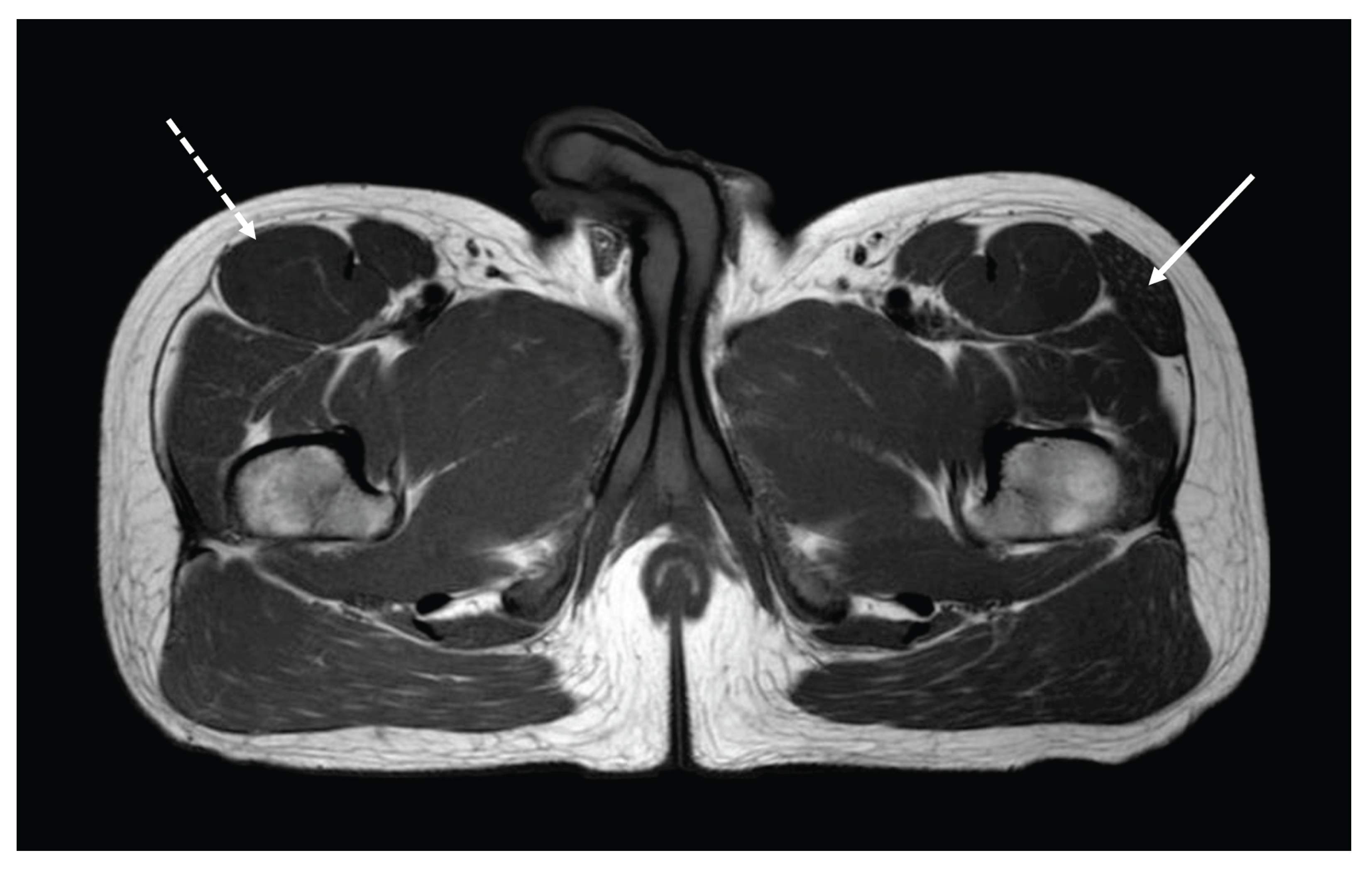
Figure 1.
