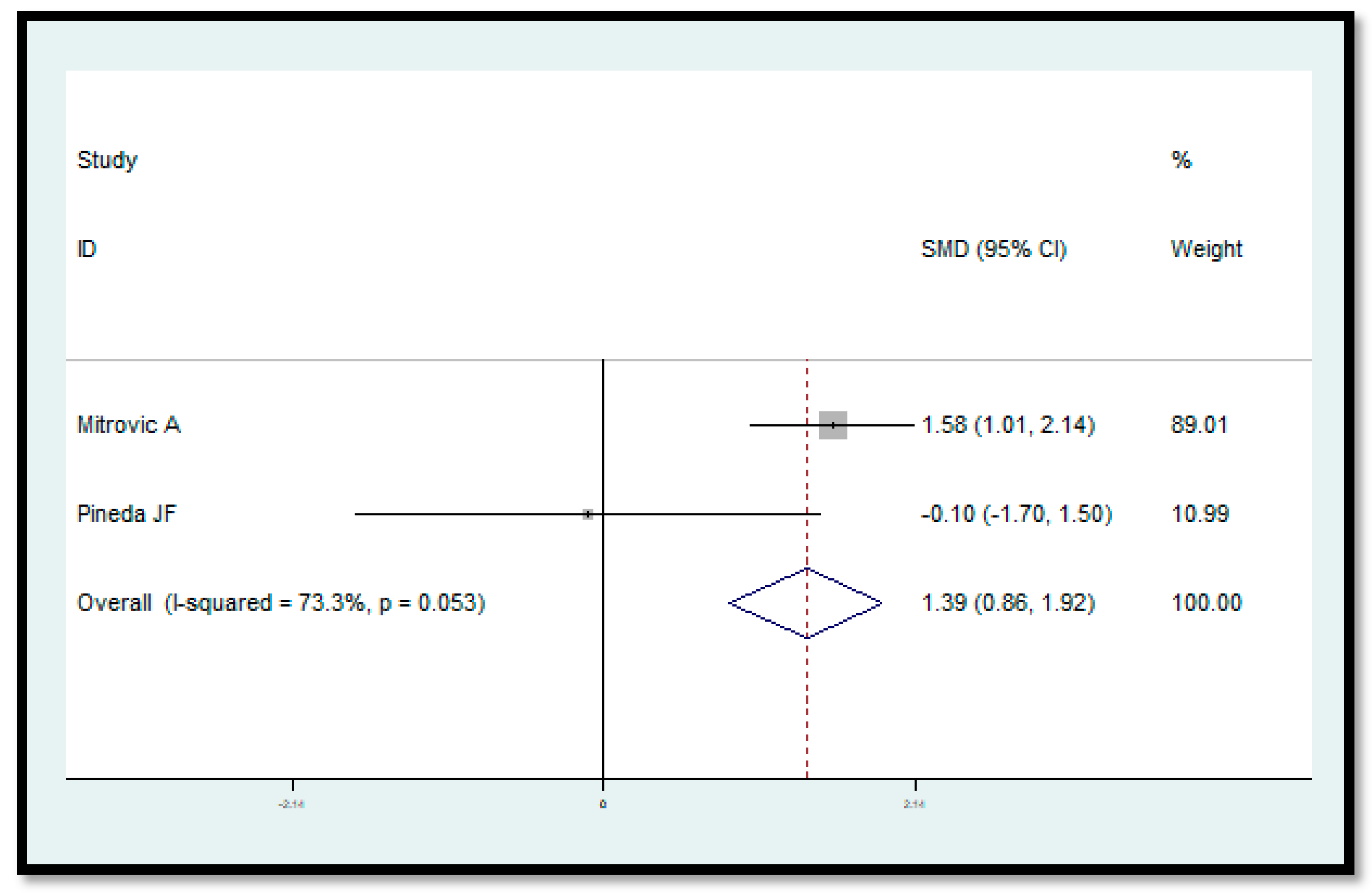
Figure 3.