A 25-year-old physician (T.B.) born from non-consanguineous parents was included as a healthy control in a muscle-MRI study conducted by the third author (G.B.) on genetic myopathies as a part of his pediatric residency thesis. T1-weighted axial sections performed at the lower girdle level surprisingly showed the agenesis of the right TFL with mild compensatory hypertrophy of the ipsilateral rectus femoris (dashed arrow) and unaffected surrounding tissues. A normal appearance of the right TFL was noted on the left side (arrow). Muscle MRI was bilaterally normal at thigh and leg levels. The tensor fasciae lata (TFL) is a muscle of the proximal anterolateral thigh that lies between the superficial and deep fibers of the iliotibial (IT) band [
1]. There is high variability in muscle belly length, although, in most patients, the TFL muscle belly ends before the greater trochanter of the femur [
1,
2]. The exact role of TFL is not entirely clear. However, it cooperates with the gluteus maximus, gluteus medius, and gluteus minimus in various hip movements, including flexion, abduction, and internal rotation [
1]. Furthermore, TFL acts via the IT band's attachment to the tibia to assist with knee flexion and lateral rotation. The TFL can be considered clinically important for assisting pelvic stability while standing and walking [
1]. Although rarely reported, conditions associated with TFL impairment may present as pain and dysfunction in the hip, pelvis, and spine region [
3]. These conditions include benign and malignant lesions, such as lipoma, liposarcoma, intramuscular lymphoma and metastases, arteriovenous malformations, muscular atrophy, and adipose pseudohypertrophy [
3]. Congenital agenesis of the TFL muscle is an extremely rare anomaly in which the muscle fails to develop during embryogenesis due to unknown reasons. Very little is known about the impact of TFL absence on human life [
4,
5].
Figure 1.
A 25-year-old physician (T.B.) born from non-consanguineous parents was included as a healthy control in a muscle-MRI study conducted by the third author (G.B.) on genetic myopathies as a part of his pediatric residency thesis. T1-weighted axial sections performed at the lower girdle level surprisingly showed the agenesis of the right TFL with mild compensatory hypertrophy of the ipsilateral rectus femoris (dashed arrow) and unaffected surrounding tissues. A normal appearance of the right TFL was noted on the left side (arrow). Muscle MRI was bilaterally normal at thigh and leg levels. The tensor fasciae lata (TFL) is a muscle of the proximal anterolateral thigh that lies between the superficial and deep fibers of the iliotibial (IT) band [
1]. There is high variability in muscle belly length, although, in most patients, the TFL muscle belly ends before the greater trochanter of the femur [
1,
2]. The exact role of TFL is not entirely clear. However, it cooperates with the gluteus maximus, gluteus medius, and gluteus minimus in various hip movements, including flexion, abduction, and internal rotation [
1]. Furthermore, TFL acts via the IT band's attachment to the tibia to assist with knee flexion and lateral rotation. The TFL can be considered clinically important for assisting pelvic stability while standing and walking [
1]. Although rarely reported, conditions associated with TFL impairment may present as pain and dysfunction in the hip, pelvis, and spine region [
3]. These conditions include benign and malignant lesions, such as lipoma, liposarcoma, intramuscular lymphoma and metastases, arteriovenous malformations, muscular atrophy, and adipose pseudohypertrophy [
3]. Congenital agenesis of the TFL muscle is an extremely rare anomaly in which the muscle fails to develop during embryogenesis due to unknown reasons. Very little is known about the impact of TFL absence on human life [
4,
5].