Forest plot showing SMD in overall studies. The Forest plot shows the effect of HBOT in increasing the endometrial thickness. The use of HBOT causes a significant change in increasing endometrial thickness (p<0.001).
Figure 3.
Forest plot showing SMD in overall studies. The Forest plot shows the effect of HBOT in increasing the endometrial thickness. The use of HBOT causes a significant change in increasing endometrial thickness (p<0.001).
2.6. Study Risk of Bias Assessment
2.6.1. Assessment of Reporting Biases
The biases were analysed using the GRADE pro tool. Where necessary, an explanation of the bias has been provided. No funnel plots have been included due to the small number of studies present, which would have made them useless.
2.7. Effect Measures
2.7.1. Types of Outcome Measures
The results of interest, directly or indirectly related to infertility (laboratory tests, ultrasounds, etc.) are summarized here. As visible in the meta-analysis, for the studies included, the RR (Risk Ratios) and the standardized mean difference (SMD) with 95% confidence intervals (CIs) are cited. Respectively used for binary and continuous outcomes.
2.7.2. Primary Outcomes
The primary outcomes included and represented below are the association between HBOT and [
1] getting pregnant, [
2] endometrial thickness, and [
3] AMH levels.
2.7.3. Secondary Outcomes
No secondary outcomes were included.
2.8. Synthesis Methods
2.8.1. Measures of the Effect of the Methods
Meta-analysis was performed using the ‘metan’ routine by the Stata statistics software (version 13 for Windows Stata Corporation, 2016). Results of the meta-analysis were reported, with 95% confidence intervals (CIs), as pooled risk ratios (RR) for binary outcome and standardized mean difference (SMD) for continuous outcome; p values < 0.05 were considered statistically significant. Meta-analysis made the SMD by the method of Cohen and the RR by the method of Woolf.
2.8.2. Dealing with Missing Data
The missing data has not been entered.
2.8.3. Assessment of Heterogeneity
Between-study heterogeneity was assessed by inspecting the forest plots and the chi-squared test for heterogeneity. I
2 statistic with a value above 50% was interpreted as representing high heterogeneity [
7] and therefore, a random-effects model analysis was performed using the method of DerSimonian & Laird, with the estimate of heterogeneity being taken from the Mantel-Haenszel model. When heterogeneity was modest (I
2 < 50%), a fixed-effects model of analysis was performed using the inverse variance method.
2.8.4. Data Synthesis
For the binary outcome (getting pregnant) the random effects method was chosen due to the large heterogeneity of the studies found. This choice is motivated by the desire to make, at a statistical level, more prudent decisions with a wider confidence interval.
2.8.5. Sensitivity Analysis
The quality of the evidence was assessed with the GRADE pro tool and, specifically, the possible biases and the following items were analysed: 'inconsistency', 'indirectness', 'imprecision'. The result is visible in Figure 5.
2.9. Reporting Bias Assessment
2.9.1. Assessment of Risk of Bias in Included Studies
The risk of bias was calculated using the GRADEpro Guideline Development Tool (McMaster University, 2015 (developed by Evidence Prime, Inc., Hamilton, ON, Canada), accessible from gradepro.org). The risk was finally classified as ‘non-serious’, ‘serious’ and ‘very serious’.
2.10. Certainty Assessment
The GRADE approach was used. It specifies four levels of certainty for a body of evidence for a given outcome: “high”, “moderate”, “low” and “very low”. GRADE assessments of certainty are determined through consideration of five domains: risk of bias, inconsistency, indirectness, imprecision and publication bias.
2.10.1. Main Results
The results, explained in this review, are summarized in the GRADE tables of evidence and Summary of Findings reported in Figure 6. This study demonstrated that there is a link, albeit a weak one due to the limited number of international studies on the subject, between HBOT and female infertility. It emerged that there is no shared protocol and that excessive heterogeneity between studies compromises the evidence and strength of the recommendation for HBOT in female infertility. Evidence suggests that HBOT is probably helpful in the area of female infertility.
3. Results
3.1. Study Selection
3.1.1. Description of Studies
Most of the studies found are observational, case reports, correspondence, pilot studies or reviews.
3.1.2. Results of the Search
The total number of studies found during the search was quite small. Below are the numbers of studies found, divided by database and also represented in the PRISMA flow chart (Figure 2): Cochrane: 3 results; Google Scholar: 10 results; Lilacs: 1 result; Scopus: 9 results; Pubmed: 24 results; Google: 2 results.
3.1.3. Included Studies
From the total of 49 results, 7 studies were eliminated as duplicates, resulting in 42 studies being included. In the end, after other human screenings, 8 studies were found to be useful for a qualitative analysis, 3 of which were useful for a quantitative meta-analysis study.
3.1.4. Excluded Studies
30 studies were excluded as they did not meet the inclusion criteria or fell within the exclusion ones.
3.2. Study Characteristics
3.2.1. Characteristics of Included Studies
The studies that were included in the review are summarized below. The hyperbaric chamber immersion profiles have been highlighted in bold and divided by individual study.
SUPPLEMENTAL FIGURES 2 TO 13
3.2.2. Summary of Findings Tables
3.3. Risk of Bias in Studies
The assessments of risk of bias were done for specific outcomes and reported in the GRADE evidence table (Figure 5) in which a comment, when needed, was added.
3.4. Results Of Individual Studies
3.4.1. Does HBOT Increase Pregnancy Probability? (Analysis 1.1) 3.4.2. Does HBOT Increase Endometrial Thickness? (Analysis 1.2) 3.4.3. Does HBOT Increase AMH Levels? (Analysis 1.3)
No meta-analysis
3.5. Results of Syntheses
3.5.1. Data and Analyses
No difference in conceived with HBO therapy (versus no HBO therapy) was observed in the meta-analysis, RR=1.149, p=0.827 (Figure 3).
Endometrial thickness of the endometrial cycle was measured without HBO and with HBO sessions. A significant change in endometrial thickness was observed in the meta-analysis, the SMD was 1.388, p<0.001 (Figure 4).
3.6. Reporting Biases
The authors carried out an in-depth search following specific inclusion and exclusion criteria, defined before the search. Any results about these were included and analyzed, without language limitations. The search was also extended to protocols not yet published. A funnel graph was not developed due to the limited number of studies in the literature. The biases inherent in the included articles were analyzed by the GRADE tool according to the criteria already specified.
3.7. Certainty of Evidence
3.7.1. Summary of Main Results
The meta-analysis of the various studies included did not show strong evidence, due to the great heterogeneity of the same and the limited number of studies in the literature.
3.7.2. Overall Completeness and Applicability of Evidence
It can be stated, as can be deduced from Figure 6, that the evidence, although built on limited studies and worthy of further study, suggests the use of HBOT in the field of female infertility. The GRADE approach suggests rating the importance of each outcome on a 9-point scale from 1 to 9. An outcome importance rating or assessment is needed to choose which outcomes should be considered when deciding on the advantages and disadvantages of an intervention or which outcomes should be included in a GRADE evidence profile.
Most of the included studies scored 'critical' or 'important', except Pineda's 2015 study [
8] on the topic of the correlation between HBOT and increased endometrial thickness. This choice is due to three reasons: first 1) the number of patients is limited, 2) the choice of patients could have influenced the result, especially when compared to the diametrically opposite results obtained by Mitrović A [
9] and finally 3) the different dive profile may have had a negative impact. On the other hand, the result of the relationship between HBOT and the increase in AHM values assumes greater importance, being the only study that met the inclusion criteria of this review.