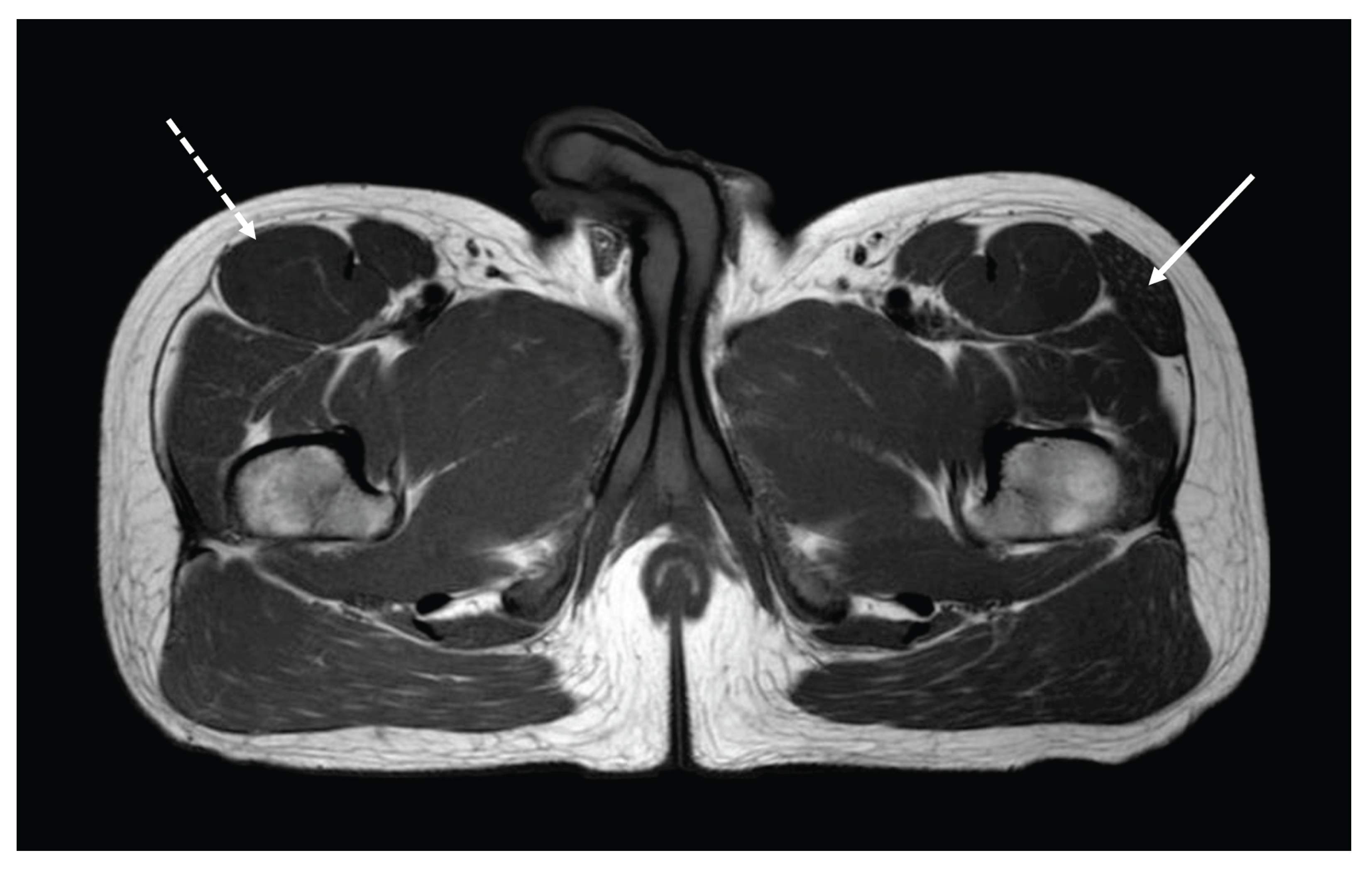
Figure 2.