3.7.3. Quality of the Evidence
The GRADE methodology was applied to assess the certainty of evidence (CoE) and is represented in Figure 6.
4. Discussion
In this review we focused on the different protocols using hyperbaric oxygen therapy for female infertility and compared them with standard therapy. We analyzed both observational and non-observational studies and tried to answer some questions considered relevant to the topic under discussion.
We found that HBOT increases endometrial thickness in a significant way. Instead, there are no significant evidences linked to pregnancy probability and AMH levels, even if a positive tendency in favor of HBOT is present.
At the moment, there are few evidences suggesting the correlation beetween HBOT and female infertility. We think the reason is in the extreme heterogeneity of the protocols used and, of course, in the limited number of studies on this theme. The lack of a universal protocol seems to be the main problem. The choice of patients, their limited number, the interventions, the ATMs used and the outcomes evaluated are not the same in the studies analyzed. In literature, besides, there are no studies that have strong scientific evidence on the topic.
The hyperoxia-normoxia paradox for female infertility was introduced theorically in this review. Even if it is only a molecular view, the use of intermittent HBOT can regulate the expression of sirtuins, especially SIRT1, essential in female fertility. This correlation was taken into consideration but was not analyzed in this review because of the absence of articles that correlated the use of HBOT in the regulation of sirtuin expression in female infertility. This subject deserves to be explored with further studies that could provide an interesting proposal on which to base the treatment of infertility. In literature there are a lot of studies that underline both how HBOT regulates sirtuins and how they increase female fertility. Nevertheless, none or few of them correlate directly HBOT with female infertility.
Another reason why it would be interesting to investigate this type of link is that inflammation, present in most gynaecological pathologies and a cause of infertility, is well controlled by hyperbaric oxygen therapy [
10].
Methods for Future Updates
For future reviews, opting for a greater number of studies on the subject, it is desirable to specify female infertility in the inclusion criteria with the exclusion of male infertility. In this review, this choice was not made due to the small number of studies present. This would have compromised the study of the link between HBOT and female infertility.
5. Conclusions
The link between HBOT and female infertility is misunderstood and little investigated worldwide. HBOT seems to be useful in increasing endometrial thickness but no evidences are present in pregnancy probability. More studies are needed to explore this promising link which, in some cases, has demonstrated its usefulness, even if indirectly.
The studies present in the literature demonstrate that even today there is no precise and globally accepted protocol on the HBOT profile to be used as a possible treatment for female infertility. It is therefore all the more necessary to standardize not only the choice of infertile patients (precise age range, exclusion of infertility of the partner, etc.) but also the quota to be reached in the hyperbaric chamber and the number of sessions. This is why, together with the great heterogeneity of the included studies, the evidence for a correlation between HBOT use and infertility is present but weak. To do this, it would be advisable to have more studies available to finally be able to compare the different protocols more precisely.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Funding
there is no funding for the project
Acknowledgements
The work is the result of two years of research on the subject in the context of the Second Level University Master in Underwater and Hyperbaric Medicine "PierGiorgio Data" of Sant'Anna School of Advanced Studies (Pisa, Italy) in collaboration with the Institute of Clinical Physiology of CNR" (VIII ed). Each of the authors of this review has provided extensive personal and valuable contributions to this work. In particular, I would like to thank Dr Pasquale Longobardi, Affiliated Researcher at the Scuola Superiore Sant'Anna and Vice President of the "Italian Hyperbaric and Underwater Medical Society", and Prof. Vincenzo Lionetti, Associate Professor of Anesthesiology (Institute of Life Sciences) and President of the Italian "Society of Cardiovascular Research", for their constant support in the conception and writing of the text and Dr Marco Scalese for the statistical contribution and revision.
Data Availability Statement
Enrico MOCCIA, none. Pasquale LONGOBARDI, none. Vincenzo LIONETTI, none. Marco SCALESE, none.