Two years earlier, T.B. had participated in the New York Marathon, unaware of his defect, completing the course in 4 hours and 16 minutes (
Figure 2). He had always led an unrestricted sporting life with no particular symptoms due to exercise. However, neurological evaluation pointed out a very slight waddling gait with normal strength tests. He had no signs of neuromuscular or other diseases. Creatine-kinase levels were in the normal range. Electromyography was not performed. Exploring his medical history, his parents reported that he likely did not crawl as an infant, a typical developmental milestone that, in light of our findings, could be associated with the normal development of the TFL muscle. Thirteen years after the marathon, T.B. is in good general health, has an unchanged clinical neurological examination, regularly plays sports, and continues not to complain of painful symptoms after exercise. Agenesis of TFL is rarely reported in the literature [
4,
5] and when present, it is often discovered incidentally during diagnostic tests for other conditions. For this reason, the real incidence is reasonably underestimated and not known. As shown in our report, individuals with TFL agenesis can lead normal lives and even engage in strenuous activities without any apparent difficulty, as the body may compensate by utilizing other muscles that perform similar functions. However, long-term monitoring is needed, as, over time, this condition could lead to increased fatigue, muscle pain, or difficulty with movements involving the hip. In some cases, therapeutic interventions focused on symptom management and rehabilitation may be necessary to improve lower limb mobility and function.
Figure 2.
Two years earlier, T.B. had participated in the New York Marathon, unaware of his defect, completing the course in 4 hours and 16 minutes (
Figure 2). He had always led an unrestricted sporting life with no particular symptoms due to exercise. However, neurological evaluation pointed out a very slight waddling gait with normal strength tests. He had no signs of neuromuscular or other diseases. Creatine-kinase levels were in the normal range. Electromyography was not performed. Exploring his medical history, his parents reported that he likely did not crawl as an infant, a typical developmental milestone that, in light of our findings, could be associated with the normal development of the TFL muscle. Thirteen years after the marathon, T.B. is in good general health, has an unchanged clinical neurological examination, regularly plays sports, and continues not to complain of painful symptoms after exercise. Agenesis of TFL is rarely reported in the literature [
4,
5] and when present, it is often discovered incidentally during diagnostic tests for other conditions. For this reason, the real incidence is reasonably underestimated and not known. As shown in our report, individuals with TFL agenesis can lead normal lives and even engage in strenuous activities without any apparent difficulty, as the body may compensate by utilizing other muscles that perform similar functions. However, long-term monitoring is needed, as, over time, this condition could lead to increased fatigue, muscle pain, or difficulty with movements involving the hip. In some cases, therapeutic interventions focused on symptom management and rehabilitation may be necessary to improve lower limb mobility and function.

Author Contributions
Conceptualization, T.B., C.B, and G.B.; methodology, T.B. and G.B.; software, G.B.; investigation, T.B., C.B., and G.B.; data curation, G.B.; writing—original draft preparation, T.B. and G.B.; writing—review and editing, C.B.; visualization, T.B.; supervision, C.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Data are available on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| TFL |
Tensor Fasciae Lata |
| IT |
Ileo-Tibial |
References
- Trammell, A.P.; Nahian, A.; Pilson, H. Anatomy, Bony Pelvis and Lower Limb: Tensor Fasciae Latae Muscle. 2023 Aug 17. In StatPearls [Internet]; Treasure Island (FL): StatPearls Publishing, Jan 2025. [Google Scholar] [PubMed]
- Cho, K.H.; Jin, Z.W.; Abe, H.; Wilting, J.; Murakami, G.; Rodríguez-Vázquez, J.F. Tensor fasciae latae muscle in human embryos and foetuses with special reference to its contribution to the development of the iliotibial tract. Folia Morphol (Warsz). 2018, 77, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, K.P.; Azzopardi, C.; Kiernan, G.; Botchu, R. Isolated pathologies of Tensor Fasciae Latae: Retrospective cohort analysis from a tertiary referral centre. J Clin Orthop Trauma. 2022, 29, 101870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meberg, A.; Skogen, P. Three different manifestations of congenital muscular aplasia in a family. Acta Paediatr Scand. 1987, 76, 375–377. [Google Scholar] [CrossRef] [PubMed]
- Randelli, F.; Papavasiliou, A.; Mazzoleni, M.G.; Fioruzzi, A.; Basile, G.; Ganz, R. Femoral head necrosis and progressive osteoarthritis of a healed intracapital osteotomy in a severe sequelae of Legg-Calvé-Perthes disease with aplasia of tensor fasciae latae. J Hip Preserv Surg. 2021, 8 (Suppl 1), i16–i24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).