Attestation Statement
• Data regarding any of the subjects in the study has not been previously published unless specified. • Data will be made available to the editors of the journal for review or query upon request.
References
- Carafa V, Rotili D, Forgione M, Cuomo F, Serretiello E, Hailu GS; et al. Sirtuin functions and modulation: From chemistry to the clinic. Clin Epigenetics [Internet]. [CrossRef]
- Yamamoto H, Schoonjans K, Auwerx J. Sirtuin functions in health and disease. Mol Endocrinol. 2007, 21, 1745–1755. [Google Scholar] [CrossRef] [PubMed]
- Di Emidio G, Falone S, Artini PG, Amicarelli F, D’alessandro AM, Tatone C. Mitochondrial sirtuins in reproduction. Antioxidants. 2021, 10, 1–26. [Google Scholar]
- Tatone C, di Emidio G, Barbonetti A, Carta G, Luciano AM, Falone S; et al. Sirtuins in gamete biology and reproductive physiology: Emerging roles and therapeutic potential in female and male infertility. Hum Reprod Update. 2018, 24, 267–289. [Google Scholar] [CrossRef] [PubMed]
- Alam F, Syed H, Amjad S, Baig M, Khan TA, Rehman R. Interplay between oxidative stress, SIRT1, reproductive and metabolic functions. Curr Res Physiol. 2021, 4, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Schottlender N, Gottfried I, Ashery U. Hyperbaric oxygen treatment: Effects on mitochondrial function and oxidative stress. Biomolecules. 2021, 11, 1–17. [Google Scholar]
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Gallardo Pineda JF, López Ortiz CGS, De Siu Moguel GJ, Castro Lopez CRE, Alcocer HM, Velasco ST. Improvement in serum anti-Müllerian hormone levels in infertile patients after hyperbaric oxygen (Preliminary results). J Bras Reprod Assist. 2015, 19, 87–90. [Google Scholar]
- Mitrović A, Nikolić B, Dragojević S, Brkić P, Ljubić A, Jovanović T. Hyperbaric oxygenation as a possible therapy of choice for infertility treatment. Bosn J Basic Med Sci. 2006, 6, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Verdini F, Cannellotto M, Romero-feris D. Oxigenación hiperbárica en el tratamiento de la infertilidad Hyperbaric oxygenation for infertility treatment. 39, 3–8.
- Feng J, Wang J, Zhang Y, Zhang Y, Jia L, Zhang D; et al. The Efficacy of Complementary and Alternative Medicine in the Treatment of Female Infertility. Evidence-based Complement Altern Med. 2021, 2021.
- Leverment J, Turner R, Bowman M, Cooke CJ. Report of the use of hyperbaric oxygen therapy (HBO2) in an unusual case of secondary infertility. Undersea Hyperb Med J Undersea Hyperb Med Soc Inc. 2004, 31, 245–250. [Google Scholar]
- Van Voorhis BJ, Greensmith JE, Dokras A, Sparks AET, Simmons ST, Syrop CH. Hyperbaric oxygen and ovarian follicular stimulation for in vitro fertilization: A pilot study. Fertil Steril. 2005, 83, 226–228. [Google Scholar] [CrossRef] [PubMed]
-
Wang D, Jiang Y, Feng J, Gao J, Yu J, Zhao J; et al. Evidence for the Use of Complementary and Alternative Medicine for Pelvic Inflammatory Disease: A Literature Review. Evidence-based Complement Altern Med. 2022, 2022.
- Yu J, Qi YL, Lu DW, Fang QJ, Li L, Sang L. Multiple Protocols Combined with Hyperbaric Oxygen Therapy on the Maintenance of Ovarian Function in Patients After Ovarian Cystectomy. Front Surg. 2022, 9.
- Available online: https://www.who.int/news-room/fact-sheets/detail/infertility.
- Available online: https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12621001671853.
- Available online: https://www.reproductivemedicine.com/toc/auto_abstract.php?id=24805.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).